Acne vulgaris

First-line therapy
Efficacy of a combined oral contraceptive containing 0.030 mg ethinylestradiol/2 mg dienogest for the treatment of papulopustular acne in comparison with placebo and 0.035 mg ethinylestradiol/2 mg cyproterone acetate.
Palombo-Kinne E, Schellschmidt I, Schumacher U, Gräser T. Contraception 2009; 79: 282–9.
Second-line therapy
Randomized trial comparing a chemical peel containing a lipophilic hydroxy acid derivative of salicylic acid with a salicylic acid peel in subjects with comedonal acne.
Levesque A, Hamzavi I, Seite S, Rougier A, Bissonnette R. J Cosmet Dermatol 2011; 10: 174–8.
Lipohydroxy acid is a lipophilic derivative of salicylic acid with comedolytic properties.



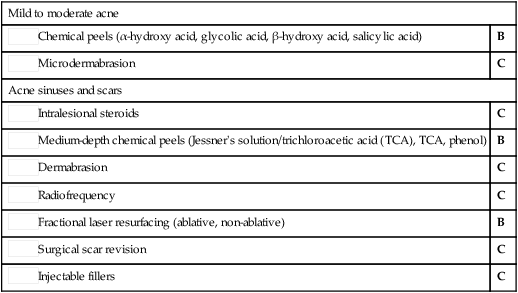
 Topical retinoids
Topical retinoids Dapsone gel with topical retinoid
Dapsone gel with topical retinoid Benzoyl peroxide with topical retinoid
Benzoyl peroxide with topical retinoid Benzoyl peroxide with topical antibiotic
Benzoyl peroxide with topical antibiotic Benzoyl peroxide with topical retinoid
Benzoyl peroxide with topical retinoid Benzoyl peroxide with topical antibiotic
Benzoyl peroxide with topical antibiotic For males use oral antibiotics (tetracyclines, macrolides) with benzoyl peroxide or topical retinoid
For males use oral antibiotics (tetracyclines, macrolides) with benzoyl peroxide or topical retinoid For females use an oral anti-androgen contraceptive with benzoyl peroxide and topical antibiotic
For females use an oral anti-androgen contraceptive with benzoyl peroxide and topical antibiotic Oral isotretinoin
Oral isotretinoin Oral isotretinoin
Oral isotretinoin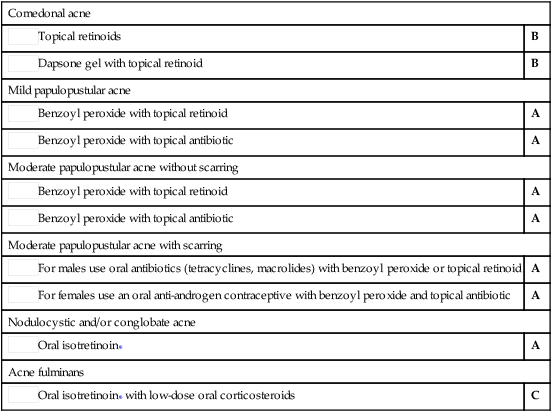
 Benzoyl peroxide (topical)
Benzoyl peroxide (topical) Azelaic acid
Azelaic acid Superficial peels (lipohydroxy acid, salicylic acid)
Superficial peels (lipohydroxy acid, salicylic acid) Azelaic acid
Azelaic acid Benzoyl peroxide (topical)
Benzoyl peroxide (topical) Topical retinoid
Topical retinoid Topical nadifloxacin
Topical nadifloxacin Azelaic acid with topical clindamycin
Azelaic acid with topical clindamycin Azelaic acid with topical erythromycin
Azelaic acid with topical erythromycin Dapsone gel
Dapsone gel Dapsone gel with topical retinoid
Dapsone gel with topical retinoid Dapsone gel with benzoyl peroxide (topical)
Dapsone gel with benzoyl peroxide (topical) Systemic antibiotic with adapalene
Systemic antibiotic with adapalene Topical erythromycin with topical retinoid
Topical erythromycin with topical retinoid Picolinic acid
Picolinic acid Oral zinc
Oral zinc Photodynamic therapy
Photodynamic therapy Intense pulsed light (IPL)
Intense pulsed light (IPL) Photodynamic therapy with IPL
Photodynamic therapy with IPL Blue light
Blue light Blue/red light combinations
Blue/red light combinations Red low-level laser therapy (LLLT)
Red low-level laser therapy (LLLT) 1,450 nm diode laser
1,450 nm diode laser Topical cyproterone acetate
Topical cyproterone acetate Zileuton
Zileuton Topical copaiba essential oil gel
Topical copaiba essential oil gel Topical 5% tea tree oil gel
Topical 5% tea tree oil gel Glycolic acid oil-in-water emulsion
Glycolic acid oil-in-water emulsion Chemical peels (α-hydroxy acid, glycolic acid, β-hydroxy acid, salicylic acid)
Chemical peels (α-hydroxy acid, glycolic acid, β-hydroxy acid, salicylic acid) Microdermabrasion
Microdermabrasion Oral antibiotic plus topical retinoid
Oral antibiotic plus topical retinoid Oral antibiotic plus azelaic acid
Oral antibiotic plus azelaic acid Oral antibiotic plus topical retinoid plus benzoyl peroxide
Oral antibiotic plus topical retinoid plus benzoyl peroxide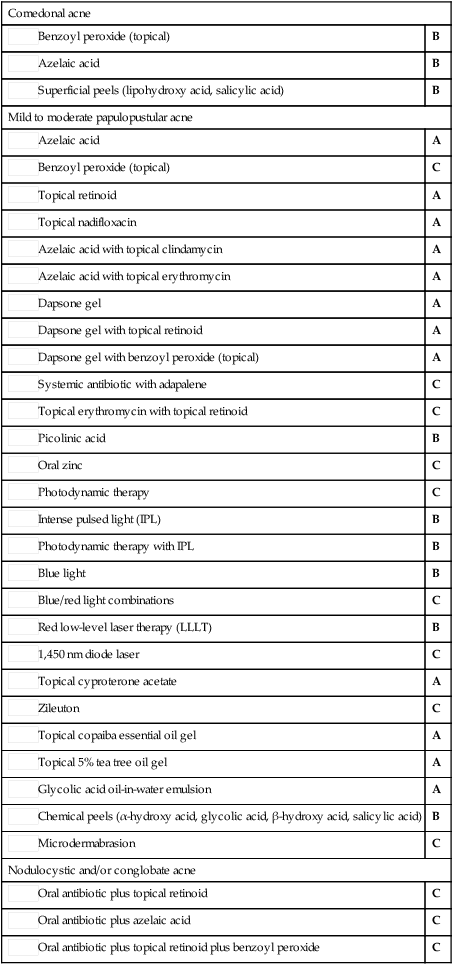
 Chemical peels (α-hydroxy acid, glycolic acid, β-hydroxy acid, salicylic acid)
Chemical peels (α-hydroxy acid, glycolic acid, β-hydroxy acid, salicylic acid) Microdermabrasion
Microdermabrasion Intralesional steroids
Intralesional steroids Medium-depth chemical peels (Jessner’s solution/trichloroacetic acid (TCA), TCA, phenol)
Medium-depth chemical peels (Jessner’s solution/trichloroacetic acid (TCA), TCA, phenol) Dermabrasion
Dermabrasion Radiofrequency
Radiofrequency Fractional laser resurfacing (ablative, non-ablative)
Fractional laser resurfacing (ablative, non-ablative) Surgical scar revision
Surgical scar revision Injectable fillers
Injectable fillers