Chapter 12 Cough, Cold, and Allergy
Antitussives
Moa (Mechanism of Action)
 Antitussives are cough suppressants. There are two ways to inhibit coughing: centrally and peripherally.
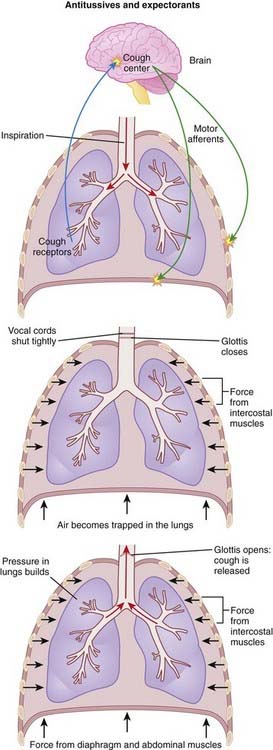
Antitussives are cough suppressants. There are two ways to inhibit coughing: centrally and peripherally. Cough is normally produced through the stimulation of sensory receptors of the glossopharyngeal and vagus nerves, innervating the mucous membranes of the lower pharynx, larynx, trachea, and smaller airways of the respiratory system. The receptors then transmit the signal to the cough center in the brain, which then triggers a reflex motor response that results in contraction of the muscles to close the glottis (vocal cords) and contraction of the muscles of expiration. The result is a sudden increase in intrathoracic pressure, followed by relaxation of the vocal cords, resulting in rapid expulsion of air (Figure 12-1).
Cough is normally produced through the stimulation of sensory receptors of the glossopharyngeal and vagus nerves, innervating the mucous membranes of the lower pharynx, larynx, trachea, and smaller airways of the respiratory system. The receptors then transmit the signal to the cough center in the brain, which then triggers a reflex motor response that results in contraction of the muscles to close the glottis (vocal cords) and contraction of the muscles of expiration. The result is a sudden increase in intrathoracic pressure, followed by relaxation of the vocal cords, resulting in rapid expulsion of air (Figure 12-1). Centrally acting agents such as dextromethorphan work by inhibiting the cough center in the brain, elevating the threshold for coughing. The exact mechanism by which they do this is still poorly understood. Dextromethorphan, for example, is an N-methyl-d-aspartate (NMDA) antagonist, although it is not known what contribution this has to its antitussive effects.
Centrally acting agents such as dextromethorphan work by inhibiting the cough center in the brain, elevating the threshold for coughing. The exact mechanism by which they do this is still poorly understood. Dextromethorphan, for example, is an N-methyl-d-aspartate (NMDA) antagonist, although it is not known what contribution this has to its antitussive effects.Important Notes
 Dextromethorphan was developed in an attempt to create a cough suppressant with the efficacy of codeine but with none of the central nervous system (CNS) side effects such as euphoria. Dextromethorphan therefore has little or no ability to induce euphoria and therefore is available without a prescription and without pharmacist consultation in most jurisdictions.
Dextromethorphan was developed in an attempt to create a cough suppressant with the efficacy of codeine but with none of the central nervous system (CNS) side effects such as euphoria. Dextromethorphan therefore has little or no ability to induce euphoria and therefore is available without a prescription and without pharmacist consultation in most jurisdictions. However, very high doses of dextromethorphan can cause dissociative effects similar to those seen with phencyclidine (PCP). PCP and dextromethorphan are both NMDA antagonists, and this is believed to be why they share similar effects. The doses needed to achieve this effect with dextromethorphan are high enough to cause toxicities resulting in hypertension, tachycardia, and respiratory depression.
However, very high doses of dextromethorphan can cause dissociative effects similar to those seen with phencyclidine (PCP). PCP and dextromethorphan are both NMDA antagonists, and this is believed to be why they share similar effects. The doses needed to achieve this effect with dextromethorphan are high enough to cause toxicities resulting in hypertension, tachycardia, and respiratory depression. Codeine can be an effective antitussive at lower doses than required for analgesia. Therefore some of the more important side effects of codeine, such as respiratory depression, can generally be avoided at the antitussive dose. The exception appears to be young children (≤5 years of age) who may be more sensitive to the respiratory depression. Codeine is therefore not recommended for children under the age of 2 and should be used with caution in children 2 to 5 years old.
Codeine can be an effective antitussive at lower doses than required for analgesia. Therefore some of the more important side effects of codeine, such as respiratory depression, can generally be avoided at the antitussive dose. The exception appears to be young children (≤5 years of age) who may be more sensitive to the respiratory depression. Codeine is therefore not recommended for children under the age of 2 and should be used with caution in children 2 to 5 years old. The use of cough and cold preparations in children, particularly combination products, has come under close scrutiny owing to concerns over deaths attributed to overdose. The use of multiple combination products facilitates overdose, as parents can be easily confused by the duplication of ingredients among products. In addition, the lack of clear evidence of efficacy of these products in young children has prompted many to question why they are used at all.
The use of cough and cold preparations in children, particularly combination products, has come under close scrutiny owing to concerns over deaths attributed to overdose. The use of multiple combination products facilitates overdose, as parents can be easily confused by the duplication of ingredients among products. In addition, the lack of clear evidence of efficacy of these products in young children has prompted many to question why they are used at all.Evidence
Over-the-Counter Preparations for Acute Cough
 A 2008 Cochrane review (25 trials, N = 3492 participants) assessed the effects of over-the-counter (OTC) cough preparations for acute cough. Six trials in adults had variable results for antitussives versus placebo. Of the two trials involving expectorants, one showed benefit versus placebo whereas the other did not. In children, antitussives (two trials), antihistamines (two trials), antihistamine-decongestant combinations (two trials), and antitussive-bronchodilator combinations were no more effective than placebo. No trials were found of expectorants, but one trial showed benefit of a mucolytic versus placebo.
A 2008 Cochrane review (25 trials, N = 3492 participants) assessed the effects of over-the-counter (OTC) cough preparations for acute cough. Six trials in adults had variable results for antitussives versus placebo. Of the two trials involving expectorants, one showed benefit versus placebo whereas the other did not. In children, antitussives (two trials), antihistamines (two trials), antihistamine-decongestant combinations (two trials), and antitussive-bronchodilator combinations were no more effective than placebo. No trials were found of expectorants, but one trial showed benefit of a mucolytic versus placebo.Expectorants
Moa (Mechanism of Action)
 Mucus serves as an airway lubricant and functions as a first level of immune defense. When mucus becomes thickened and/or dried out by infections, the functions of the mucus, including the clearing of infections, becomes impaired.
Mucus serves as an airway lubricant and functions as a first level of immune defense. When mucus becomes thickened and/or dried out by infections, the functions of the mucus, including the clearing of infections, becomes impaired.Important Notes
 There has been a longstanding controversy over the use of expectorants. This is partly because of the limited data demonstrating their efficacy.
There has been a longstanding controversy over the use of expectorants. This is partly because of the limited data demonstrating their efficacy. The use of cough and cold preparations in children, particularly combination products, has come under close scrutiny because of concerns over deaths attributed to overdose. The use of multiple combination products facilitates overdose, as parents can be easily confused by the duplication of ingredients among products. In addition, the lack of clear evidence of efficacy of these products in young children has prompted many to question why they are used at all.
The use of cough and cold preparations in children, particularly combination products, has come under close scrutiny because of concerns over deaths attributed to overdose. The use of multiple combination products facilitates overdose, as parents can be easily confused by the duplication of ingredients among products. In addition, the lack of clear evidence of efficacy of these products in young children has prompted many to question why they are used at all. Guaifenesin is the most widely used expectorant. Other agents that have been used as expectorants include ammonium chloride, which can cause acidosis in patients with renal failure; terpin hydrate, which can cause nausea and vomiting; potassium iodide, which has several side effects; and iodinated glycerol.
Guaifenesin is the most widely used expectorant. Other agents that have been used as expectorants include ammonium chloride, which can cause acidosis in patients with renal failure; terpin hydrate, which can cause nausea and vomiting; potassium iodide, which has several side effects; and iodinated glycerol.Evidence
Over-the-Counter Preparations for Acute Cough
 A 2008 Cochrane review (25 trials, N = 3492 participants) assessed the effects of OTC cough preparations for acute cough. Of the two trials involving expectorants, one showed benefit versus placebo whereas the other did not. In children, no trials were found of expectorants, but one trial showed benefit of a mucolytic versus placebo.
A 2008 Cochrane review (25 trials, N = 3492 participants) assessed the effects of OTC cough preparations for acute cough. Of the two trials involving expectorants, one showed benefit versus placebo whereas the other did not. In children, no trials were found of expectorants, but one trial showed benefit of a mucolytic versus placebo.Decongestants
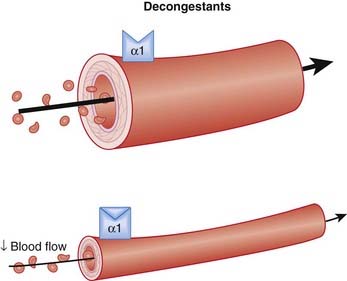
Moa (Mechanism of Action) (Figure 12-2)
 Nasal congestion occurs when the nasal passages become edematous, usually a result of an inflammatory response to an upper respiratory tract infection, an allergic response, or a response to chemical irritant
Nasal congestion occurs when the nasal passages become edematous, usually a result of an inflammatory response to an upper respiratory tract infection, an allergic response, or a response to chemical irritant The main mechanism by which they reduce nasal congestion is by constricting precapillary blood vessels, which reduces capillary hydrostatic pressure, blood flow, and volume. Hydrostatic pressure is one of the forces that pushes plasma out of a blood vessel into the tissues, causing edema. Capillary permeability and oncotic pressure are the two other factors that influence the formation of tissue edema.
The main mechanism by which they reduce nasal congestion is by constricting precapillary blood vessels, which reduces capillary hydrostatic pressure, blood flow, and volume. Hydrostatic pressure is one of the forces that pushes plasma out of a blood vessel into the tissues, causing edema. Capillary permeability and oncotic pressure are the two other factors that influence the formation of tissue edema. By reducing hydrostatic pressure, the outward force that pushes fluid out of the vessel becomes an inward force that drives fluid into the vessel. The net effect is to reduce leakage in blood vessels, therefore reducing congestion.
By reducing hydrostatic pressure, the outward force that pushes fluid out of the vessel becomes an inward force that drives fluid into the vessel. The net effect is to reduce leakage in blood vessels, therefore reducing congestion. Through reduction of blood flow and volume, a smaller amount of fluid is made available to the leaky capillaries, and thus edema formation decreases as well.
Through reduction of blood flow and volume, a smaller amount of fluid is made available to the leaky capillaries, and thus edema formation decreases as well.Pharmacokinetics
Contraindications
 Concomitant use with monoamine oxidase inhibitors (MAOIs): Monoamine oxidase breaks down amines such as norepinephrine. Concomitant use of MAOIs with indirect-acting decongestants such as pseudoephedrine that increase norepinephrine can lead to excess norepinephrine and hypertensive crisis. MOAIs are used to treat depression and are not commonly used because newer agents have replaced them.
Concomitant use with monoamine oxidase inhibitors (MAOIs): Monoamine oxidase breaks down amines such as norepinephrine. Concomitant use of MAOIs with indirect-acting decongestants such as pseudoephedrine that increase norepinephrine can lead to excess norepinephrine and hypertensive crisis. MOAIs are used to treat depression and are not commonly used because newer agents have replaced them.Side Effects
 CNS stimulation: The phenylamines (phenylephrine, ephedrine, pseudoephedrine) share common structural features with amphetamine, and therefore they also stimulate the CNS. This manifests as:
CNS stimulation: The phenylamines (phenylephrine, ephedrine, pseudoephedrine) share common structural features with amphetamine, and therefore they also stimulate the CNS. This manifests as:
 Rhinitis medicamentosa: Rebound congestion is typically only seen with topical agents. This is a pharmacologic phenomenon that occurs with chronic use, secondary to changes in receptor density. Patients will find that their decongestant does not work as well, that their congestion is much worse when they miss a dose of the drug, or both. The net effect is that the patient finds that he or she is unable to discontinue the decongestant.
Rhinitis medicamentosa: Rebound congestion is typically only seen with topical agents. This is a pharmacologic phenomenon that occurs with chronic use, secondary to changes in receptor density. Patients will find that their decongestant does not work as well, that their congestion is much worse when they miss a dose of the drug, or both. The net effect is that the patient finds that he or she is unable to discontinue the decongestant. Increased blood pressure: Constriction caused by peripheral α1 receptors leads to increased resistance and therefore increased blood pressure. This problem is more likely to be seen with oral agents and is usually a problem only in patients who have hypertension.
Increased blood pressure: Constriction caused by peripheral α1 receptors leads to increased resistance and therefore increased blood pressure. This problem is more likely to be seen with oral agents and is usually a problem only in patients who have hypertension. Urinary retention: Stimulation of α1 receptors in the bladder leads to constriction of the urinary sphincter, restricting the flow of urine. This is typically a problem only in patients with preexisting urinary retention or in conditions such as enlarged prostate, in which patients are more prone to urinary retention.
Urinary retention: Stimulation of α1 receptors in the bladder leads to constriction of the urinary sphincter, restricting the flow of urine. This is typically a problem only in patients with preexisting urinary retention or in conditions such as enlarged prostate, in which patients are more prone to urinary retention.Important Notes
 Rhinitis medicamentosa is an uncomfortable complication of topical decongestant use. However, because it is a simple pharmacodynamic phenomenon, patients should inevitably improve once receptor densities have returned to their predrug state. This typically takes 1 to 2 weeks, and in the intervening period the patient may benefit from oral decongestants to get through the periods of severe congestion.
Rhinitis medicamentosa is an uncomfortable complication of topical decongestant use. However, because it is a simple pharmacodynamic phenomenon, patients should inevitably improve once receptor densities have returned to their predrug state. This typically takes 1 to 2 weeks, and in the intervening period the patient may benefit from oral decongestants to get through the periods of severe congestion. Vasoconstrictors have the greatest efficacy among decongestants; however, there are other agents that are used to relieve nasal congestion. Camphor, menthol, and eucalyptus oil are all considered to be relatively innocuous, although their efficacy in treating nasal congestion and the mechanism by which they exert their effects are not well studied.
Vasoconstrictors have the greatest efficacy among decongestants; however, there are other agents that are used to relieve nasal congestion. Camphor, menthol, and eucalyptus oil are all considered to be relatively innocuous, although their efficacy in treating nasal congestion and the mechanism by which they exert their effects are not well studied. The use of cough and cold preparations in children, particularly combination products, has come under close scrutiny because of concerns over deaths attributed to overdose. The use of multiple combination products facilitates overdose, as parents can be easily confused by the duplication of ingredients among products. In addition, the lack of clear evidence of efficacy of these products in young children has prompted many to question why they are used at all.
The use of cough and cold preparations in children, particularly combination products, has come under close scrutiny because of concerns over deaths attributed to overdose. The use of multiple combination products facilitates overdose, as parents can be easily confused by the duplication of ingredients among products. In addition, the lack of clear evidence of efficacy of these products in young children has prompted many to question why they are used at all.Evidence
Nasal Congestion in the Common Cold
 A 2009 Cochrane review (seven trials, all in adults) assessed the efficacy of nasal decongestants in reducing symptoms of nasal congestion in adults and children with the common cold. There was a 6% decrease in subjective symptoms after a single oral dose of decongestant versus placebo. From a clinical standpoint, this is a small difference. With repeated use over 3 to 5 days, the benefit decreased to 4%. Only two trials reported safety measures, but in these two trials there was a small increased risk of insomnia versus placebo.
A 2009 Cochrane review (seven trials, all in adults) assessed the efficacy of nasal decongestants in reducing symptoms of nasal congestion in adults and children with the common cold. There was a 6% decrease in subjective symptoms after a single oral dose of decongestant versus placebo. From a clinical standpoint, this is a small difference. With repeated use over 3 to 5 days, the benefit decreased to 4%. Only two trials reported safety measures, but in these two trials there was a small increased risk of insomnia versus placebo.FYI Notes
 Ephedrine is structurally related to the amphetamines. The main difference from a pharmacologic perspective is that ephedrine and pseudoephedrine have less effect on the CNS. Ephedrine is also used to raise heart rate and blood pressure, most commonly in anesthetized patients. It is given intravenously for this indication.
Ephedrine is structurally related to the amphetamines. The main difference from a pharmacologic perspective is that ephedrine and pseudoephedrine have less effect on the CNS. Ephedrine is also used to raise heart rate and blood pressure, most commonly in anesthetized patients. It is given intravenously for this indication. Although phenylpropanolamine is also supposed to have fewer CNS effects than amphetamine, its use in children has come under scrutiny because of CNS adverse effects such as agitation, irritability, and insomnia. Most jurisdictions have removed phenylpropanolamine from the market or severely restricted access to it.
Although phenylpropanolamine is also supposed to have fewer CNS effects than amphetamine, its use in children has come under scrutiny because of CNS adverse effects such as agitation, irritability, and insomnia. Most jurisdictions have removed phenylpropanolamine from the market or severely restricted access to it. Decongestants are available without a prescription in most jurisdictions. However, their use is often still monitored closely, as they have become drugs of abuse for their stimulant properties. Ephedrine and pseudoephedrine can also readily be converted into amphetamine derivatives such as methamphetamine (also known as crystal meth).
Decongestants are available without a prescription in most jurisdictions. However, their use is often still monitored closely, as they have become drugs of abuse for their stimulant properties. Ephedrine and pseudoephedrine can also readily be converted into amphetamine derivatives such as methamphetamine (also known as crystal meth).H1 Antagonists
Moa (Mechanism of Action)
 Histamine is mainly synthesized in mast cells and basophils of the immune system, enterochromaffin-like cells in gastric mucosa, and certain neurons that release it as a neurotransmitter.
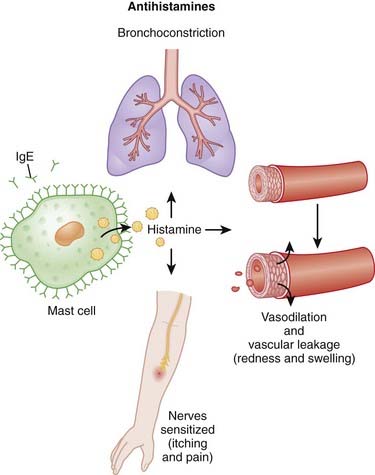
Histamine is mainly synthesized in mast cells and basophils of the immune system, enterochromaffin-like cells in gastric mucosa, and certain neurons that release it as a neurotransmitter. Histamine plays a key role in allergic reactions, also known as immunoglobulin E (IgE)–mediated hypersensitivity reactions. The role of histamine in the immune response is largely mediated by H1 receptors. Classic hallmarks of an immune response that is mediated by H1 include the following (Figure 12-3):
Histamine plays a key role in allergic reactions, also known as immunoglobulin E (IgE)–mediated hypersensitivity reactions. The role of histamine in the immune response is largely mediated by H1 receptors. Classic hallmarks of an immune response that is mediated by H1 include the following (Figure 12-3):
 H1-receptor antagonists competitively antagonize histamine at these receptors, mitigating the immune response to an allergen.
H1-receptor antagonists competitively antagonize histamine at these receptors, mitigating the immune response to an allergen.Pharmacokinetics
 Antihistamines vary in their ability to cross the blood-brain barrier. Second-generation agents penetrate much more slowly and in lower quantities compared with first-generation agents. This is one reason why second-generation agents are much less sedating than first-generation agents.
Antihistamines vary in their ability to cross the blood-brain barrier. Second-generation agents penetrate much more slowly and in lower quantities compared with first-generation agents. This is one reason why second-generation agents are much less sedating than first-generation agents.Side Effects
Important Notes
 Two factors appear to play a role in distinguishing sedating from nonsedating antihistamines. Aside from the pharmacokinetic property of being able to cross into the CNS, some antihistamines also antagonize serotonin (5-HT2) receptors. For the agents that cross into the CNS, this contributes further to their sedating properties.
Two factors appear to play a role in distinguishing sedating from nonsedating antihistamines. Aside from the pharmacokinetic property of being able to cross into the CNS, some antihistamines also antagonize serotonin (5-HT2) receptors. For the agents that cross into the CNS, this contributes further to their sedating properties. Antihistamines are not typically useful for life-threatening anaphylactic reactions, which are managed acutely with an injection of epinephrine. Antihistamines typically do not work quickly enough to be useful in these situations, but they also fail to address many of the most important characteristics of anaphylaxis, such as hypotension and bronchoconstriction. Although histamine elicits these life-threatening responses, it is believed that this is possibly mediated by another histamine receptor and therefore is not addressed through H1 blockade.
Antihistamines are not typically useful for life-threatening anaphylactic reactions, which are managed acutely with an injection of epinephrine. Antihistamines typically do not work quickly enough to be useful in these situations, but they also fail to address many of the most important characteristics of anaphylaxis, such as hypotension and bronchoconstriction. Although histamine elicits these life-threatening responses, it is believed that this is possibly mediated by another histamine receptor and therefore is not addressed through H1 blockade. The use of cough and cold preparations in children, particularly combination products, has come under close scrutiny because of concerns over deaths attributed to overdose. The use of multiple combination products facilitates overdose, as parents can be easily confused by the duplication of ingredients among products. In addition, the lack of clear evidence of efficacy of these products in young children has prompted many to question why they are used at all.
The use of cough and cold preparations in children, particularly combination products, has come under close scrutiny because of concerns over deaths attributed to overdose. The use of multiple combination products facilitates overdose, as parents can be easily confused by the duplication of ingredients among products. In addition, the lack of clear evidence of efficacy of these products in young children has prompted many to question why they are used at all.Advanced
 There are also H3 receptors, associated with the nervous system, and H4 receptors, associated with leukocytes, that are current targets of drug development for unrelated indications.
There are also H3 receptors, associated with the nervous system, and H4 receptors, associated with leukocytes, that are current targets of drug development for unrelated indications. The antiinflammatory effects of antihistamines are currently being studied for their potential role in treating asthma. Studies to date have shown mixed success with antihistamines in asthma.
The antiinflammatory effects of antihistamines are currently being studied for their potential role in treating asthma. Studies to date have shown mixed success with antihistamines in asthma.Evidence
For the Common Cold
 A 2003 Cochrane review (32 trials, N = 8930 participants) assessed the effects of antihistamines in reducing nasal symptoms in patients with common cold. First-generation antihistamines were found to have a small effect on rhinorrhea and sneezing, but this was not considered to be clinically significant. First-generation agents also were associated with the side effect of sedation. Combinations of antihistamines and decongestants were not found to be effective in young children.
A 2003 Cochrane review (32 trials, N = 8930 participants) assessed the effects of antihistamines in reducing nasal symptoms in patients with common cold. First-generation antihistamines were found to have a small effect on rhinorrhea and sneezing, but this was not considered to be clinically significant. First-generation agents also were associated with the side effect of sedation. Combinations of antihistamines and decongestants were not found to be effective in young children.FYI Notes
 Many of the first-generation antihistamines, particularly dimenhydrinate, are used off-label as sleep aids owing to their propensity for inducing sedation.
Many of the first-generation antihistamines, particularly dimenhydrinate, are used off-label as sleep aids owing to their propensity for inducing sedation. The efficacy and safety of second-generation antihistamines has been more thoroughly studied compared with first-generation agents.
The efficacy and safety of second-generation antihistamines has been more thoroughly studied compared with first-generation agents. Doxepin, which is classed as a tricyclic antidepressant, also possesses significant antihistamine activity. It is actually much more potent than most marketed antihistamines.
Doxepin, which is classed as a tricyclic antidepressant, also possesses significant antihistamine activity. It is actually much more potent than most marketed antihistamines.Mast Cell Stabilizers
Moa (Mechanism of Action)
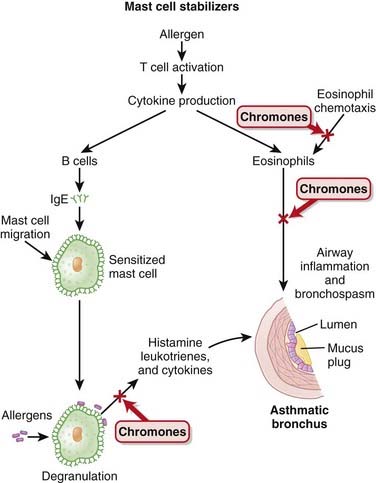
 The degranulation of mast cells and eosinophils is an important step in the response to an allergen. Degranulation leads to release of a variety of proinflammatory factors, including histamine, leukotrienes, and various cytokines. These factors then act on tissues to elicit the classic signs of an allergic reaction.
The degranulation of mast cells and eosinophils is an important step in the response to an allergen. Degranulation leads to release of a variety of proinflammatory factors, including histamine, leukotrienes, and various cytokines. These factors then act on tissues to elicit the classic signs of an allergic reaction. Mast cell stabilizers work by preventing this degranulation from occurring. The mechanism by which they accomplish this is still not confirmed.
Mast cell stabilizers work by preventing this degranulation from occurring. The mechanism by which they accomplish this is still not confirmed.Evidence
Sodium Cromoglycate versus Placebo in Pediatric Asthma
 A 2008 Cochrane review (23 trials, N = 1026 participants) examined the efficacy of sodium cromoglycate versus placebo in prophylactic treatment of pediatric asthma. Most of the studies had small sample sizes, and most were crossover studies, thus limiting confidence in the results. The authors concluded that there is insufficient evidence to be certain about the beneficial effects of sodium cromoglycate for this indication and in this population.
A 2008 Cochrane review (23 trials, N = 1026 participants) examined the efficacy of sodium cromoglycate versus placebo in prophylactic treatment of pediatric asthma. Most of the studies had small sample sizes, and most were crossover studies, thus limiting confidence in the results. The authors concluded that there is insufficient evidence to be certain about the beneficial effects of sodium cromoglycate for this indication and in this population.Sodium Cromoglycate versus Inhaled Corticosteroids in Chronic Asthma
 A 2006 Cochrane review (17 trials, N = 1279 children; eight trials, N = 321 adults) compared inhaled corticosteroids with sodium cromoglycate in adults and children with chronic asthma. In children and adults, sodium cromoglycate was inferior to inhaled corticosteroids with respect to use of rescue bronchodilators and improved performance on pulmonary function tests. Sodium cromoglycate was also inferior with respect to improvement of symptoms, although in adults these improvements were significant only in crossover trials and not in those of parallel design. There were no differences in adverse effects between inhaled corticosteroids and sodium cromoglycate in either children or adults.
A 2006 Cochrane review (17 trials, N = 1279 children; eight trials, N = 321 adults) compared inhaled corticosteroids with sodium cromoglycate in adults and children with chronic asthma. In children and adults, sodium cromoglycate was inferior to inhaled corticosteroids with respect to use of rescue bronchodilators and improved performance on pulmonary function tests. Sodium cromoglycate was also inferior with respect to improvement of symptoms, although in adults these improvements were significant only in crossover trials and not in those of parallel design. There were no differences in adverse effects between inhaled corticosteroids and sodium cromoglycate in either children or adults.