Xanthomas
Lucile E. White, Marcelo G. Horenstein and Christopher R. Shea
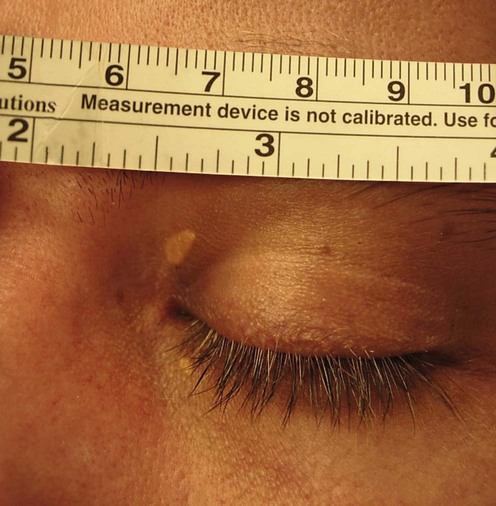
(Courtesy of Arlene Ruiz de Luzuriaga, MD, MPH)
First-line therapies
Second-line therapies
Lucile E. White, Marcelo G. Horenstein and Christopher R. Shea
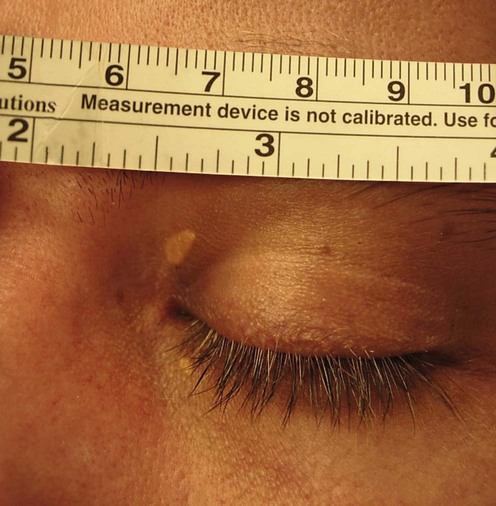
(Courtesy of Arlene Ruiz de Luzuriaga, MD, MPH)
