Chapter 5 Wrist and Hand Ultrasound
![]() Additional videos for this topic are available online at www.expertconsult.com.
Additional videos for this topic are available online at www.expertconsult.com.
Wrist and Hand Anatomy
The wrist consists of several synovial articulations between the distal radius, the distal ulna, the proximal carpal row (scaphoid, lunate, triquetrum, pisiform), and the distal carpal row (trapezium, trapezoid, capitate, and hamate). The radiocarpal joint between the distal radius and the proximal carpal row and the distal radioulnar joint between the radius and the ulna are separated by fibrocartilage, called the triangular fibrocartilage, which extends from the ulnar aspect of the distal radius to the base of the ulnar styloid. The midcarpal joint is located between the carpal bones and is separated from the radiocarpal joint by two intrinsic ligaments, the scapholunate and lunotriquetral ligaments. The scapholunate ligament is U shaped in the sagittal plane, with the open end of the U distal, and it consists of a volar portion, a thin proximal or central portion, and a thick and mechanically important dorsal portion.1
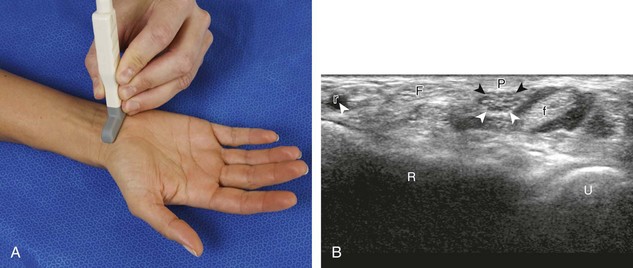
Structures enter the wrist through several fibro-osseous tunnels. In the volar wrist, the carpal tunnel contains the median nerve and the flexor digitorum profundus, flexor digitorum superficialis, and flexor pollicis longus tendons (Fig. 5-1A-E). The fibrous flexor retinaculum extends from the pisiform and hamate to the scaphoid and trapezium, to form the roof of the carpal tunnel. The Guyon or ulnar canal is also volar adjacent to the pisiform, which contains the ulnar nerve and ulnar artery and veins. Other tendons, the flexor carpi radialis and the palmaris longus tendons, are located outside the carpal tunnel, although the flexor carpi radialis is within its own fibro-osseous canal and distally is associated with the trapezium.
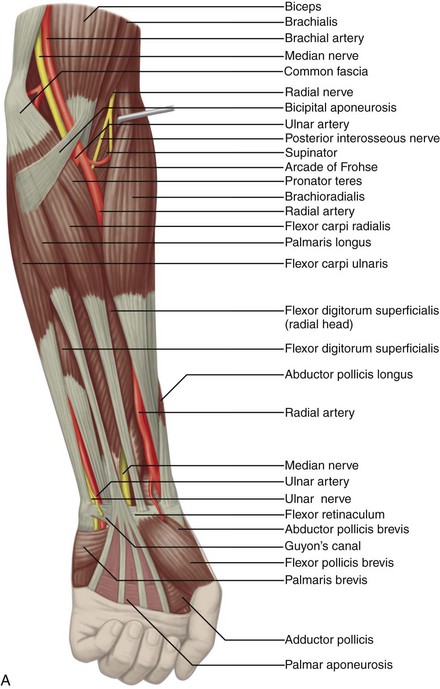

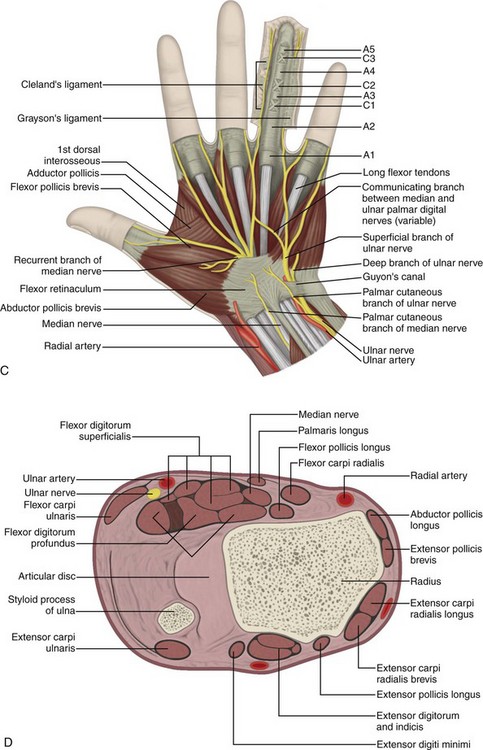
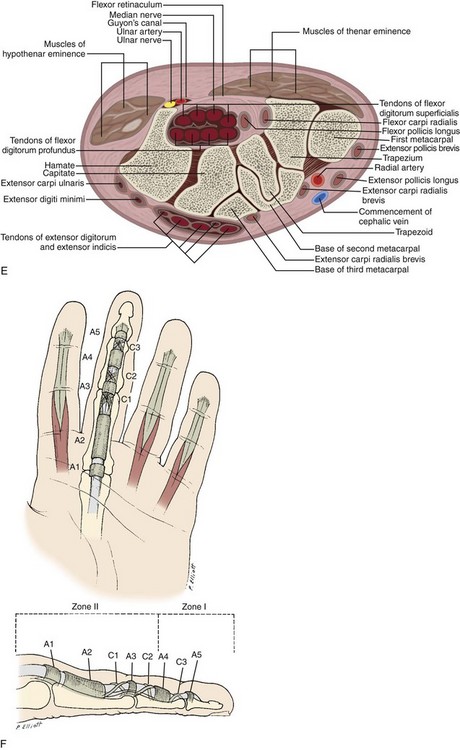
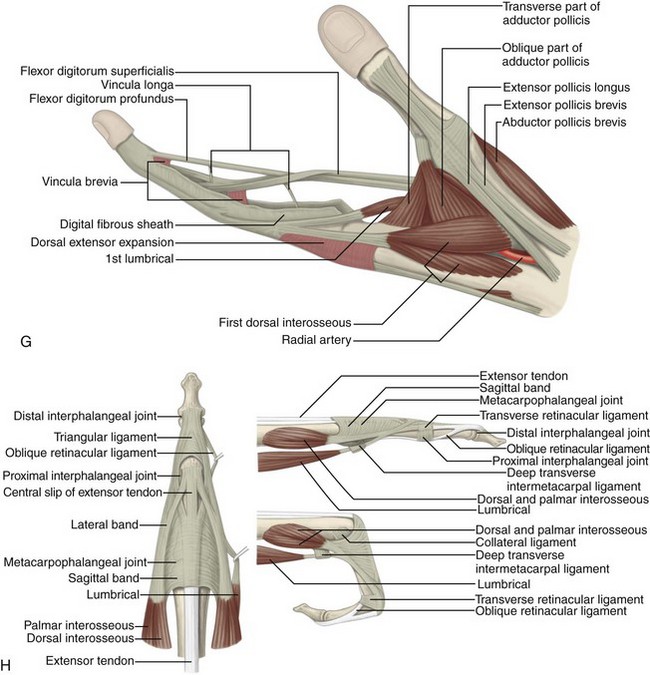
FIGURE 5-1 Forearm, wrist, and hand anatomy.
(From Standring S: Gray’s anatomy: the anatomical basis of clinical practice, ed 39, Edinburgh, 2005, Churchill Livingstone.)
The tendons of the dorsal wrist are also separated into six fibro-osseous compartments (see Fig. 5-1C). From radial to ulnar, they include the (1) abductor pollicis longus and extensor pollicis brevis, (2) extensor carpi radialis longus and brevis, (3) extensor pollicis longus, (4) extensor digitorum and extensor indicis, (5) extensor digiti minimi, and (6) extensor carpi ulnaris. A helpful bone landmark for orientation is the dorsal tubercle of the radius or Lister tubercle, which is located between the extensor carpi radialis tendons in the second compartment and the extensor pollicis longus tendon in the third compartment. The extensor carpi ulnaris is also found within a characteristic groove in the ulna.
The anatomy of the volar aspect of the fingers includes the flexor digitorum superficialis and profundus tendons. Each flexor superficialis tendon splits at the proximal interphalangeal joint, with each limb coursing to each side of the flexor digitorum profundus tendon to insert on the middle phalanx (see Fig. 5-1F-H). The flexor digitorum profundus terminates at the distal phalanx. The flexor tendons are tethered or secured to the adjacent phalanges through a series of fibrous pulleys to prevent bowstringing of the tendons with flexion (see Fig. 5-1F). The annular pulleys consist of the A1 pulley located at the metacarpophalangeal joint, the longer A2 pulley at the level of the proximal phalanx, the A3 pulley at the proximal interphalangeal joint, the A4 pulley at the level of the middle phalanx, and the A5 pulley at the distal interphalangeal joint.2 Smaller cruciform pulleys are located between these pulleys along the course of the flexor tendons. At the volar aspect of each metacarpophalangeal and interphalangeal joint is a fibrous structure called the volar or palmar plate.
At the dorsal aspect of each finger, the extensor digitorum tendon attaches to the middle phalanx as a central band, whereas slips of the extensor tendon that contribute to the lateral bands attach to the distal phalanx. The metacarpophalangeal joints have an overlying aponeurotic sheet or extensor hood, which consists of transverse-oriented sagittal bands that stabilize the extensor tendons.3 The metacarpophalangeal and interphalangeal joints are synovial articulations with prominent dorsal joint recesses. Each joint is stabilized with ulnar and radial collateral ligaments. The soft tissue distally at the volar aspect of distal phalanx is called the pulp.
Ultrasound Examination Technique
Tables 5-1 and 5-2 are ultrasound examination checklists. Examples of diagnostic wrist and hand ultrasound reports are available online at www.expertconsult.com (see eBox 5-1 and 5-2).
| Location | Structures of Interest/Pathologic Features |
|---|---|
| Volar (no. 1) |
TABLE 5-2 Finger Ultrasound Examination Checklist
| Location | Structures of Interest |
|---|---|
| Volar | |
| Dorsal | |
| Other |
eBox 5-1 Sample Diagnostic Wrist Ultrasound Report
Normal
Examination: Ultrasound of the Wrist
History: Numbness, evaluate for carpal tunnel syndrome
Findings: The median nerve is unremarkable in appearance, measuring 8 mm2 at the wrist crease and 7 mm2 at the pronator quadratus. No evidence of tenosynovitis. The radiocarpal, midcarpal, and distal radioulnar joints are normal without effusion or synovial hypertrophy. The wrist tendons are normal without tear or tenosynovitis. Normal dorsal component of the scapholunate ligament. No dorsal or volar ganglion cyst. Unremarkable Guyon canal. Additional focused evaluation at site of maximal symptoms was unrevealing.
Impression: Unremarkable ultrasound examination of the wrist.
eBox 5-2 Sample Diagnostic Wrist Ultrasound Report
abnormal
Examination: Ultrasound of the Wrist
History: Numbness, evaluate for carpal tunnel syndrome
Findings: The median nerve is hypoechoic and enlarged, measuring 15 mm2 at the wrist crease and 7 mm2 at the pronator quadratus. No evidence for tenosynovitis. The radiocarpal, midcarpal, and distal radioulnar joints are normal without effusion or synovial hypertrophy. The wrist tendons are normal without tear or tenosynovitis. Normal dorsal component of the scapholunate ligament. No dorsal ganglion cyst. A 7-mm volar ganglion cyst is noted between the radial artery and flexor carpi radialis tendon. Unremarkable Guyon canal. Additional focused evaluation at site of maximal symptoms was unrevealing.
Wrist: Volar Evaluation
Median Nerve, Flexor Digitorum Tendons, and Volar Joint Recesses
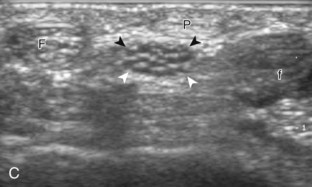
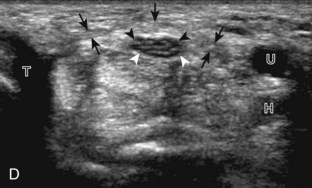
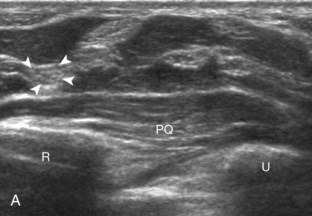
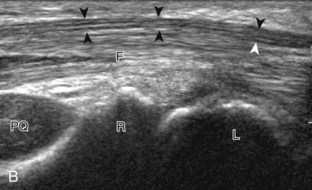
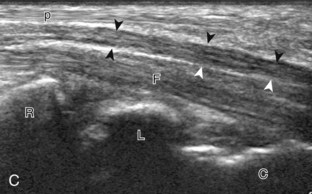
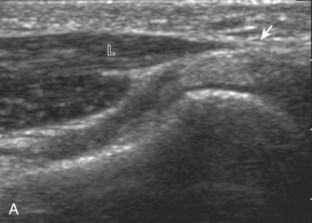
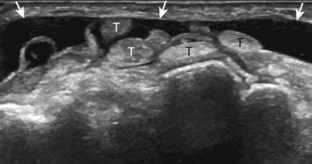
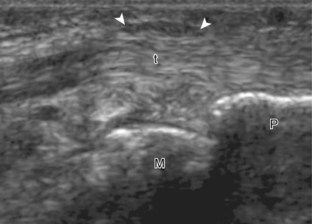
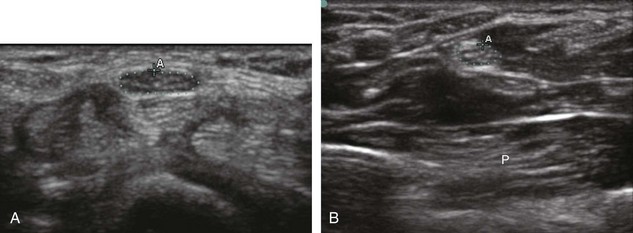
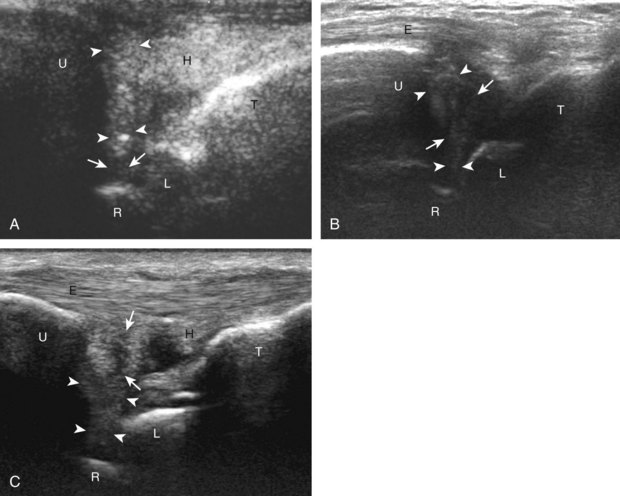
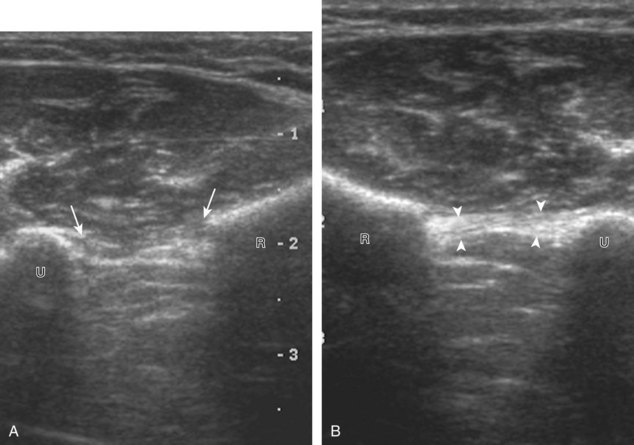
The primary structures evaluated from the volar aspect at midline are the median nerve, the flexor tendons, and the volar aspects of the wrist joints. Examination begins short axis to the tendons and median nerve because this allows proper orientation and accurate identification of the structures. For evaluation of the median nerve, the transducer is placed in the transverse plane at the level of the wrist crease, which is at the proximal aspect of the carpal tunnel (Fig. 5-2). Normal peripheral nerves have a honeycomb appearance when they are imaged in short axis from hypoechoic nerve fascicles and surrounding hyperechoic connective tissue (see Fig. 5-2B).4 Toggling the transducer to angle the sound beam along the long axis of the median nerve will help to show the characteristic appearance of the nerve when the sound beam is perpendicular (Video 5-1)![]() . Because peripheral nerve trunks are composed of both hypoechoic and hyperechoic elements, the median nerve appears relatively hypoechoic when surrounded by hyperechoic tissue (e.g., in the carpal tunnel) and relatively hyperechoic when surrounded by hypoechoic muscle (e.g., in the forearm). At the wrist crease, the round or oval median nerve is identified by its hypoechoic nerve fascicles, which are most conspicuous surrounded by the adjacent hyperechoic tendons (see Fig. 5-2C). If differentiation between the median nerve and adjacent tendons is difficult, median nerve identification is easily accomplished with movement of the transducer proximally in the transverse plane. During this maneuver, the normal median nerve courses radial to the flexor tendons and then moves ulnar and deep between the flexor digitorum superficialis and profundus (Fig. 5-3) (Video 5-2)
. Because peripheral nerve trunks are composed of both hypoechoic and hyperechoic elements, the median nerve appears relatively hypoechoic when surrounded by hyperechoic tissue (e.g., in the carpal tunnel) and relatively hyperechoic when surrounded by hypoechoic muscle (e.g., in the forearm). At the wrist crease, the round or oval median nerve is identified by its hypoechoic nerve fascicles, which are most conspicuous surrounded by the adjacent hyperechoic tendons (see Fig. 5-2C). If differentiation between the median nerve and adjacent tendons is difficult, median nerve identification is easily accomplished with movement of the transducer proximally in the transverse plane. During this maneuver, the normal median nerve courses radial to the flexor tendons and then moves ulnar and deep between the flexor digitorum superficialis and profundus (Fig. 5-3) (Video 5-2)![]() .4 In addition, the median nerve now appears relatively hyperechoic as a result of the connective tissue and fat because it is surrounded by hypoechoic muscle. The characteristic course, location, and echogenicity assist in identification of the median nerve. An additional method to differentiate the median nerve from the adjacent flexor tendons at the wrist crease in the transverse plane is angulation of or toggling the transducer along the long axis of the tendons. This maneuver causes the hyperechoic tendons to become hypoechoic as a result of anisotropy, whereas the hypoechoic median nerve fascicles remain unchanged (see Video 5-1). Evaluation of the median nerve is then continued distally into the carpal tunnel, where the thin and hyperechoic flexor retinaculum can be visualized (see Fig. 5-2D). A small branch of the median nerve, the palmar cutaneous branch, originates proximal to the carpal tunnel and courses superficial to the flexor retinaculum and ulnar to flexor carpi radialis tendon (see Fig. 5-2E).5 The transducer is turned 90 degrees to visualize the median nerve in long axis (Fig. 5-4) (Video 5-3)
.4 In addition, the median nerve now appears relatively hyperechoic as a result of the connective tissue and fat because it is surrounded by hypoechoic muscle. The characteristic course, location, and echogenicity assist in identification of the median nerve. An additional method to differentiate the median nerve from the adjacent flexor tendons at the wrist crease in the transverse plane is angulation of or toggling the transducer along the long axis of the tendons. This maneuver causes the hyperechoic tendons to become hypoechoic as a result of anisotropy, whereas the hypoechoic median nerve fascicles remain unchanged (see Video 5-1). Evaluation of the median nerve is then continued distally into the carpal tunnel, where the thin and hyperechoic flexor retinaculum can be visualized (see Fig. 5-2D). A small branch of the median nerve, the palmar cutaneous branch, originates proximal to the carpal tunnel and courses superficial to the flexor retinaculum and ulnar to flexor carpi radialis tendon (see Fig. 5-2E).5 The transducer is turned 90 degrees to visualize the median nerve in long axis (Fig. 5-4) (Video 5-3)![]() . The variable appearance of peripheral nerve echogenicity relative to the surrounding tissue echogenicity is well demonstrated when imaging the median nerve in long axis in the distal forearm (see Fig. 5-4D). Proximal to the wrist joint in the transverse plane, the pronator quadratus can be identified extending between the distal radius and ulna (see Fig. 5-3A).
. The variable appearance of peripheral nerve echogenicity relative to the surrounding tissue echogenicity is well demonstrated when imaging the median nerve in long axis in the distal forearm (see Fig. 5-4D). Proximal to the wrist joint in the transverse plane, the pronator quadratus can be identified extending between the distal radius and ulna (see Fig. 5-3A).
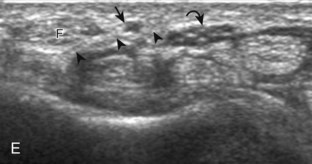
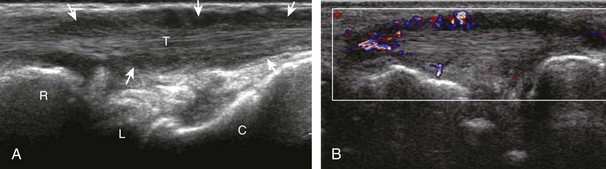
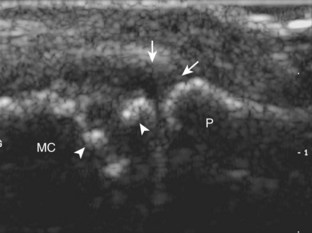
Attention is then turned back to the flexor tendons, with each tendon evaluated in both short axis and long axis. The flexor digitorum superficialis and profundus are identified around the median nerve as described earlier, proximally as hypoechoic muscle and distally as fibrillar and hyperechoic tendons (see Figs. 5-2 and 5-3). Just beyond the wrist crease, the thin hyperechoic flexor retinaculum is seen as it extends from the proximal scaphoid pole to the pisiform and from the trapezium to the hook of the hamate, which represents the roof the carpal tunnel (see Fig. 5-2D). If the retinaculum is not imaged perpendicular to the ultrasound beam, it will appear hypoechoic as a result of anisotropy. The flexor digitorum tendons travel through the carpal tunnel to the digits, whereas the palmaris longus tendon, typically directly superficial to the median nerve, remains outside of the carpal tunnel. In the sagittal plane and long axis to the flexor tendons, the volar radiocarpal and midcarpal joint recesses are identified by the adjacent bone contours; the volar lip of the distal radius, the lunate bone, and the capitate bone have characteristic shapes (see Fig. 5-4B and C). Between the distal radius and the lunate is the volar recess of the radiocarpal joint, and between the lunate and capitate bones is the volar recess of the midcarpal joint. The distal radioulnar joint is identified with placement of the transducer in the transverse plane between the distal radius and ulna. This joint and the volar recesses are evaluated for anechoic fluid or variable-echogenicity synovial hypertrophy and other joint disorders.
Scaphoid, Flexor Carpi Radialis Tendon, Radial Artery, and Volar Ganglion Cysts
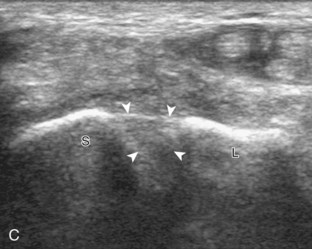
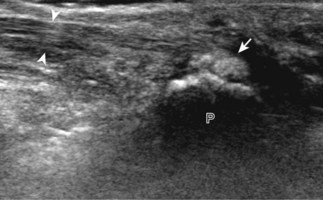
Evaluation of the radial aspect of the volar wrist begins in the transverse plane at the wrist crease. In this position, the various tendons of the volar wrist are identified. Just radial to the median nerve and somewhat similar in size is the flexor carpi radialis tendon, located outside the carpal tunnel in its own fibro-osseous canal (see Fig. 5-2B). Ultrasound evaluation is completed in both long and short axis from proximal to the distal insertion of the flexor carpi radialis tendon on the second and third metacarpals, although some fibers insert onto the trapezium tuberosity.6 With placement of the transducer over the distal aspect of the flexor carpi radialis tendon in long axis (Fig. 5-5), the characteristic bilobed or peanut-shaped bone contours of the scaphoid bone are identified deep to this tendon (see Fig. 5-5C). The normal smooth and hyperechoic bone surface of the scaphoid bone is evaluated for cortical step-off fracture. Returning to the wrist crease in the transverse plane (Fig. 5-6A), the radial artery and veins are identified immediately radial to the flexor carpi radialis tendon (see Fig. 5-6B). With the flexor carpi radialis tendon and radial artery in view, the transducer is moved both proximally and distally from the radiocarpal joint to evaluate for ganglion cysts. Placement of the transducer in the transverse plane between the scaphoid and lunate will show the normal hyperechoic and fibrillar volar component of the scapholunate ligament (see Fig. 5-6C).
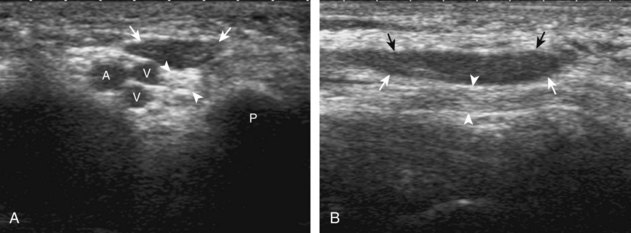
Ulnar Artery, Vein, and Nerve (Guyon Canal)
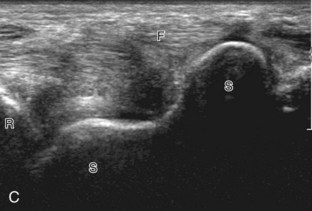
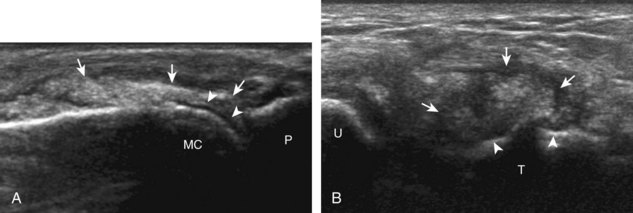
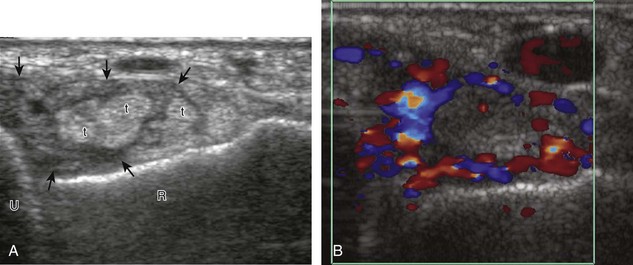
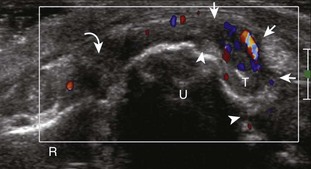
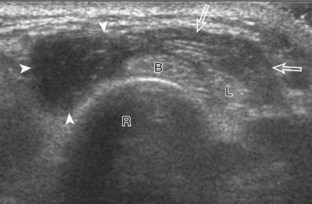
Evaluation of the ulnar aspect of the volar wrist begins in the transverse plane at the wrist crease (see Fig. 5-2A). Moving the transducer ulnar to the carpal tunnel (Fig. 5-7A), the bone landmark of the pisiform is identified (see Fig. 5-7B). Between the pisiform and the ulnar artery, the ulnar nerve is identified as hypoechoic nerve fascicles and surrounding hyperechoic connective tissue. The ulnar veins are usually not visible because they are easily compressed by pressure of the ultrasound transducer. As the transducer is moved distally, the hyperechoic and shadowing surface of the hook of the hamate is seen deep to the ulnar nerve and artery. The ulnar nerve branches, with a deep motor branch coursing along the ulnar side of the hamate hook and one to two predominantly sensory branches superficial to the hamate hook (see Fig. 5-7C). It is important to evaluate this area because ulnar nerve and artery abnormalities occur in this location as a result of compression by the adjacent hook of the hamate during trauma. Evaluation of the ulnar artery and nerve is also completed in long axis (Fig. 5-8). Another ulnar-sided tendon, the flexor carpi ulnaris, can also be identified by scanning proximal to the pisiform bone.
Wrist: Dorsal Evaluation
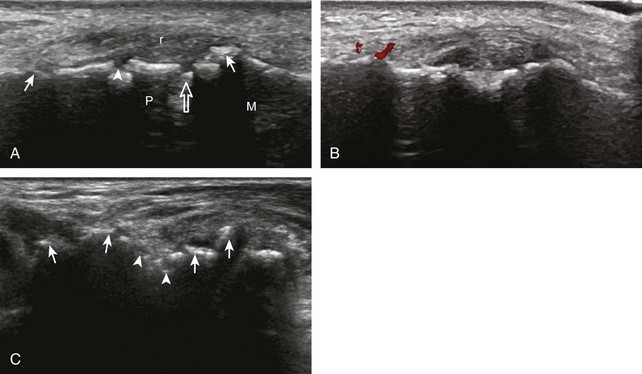
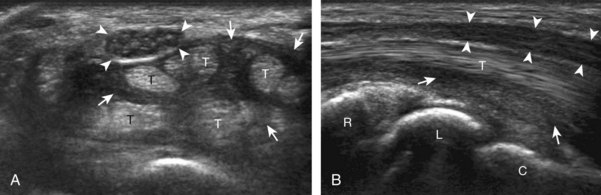
Dorsal Wrist Tendons and Dorsal Joint Recesses
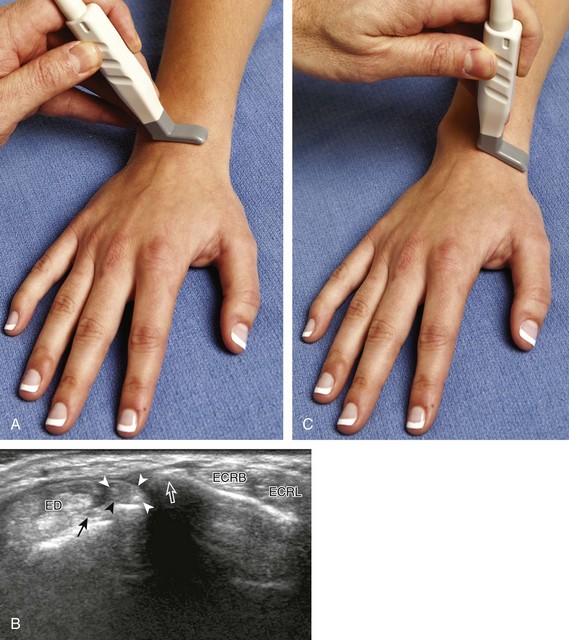
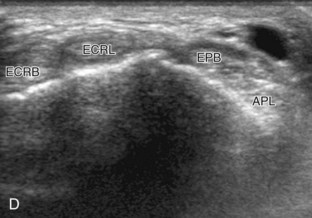
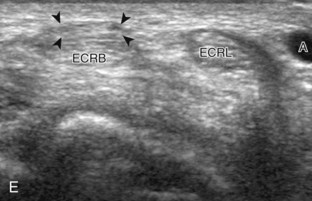
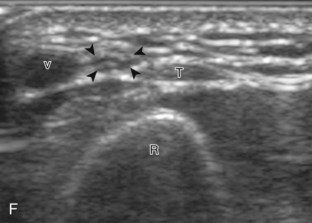
The primary structures of the dorsal wrist are the various extensor and abductor tendons of the six wrist compartments and the dorsal radiocarpal, midcarpal, and distal radioulnar joint recesses. Evaluation of the dorsal tendons begins in the transverse plane over the Lister tubercle of the dorsal radius (Fig. 5-9A and B). This structure serves as an important starting point for dorsal wrist evaluation and assists in accurate identification of the wrist tendons. The Lister tubercle is seen as a pronounced bony prominence. If one has difficulty finding this structure with ultrasound, it can easily be palpated at physical examination. Once the Lister tubercle is identified, the tendon immediately ulnar to it is the extensor pollicis longus of the third wrist compartment (see Fig. 5-9B). Often there is an additional smaller dorsal radial protuberance at the ulnar aspect of the extensor pollicis longus as well. With movement of the transducer in the radial direction (see Fig. 5-9C), the extensor carpi radialis brevis and then the extensor carpi radialis longus tendons are seen in the second wrist compartment (Fig. 5-9D). On further radial movement of the transducer, the extensor pollicis brevis and abductor pollicis longus tendons are seen in the first wrist compartment (see Fig. 5-9D). It may be helpful to remember that the names of the tendons alternate from longus to brevis, beginning at the extensor pollicis longus and moving in a radial direction. The extensor pollicis longus tendon courses toward the first digit superficial to the extensor carpi radialis and ulnaris tendons in an oblique fashion proximally to distally. Therefore, when short axis to the extensor carpi radialis brevis and longus tendons and moving distally, the extensor pollicis longus is seen moving in an ulnar to radial direction over the extensor carpi radialis brevis and longus tendons (see Fig. 5-9E) (Video 5-4)![]() . In the region of the first extensor wrist compartment, the superficial branch of the radial nerve can be seen as it courses from the volar to the dorsal aspect of the distal forearm superficial to the first extensor wrist compartment tendons and extensor retinaculum, near branches of the cephalic vein (see Fig. 5-9F).
. In the region of the first extensor wrist compartment, the superficial branch of the radial nerve can be seen as it courses from the volar to the dorsal aspect of the distal forearm superficial to the first extensor wrist compartment tendons and extensor retinaculum, near branches of the cephalic vein (see Fig. 5-9F).
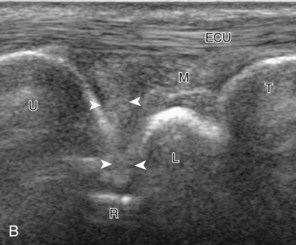
Beginning again in the transverse plane at the Lister tubercle, transducer movement ulnar from the extensor pollicis longus tendon (Fig. 5-10A) shows the extensor indicis and multiple tendons of the extensor digitorum in the fourth wrist compartment, and the extensor digiti minimi in the fifth wrist compartment near the distal radioulnar joint (see Fig. 5-10B). The posterior interosseous nerve is identified deep within the radial aspect of the fourth dorsal extensor compartment (see Fig. 5-9B).7 Finally, over the most ulnar aspect of the ulna, the extensor carpi ulnar tendon is identified in a concave groove of the ulna in the sixth wrist compartment (see Fig. 5-10C). The extensor carpi ulnaris tendon often has a thin hypoechoic longitudinal cleft that should not be interpreted as a tendon tear. In addition, up to 50% of the extensor carpi ulnar tendon can be located outside of the groove and still be considered within normal.8

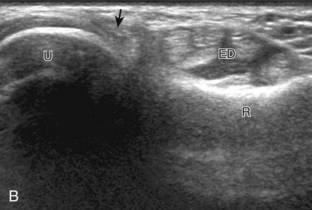
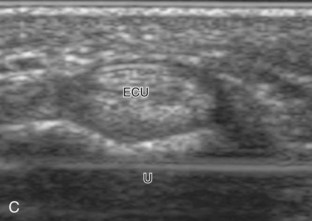
FIGURE 5-10 Dorsal wrist evaluation (extensor compartments 4 to 6).
A, Transverse imaging ulnar to that shown in Figure 5-9A shows (B) the extensor digitorum and extensor indicis (ED), the extensor digiti minimi (arrow), and the distal radioulnar joint between the radius (R) and ulna (U). Transverse imaging over the lateral ulna shows (C) the extensor carpi ulnaris (ECU).
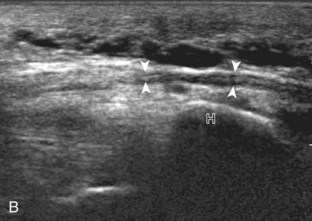
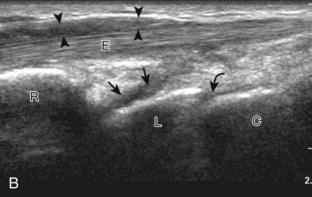
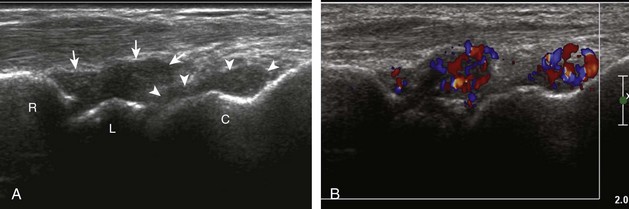
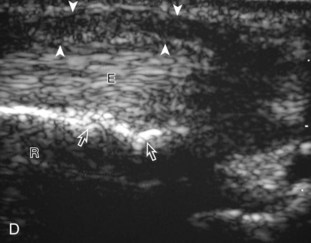
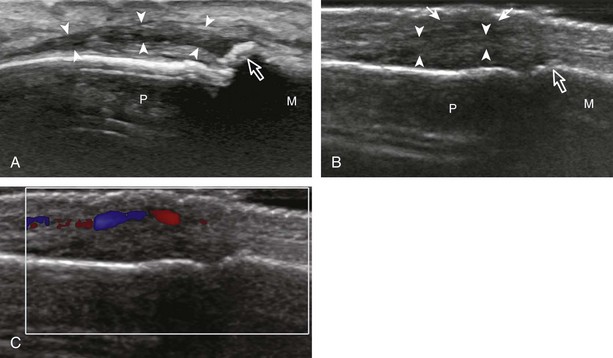
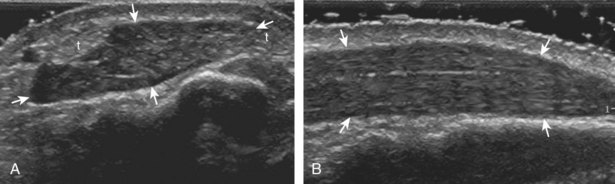
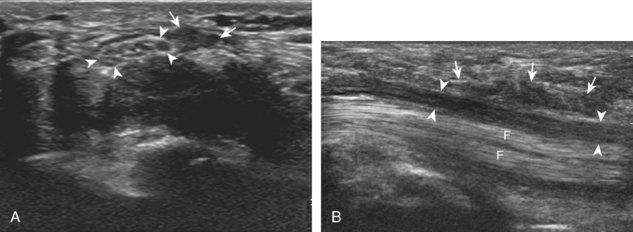
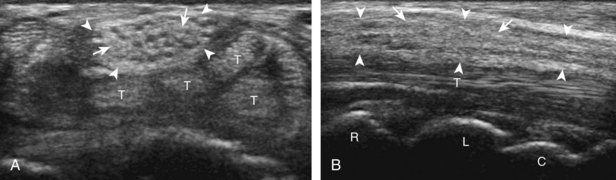
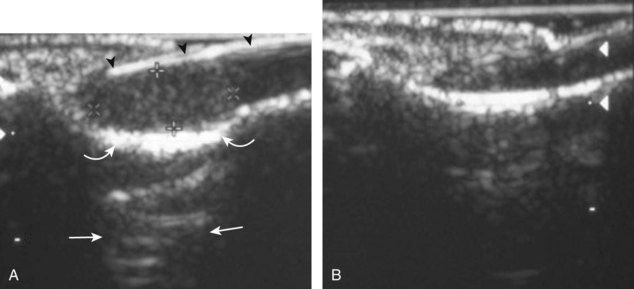
Each of the extensor tendons is also imaged in long axis throughout the wrist (Fig. 5-11). The extensor retinaculum courses transversely but slightly obliquely over the extensor tendons and appears hyperechoic, measuring up to 1.7 mm thick and 23 mm wide in cross section (see Fig. 5-11B).9 If imaged oblique to the ultrasound beam, the extensor retinaculum can appear artifactually hypoechoic as a result of anisotropy, which should not be misinterpreted as tenosynovitis. Similar to the volar wrist, the dorsal recesses of the radiocarpal joint (between the radius and proximal carpal row), the midcarpal joint, and the distal radioulnar joint are identified with recognition of the characteristic bone contours for orientation. The radiocarpal and midcarpal joint recesses are optimally evaluated in the sagittal plane, whereas the distal radioulnar joint is evaluated in the transverse plane (see Fig. 5-10B).
Scapholunate Ligament (Dorsal Component) and Dorsal Ganglion Cysts
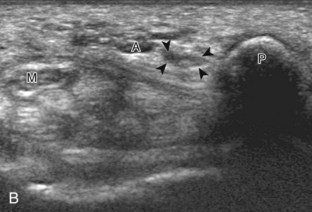
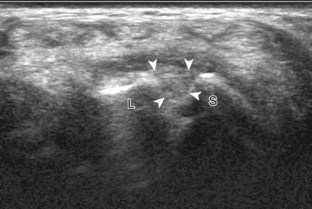
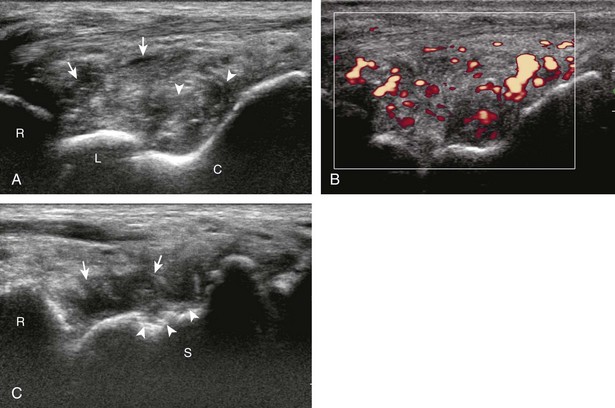
Similar to the dorsal tendons, evaluation of the scapholunate ligament begins in the transverse plane over the Lister tubercle (see Fig. 5-9A). The transducer is then moved distally. The bone contours of the radius are interrupted by the radiocarpal joint, so the next osseous structure in view is the scaphoid bone. With movement of the transducer in the ulnar direction, the adjacent lunate bone is brought into view. Between the dorsal aspects of the scaphoid and the lunate is a triangular area where one sees the dorsal aspect of the scapholunate ligament, which has a compact hyperechoic fibrillar echotexture (Fig. 5-12).10 Directly superficial to the dorsal aspect of the scapholunate ligament, the dorsal radiocarpal ligament (or dorsal radiotriquetral ligament) is identified.11,12 This area is also a common site for dorsal wrist ganglion cysts.
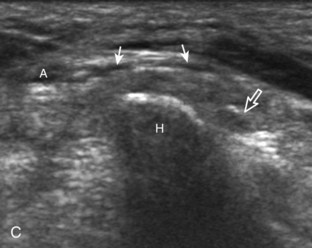
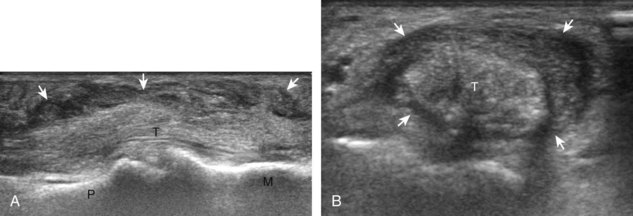
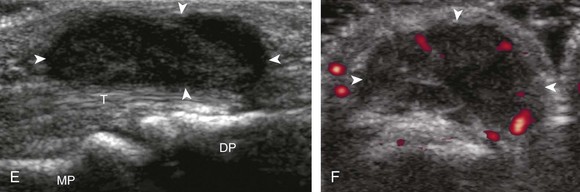
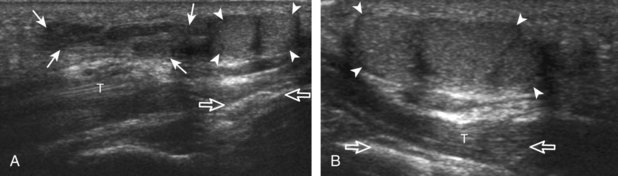
Triangular Fibrocartilage Complex
The triangular fibrocartilage complex consists of the triangular fibrocartilage, the meniscus homologue, the extensor carpi ulnaris tendon sheath, and the volar and dorsal radiocarpal ligaments. For evaluation of the triangular fibrocartilage, the transducer is placed in the sagittal plane over the dorsal lateral wrist to identify the bone contours of the distal ulna and then moved toward the coronal plane with the wrist in slight radial deviation (Fig. 5-13A). A hyperechoic slab of tissue is identified as it extends from the ulnar styloid base to the radius, which represents the triangular fibrocartilage (see Fig. 5-13B).11 It is important to ensure complete evaluation of the triangular fibrocartilage to the radial attachment because this may be a site of traumatic tears. Evaluation of the triangular fibrocartilage can be difficult given its orientation in the transverse plane extending away from the transducer, and often a lower frequency is helpful. The meniscus homologue is seen as a hyperechoic triangular structure with its base adjacent to the extensor carpi ulnar tendon and in contact with the triquetrum, and this should not be mistaken for the triangular fibrocartilage, which is thinner and directly over the ulnar head.
Finger Evaluation
Volar
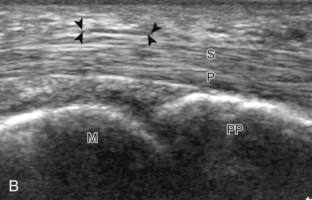
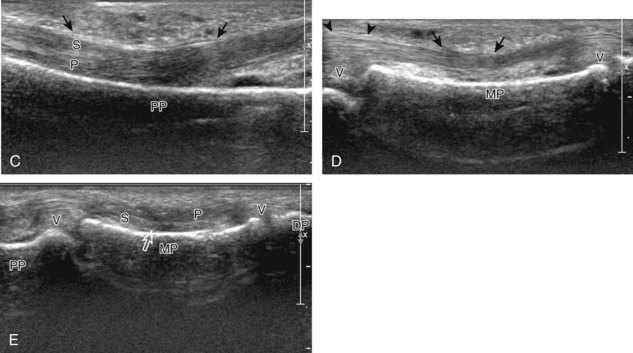
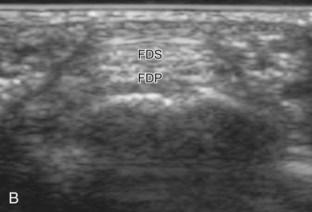
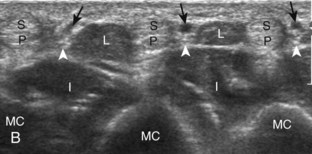
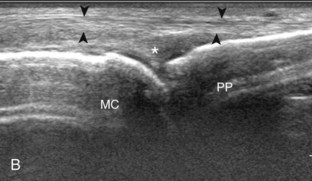
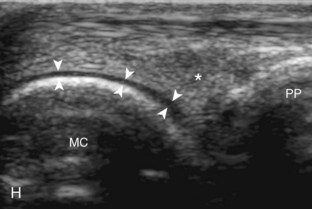
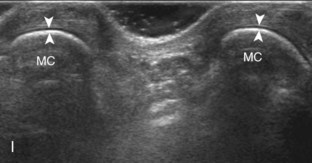
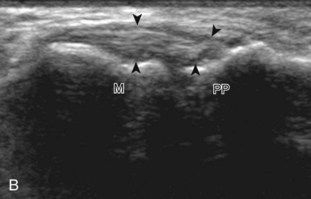
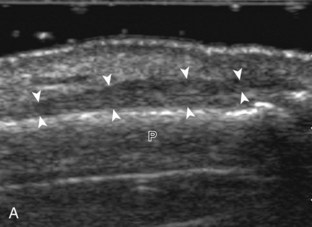
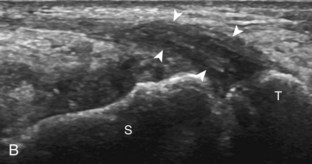
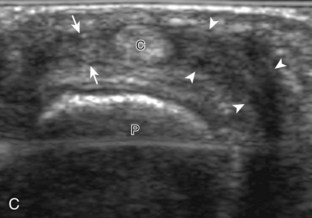
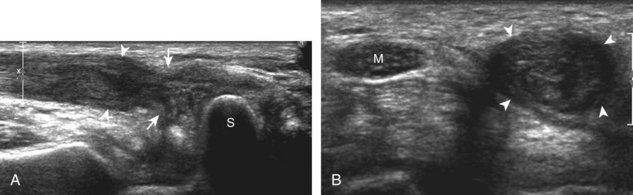
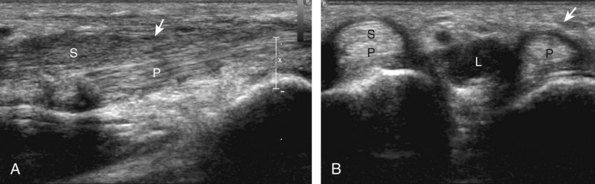
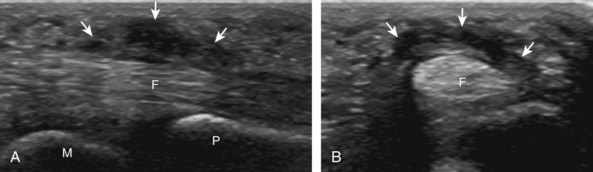
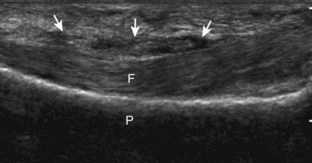
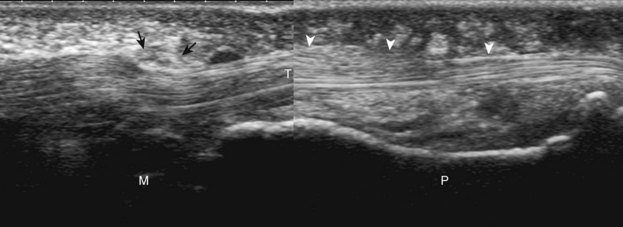
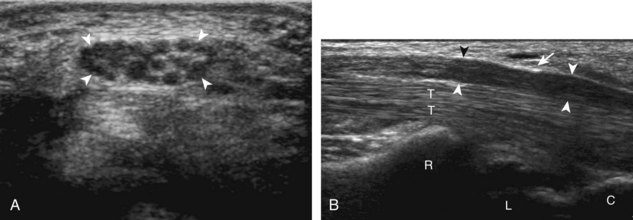
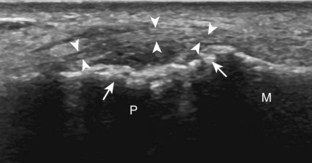
At the volar aspect of the finger in long axis (Fig. 5-14A), both the hyperechoic and fibrillar flexor digitorum superficialis and profundus tendons can be seen at the level of the metacarpophalangeal joint with the overlying A1 pulley (see Fig. 5-14B). The pulleys often have a trilaminar appearance at ultrasound. At close inspection, a pulley itself is fibrous, fibrillar, and therefore hyperechoic when imaged perpendicular to the sound beam; however, a normal pulley often appears hypoechoic relative to the adjacent superficial hyperechoic fat and connective tissue and from anisotropy. The trilaminar appearance consists of the superficial reflective surface of the pulley, the relatively hypoechoic pulley, and the deeper hyper-reflective surface of the adjacent flexor tendon sheath. With regard to imaging the flexor tendons in long axis, the individual tendons can be distinguished from each other with isolated passive movement of the distal phalanx because this will cause movement of the flexor digitorum profundus. At the level of the proximal phalanx, the A2 pulley can be identified; slight obliquity of the transducer may make the pulley appear hypoechoic from anisotropy and can aid in its identification (see Fig. 5-14C). At the level of the proximal interphalangeal joint, the hyperechoic volar plate is identified (see Fig. 5-14D and E). The A3 and A4 pulleys are also identified superficial to the flexor tendons, at the level of the proximal interphalangeal joint and middle phalanx, respectively (see Fig. 5-14D).2 Just distal to the proximal interphalangeal joint, the flexor digitorum superficialis inserts on the middle phalanx, whereas the flexor digitorum profundus extends distally over the volar plate of the distal interphalangeal joint to insert on the distal phalanx (see Fig. 5-14E). The flexor digitorum superficialis inserts on the middle phalanx by dividing into two bundles, with each segment moving around the flexor digitorum profundus tendon. This is best appreciated by imaging in short axis (Fig. 5-15A and B). More proximally over the palm of the hand (Fig. 5-16), the lumbrical and interosseous muscles can be identified, as can the common and proper palmar digital arteries and nerves. The volar metacarpophalangeal and interphalangeal joints are also evaluated in the sagittal plane for volar plate abnormality and joint recess distention from fluid or synovial disorders.
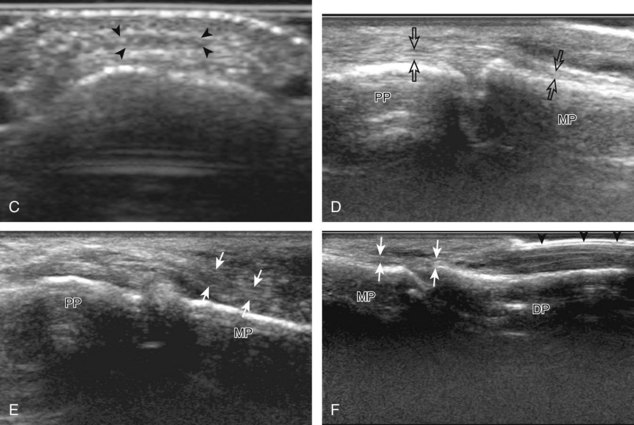
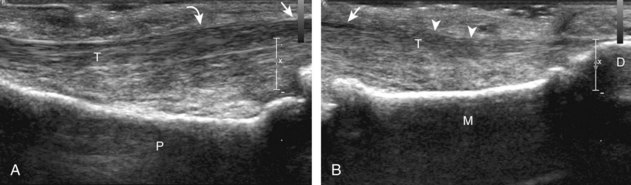
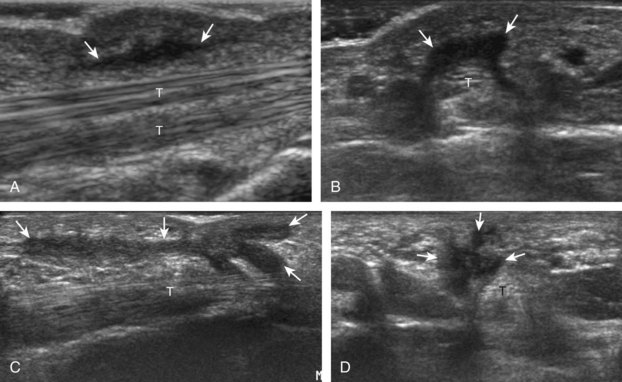
Dorsal
At the dorsal aspect of each digit, the thin, hyperechoic, and fibrillar extensor digitorum tendon extends over the metacarpophalangeal joint in the sagittal plane (Fig. 5-17A and B). At the level of the proximal interphalangeal joint, the central band of the extensor tendon inserts on the middle phalanx (see Fig. 5-17C and D). With movement of the transducer just off midline of the phalanx, the slips of the extensor tendon to the lateral bands can be seen (see Fig. 5-17E), which insert distally on the distal phalanx (see Fig. 5-17F). The ultrasound beam penetrates through the nail and allows visualization of the underlying hypoechoic nail bed, subungual space, and the surface of the distal phalanx (see Fig. 5-17F). At the level of the metacarpophalangeal joint, the transducer is positioned short axis to the extensor tendon, and the finger is flexed to evaluate for subluxation of the tendon, which would indicate extensor hood injury. The joints of each digit are also evaluated for distention from fluid or synovial hypertrophy, where often the dorsal joint recess is pronounced as it extends proximally beneath the extensor tendon. In addition, the hypoechoic hyaline articular cartilage of each joint can be visualized (see Fig. 5-17B), which is accessible with flexion of the digits (see Fig. 5-17G to I). A triangular region of connective tissue is normally found superficial to the metacarpophalangeal joint articulation (see Fig. 5-17H).13
Ligaments
The collateral ligaments of the digits can also be assessed with ultrasound in the coronal plane around each individual joint. To specifically evaluate the ulnar collateral ligament of the first metacarpophalangeal joint, the hand is placed around a rolled up towel, and the transducer is placed in the coronal plane relative to the first metacarpophalangeal joint (Fig. 5-18A). The ulnar collateral ligament will appear in long axis as hyperechoic with a compact fibrillar echotexture, extending from a broad concavity in the metacarpal to the proximal phalanx (see Fig. 5-18B). Because the subcutaneous fat directly overlying the ulnar collateral ligament is quite hyperechoic, the ligament may appear relatively hypoechoic but should be of relatively uniform thickness. Additionally, the ligament may appear artifactually hypoechoic where it is oblique to the sound beam from anisotropy. The overlying adductor pollicis aponeurosis, which is specific to the ulnar collateral ligament of the first metacarpophalangeal joint, is seen as a thin structure over the ulnar collateral ligament. Passive flexion of the interphalangeal joint will produce isolated movement of the adductor pollicis aponeurosis, which assists in its identification (Video 5-5)![]() . An additional dynamic maneuver in assessment of any collateral ligament is stressing the joint (valgus for ulnar ligaments, varus for radial ligaments). This is accomplished with minimal stress and is helpful because joint fluid will often move into the ligament tear under ultrasound visualization. Other ulnar and radial collateral ligaments of the digits similarly appear as compact and hyperechoic fibrillar structures, which extend across each joint. Any suspected ligament tear can be assessed using dynamic imaging with valgus and varus joint angulation under ultrasound visualization.
. An additional dynamic maneuver in assessment of any collateral ligament is stressing the joint (valgus for ulnar ligaments, varus for radial ligaments). This is accomplished with minimal stress and is helpful because joint fluid will often move into the ligament tear under ultrasound visualization. Other ulnar and radial collateral ligaments of the digits similarly appear as compact and hyperechoic fibrillar structures, which extend across each joint. Any suspected ligament tear can be assessed using dynamic imaging with valgus and varus joint angulation under ultrasound visualization.
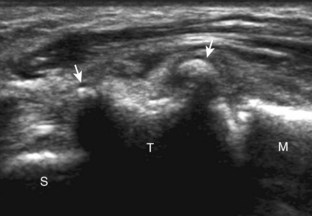
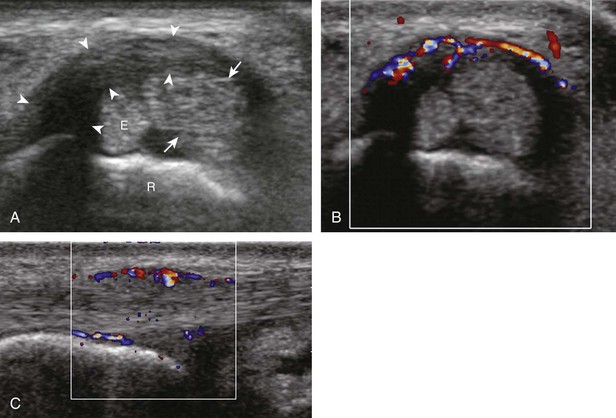
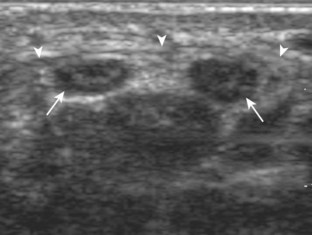
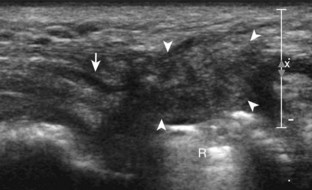
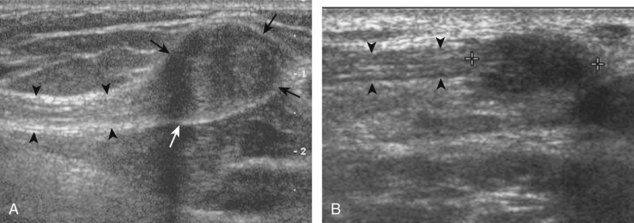
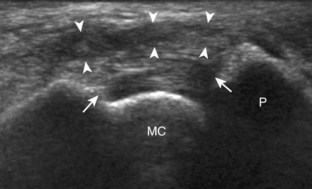
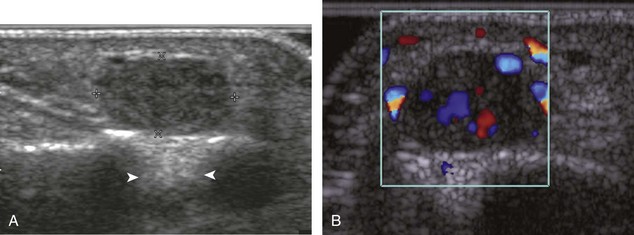
Joint Abnormalities
Because there are multiple synovial articulations of the hand and wrist, it is important to evaluate each individual site for joint abnormalities. In the sagittal plane, the volar and dorsal recesses of the radiocarpal and midcarpal joints are assessed for abnormal distention (Fig. 5-19A and B). The distal radioulnar joint is assessed from both dorsal and volar aspects in the transverse plane (see Fig. 5-19C). The digits are assessed in the sagittal plane over each joint, including the dorsal and volar joint recesses (see Fig. 5-19D and E) (Video 5-6)![]() . Anechoic distention of a joint recess typically represents simple fluid, although possible etiologies include degenerative, reactive, traumatic, and inflammatory causes; if there is concern for infection, ultrasound-guided aspiration should be considered. In the setting of trauma, one must evaluate the osseous structures at any focal area of symptoms for step-off deformity, which would indicate fracture.
. Anechoic distention of a joint recess typically represents simple fluid, although possible etiologies include degenerative, reactive, traumatic, and inflammatory causes; if there is concern for infection, ultrasound-guided aspiration should be considered. In the setting of trauma, one must evaluate the osseous structures at any focal area of symptoms for step-off deformity, which would indicate fracture.
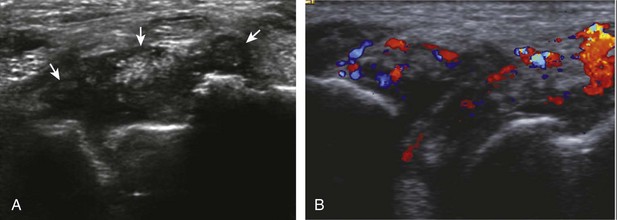
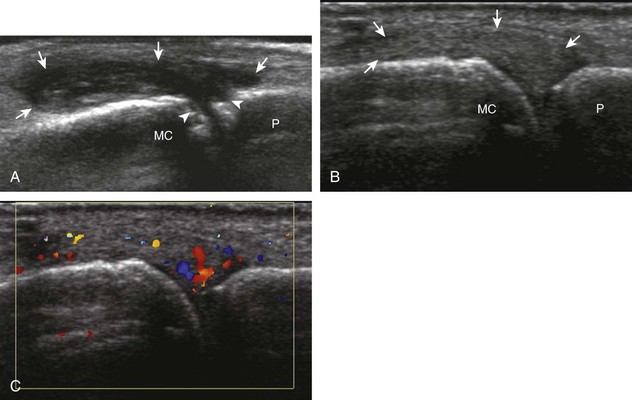
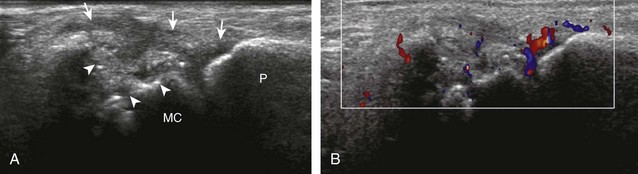
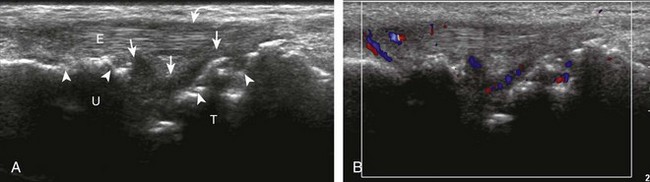
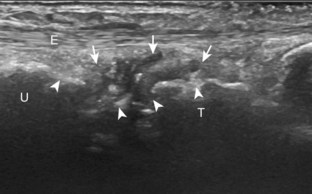
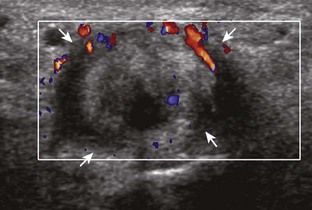
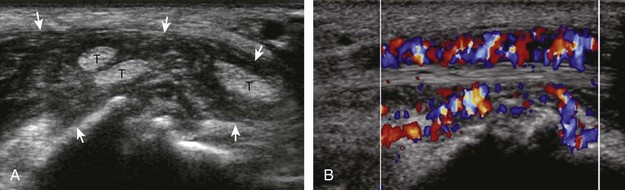
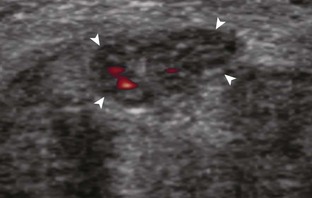
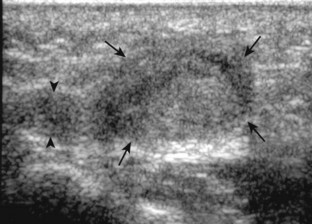
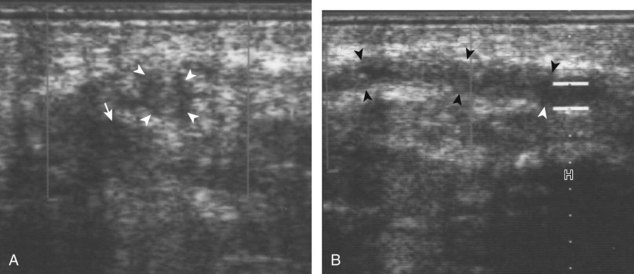
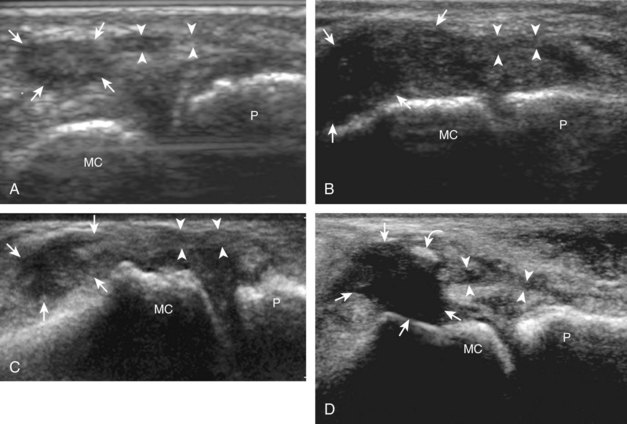
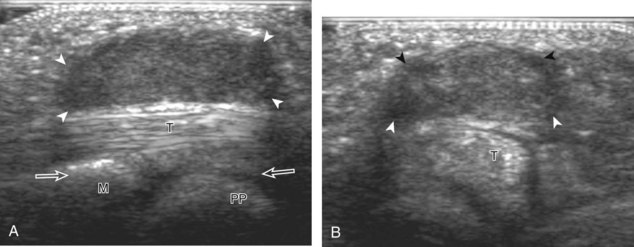
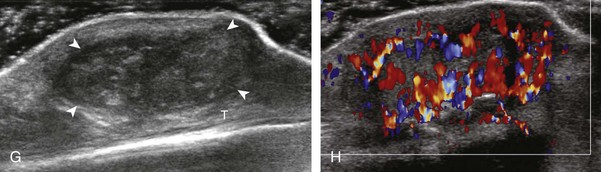
If a joint recess distention is not anechoic, considerations include complex fluid versus synovial hypertrophy (Figs. 5-20 and 5-21). Differentiation between these two etiologies may be difficult because both may appear hypoechoic or isoechoic compared with the overlying subcutaneous tissues. If joint recess distention collapses with transducer pressure or joint movement (see Video 5-6), or if swirling of echoes within the recess is identified, and if there is no internal flow on color or power Doppler imaging, then complex fluid is suspected. In contrast, if there is no displacement, little compressibility of the joint recess, and flow on color or power Doppler imaging, then synovial hypertrophy is likely (see Fig. 5-21) (Video 5-7)![]() .14 Ultrasound-guided aspiration may be needed to make this determination. Because dorsal wrist ganglion cysts occur at the site of the dorsal radiocarpal joint recess and may appear similar, dynamic imaging with compression and joint movement also helps in their differentiation because a ganglion cyst is multilocular and noncompressible, whereas a fluid-filled joint recess is compressible (see Fig. 5-87) (see Video 5-6).15 Possible etiologies for both complex fluid and synovial hypertrophy include hemorrhage and inflammation, which includes infection (Fig. 5-22), rheumatoid arthritis (Fig. 5-23), and gout (Fig. 5-24).
.14 Ultrasound-guided aspiration may be needed to make this determination. Because dorsal wrist ganglion cysts occur at the site of the dorsal radiocarpal joint recess and may appear similar, dynamic imaging with compression and joint movement also helps in their differentiation because a ganglion cyst is multilocular and noncompressible, whereas a fluid-filled joint recess is compressible (see Fig. 5-87) (see Video 5-6).15 Possible etiologies for both complex fluid and synovial hypertrophy include hemorrhage and inflammation, which includes infection (Fig. 5-22), rheumatoid arthritis (Fig. 5-23), and gout (Fig. 5-24).
Synovial hypertrophy appears as nondisplaceable and poorly or noncompressible distention of a joint recess that is hypoechoic or less frequently isoechoic or hyperechoic compared with the adjacent subdermal fat (Fig. 5-25) (Video 5-8)![]() .16 Active inflammatory synovitis is usually hypoechoic with hyperemia on color or power Doppler imaging. When evaluating superficial structures, it is important to float the transducer on a thick layer of gel so as to not compress the vascularity (see Fig. 2-29 in Chapter 2) (Video 5-9)
.16 Active inflammatory synovitis is usually hypoechoic with hyperemia on color or power Doppler imaging. When evaluating superficial structures, it is important to float the transducer on a thick layer of gel so as to not compress the vascularity (see Fig. 2-29 in Chapter 2) (Video 5-9)![]() . Minimal synovial thickening without hyperemia is not specific for one diagnosis and may be seen with osteoarthritis. Assessing multiple joints and review of history, laboratory values, and radiographic findings are important for the synthesis of a concise diagnosis of arthritis. Synovial proliferative disorders such as pigmented villonodular synovitis and synovial osteochondromatosis are other considerations. In the latter condition, superimposed hyperechoic calcifications may be seen in the synovial tissue.
. Minimal synovial thickening without hyperemia is not specific for one diagnosis and may be seen with osteoarthritis. Assessing multiple joints and review of history, laboratory values, and radiographic findings are important for the synthesis of a concise diagnosis of arthritis. Synovial proliferative disorders such as pigmented villonodular synovitis and synovial osteochondromatosis are other considerations. In the latter condition, superimposed hyperechoic calcifications may be seen in the synovial tissue.
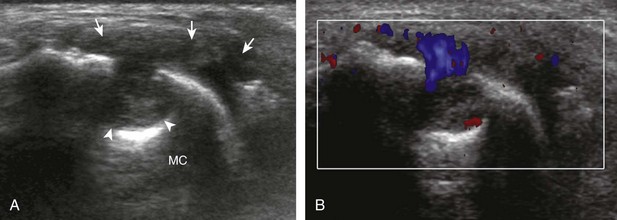
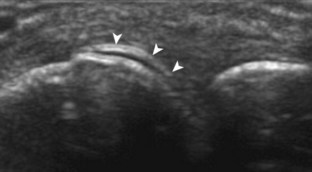
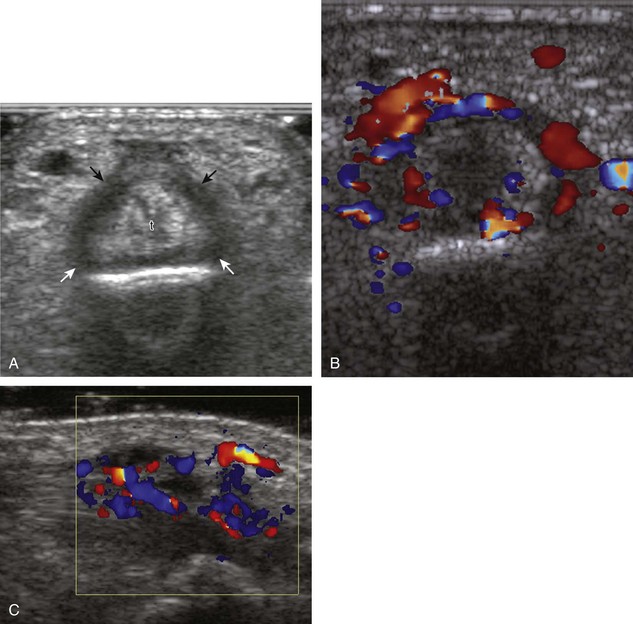
If inflammatory synovitis is suspected, it is important to evaluate the hypoechoic hyaline articular cartilage and the subjacent bone cortex for erosions (Figs. 5-26 to 5-29). Thinning or defects of the hyaline cartilage may be identified. An erosion appears as discontinuity or irregularity of the normally smooth and hyperechoic bone visible in two planes.16,17 When a bone erosion is suspected, the presence of adjacent synovitis increases the likelihood of a true erosion. Compared with radiography, ultrasound is more sensitive in detection of hand and wrist erosions and has the benefit of evaluating synovial thickness and hyperemia.18 When a potential erosion is seen at ultrasound, correlation with history, radiography, and other joints is essential because a false-positive rate of 29% has been reported; prominent concavities of the distal metacarpals and irregular osteophytes may simulate erosions.19 A small depression in the dorsal metacarpal at the edge of the hyaline cartilage can be a normal variation, especially at the second metacarpal (Fig. 5-30); unlike an erosion, this depression is smooth and shallow without cortical disruption or adjacent synovial hypertrophy.13 The finding of a true erosion with overlying synovitis is not specific for one diagnosis because many inflammatory conditions can produce these findings.
Because ultrasound is very sensitive in the identification of bone cortex surface abnormalities and irregularity, it is important to consider the various causes of such findings. In addition to an erosion, bone proliferation from a seronegative spondyloarthropathy or an osteophyte from osteoarthritis may also appear as cortical irregularity, and correlation with history, distribution of findings, and radiographs is essential. Bone irregularity from degenerative change can be differentiated from seronegative spondyloarthropathy in several ways. With degenerative change, bone proliferation is at the margins of a synovial articulation (osteophytes) (Fig. 5-31; see Fig. 5-19D and E), whereas bone proliferation with spondyloarthropathy can occur anywhere along the surface of a bone and particularly occurs at tendon or ligament attachments with possible hyperemia (Fig. 5-32). Inflammatory enthesopathy is also characterized by an abnormal hypoechoic tendon or ligament at their attachment site, with possible hyperemia, in association with bone proliferation or erosion at the tendon or ligament attachment.20
There are various protocols for inflammatory arthritis screening of the wrist and hand. With regard to rheumatoid arthritis, the second metacarpal is an important target to assess because it is a frequent site of involvement; assessment in the coronal plane at the radial aspect should complement dorsal assessment (see Fig. 5-26). Evaluation of the dorsal recess of the three wrist joints (radioulnar, radiocarpal, midcarpal), as well as the third metacarpophalangeal, is also essential.14 It has been shown that proximal interphalangeal joint assessment should include both dorsal and volar imaging.21,22 Focused assessment at any symptomatic site should also be completed, with consideration for the fifth metatarsophalangeal joint of the foot, another common site of rheumatoid arthritis involvement.23 A limited examination of the hand and wrist for assessment of rheumatoid arthritis has been proposed, which includes the joints of the wrist, the index and long fingers (metacarpophalangeal and proximal interphalangeal joints), and second and fifth metatarsophalangeal joints.24 However, a global or comprehensive examination of all key and symptomatic joint recesses of the wrist and hand for synovial hypertrophy can easily be accomplished with ultrasound. With regard to other inflammatory arthritis conditions, ultrasound assessment may be directed by symptoms or radiographic findings. For example, bone proliferation of psoriatic arthritis may occur anywhere, including the carpus or a single digit at ligament attachments (see Fig. 5-32). A gouty tophus may also occur at variable sites (Fig. 5-33) (Video 5-10)![]() , and one may also see monosodium urate crystals as complex fluid (see Fig. 5-24A) or layering over the hyaline cartilage (the double contour sign) (Fig. 5-34).
, and one may also see monosodium urate crystals as complex fluid (see Fig. 5-24A) or layering over the hyaline cartilage (the double contour sign) (Fig. 5-34).
Tendon and Muscle Abnormalities
Possible tendon abnormalities of the wrist and hand include tenosynovitis (and paratendinitis if inflammation surrounds a tendon that has no tendon sheath), tendinosis, and tendon tear. Tenosynovitis is characterized by distention of the synovial sheath around the tendon. Similar to a joint recess, distention of a tendon sheath may be predominantly anechoic (Figs. 5-35 and 5-36) (Video 5-11)![]() . If tendon sheath distention is not anechoic, possibilities include complex fluid versus synovial hypertrophy (Fig. 5-37). Compressibility, movement of internal echoes with transducer pressure, and lack of flow on color and power Doppler imaging suggest complex fluid rather than synovial hypertrophy, whereas noncompressibility and flow on color Doppler imaging suggest synovial hypertrophy (Video 5-12)
. If tendon sheath distention is not anechoic, possibilities include complex fluid versus synovial hypertrophy (Fig. 5-37). Compressibility, movement of internal echoes with transducer pressure, and lack of flow on color and power Doppler imaging suggest complex fluid rather than synovial hypertrophy, whereas noncompressibility and flow on color Doppler imaging suggest synovial hypertrophy (Video 5-12)![]() .25 Synovial hypertrophy may appear hypoechoic, isoechoic, or hyperechoic compared with subdermal fat (Fig. 5-38). Tenosynovitis may cause erosion of an adjacent bone, such as the ulnar styloid with rheumatoid arthritis (Fig. 5-39). Regardless of appearance, possible etiologies of tenosynovitis include degenerative, traumatic, proliferative, and inflammatory, including crystal deposition (Figs. 5-40 and 5-41) (Video 5-13)
.25 Synovial hypertrophy may appear hypoechoic, isoechoic, or hyperechoic compared with subdermal fat (Fig. 5-38). Tenosynovitis may cause erosion of an adjacent bone, such as the ulnar styloid with rheumatoid arthritis (Fig. 5-39). Regardless of appearance, possible etiologies of tenosynovitis include degenerative, traumatic, proliferative, and inflammatory, including crystal deposition (Figs. 5-40 and 5-41) (Video 5-13)![]() and infection (Fig. 5-42).26 It is important not to mistake the normal appearance of the extensor retinaculum at the level of the radiocarpal joint dorsally for tenosynovitis; the normal hyperechoic retinaculum may appear artifactually hypoechoic due to anisotropy, which adds to the potential confusion (see Fig. 5-11B).9
and infection (Fig. 5-42).26 It is important not to mistake the normal appearance of the extensor retinaculum at the level of the radiocarpal joint dorsally for tenosynovitis; the normal hyperechoic retinaculum may appear artifactually hypoechoic due to anisotropy, which adds to the potential confusion (see Fig. 5-11B).9
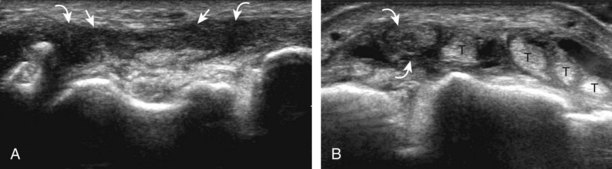
A specific stenosing tenosynovitis involves the extensor pollicis brevis and abductor pollicis longus tendons in the first dorsal wrist compartment, which is called de Quervain disease.26 This condition is characterized by thickening of the tissues around the involved tendons, with possible hyperemia, tendinosis, and cortical irregularity of the radius, associated with pain (Figs. 5-43 and 5-44) (Videos 5-14 and 5-15)![]() .27 The tendon sheath is thickened at the level of the radius, typically dorsally adjacent to the extensor pollicis brevis tendon, and associated tenosynovial fluid may only be seen proximal or distal to the retinaculum. A hypoechoic septum-like structure is often present that causes subcompartmentalization of the first extensor compartment, possibly with an osseous ridge, which is important when injection of the tendon sheath is considered.28,29 The abductor pollicis longus tendon may also have multiple tendon slips, which should not be mistaken for longitudinal tendon tears.28,29
.27 The tendon sheath is thickened at the level of the radius, typically dorsally adjacent to the extensor pollicis brevis tendon, and associated tenosynovial fluid may only be seen proximal or distal to the retinaculum. A hypoechoic septum-like structure is often present that causes subcompartmentalization of the first extensor compartment, possibly with an osseous ridge, which is important when injection of the tendon sheath is considered.28,29 The abductor pollicis longus tendon may also have multiple tendon slips, which should not be mistaken for longitudinal tendon tears.28,29
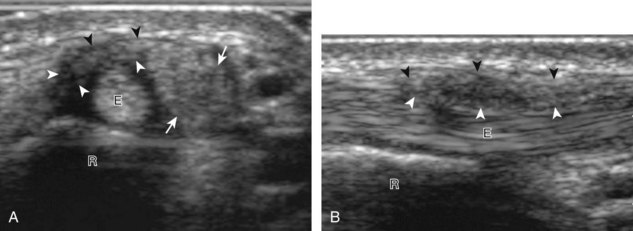
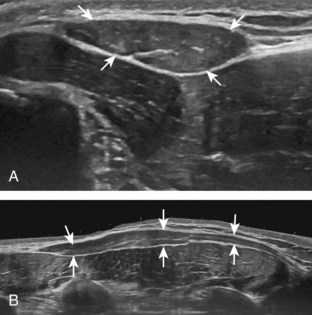
FIGURE 5-43 De Quervain disease.
(From Jacobson JA, Miller BS, Morag Y: Golf and racquet sports injuries. Semin Musculoskelet Radiol 9:346–359, 2005.)
Other tendon abnormalities include tendinosis and tendon tear. Tendinosis represents tendon degeneration, typically from overuse, and is characterized by hypoechoic swelling without disruption of tendon fibers (Fig. 5-45). Involvement from psoriatic arthritis may also cause hypoechoic thickening of a tendon and adjacent soft tissues, often with adjacent enthesopathy (Fig. 5-46).30 In the setting of inflammatory arthritis, abnormal tendon hypoechogenicity and increased flow on color or power Doppler imaging can indicate true tendinitis (see Figs. 5-39 and 5-46) (see Video 5-13). Calcium hydroxyapatite deposition appears hyperechoic with variable shadowing and may cause calcific tendinosis (Fig. 5-47). Partial tendon fiber disruption indicates partial-thickness tendon tear (Fig. 5-48). Involvement of the flexor carpi radialis tendon near the trapezium may be associated with osteoarthrosis (see Fig. 5-45B).6 The finding of complete fiber disruption indicates a full-thickness tendon tear (Figs. 5-49 and 5-50).31 Tendon injuries in the digits may also include bone avulsions, which will appear as a hyperechoic fragment (Fig. 5-51). This finding is best confirmed on radiography. In this setting, tendon retraction typically occurs, which is a helpful finding that indicates a full-thickness tear. If there is a question of partial versus full-thickness tendon tear, dynamic imaging with passive and active tendon movement can show either continuous fiber movement excluding a full-thickness tear (Video 5-16)![]() or lack of tendon translation across the abnormal site, which would indicate a full-thickness tear. Dynamic evaluation is also important for a diagnosis of tendon subluxation. The extensor carpi ulnaris subluxation is considered abnormal if greater than 50% of the tendon moves beyond the osseous groove in the ulna (Fig. 5-52) (Video 5-17)
or lack of tendon translation across the abnormal site, which would indicate a full-thickness tear. Dynamic evaluation is also important for a diagnosis of tendon subluxation. The extensor carpi ulnaris subluxation is considered abnormal if greater than 50% of the tendon moves beyond the osseous groove in the ulna (Fig. 5-52) (Video 5-17)![]() .8 Extensor tendon subluxation can be seen during finger flexion with extensor hood injuries, termed boxer knuckle (Fig. 5-53).32 If the patient has symptoms of intermittent snapping, clicking, or popping, the patient is asked to reproduce the symptom while evaluating the area with ultrasound.
.8 Extensor tendon subluxation can be seen during finger flexion with extensor hood injuries, termed boxer knuckle (Fig. 5-53).32 If the patient has symptoms of intermittent snapping, clicking, or popping, the patient is asked to reproduce the symptom while evaluating the area with ultrasound.
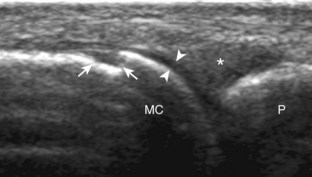
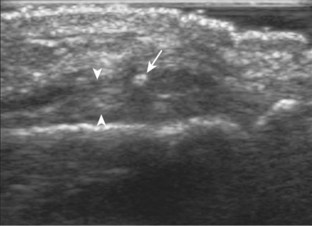
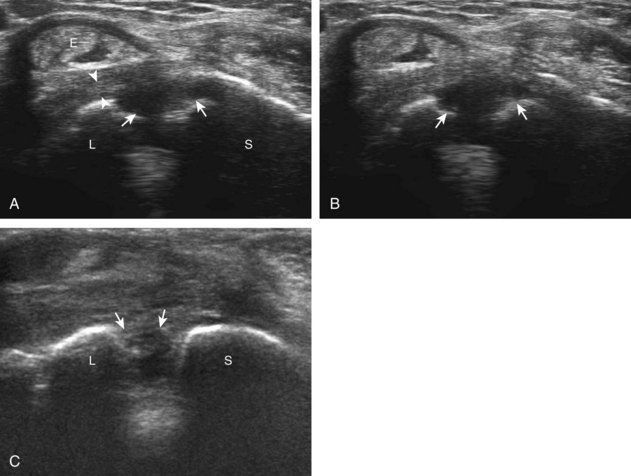
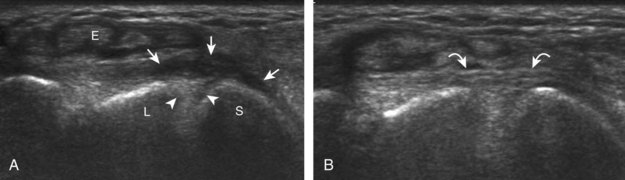
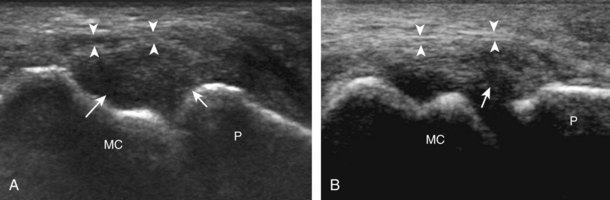
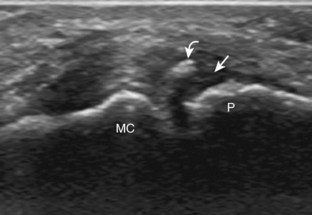
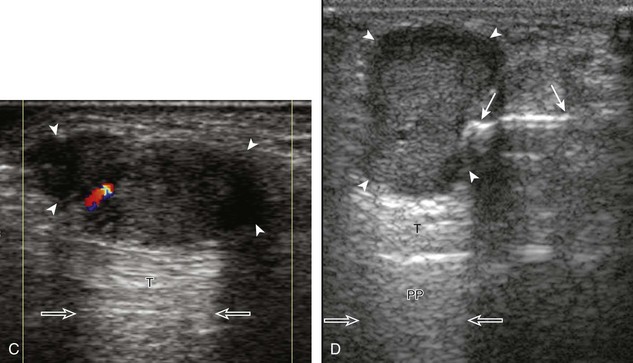
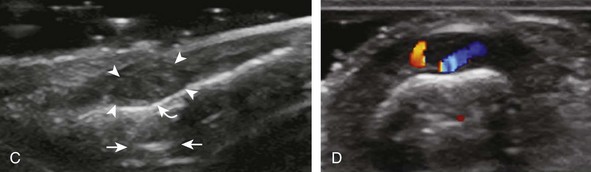
Ultrasound can be effective in the evaluation of pulley injuries of the digits.2 A pulley tear will appear as abnormal hypoechogenicity or absence of the pulley (Figs. 5-54 and 5-55). An important indirect sign of a pulley tear is abnormal volar displacement of the flexor tendons, called bowstringing, evaluated dynamically during active forced finger flexion (Fig. 5-56).33–35 Injury to the A2 pulley is common, often with adjacent pulley involvement. Less commonly, a pulley injury to the thumb may also be seen (Fig. 5-57). Another digit abnormality around the hand and digits is trigger finger, whereby impaired flexor tendon gliding is caused by tendon constriction due to thickening of the A1 pulley or tendon sheath (Fig. 5-58; see Fig. 5-57) (Video 5-18)![]() , with possible cyst formation (see Ganglion Cyst), pulley hyperemia, tendinosis, and tenosynovitis.36,37
, with possible cyst formation (see Ganglion Cyst), pulley hyperemia, tendinosis, and tenosynovitis.36,37
There are various other muscle and tendon abnormalities of the forearm, wrist, and hand, which are either uncommon or have nonspecific imaging features. However, there is a specific abnormality called intersection syndrome, in which a patient has pain where the muscles of the first and second wrist compartments cross in the distal forearm.27 At imaging, pain is produced with transducer pressure and hypoechoic swelling or adjacent fluid may be seen (Fig. 5-59). A more distal intersection syndrome may occur where the extensor pollicis longus tendon crosses over the extensor carpi radialis longus and brevis tendons. There exist a number of normal variations in the hand and wrist, including multiple tendon slips and the presence of accessory tendons and muscles, such as the extensor digitorum brevis manus, which may simulate a soft tissue mass at physical examination (Fig. 5-60) (Video 5-19)![]() .38,39 Masses of the tendons are discussed later with other hand and wrist masses.
.38,39 Masses of the tendons are discussed later with other hand and wrist masses.
Peripheral Nerve Abnormalities
Carpal Tunnel Syndrome
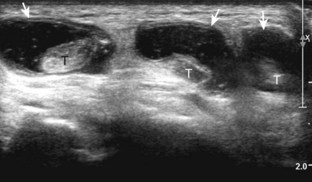
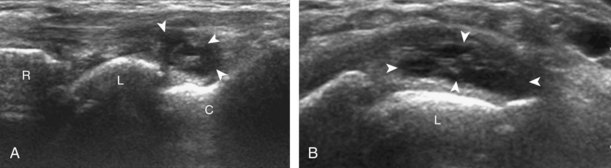
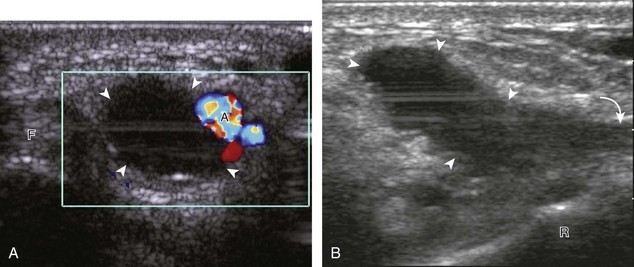
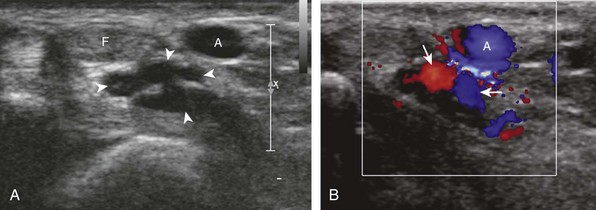
The most common upper extremity entrapment neuropathy is carpal tunnel syndrome, which involves the median nerve at the level of the wrist.40 Because the median nerve traverses the fibro-osseous carpal tunnel, any situation that decreases the size of the carpal tunnel or increases the volume of its contents can cause median nerve compression, such as trauma, mass, or tenosynovitis. At sonography, carpal tunnel syndrome is characterized by hypoechoic swelling of the median nerve as it enters into the carpal tunnel, although distal nerve swelling is also possible (Fig. 5-61) (Video 5-20)![]() . With regard to quantitative assessment for carpal tunnel syndrome, there have been many studies that recommend different size criteria and depend on how one balances sensitivity and specificity. Most studies conclude a cutoff of 9 to 12 mm2 as an indicator for carpal tunnel syndrome.40 However, another study has shown that a difference in median nerve area of 2 mm2 or more comparing proximal (at proximal pronator quadratus) and distal (at carpal tunnel) can diagnose carpal tunnel syndrome with 99% accuracy (Fig. 5-62). Of note, the circumferential trace method of measuring area is preferred, given variations in the shape of the median nerve. Other findings with carpal tunnel syndrome include bowing of the retinaculum in the transverse plane and flattening of the median nerve best seen in long axis, where the abrupt transition in size has been termed the notch sign. Also, imaging of the carpal tunnel during movement of the digits has shown decreased transverse sliding of the median nerve in carpal tunnel syndrome.41 Demonstration of blood flow on color Doppler imaging has also been shown to be an accurate indicator of carpal tunnel syndrome (Fig. 5-63).42,43 A bifid or high division of the median nerve, usually associated with a persistent median artery between the two nerve trunks, is a normal variant seen in 15% of the asymptomatic population that is often incomplete but not typically bilateral.44,45 Carpal tunnel syndrome may exist in this situation as well, where the hypoechoic and swollen two median nerve trunk areas combined show a difference of 4 mm2 or more comparing proximal (at pronator quadratus) and distal (at carpal tunnel) (Fig. 5-64) (Video 5-21)
. With regard to quantitative assessment for carpal tunnel syndrome, there have been many studies that recommend different size criteria and depend on how one balances sensitivity and specificity. Most studies conclude a cutoff of 9 to 12 mm2 as an indicator for carpal tunnel syndrome.40 However, another study has shown that a difference in median nerve area of 2 mm2 or more comparing proximal (at proximal pronator quadratus) and distal (at carpal tunnel) can diagnose carpal tunnel syndrome with 99% accuracy (Fig. 5-62). Of note, the circumferential trace method of measuring area is preferred, given variations in the shape of the median nerve. Other findings with carpal tunnel syndrome include bowing of the retinaculum in the transverse plane and flattening of the median nerve best seen in long axis, where the abrupt transition in size has been termed the notch sign. Also, imaging of the carpal tunnel during movement of the digits has shown decreased transverse sliding of the median nerve in carpal tunnel syndrome.41 Demonstration of blood flow on color Doppler imaging has also been shown to be an accurate indicator of carpal tunnel syndrome (Fig. 5-63).42,43 A bifid or high division of the median nerve, usually associated with a persistent median artery between the two nerve trunks, is a normal variant seen in 15% of the asymptomatic population that is often incomplete but not typically bilateral.44,45 Carpal tunnel syndrome may exist in this situation as well, where the hypoechoic and swollen two median nerve trunk areas combined show a difference of 4 mm2 or more comparing proximal (at pronator quadratus) and distal (at carpal tunnel) (Fig. 5-64) (Video 5-21)![]() .46 After surgical carpal tunnel release for treatment of carpal tunnel syndrome, the retinaculum may be thickened or disrupted, whereas the median nerve may return to normal size although displaced in a volar direction (Fig. 5-65).47 After steroid injection into the carpal tunnel, the median nerve may show a decrease in size as early as 7 days after injection.48 Uncommonly, median nerve compression in the carpal tunnel may be secondary to extrinsic compression by a mass, ganglion cyst (Fig. 5-66), or tenosynovitis (Fig. 5-67). A rare cause of enlargement of the median nerve is fibrolipomatous hamartoma, in which there is diffuse fatty infiltration of the nerve separating the normal-appearing nerve fascicles (Fig. 5-68).49
.46 After surgical carpal tunnel release for treatment of carpal tunnel syndrome, the retinaculum may be thickened or disrupted, whereas the median nerve may return to normal size although displaced in a volar direction (Fig. 5-65).47 After steroid injection into the carpal tunnel, the median nerve may show a decrease in size as early as 7 days after injection.48 Uncommonly, median nerve compression in the carpal tunnel may be secondary to extrinsic compression by a mass, ganglion cyst (Fig. 5-66), or tenosynovitis (Fig. 5-67). A rare cause of enlargement of the median nerve is fibrolipomatous hamartoma, in which there is diffuse fatty infiltration of the nerve separating the normal-appearing nerve fascicles (Fig. 5-68).49
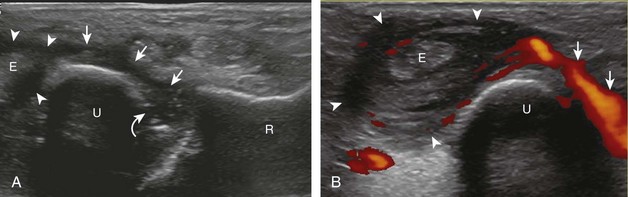
Ulnar Tunnel Syndrome
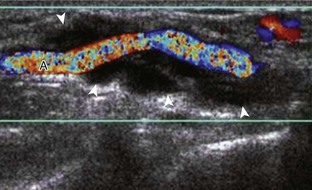
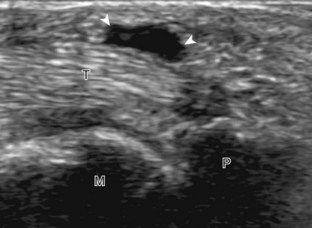
Another less common entrapment syndrome involves the ulnar nerve in Guyon canal, called ulnar tunnel syndrome.50 The cause of this syndrome is most commonly trauma. Because the hook of the hamate bone is directly deep to the ulnar nerve and artery, direct impact on the ulnar aspect of the hand can cause peripheral nerve or vascular injury. This may take the form of ulnar nerve contusion, ulnar nerve compression from an ulnar artery aneurysm (Fig. 5-69, online), or swelling within the ulnar tunnel, possibly associated with ulnar artery thrombosis (Fig. 5-70, online). At sonography, an abnormal ulnar nerve will appear hypoechoic with symptoms reproduced with transducer pressure when the ulnar nerve is compressed between the transducer and the hook of the hamate bone. To find the hook of the hamate bone, place the transducer in the sagittal plane just radial and distal to the pisiform bone, which is easily identified at sonography and physical examination. Ulnar artery aneurysm will appear as a heterogeneous mass in continuity with the ulnar artery, which demonstrates to-and-fro (yin-yang) flow on color or power Doppler imaging. No flow may be present with thrombosis. There exists a related entity called hypothenar hammer syndrome, in which direct trauma results in ulnar artery thrombosis or aneurysm and distal emboli to the digits, causing vascular insufficiency.51 Other causes of ulnar tunnel syndrome include vascular abnormalities and ganglion cyst. The ulnar nerve may also be compressed by an accessory abductor digiti minimi muscle, a normal variant seen in up to 24% of the population (Fig. 5-71).39
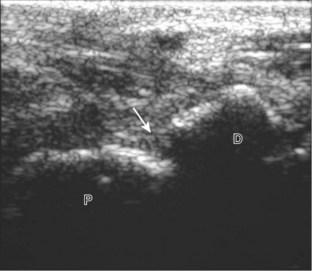
Radial Nerve Compression
The superficial branch of the radial nerve is located in the superficial and radial aspect of the mid-forearm. As the nerve continues distally, it crosses over the radial aspect of the forearm and the extensor pollicis brevis and abductor pollicis longus muscles. More distally, the superficial branch of the radial nerve continues into the dorsal wrist superficial to the extensor retinaculum. Compression of the superficial branch of the radial nerve may occur in the distal forearm, called Wartenberg syndrome, and can be caused by hematoma at an intravenous catheter site. Involvement from a mass or scar tissue is also possible (Fig. 5-72) (Video 5-22) ![]() .27,50
.27,50
Transection Neuromas
Injury to a peripheral nerve may have a variable appearance, depending on the type and degree of injury.52 After complete nerve transection, a neuroma may develop as the normal response of a transected nerve attempting to regenerate, which results in a tangled area of nerve fibers and scar tissue.53 At sonography, a neuroma will appear as a heterogeneous but predominantly hypoechoic mass (Fig. 5-73, online). Its appearance is not specific until continuity between the mass and the peripheral nerve is recognized. The segment of peripheral nerve that enters into the neuroma is often abnormally hypoechoic, which aids in its identification.
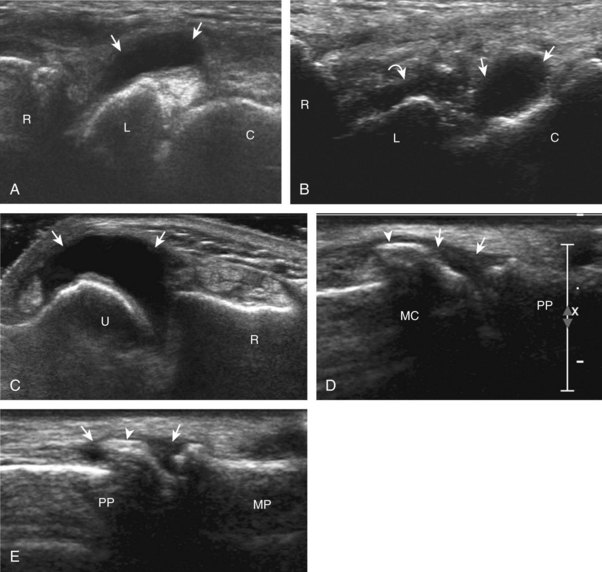
Ligament and Osseous Abnormalities
Scapholunate Ligament Injury
Acute trauma and repetitive overuse conditions may cause abnormalities to the wrist ligaments, cartilage, and adjacent osseous structures. With regard to the intrinsic wrist ligaments, the scapholunate ligament is one of many important stabilizing structures. Normally, a ligament has a hyperechoic and fibrillar echotexture, more compact than that of tendon, which connects bone to bone. An abnormal ligament may appear hypoechoic and thickened if partially torn, or it may not be visible, possibly replaced with anechoic fluid or hypoechoic synovitis when completely torn (Fig. 5-74).10,54 The space between the lunate and scaphoid bones may also be increased, which may further increase with clenched-fist maneuver or ulnar and radial deviation. The volar aspect of the scapholunate ligament, as well as the volar and dorsal aspects of the lunotriquetral ligaments, may also be evaluated.55 In addition to the intrinsic ligaments of the wrist, the various extrinsic wrist ligaments may also be evaluated for injury or abnormality, such as the dorsal radiocarpal ligament, which lies dorsal and superficial to the scapholunate ligament (Fig. 5-75).
Ulnar Collateral Ligament Injury (Thumb)
In addition to the wrist ligaments, the collateral ligaments of the digits may also be evaluated for tear. One specific ligament, the ulnar collateral ligament of the first metacarpophalangeal joint, deserves emphasis because of important surgical implications.56 This injury has been historically termed gamekeeper’s thumb because the injury occurs in hunters who strangle rabbits. More currently, this injury is called skier’s thumb. Similar to other ligament injuries, an injured ulnar collateral ligament may appear hypoechoic and swollen (Fig. 5-76A).57 Partial-thickness tear is characterized by partial disruption of the ligament fibers (see Fig. 5-76B), whereas complete fiber disruption will show complete fiber discontinuity (Fig. 5-77). Differentiation between a partial tear and nondisplaced full-thickness tear is extremely difficult; however, the primary goal is to identify a displaced full-thickness ulnar collateral ligament tear (or Stener lesion). Visualization of an echogenic avulsion fracture fragment may be a clue to full-thickness tear. Gentle valgus stress of the first metacarpophalangeal joint under ultrasound observation may help demonstrate a full-thickness ligament tear and retraction if fluid is identified entering into the torn ligament gap (Video 5-23A)![]() .
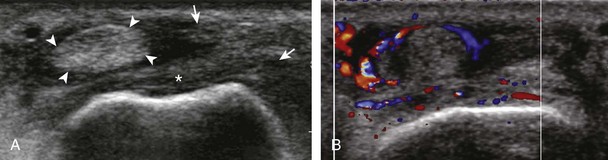
.
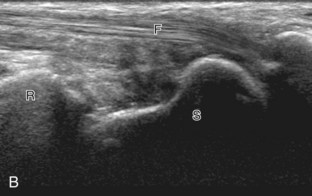
A Stener lesion represents a distal full-thickness ulnar collateral ligament tear of the first metacarpophalangeal joint, which is displaced proximal to the adductor pollicis aponeurosis (Fig. 5-78).56 In this situation, the ligament will not heal spontaneously, and therefore surgery is indicated to avoid chronic instability. At ultrasound, the Stener lesion will appear as a hypoechoic but heterogeneous, round, mass-like structure located proximal to the metacarpophalangeal joint in the plane of the normal ulnar collateral ligament (Fig. 5-79) (see Videos 5-23 and 5-24)![]() . Shadowing is often present deep to the Stener lesion related to sound beam refraction at the torn ligament end. In addition, normal ligament fibers are absent in their expected location crossing the first metacarpophalangeal joint. A hyperechoic and possibly shadowing focus attached to the retracted ligament distally is characteristic of a bone avulsion (see Fig. 5-79C). The ultrasound appearance of a Stener lesion has been likened to a yo-yo on a string, similar to findings on magnetic resonance imaging.58 The string of the yo-yo represents the adductor pollicis aponeurosis, and the yo-yo represents the balled-up and displaced proximal portion of the ulnar collateral ligament. Although the shape of the Stener lesion can be round, oval, or elongated (see Fig. 5-79C), the position of the displaced ligament is proximal to the leading edge of or uncommonly superficial to the adductor pollicis aponeurosis. Passive flexion of the interphalangeal joint will cause the adductor pollicis aponeurosis to slide over the ulnar collateral ligament, which assists in its identification and differentiation from the adjacent Stener lesion (see Videos 5-23 and 5-24). The adductor pollicis aponeurosis may be hypoechoic and thickened from injury as well (Fig. 5-80) (Video 5-25)
. Shadowing is often present deep to the Stener lesion related to sound beam refraction at the torn ligament end. In addition, normal ligament fibers are absent in their expected location crossing the first metacarpophalangeal joint. A hyperechoic and possibly shadowing focus attached to the retracted ligament distally is characteristic of a bone avulsion (see Fig. 5-79C). The ultrasound appearance of a Stener lesion has been likened to a yo-yo on a string, similar to findings on magnetic resonance imaging.58 The string of the yo-yo represents the adductor pollicis aponeurosis, and the yo-yo represents the balled-up and displaced proximal portion of the ulnar collateral ligament. Although the shape of the Stener lesion can be round, oval, or elongated (see Fig. 5-79C), the position of the displaced ligament is proximal to the leading edge of or uncommonly superficial to the adductor pollicis aponeurosis. Passive flexion of the interphalangeal joint will cause the adductor pollicis aponeurosis to slide over the ulnar collateral ligament, which assists in its identification and differentiation from the adjacent Stener lesion (see Videos 5-23 and 5-24). The adductor pollicis aponeurosis may be hypoechoic and thickened from injury as well (Fig. 5-80) (Video 5-25)![]() .
.
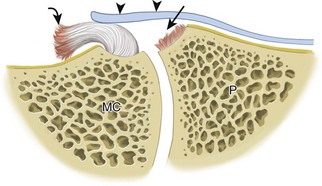
FIGURE 5-78 Stener lesion.
(Modified from an illustration by Carolyn Nowak, Ann Arbor, Michigan; http://www.carolyncnowak.com/MedTech.html.)
Other Ligament Injuries
Other collateral ligaments may be evaluated for tear, such as the radial collateral ligament of the thumb (Fig. 5-81). A hyperechoic bone fragment at a joint but not at the attachment of a ligament could relate to capsular (Fig. 5-82A) or volar plate avulsion fracture (see Fig. 5-82B). Cortical irregularity at a ligament attachment is not always due to trauma, and in the correct clinical setting, a seronegative spondyloarthropathy should be considered. Ultrasound findings in this scenario, such as psoriatic arthritis, include cortical irregularity or erosions and bone proliferation at a ligament attachment site (termed enthesopathy) with flow on color or power Doppler imaging and hypoechoic swelling of the adjacent ligament (Fig. 5-83) (Video 5-26)![]() . The overlying soft tissues may also be swollen and hypoechoic.
. The overlying soft tissues may also be swollen and hypoechoic.
Ligament abnormalities of the wrist may be associated with triangular fibrocartilage abnormalities, often associated with ulnar-sided wrist pain. Although often difficult to evaluate comprehensively with ultrasound, abnormalities of the triangular fibrocartilage will appear as abnormal hypoechogenicity, thinning, or absence (Fig. 5-84).11,59 It is important to identify the radius attachment of the triangular fibrocartilage to ensure complete evaluation.
An additional ligamentous-like abnormality involves the interosseous membrane between the radius and ulna of the forearm. This complex structure is comprised of a large main fiber bundle, a proximal dorsal oblique bundle, several accessory bundles, and a distal membranous portion.60 Sonographic evaluation of the interosseous membrane begins in the transverse plane of the dorsal mid-forearm. The transducer is angled slightly distally toward the ulna to elongate the interosseous membrane fibers. With injury of the interosseous membrane, the normally thin and hyperechoic appearance is replaced with hypoechoic thickening or disruption and nonvisualization (Fig. 5-85).61 Interosseous membrane injury is an important component of the Essex-Lopresti injury, in which a comminuted radial head fracture at the elbow is associated with interosseous membrane injury and distal radioulnar joint disruption.62
Osseous Injury
Injury to bone can be visible at sonography if a fracture extends to the visible portion of the bone cortex, commonly creating cortical disruption and a step-off deformity or an avulsion fracture fragment (see Fig. 5-82). The finding of the focal cortical step-off deformity is fairly specific for fracture, which is unlike the cortical irregularity at the margin of a joint with osteoarthritis from an osteophyte, although correlation with radiography is essential (see Figs. 5-19D and E and 5-31). Hyperemia, adjacent hypoechoic soft tissue swelling, and point tenderness with transducer pressure are other important associated findings of fracture. Although fractures may occur anywhere in the hand and wrist, it is the scaphoid fracture that receives much attention because a nontreated scaphoid fracture may result in nonunion and osteonecrosis of the proximal scaphoid pole. At sonography, it is important to evaluate the scaphoid bone for a cortical step-off deformity and adjacent soft tissue hematoma when there is history of trauma and snuffbox tenderness (Fig. 5-86).63 Small avulsion fractures of the hand and wrist are seen at tendon and ligament insertions and appear as focal hyperechoic, possibly shadowing foci.
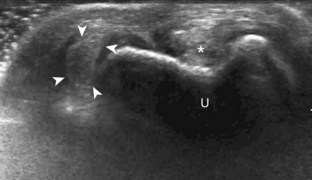
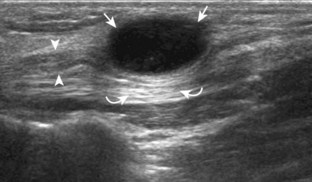
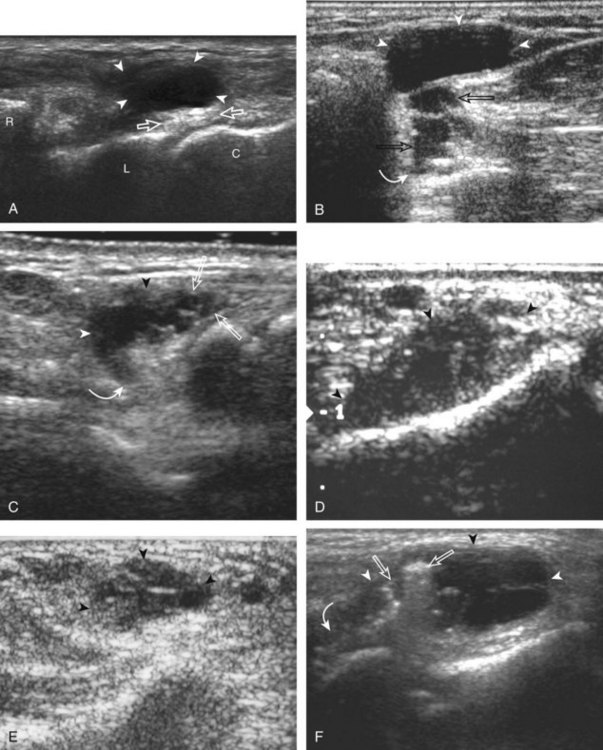
Ganglion Cyst
Most wrist masses are benign, and are most commonly ganglion cysts. Although the cause of ganglion cysts is uncertain, they may be degenerative, related to prior injury, or idiopathic. At sonography, a ganglion cyst may appear as an anechoic simple cyst with an imperceptible wall, no nodularity, and increased through-transmission (Fig. 5-87A).15,64,65 However, many ganglion cysts have a more variable appearance, possibly appearing multilocular (see Fig. 5-87B), irregular (see Fig. 5-87C), nodular, hypoechoic (see Fig. 5-87D), and mixed hypoechoic-isoechoic (see Fig. 5-87E).65,66 Hyperechoic foci from communicating intra-articular vacuum joint gas (see Fig. 5-87F) and hyperechoic hemorrhage (see Fig. 5-87G) are also possible. Increased through-transmission is typically present but may be absent when ganglion cysts are small.65 Given this somewhat variable appearance of wrist ganglion cysts, it is the location of the presumed ganglion that becomes very important in consideration of the correct diagnosis. Many ganglion cysts are located dorsal, adjacent to the scapholunate ligament (Fig. 5-88).15 It is important to differentiate a dorsal ganglion cyst from a distended dorsal wrist joint recess; with wrist movement or transducer pressure, a joint recess typically collapses, whereas a ganglion cyst is noncompressible (Fig. 5-19) (Videos 5-27 and 5-28)![]() .15 Another very common and often underreported site for ganglion cysts is volar, between the radial artery and the flexor carpi radialis tendon, with communication to the radiocarpal joint between the radius and scaphoid (Fig. 5-89) (Video 5-29)
.15 Another very common and often underreported site for ganglion cysts is volar, between the radial artery and the flexor carpi radialis tendon, with communication to the radiocarpal joint between the radius and scaphoid (Fig. 5-89) (Video 5-29)![]() . In this location, a ganglion cyst may appear pulsatile from the adjacent radial artery that may clinically simulate a radial artery aneurysm (Fig. 5-90). Pulsation from the adjacent radial artery may cause artifactual flow within the ganglion cyst (Fig. 5-91). Volar ganglion cysts may be small and nonpalpable, but symptomatic regardless; therefore, imaging between the radial artery and flexor carpi radialis tendons in addition to over the scapholunate ligament should be part of a scanning routine for wrist pain. A ganglion cyst may occur elsewhere in the wrist and hand and may cause carpal tunnel syndrome (see Fig. 5-66) and trigger finger (Fig. 5-92). It is also important to identify and describe any connection between a ganglion cyst and joint or tendon sheath because this becomes important with surgical removal. Percutaneous ultrasound-guided aspiration and steroid injection have been shown to be effective in the treatment of wrist ganglion cysts.67
. In this location, a ganglion cyst may appear pulsatile from the adjacent radial artery that may clinically simulate a radial artery aneurysm (Fig. 5-90). Pulsation from the adjacent radial artery may cause artifactual flow within the ganglion cyst (Fig. 5-91). Volar ganglion cysts may be small and nonpalpable, but symptomatic regardless; therefore, imaging between the radial artery and flexor carpi radialis tendons in addition to over the scapholunate ligament should be part of a scanning routine for wrist pain. A ganglion cyst may occur elsewhere in the wrist and hand and may cause carpal tunnel syndrome (see Fig. 5-66) and trigger finger (Fig. 5-92). It is also important to identify and describe any connection between a ganglion cyst and joint or tendon sheath because this becomes important with surgical removal. Percutaneous ultrasound-guided aspiration and steroid injection have been shown to be effective in the treatment of wrist ganglion cysts.67
Other Masses
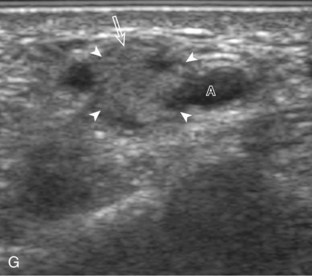
Giant Cell Tumor of the Tendon Sheath and Similar Masses
The differential diagnosis of a palpable abnormality of a digit near a tendon includes a cyst, such as a ganglion cyst or mucous cyst associated with osteoarthritis, or a solid mass. If in contact with a tendon, a giant cell tumor of the tendon sheath (also called localized pigmented villonodular tenosynovitis) should be strongly considered (Video 5-30)![]() .68–70 This hypoechoic solid mass is in contact with the tendon sheath but does not move with tendon translation (Fig. 5-93). Increased through-transmission may be present, as with other solid masses, and may initially be misinterpreted as a hypoechoic complex cyst; however, internal flow on color or power Doppler imaging indicates a solid mass. Another solid mass of the digit that may appear similar is a fibroma or, less commonly, an angioleiomyoma (Fig. 5-94). Because solid masses are not specific for one diagnosis, pathologic confirmation is necessary.
.68–70 This hypoechoic solid mass is in contact with the tendon sheath but does not move with tendon translation (Fig. 5-93). Increased through-transmission may be present, as with other solid masses, and may initially be misinterpreted as a hypoechoic complex cyst; however, internal flow on color or power Doppler imaging indicates a solid mass. Another solid mass of the digit that may appear similar is a fibroma or, less commonly, an angioleiomyoma (Fig. 5-94). Because solid masses are not specific for one diagnosis, pathologic confirmation is necessary.
Dupuytren Contracture
Patients with this fibrosing condition present with a palpable mass or nodularity superficial to the flexor tendons of the hand caused by thickening of the palmar aponeurosis, which can result in contracture.71 At ultrasound, an elongated plaque-like hypoechoic area is identified, typically superficial to one or more of the flexor tendons without flow on color or power Doppler imaging (Fig. 5-95). Uncommonly, a ruptured epidermal inclusion cyst may create a similar appearance. Although a typical epidermal inclusion cyst has a characteristic appearance at ultrasound (round or oval, hypoechoic to mildly echogenic with a possible hypoechoic halo), a ruptured epidermal inclusion cyst may have an irregular shape (Fig. 5-96).72,73
Glomus Tumor
A glomus tumor arises from a neuromyoarterial glomus body, most commonly beneath the nail or about the distal aspect of the digit. Clinically, this tumor may present with pain, point tenderness, and sensitivity to cold exposure. At ultrasound, a glomus tumor will appear as a focal hypoechoic mass with hyperemia, increased through-transmission, and possible cortical bone remodeling (Fig. 5-97) (Video 5-31)![]() .74 Because the imaging appearance is not specific for one diagnosis, it is the location of the abnormality that is important in suggesting the correct diagnosis.
.74 Because the imaging appearance is not specific for one diagnosis, it is the location of the abnormality that is important in suggesting the correct diagnosis.
Miscellaneous Masses
Although most solid masses are not specific for one diagnosis at ultrasound, associated imaging features may allow a precise diagnosis is some cases. For example, continuity between a mass and peripheral nerve is consistent with a peripheral nerve sheath tumor or a nerve transection neuroma (see Chapter 2). If a heterogeneous mass shows typical to-and-fro yin-yang flow on color or power Doppler imaging and there is continuity with a vascular structure, then pseudoaneurysm is the likely diagnosis. Other tumors may involve the hand and the wrist, including benign tumors such as soft tissue chondromas and malignant tumors such as malignant fibrous histiocytoma. Retained soft tissue foreign bodies may produce a mass-like appearance (see Chapter 2).
1 Linkous MD, Pierce SD, Gilula LA. Scapholunate ligamentous communicating defects in symptomatic and asymptomatic wrists: characteristics. Radiology. 2000;216:846–850.
2 Boutry N, Titecat M, Demondion X, et al. High-frequency ultrasonographic examination of the finger pulley system. J Ultrasound Med. 2005;24:1333–1339.
3 Theumann NH, Pfirrmann CW, Drape JL, et al. MR imaging of the metacarpophalangeal joints of the fingers: part I. Conventional MR imaging and MR arthrographic findings in cadavers. Radiology. 2002;222:437–445.
4 Jamadar DA, Jacobson JA, Hayes CW. Sonographic evaluation of the median nerve at the wrist. J Ultrasound Med. 2001;20:1011–1014.
5 Tagliafico A, Pugliese F, Bianchi S, et al. High-resolution sonography of the palmar cutaneous branch of the median nerve. AJR Am J Roentgenol. 2008;191:107–114.
6 Parellada AJ, Morrison WB, Reiter SB, et al. Flexor carpi radialis tendinopathy: spectrum of imaging findings and association with triscaphe arthritis. Skeletal Radiol. 2006;35:572–578.
7 Smith J, Rizzo M, Finnoff JT, et al. Sonographic appearance of the posterior interosseous nerve at the wrist. J Ultrasound Med. 2011;30:1233–1239.
8 Lee KS, Ablove RH, Singh S, et al. Ultrasound imaging of normal displacement of the extensor carpi ulnaris tendon within the ulnar groove in 12 forearm-wrist positions. AJR Am J Roentgenol. 2009;193:651–655.
9 Robertson BL, Jamadar DA, Jacobson JA, et al. Extensor retinaculum of the wrist: sonographic characterization and pseudotenosynovitis appearance. AJR Am J Roentgenol. 2007;188:198–202.
10 Jacobson JA, Oh E, Propeck T, et al. Sonography of the scapholunate ligament in four cadaveric wrists: correlation with MR arthrography and anatomy. AJR Am J Roentgenol. 2002;179:523–527.
11 Taljanovic MS, Goldberg MR, Sheppard JE, et al. US of the intrinsic and extrinsic wrist ligaments and triangular fibrocartilage complex: normal anatomy and imaging technique. Radiographics. 2011;31:e44.
12 Theumann NH, Pfirrmann CW, Antonio GE, et al. Extrinsic carpal ligaments: normal MR arthrographic appearance in cadavers. Radiology. 2003;226:171–179.
13 Boutry N, Larde A, Demondion X, et al. Metacarpophalangeal joints at US in asymptomatic volunteers and cadaveric specimens. Radiology. 2004;232:716–724.
14 McNally EG. Ultrasound of the small joints of the hands and feet: current status. Skeletal Radiol. 2008;37:99–113.
15 Cardinal E, Buckwalter KA, Braunstein EM, et al. Occult dorsal carpal ganglion: comparison of US and MR imaging. Radiology. 1994;193:259–262.
16 Wakefield RJ, Balint PV, Szkudlarek M, et al. Musculoskeletal ultrasound including definitions for ultrasonographic pathology. J Rheumatol. 2005;32:2485–2487.
17 Lund PJ, Heikal A, Maricic MJ, et al. Ultrasonographic imaging of the hand and wrist in rheumatoid arthritis. Skeletal Radiol. 1995;24:591–596.
18 Lopez-Ben R, Bernreuter WK, Moreland LW, et al. Ultrasound detection of bone erosions in rheumatoid arthritis: a comparison to routine radiographs of the hands and feet. Skeletal Radiol. 2004;33:80–84.
19 Finzel S, Ohrndorf S, Englbrecht M, et al. A detailed comparative study of high-resolution ultrasound and micro-computed tomography for detection of arthritic bone erosions. Arthritis Rheum. 2011;63:1231–1236.
20 Gutierrez M, Filippucci E, De Angelis R, et al. A sonographic spectrum of psoriatic arthritis: “the five targets.”. Clin Rheumatol. 2010;29:133–142.
21 Backhaus M, Burmester GR, Gerber T, et al. Guidelines for musculoskeletal ultrasound in rheumatology. Ann Rheum Dis. 2001;60:641–649.
22 Vlad V, Berghea F, Libianu S, et al. Ultrasound in rheumatoid arthritis: volar versus dorsal synovitis evaluation and scoring. BMC Musculoskelet Disord. 2011;12:124.
23 Sheane BJ, Beddy P, O’Connor M, et al. Targeted ultrasound of the fifth metatarsophalangeal joint in an early inflammatory arthritis cohort. Arthritis Rheum. 2009;61:1004–1008.
24 Backhaus M, Ohrndorf S, Kellner H, et al. Evaluation of a novel 7-joint ultrasound score in daily rheumatologic practice: a pilot project. Arthritis Rheum. 2009;61:1194–1201.
25 Breidahl WH, Stafford Johnson DB, Newman JS, et al. Power Doppler sonography in tenosynovitis: significance of the peritendinous hypoechoic rim. J Ultrasound Med. 1998;17:103–107.
26 Daenen B, Houben G, Bauduin E, et al. Sonography in wrist tendon pathology. J Clin Ultrasound. 2004;32:462–469.
27 De Maeseneer M, Marcelis S, Jager T, et al. Spectrum of normal and pathologic findings in the region of the first extensor compartment of the wrist: sonographic findings and correlations with dissections. J Ultrasound Med. 2009;28:779–786.
28 Choi SJ, Ahn JH, Lee YJ, et al. de Quervain disease: US identification of anatomic variations in the first extensor compartment with an emphasis on subcompartmentalization. Radiology. 2011;260:480–486.
29 Rousset P, Vuillemin-Bodaghi V, Laredo JD, et al. Anatomic variations in the first extensor compartment of the wrist: accuracy of US. Radiology. 2010;257:427–433.
30 Gutierrez M, Filippucci E, Salaffi F, et al. Differential diagnosis between rheumatoid arthritis and psoriatic arthritis: the value of ultrasound findings at metacarpophalangeal joints level. Ann Rheum Dis. 2011;70:1111–1114.
31 De Maeseneer M, Marcelis S, Osteaux M, et al. Sonography of a rupture of the tendon of the extensor pollicis longus muscle: initial clinical experience and correlation with findings at cadaveric dissection. AJR Am J Roentgenol. 2005;184:175–179.
32 Lopez-Ben R, Lee DH, Nicolodi DJ. Boxer knuckle (injury of the extensor hood with extensor tendon subluxation): diagnosis with dynamic US: report of three cases. Radiology. 2003;228:642–646.
33 Hauger O, Chung CB, Lektrakul N, et al. Pulley system in the fingers: normal anatomy and simulated lesions in cadavers at MR imaging, CT, and US with and without contrast material distention of the tendon sheath. Radiology. 2000;217:201–212.
34 Klauser A, Frauscher F, Bodner G, et al. Finger pulley injuries in extreme rock climbers: depiction with dynamic US. Radiology. 2002;222:755–761.
35 Martinoli C, Bianchi S, Nebiolo M, et al. Sonographic evaluation of digital annular pulley tears. Skeletal Radiol. 2000;29:387–391.
36 Guerini H, Pessis E, Theumann N, et al. Sonographic appearance of trigger fingers. J Ultrasound Med. 2008;27:1407–1413.
37 Serafini G, Derchi LE, Quadri P, et al. High resolution sonography of the flexor tendons in trigger fingers. J Ultrasound Med. 1996;15:213–219.
38 Ouellette H, Thomas BJ, Torriani M. Using dynamic sonography to diagnose extensor digitorum brevis manus. AJR Am J Roentgenol. 2003;181:1224–1226.
39 Timins ME. Muscular anatomic variants of the wrist and hand: findings on MR imaging. AJR Am J Roentgenol. 1999;172:1397–1401.
40 Klauser AS, Faschingbauer R, Bauer T, et al. Entrapment neuropathies II: carpal tunnel syndrome. Semin Musculoskelet Radiol. 2010;14:487–500.
41 Nakamichi K, Tachibana S. Restricted motion of the median nerve in carpal tunnel syndrome. J Hand Surg [Br]. 1995;20:460–464.
42 Ghasemi-Esfe AR, Khalilzadeh O, Vaziri-Bozorg SM, et al. Color and power Doppler US for diagnosing carpal tunnel syndrome and determining its severity: a quantitative image processing method. Radiology. 2011;261:499–506.
43 Mallouhi A, Pultzl P, Trieb T, et al. Predictors of carpal tunnel syndrome: accuracy of gray-scale and color Doppler sonography. AJR Am J Roentgenol. 2006;186:1240–1245.
44 Granata G, Caliandro P, Pazzaglia C, et al. Prevalence of bifid median nerve at wrist assessed through ultrasound. Neurol Sci. 2011;32:615–618.
45 Propeck T, Quinn TJ, Jacobson JA, et al. Sonography and MR imaging of bifid median nerve with anatomic and histologic correlation. AJR Am J Roentgenol. 2000;175:1721–1725.
46 Klauser AS, Halpern EJ, Faschingbauer R, et al. Bifid median nerve in carpal tunnel syndrome: assessment with US cross-sectional area measurement. Radiology. 2011;259:808–815.
47 Abicalaf CA, de Barros N, Sernik RA, et al. Ultrasound evaluation of patients with carpal tunnel syndrome before and after endoscopic release of the transverse carpal ligament. Clin Radiol. 2007;62:891–894. discussion 5–6
48 Cartwright MS, White DL, Demar S, et al. Median nerve changes following steroid injection for carpal tunnel syndrome. Muscle Nerve. 2011;44:25–29.
49 De Maeseneer M, Jaovisidha S, Lenchik L, et al. Fibrolipomatous hamartoma: MR imaging findings. Skeletal Radiol. 1997;26:155–160.
50 Jacobson JA, Fessell DP, Lobo Lda G, et al. Entrapment neuropathies I: upper limb (carpal tunnel excluded). Semin Musculoskelet Radiol. 2010;14:473–486.
51 Velling TE, Brennan FJ, Hall LD, et al. Sonographic diagnosis of ulnar artery aneurysm in hypothenar hammer syndrome: report of 2 cases. J Ultrasound Med. 2011;20:921–924.
52 Tagliafico A, Altafini L, Garello I, et al. Traumatic neuropathies: spectrum of imaging findings and postoperative assessment. Semin Musculoskelet Radiol. 2010;14:512–522.
53 Thomas AJ, Bull MJ, Howard AC, et al. Perioperative ultrasound guided needle localisation of amputation stump neuroma. Injury. 1999;30:689–691.
54 Renoux J, Zeitoun-Eiss D, Brasseur JL. Ultrasonographic study of wrist ligaments: review and new perspectives. Semin Musculoskelet Radiol. 2009;13:55–65.
55 Boutry N, Lapegue F, Masi L, et al. Ultrasonographic evaluation of normal extrinsic and intrinsic carpal ligaments: preliminary experience. Skeletal Radiol. 2005;34:513–521.
56 Hergan K, Mittler C, Oser W. Ulnar collateral ligament: differentiation of displaced and nondisplaced tears with US and MR imaging. Radiology. 1995;194:65–71.
57 Ebrahim FS, De Maeseneer M, Jager T, et al. US diagnosis of UCL tears of the thumb and Stener lesions: technique, pattern-based approach, and differential diagnosis. Radiographics. 2006;26:1007–1020.
58 Spaeth HJ, Abrams RA, Bock GW, et al. Gamekeeper thumb: differentiation of nondisplaced and displaced tears of the ulnar collateral ligament with MR imaging. Work in progress. Radiology. 1993;188:553–556.
59 Chiou HJ, Chang CY, Chou YH, et al. Triangular fibrocartilage of wrist: presentation on high resolution ultrasonography. J Ultrasound Med. 1998;17:41–48.
60 McGinley JC, Roach N, Gaughan JP, et al. Forearm interosseous membrane imaging and anatomy. Skeletal Radiol. 2004;33:561–568.
61 Rodriguez-Martin J, Pretell-Mazzini J. The role of ultrasound and magnetic resonance imaging in the evaluation of the forearm interosseous membrane: a review. Skeletal Radiol. 2011;40:1515–1522.
62 Failla JM, Jacobson J, van Holsbeeck M. Ultrasound diagnosis and surgical pathology of the torn interosseous membrane in forearm fractures/dislocations. J Hand Surg [Am]. 1999;24:257–266.
63 Platon A, Poletti PA, Van Aaken J, et al. Occult fractures of the scaphoid: the role of ultrasonography in the emergency department. Skeletal Radiol. 2011;40:869–875.
64 Bianchi S, Abdelwahab IF, Zwass A, et al. Ultrasonographic evaluation of wrist ganglia. Skeletal Radiol. 1994;23:201–203.
65 Wang G, Jacobson JA, Feng FY, et al. Sonography of wrist ganglion cysts: variable and noncystic appearances. J Ultrasound Med. 2007;26:1323–1328. quiz 30–31
66 Teefey SA, Dahiya N, Middleton WD, et al. Ganglia of the hand and wrist: a sonographic analysis. AJR Am J Roentgenol. 2008;191:716–720.
67 Breidahl WH, Adler RS. Ultrasound-guided injection of ganglia with corticosteroids. Skeletal Radiol. 1996;25:635–638.
68 Middleton WD, Patel V, Teefey SA, et al. Giant cell tumors of the tendon sheath: analysis of sonographic findings. AJR Am J Roentgenol. 2004;183:337–339.
69 Murphey MD, Rhee JH, Lewis RB, et al. Pigmented villonodular synovitis: radiologic-pathologic correlation. Radiographics. 2008;28:1493–1518.
70 Wang Y, Tang J, Luo Y. The value of sonography in diagnosing giant cell tumors of the tendon sheath. J Ultrasound Med. 2007;26:1333–1340.
71 Yacoe ME, Bergman AG, Ladd AL, et al. Dupuytren’s contracture: MR imaging findings and correlation between MR signal intensity and cellularity of lesions. AJR Am J Roentgenol. 1993;160:813–817.
72 Jin W, Ryu KN, Kim GY, et al. Sonographic findings of ruptured epidermal inclusion cysts in superficial soft tissue: emphasis on shapes, pericystic changes, and pericystic vascularity. J Ultrasound Med. 2008;27:171–176. quiz 7–8
73 Kim HK, Kim SM, Lee SH, et al. Subcutaneous epidermal inclusion cysts: ultrasound (US) and MR imaging findings. Skeletal Radiol. 2011;40:1415–1419.
74 Glazebrook KN, Laundre BJ, Schiefer TK, et al. Imaging features of glomus tumors. Skeletal Radiol. 2011;40:855–862.