Wells syndrome

Management strategy
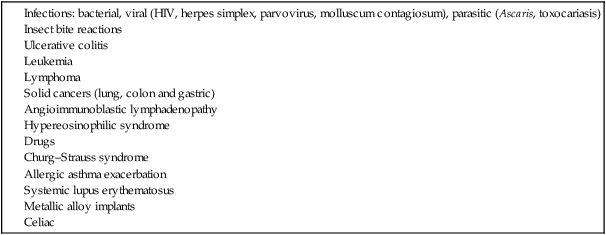
Although there is no known cause, several precipitating factors have been suggested (Table 247.1). Some of the associations are well reported, others anecdotal. The tumor necrosis factor antagonists may produce injection site or widespread lesions; etanercept and adalimumab may induce Wells syndrome localized to injection sites. Minocycline can also induce a Wells syndrome-like disorder.





 Cetirizine
Cetirizine Cyclosporine
Cyclosporine Dapsone
Dapsone Interferon-α
Interferon-α Minocycline
Minocycline Sulfasalzine
Sulfasalzine Griseofulvin
Griseofulvin Tacrolimus
Tacrolimus