Vitreous
Normal Anatomy
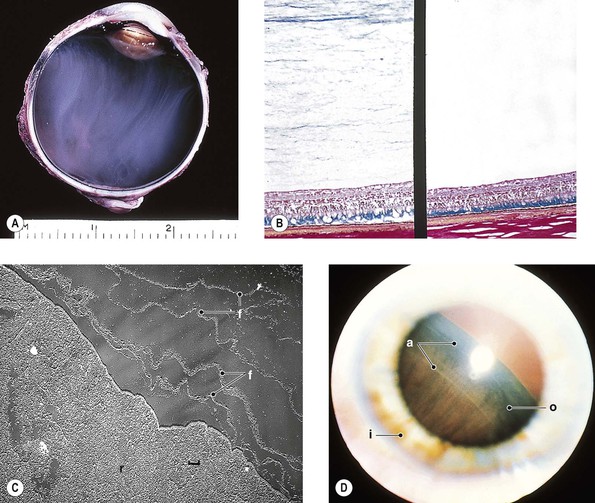
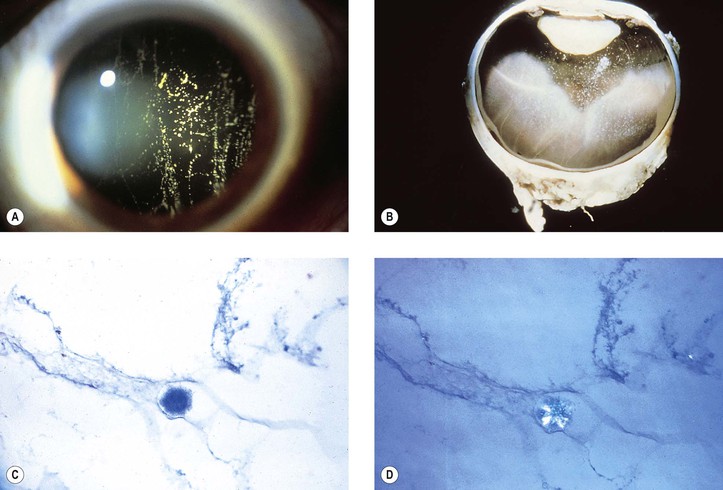
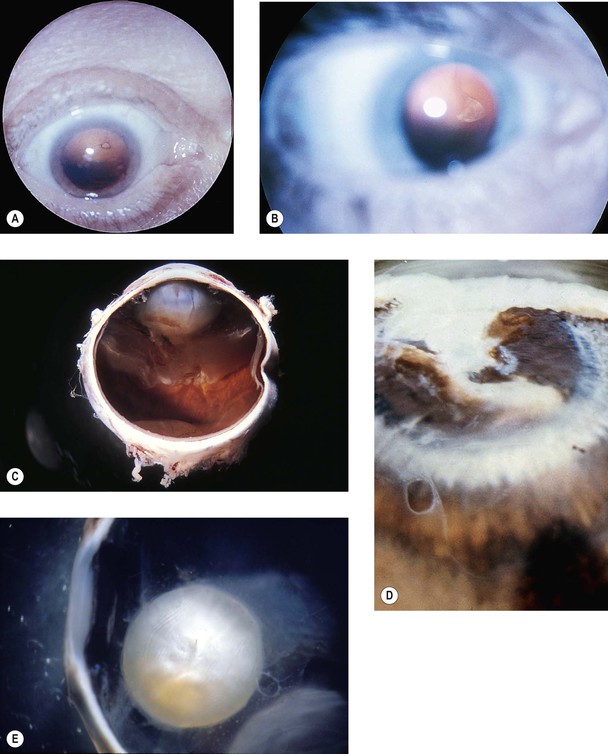
I. The transparent vitreous body, or hyaloid (Fig. 12.1), is one of the most delicate connective tissues in the body.
II. Embryology
B. The hyaloid vessel, which atrophies and disappears before birth, passes through the canal.
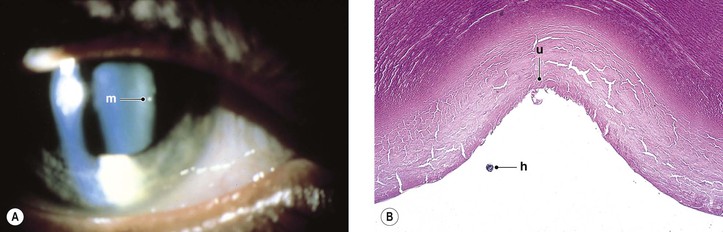
C. Persisting remnants of the primary vitreous or hyaloid vessel produce congenital anomalies (see later), the most common being retention of tissue fragments on the back of the lens (Mittendorf’s dot; Fig. 12.2), retention of tissue on the nasal optic disc (Bergmeister’s papilla), and persistent primary vitreous (see Chapter 18).
Congenital Anomalies
Persistent Primary Vitreous
A. Anterior remnants (see Fig. 12.2; see also Fig. 9.3)
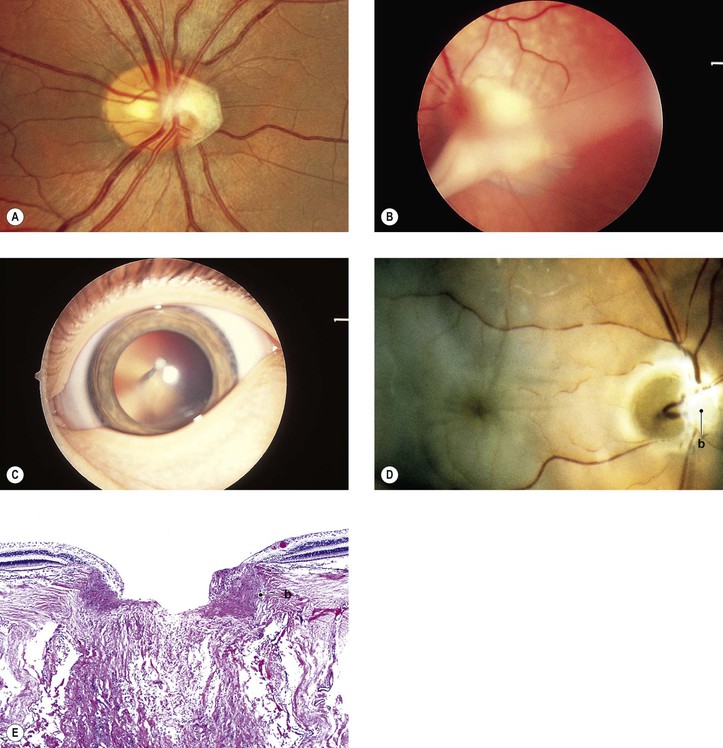
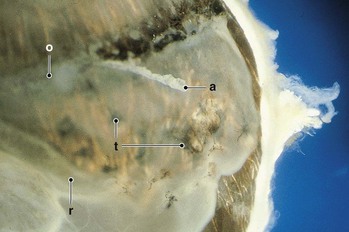
B. Posterior remnants (Fig. 12.3)
1. Vascular loops from the optic disc may remain within Cloquet’s canal.
Persistent Hyperplastic Primary Vitreous (Persistent Fetal Vasculature)
II. Posterior (congenital retinal septum; ablatio falciformis congenita)
A. Posterior persistent hyperplastic primary vitreous (PHPV; see Fig. 12.3) is most often unilateral and present at birth. Poor vision and strabismus are the most common presenting complaints.
Vitreous Adhesions
Post Nonsurgical and Surgical Trauma
I. Vitreocorneal adhesions may cause corneal “touch” syndrome (see Fig. 5.5).
B. The cornea becomes thickened and edematous in the region of touch.
III. Cyclovitreal adhesions may lead to a cyclitic membrane and subsequent neural retinal detachment.
IV. Vitreoretinal adhesions may lead to the macular vitreous traction syndrome (cystoid macular edema; Irvine–Gass syndrome; see Chapter 5) or to wrinkling of the internal limiting membrane, namely “cellophane” retina (see Figs. 11.43–11.45).
Postinflammation
See Chapters 3 and 4.
Idiopathic
Idiopathic vitreous adhesions may follow partial vitreoretinal separation (posterior vitreous detachment).
Vitreous Opacities
Hyaloid Vessel Remnants
Muscae volitantes are minute remnants of the hyaloid vascular system or detachments of small folds of poorly differentiated retinal tissue, usually present in the anterior vitreous.
Acquired Vitreous Strands and Floaters
II. Separation of the vitreous attachment to the optic disc after posterior vitreoretinal separation may cause a complete or incomplete ringlike floater (vitreous “peephole”; see subsection on vitreous detachment, later).
III. Symptomatic degenerative vitreous floaters may have a negative impact on the quality of life.
Inflammatory Cells
II. Whitish masses (“white balls”) may be seen inferiorly with vitreitis (e.g., sarcoidosis).
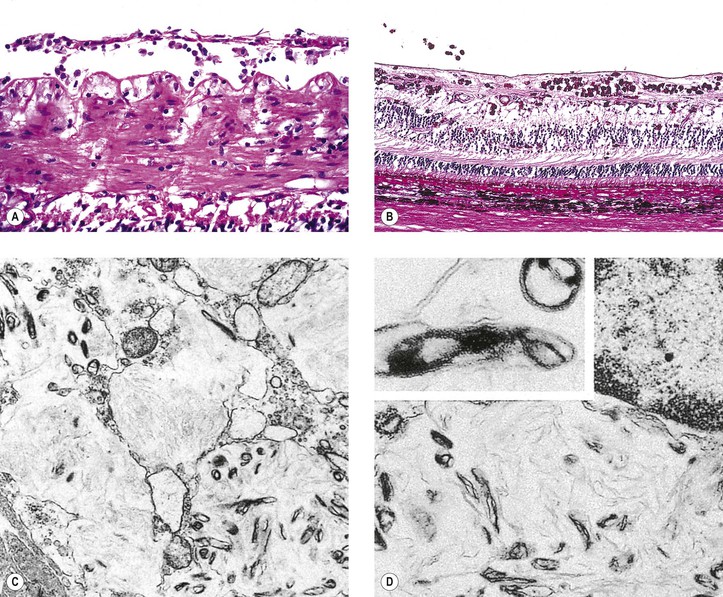
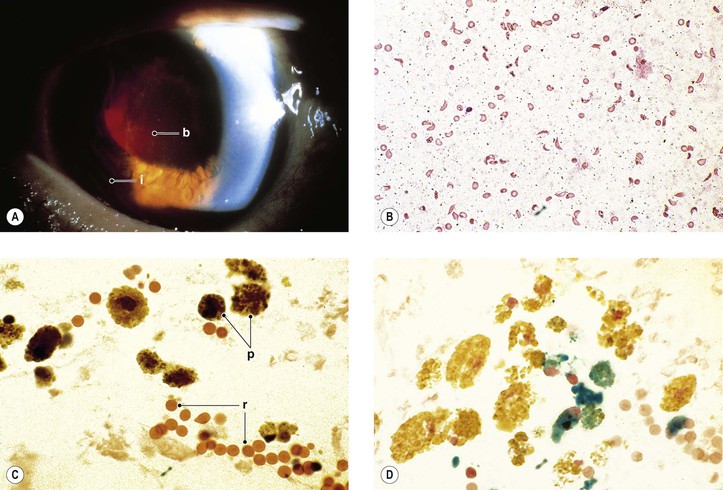
III. Numerous vitreous opacities, foamy “Whipple” macrophages, may be found in persons with Whipple’s disease (Fig. 12.4).
A. Whipple’s disease is a disorder of men, usually older than 35 years of age.
C. Ocular findings, in addition to vitreous opacities, include inflammations and ophthalmoplegia.
D. Foamy macrophages containing periodic acid–Schiff (PAS)-positive cytoplasm may be found in intestinal and rectal mucosa, mesenteric and extra-abdominal lymphatic tissue, heart, lungs, liver, adrenals, spleen, serous membranes, neural retina, and vitreous.
Red Blood Cells
I. Red blood cells in the vitreous compartment (see Figs. 12.11 and 12.12) are most often caused by neural retinal tears but may have other causes. Red blood cells may be subvitreal (between vitreous body and internal limiting membrane of the neural retina) or intravitreal (within the vitreous body).
II. Hypoxia of the vitreous body may be demonstrated when blood enters it in a patient who has sickle-cell trait or disease.
Iridescent Particles
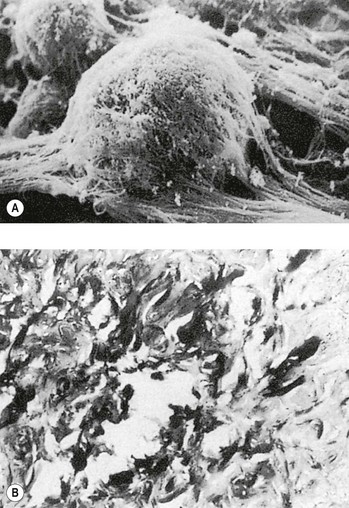
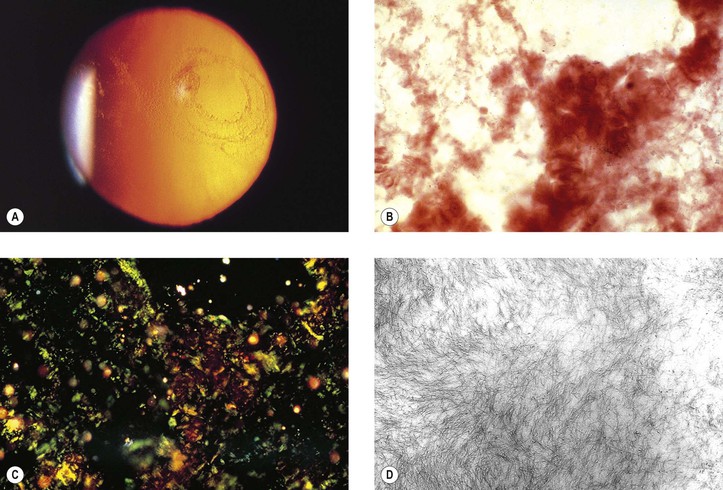
I. Asteroid hyalosis (Benson’s disease; Figs. 12.5 and 12.6) consists of complex lipids embedded in an amorphous matrix containing mainly calcium and phosphorus and attached to the vitreous framework.
B. Asteroid hyalosis has the following clinical properties:
II. Synchysis scintillans (cholesterolosis; see Figs. 5.39 and 5.40) consists of degenerative material not attached to the vitreous framework.
A. Synchysis scintillans has the following clinical properties:
1. It is golden in color both to retroillumination and to direct view.
2. Usually it is unilateral and most common in men in their fourth or fifth decade.
3. It frequently follows an intravitreal (within vitreous body) hemorrhage.
4. The material settles inferiorly when the eye is immobile.
Retinal Fragments
A free-floating operculum is the nonattached or separated neural retinal tissue derived from a neural retinal hole.
Traumatic Avulsion of Vitreous Base
The condition is rare and usually caused by trauma or shrinkage of vitreal fibrous membranes (Fig. 12.7).
Amyloid
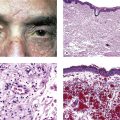
I. Primary familial amyloidosis (AL amyloidosis; Fig. 12.10; see also Chapter 7)
D. Glaucoma may be caused by amyloid deposition in the aqueous outflow areas.
E. Systemic amyloid deposition is widespread.
2. The walls of retinal and choroidal blood vessels may be thickened by the amyloid material.
II. Familial amyloidotic polyneuropathy (FAP)
A. FAP is a hereditary form of systemic amyloidosis that involves vitreous (types I and II) and peripheral nerves. FAP, first described in an Indian pedigree with Swiss origins, also has been described in Portuguese, Swedish, and Japanese kindreds.
1. In both FAP types I and II, the responsible protein is mutant transthyretin, designated amyloid AF.
4. Patients with types III and IV FAP do not acquire vitreous opacities, but they do develop peripheral neuropathy, nephropathy, and peptic ulcers.
a. In type III FAP, mutant apolipoprotein A1 is the responsible precursor protein.
Familial Exudative Vitreoretinopathy
Autosomal-Dominant Vitreoretinochoroidopathy (ADVIRC; Peripheral Annular Pigmentary Dystrophy of the Retina)
I. ADVIRC clinically shows a stationary or slowly progressive, circumferential (360°), bilateral and symmetric involvement of a coarse, peripheral hyperpigmentation and hypopigmentation of the fundus; a relatively discrete posterior border occurs in the region of the equator.
II. Histologically, disorganization of the peripheral neural retina occurs with focally atrophic retinal pigment epithelium (RPE).
A. Altered RPE cells surround retinal vessels and line the internal limiting membrane.
B. The equatorial neural retina shows an unusual multifocal loss of photoreceptors.
Autosomal-Dominant Neovascular Inflammatory Vitreoretinopathy (ADNIV)
Erosive Vitreoretinopathy
I. Erosive vitreoretinopathy is characterized by pronounced vitreous abnormalities, complicated neural retinal detachments, and a progressive pigmentary retinopathy.
B. Clinically, nyctalopia, progressive visual field loss, marked vitreous syneresis, progressive atrophy of the RPE, and combined traction–rhegmatogenous neural retinal detachments are seen.
2. Electroretinography demonstrates diffuse rod–cone dysfunction.
Knobloch Syndrome
I. Knobloch syndrome is characterized by high myopia, vitreoretinal degeneration, retinal detachment, and a localized defect in the occipital region of the skull.
A. It is inherited as an autosomal recessive disease.
II. Endostatin is absent from the serum.
III. Persistent hyperplastic primary vitreous may be present.
Vitreous Hemorrhage
Definitions
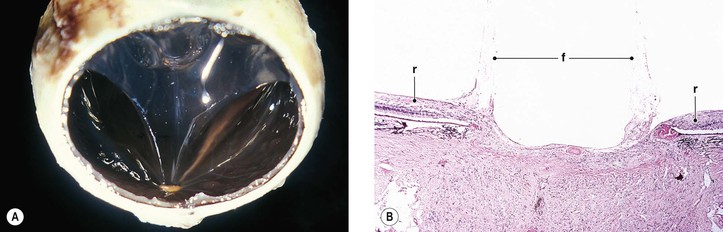
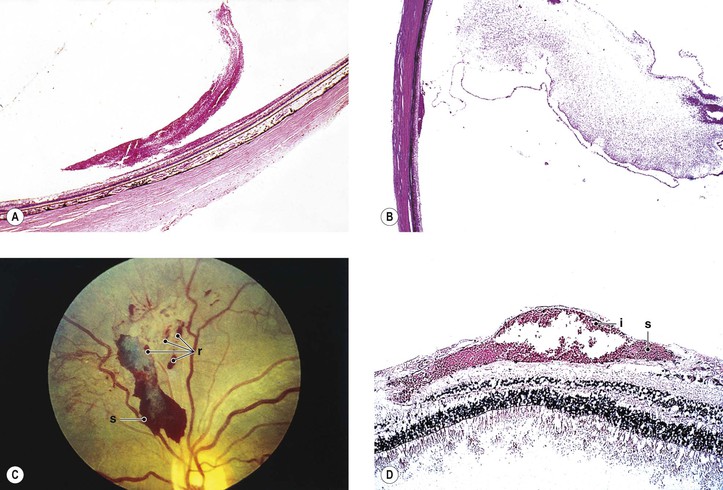
I. Subvitreal hemorrhage (Fig. 12.11)—blood is present between the internal limiting membrane of the neural retina and the posterior “face” of the vitreous and takes weeks to months to clear. This type of hemorrhage is commonly seen in diabetic patients.
II. Intravitreal hemorrhage (Fig. 12.12; see Fig. 12.11)—blood is present in the vitreous body and takes many months to years to clear.
Complications
I. Organization
A. Membranes may lie on the internal surface of the neural retina (i.e., epiretinal) and cause a cellophane retina or fixed retinal folds (see Figs. 11.43–11.45).
B. Many of the delicate epiretinal (on the retinal surface) and preretinal (elevated from the retinal surface) membranes, especially those of the macular and paravascular regions, are believed to form from inward migration and proliferation of the various small glial cells normally present in the nerve fiber and ganglion cell layers.
1. Other cells, such as RPE cells, fibrocytes, and myofibroblasts, can also be found.
2. As the membranes shrink or contract, fixed folds of the retina develop (see Chapter 11).
D. When the membranous process is extensive and associated with a total neural retinal detachment, it is called proliferative vitreoretinopathy (PVR); the older terminologies were massive vitreous retraction and massive periretinal proliferation.
1. PVR may follow perforating trauma, neural retinal detachment, and surgical manipulation.
4. The provariant of p53 codon 72 polymorphism may be a significant risk factor for PVR development.
E. Histologically, glial, fibrous, or RPE membranes, or any combination, are seen on the internal, external, or both surfaces of the retina.
1. T lymphocytes and macrophages may be present in the membranes.
Access the complete reference list online at ![]()