54
Vitiligo and Other Disorders of Hypopigmentation
Introduction/Definitions
• Hypomelanosis: an absence or reduction of melanin in the skin that may be due to any one or a combination of the following:
1. A decrease in the number of melanocytes (e.g. vitiligo).
2. A decrease in melanin synthesis by a normal number of melanocytes (e.g. albinism).
3. A decrease in the transfer of melanin to keratinocytes (e.g. postinflammatory hypopigmentation).
• Amelanosis: total absence of melanin in the skin.
• Depigmentation: usually implies a total loss of skin color (e.g. as in vitiligo).
• Poliosis: a lock of scalp hair, eyebrows, or eyelashes that is white or lighter in color.
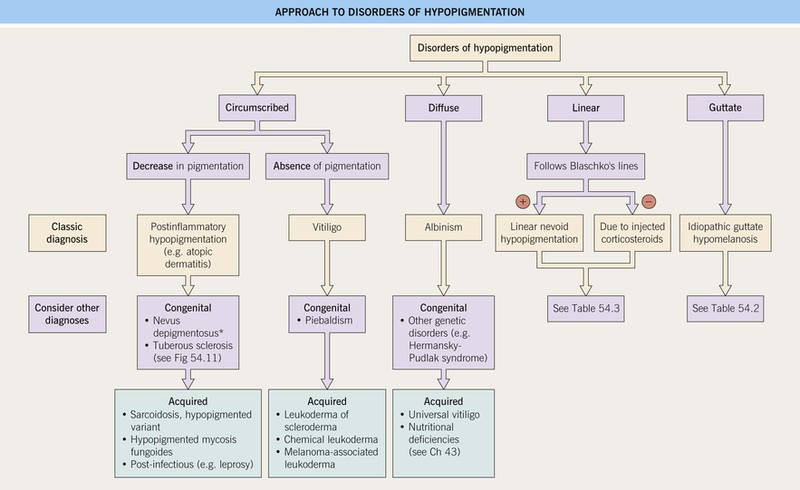
Approach to Disorders of Hypopigmentation
Vitiligo
• An acquired disease, due to autoimmune destruction of melanocytes, that is characterized by circumscribed, amelanotic macules or patches of the skin and mucous membranes (Fig. 54.2); hairs within involved areas may be depigmented or pigmented; the uveal tract and retinal pigmented epithelium can also be affected.


Fig. 54.2 Vitiligo. A Complete loss of pigment of the glans penis. Note the lack of any secondary changes. B Depigmentation of the volar wrists as well as the palmar surfaces; easily recognizable in darkly pigmented individuals. Courtesy, Jean L. Bolognia, MD.
• Two major subtypes of vitiligo: generalized (most common) and localized (Fig. 54.3).
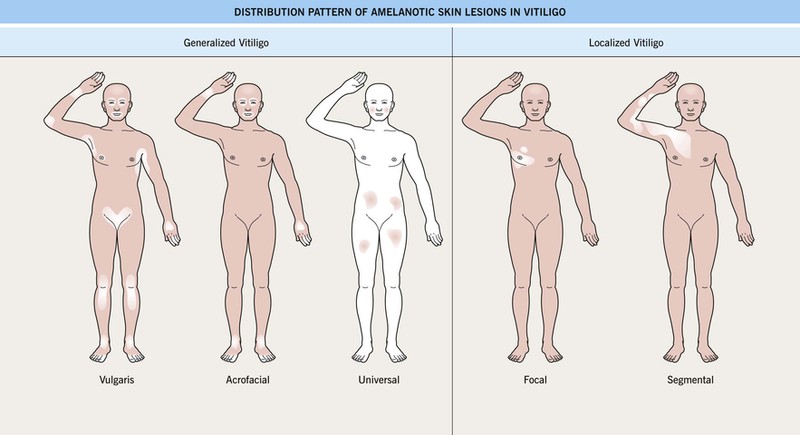
Fig. 54.3 Distribution of amelanotic skin lesions in vitiligo. Vitiligo is clinically divided into two broad categories: generalized and localized. The three distribution patterns in generalized vitiligo include vulgaris, acrofacial, and universal. In focal vitiligo, the amelanotic macules or patches are limited to one or only a few areas, but not necessarily in a segmental pattern, as in segmental vitiligo, which is also unilateral and respects the midline. Adapted with permission from Le Poole C, Boissy RE. Vitiligo. Semin. Cutan. Med. Surg. 1997;16:3–14.
• 10–15% of patients with generalized vitiligo have systemic autoimmune diseases, in particular thyroid disease (Hashimoto’s thyroiditis or Grave’s disease), pernicious anemia, Addison’s disease, and AI-CTD (e.g. SLE); associated cutaneous disorders include halo melanocytic nevi, alopecia areata, and lichen sclerosus.
– Includes acrofacial, vulgaris, and universal (see Fig. 54.3); occasionally an inflammatory edge is seen (Fig. 54.4).

Fig. 54.4 Inflammatory vitiligo. There is a figurate outline to the inflammatory border, which is sometimes misdiagnosed as tinea corporis. Courtesy, Jean-Paul Ortonne, MD.
– Course is unpredictable, but often progressive.
– Usually begins in childhood; typically presents in a unilateral, segmental pattern that respects the midline and usually remains stable in size after 1–2 years (Fig. 54.5).


Fig. 54.5 Segmental vitiligo. A Unilateral band of depigmentation on the face, the most common location for segmental vitiligo. Note the pigmented and depigmented hairs within the affected area. B Under normal light, vitiligo can be subtle in lightly pigmented individuals. The clue to the diagnosis is the poliosis of the eyelashes. A, Courtesy, Kalman Watsky MD; B, Courtesy, Jean L. Bolognia, MD.
– DDx: nevus depigmentosus (decreased but not total loss of pigment).
• DDx of depigmented lesion(s).
• Vitiligo and ocular disease.
• Rx: primarily directed at repigmentation of patient-desired areas (Fig. 54.7).
– The efficacy of treatment depends on four variables.
1. Site: face, neck, mid extremities > acral, mucosal (i.e. sites without hairs).
2. Extent of involvement: small area > large area.
3. Stability: stable > active or progressive.
4. Pigmented hairs within the vitiligo patch: presence > absence.
– Repigmentation usually appears in a perifollicular pattern (Fig. 54.6) and/or from the periphery of lesions.
– 10–20% monobenzyl ether of hydroquinone (MBEH) is sometimes used as depigmentation therapy for widespread or treatment-resistant vitiligo, but it can be permanent and lead to loss of pigment in areas distant to the sites of application.

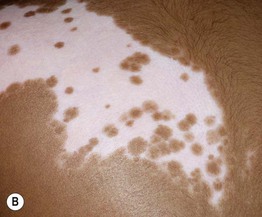
Fig. 54.6 Perifollicular repigmentation. Vitiligo on the elbow (A) and segmental vitiligo on the back (B) responding to PUVA and narrowband UVB therapy, respectively, with repigmentation in a prominent perifollicular pattern as well as from the periphery. The areas of repigmentation are darker in color than the uninvolved skin in (A). A, Courtesy, Jean L. Bolognia, MD; B, Courtesy, Julie V. Schaffer, MD.
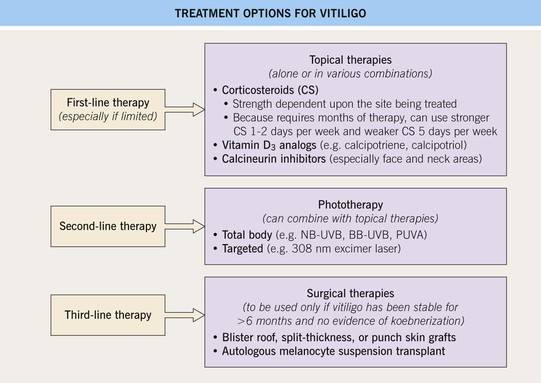
Fig. 54.7 Treatment options for vitiligo. Treatment of vitiligo is directed at repigmentation of patient-desired areas. Camouflage can be offered to all patients for temporary (e.g. makeup, self-tanners) or more permanent (e.g. tattoos) cosmetic relief. Referral to a support group [e.g. National Vitiligo Foundation (www.mynvfi.org)] may also be helpful. 10–20% monobenzyl ether of hydroquinone (MBEH) is sometimes used as depigmentation therapy for widespread or treatment-resistant vitiligo, but it can be permanent and lead to loss of pigment in areas distant to the sites of application. NB-UVB, narrowband ultraviolet B; BB-UVB, broadband UVB; PUVA, psoralens plus ultraviolet A.
Hereditary Hypomelanosis
Oculocutaneous Albinism (OCA)
• Estimated frequency is 1 : 20 000, but may be 1 : 1500 in areas of Africa.
• Four subtypes of OCA (Table 54.1) exist; nearly always inherited in an autosomal recessive manner; OCA1 and OCA2 constitute ~90% of all cases of OCA.
Table 54.1
Classification of oculocutaneous albinism (OCA).
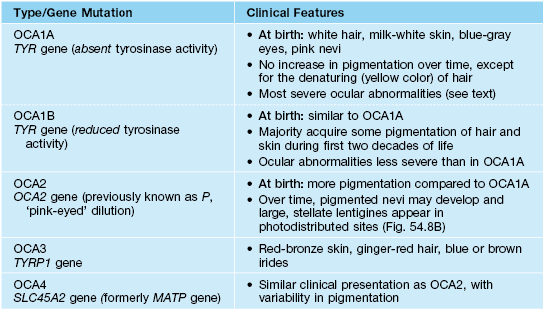
TYR, tyrosinase; OCA, oculocutaneous albinism; TYRP1, tyrosinase-related protein-1; SLC45A2, solute carrier family 45 member 2.
• Early ophthalmologic consultation and strict photoprotection are mandatory; the development of aggressive SCCs (Fig. 54.8A) is a significant cause of morbidity and mortality.
Disorders of Melanocyte Development
Piebaldism
• Presents at birth with poliosis of the mid frontal scalp and stable circumscribed areas of amelanosis in a characteristic distribution pattern, favoring the anterior trunk, mid extremities, and central forehead (Fig. 54.9).


Fig. 54.9 Piebaldism. A White forelock (poliosis) and characteristic triangular amelanotic patch on the mid-forehead. Note the normally pigmented macules of varying sizes within the leukoderma, primarily at the periphery. B Mother and son with the characteristic involvement of the mid-extremities. Note the normally pigmented macules within the leukoderma. A, Courtesy Diane Davidson, MD; B, Courtesy, Jean L. Bolognia, MD.
• Areas of amelanosis contain normally pigmented and hyperpigmented macules and patches within them (see Fig. 54.9); the latter can be seen in uninvolved skin.
• Rx: amenable to autologous skin grafting given its stability.
Waardenburg Syndrome (WS)
• A rare autosomal dominant or recessive disorder characterized by.
– Skin lesions resembling piebaldism, including the white forelock.
– Congenital deafness (10–40%).
– Partial or total heterochromia iridis.
– Medial eyebrow hyperplasia (synophrys).
• Four clinical subtypes have been described.
– WS2: lacks dystopia canthorum (Fig. 54.10).

Fig. 54.10 Waardenburg syndrome type 2. Heterochromia iridis in the absence of dystopia canthorum. The white forelock is seen in the upper left corner. Courtesy, Daniel Albert, MD.
– WS3: associated limb abnormalities.
Disorders of Melanosome Biogenesis
Hermansky–Pudlak Syndrome (HPS)
Disorders of Melanosome Transport and/or Transfer to Keratinocytes
Other
Tuberous Sclerosis (TS) (See Chapter 50)
• Hypomelanotic macules are often the first sign of TS.
• These hypomelanotic macules are typically multiple in number; polygonal is the most common shape, followed by lance-ovate or ‘ash leaf’ (Fig. 54.11); less often, the macules are ‘thumbprint’-like, guttate/confetti, or segmental (see Fig. 54.11; Table 54.2); lesions favor the trunk or extremities.

Fig. 54.11 Tuberous sclerosis. Two types of hypomelanotic macules, lance-ovate (ash leaf) and confetti (idiopathic guttate hypomelanosis-like). Courtesy, David Strobel, MD.
Table 54.2
Differential diagnosis of guttate leukoderma.
The size of the lesions in guttate leukoderma is smaller than in guttate psoriasis. Guttate hypopigmentation may also be seen in the setting of dyschromatoses (see Chapter 55).
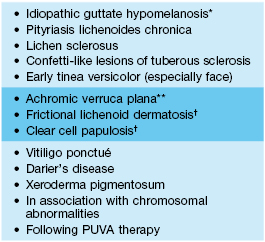
* Seen in adults.
** Minimally elevated flat-topped papules.
† Often papular.
Adapted from Bolognia JL, Shapiro PE. Albinism and other disorders of hypopigmentation. In Arndt KA, et al. (Eds.), Cutaneous Medicine and Surgery. Philadelphia: Saunders, 1995.
Hypopigmentation in Mosaic Patterns
Linear Nevoid Hypopigmentation
• Localized or widespread streaks and swirls of hypopigmentation that follow Blaschko’s lines, which represent pathways of epidermal cell migration during embryogenesis (Fig. 54.12; see Fig. 51.1).

Fig. 54.12 Linear nevoid hypopigmentation. Note the S-shaped pattern of the hypopigmented streaks along Blaschko’s lines.
• ~10–30% of affected individuals have associated extracutaneous abnormalities, which usually develop during infancy and most often affect the CNS (e.g. seizures, developmental delay), eyes, or musculoskeletal system; evaluation is directed by clinical findings.
• DDx: outlined in Table 54.3 (see Fig. 54.14).
Table 54.3
Differential diagnosis of linear hypopigmentation.
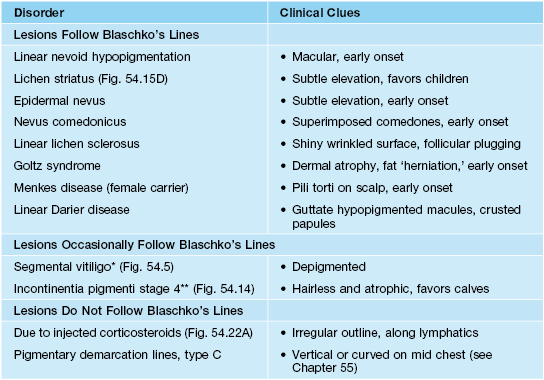
* More often in a unilateral band or block-like configuration.
** Linear streaks typically resemble Chinese characters.

Fig. 54.13 Nevus depigmentosus. Hypomelanotic patch with a decrease, but not absence, of pigmentation. Note how the lesion breaks apart into smaller macules at its periphery, resembling a ‘splash of paint.’
Postinflammatory Hypomelanoses
• Inflammatory skin conditions can potentially result in postinflammatory hypopigmentation or hyperpigmentation or both (see Chapter 55).
• Postinflammatory hypopigmentation is a very common skin disorder that follows a wide variety of dermatoses, most commonly atopic dermatitis, seborrheic dermatitis, and psoriasis, as well as pityriasis lichenoides chronica, lichen striatus, and lichen sclerosus (Fig. 54.15).
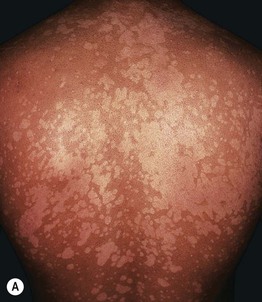




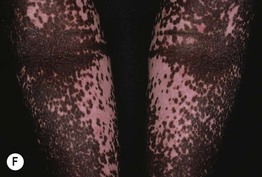


Fig. 54.15 Postinflammatory hypomelanosis. Hypopigmentation secondary to psoriasis (A), seborrheic dermatitis in an infant (B), pityriasis lichenoides chronica (C), lichen striatus (note the flat-topped papules) (D), and hypopigmented mycosis fungoides (E). Complete pigment loss in patients with severe atopic dermatitis (F), discoid lupus erythematosus (G), and neonatal lupus erythematosus (H). B, Courtesy, Jean L. Bolognia, MD. H, Courtesy, Julie V. Schaffer, MD.
• Rx of underlying dermatosis is followed by gradual resolution.
Pityriasis Alba (See Chapter 10)
Sarcoidosis
Hypopigmented Mycosis Fungoides (MF) (See Chapter 98)
• A variant of early stage MF that is most commonly observed in darkly pigmented individuals (see Fig. 54.15E); seen in adults, as well as children and adolescents.
• Atrophy often observed within the hypopigmented patches.
• Histopathology reveals typical features of MF.
• DDx: hypopigmented parapsoriasis, pityriasis lichenoides chronica (PLC).
Cutaneous Lupus Erythematosus (LE) (See Chapter 33)
Systemic Sclerosis (SSc or Generalized Scleroderma) (See Chapter 35)
• Patients with SSc can develop several pigmentary abnormalities, including diffuse hypermelanosis with photoaccentuation, mixed hyper- and hypopigmentation in areas of chronic sclerosis, and a characteristic leukoderma in both sclerotic and nonsclerotic skin (Fig. 54.16).

Fig. 54.16 Leukoderma of scleroderma. Uniform retention of perifollicular pigment within areas of leukoderma. Hyperpigmentation is also seen overlying a superficial vein.
• This ‘leukoderma of scleroderma’ presents as circumscribed areas of depigmentation but with perifollicular and supravenous retention of pigment (see Fig. 54.16).
Lichen Sclerosus (LS) (See Chapter 36)
Infectious and Parasitic Hypomelanosis
Tinea (Pityriasis) Versicolor (See Chapter 64)
• Typically presents symmetrically on the upper trunk and shoulders or flexural areas (e.g. groin and inframammary) as round to oval macules or thin papules that coalesce into patches or thin plaques; the lesions vary in color from pink to light tan to brown, hence the term versicolor (Fig. 54.18).


Fig. 54.18 Tinea (pityriasis) versicolor. A Hypopigmented variant with obvious scale. B Guttate hypopigmented lesions on the cheek; note the classic scaly lesions in the posterior auricular area. B, Courtesy, Julie V. Schaffer, MD.
• Diagnosis is easily confirmed by KOH examination of the associated scale.
• Hypomelanosis without any scaling may remain for months after treatment.
Leprosy (See Chapter 62)
• Tuberculoid leprosy (Fig. 54.19): fewer larger hypopigmented patches with discrete, often raised, borders; favor posterolateral aspects of extremities, back, buttocks, face; associated anhidrosis, alopecia, and loss of sensation.

Fig. 54.19 Tuberculoid leprosy. Large thin hypopigmented plaque on the elbow with a raised light pink border.
• Borderline leprosy: occasionally, ill-defined hypomelanotic macules are seen.
Treponematoses (See Chapters 61 and 69)
Onchocerciasis (River Blindness) (See Chapter 70)
• A later cutaneous finding is leukoderma of the shins with follicular pigmentation, resembling leopard skin (Fig. 54.20).
Melanoma-Associated Leukoderma (See Chapter 93)
• Thought to result from an immune reaction directed against shared antigens on normal and malignant melanocytes (Fig. 54.21).
Chemical Leukoderma
• Contact with a number of chemical agents can lead to hypomelanosis of the skin and hair (Fig. 54.22).


Fig. 54.22 Chemical leukoderma. A Hypopigmentation due to injection of corticosteroids into the anatomic snuff box. The outline is both stellate and linear. Typically appears several weeks to months after the injection. In most cases repigmentation occurs within one year after stopping the injections. B Depigmentation developed at sites of contact with rubber swimming goggles. B, Courtesy, Kalman Watsky, MD.
• Depigmenting compounds have chemical structures that are similar to melanin precursors; they include catechols, phenols, or quinones (e.g. hydroquinone [HQ] or monobenzyl ether of HQ [MBEH]).
• Topical and injected CS can also lead to hypopigmentation (see Fig. 54.22).
Miscellaneous
Idiopathic Guttate Hypomelanosis (IGH)
Progressive Macular Hypomelanosis of the Trunk (PMH)
• Characterized by asymptomatic, poorly defined, small, round to oval, non-scaly, hypopigmented macules and patches, primarily on the trunk and proximal upper extremities, often with confluence of lesions (Fig. 54.24).

Fig. 54.24 Progressive macular hypomelanosis. Note the coalescence of the non-scaly hypopigmented macules on the center of the back. Courtesy, Jean-Paul Ortonne, MD.
• A less common variant is seen in Afro-Caribbean females as larger patches.
Hair Hypomelanosis
For further information see Chs. 65 and 66. From Dermatology, Third Edition.