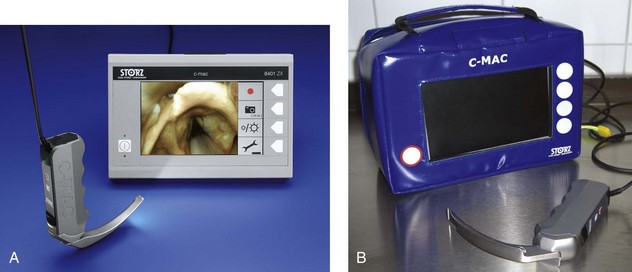
Chapter 25 Video Laryngoscopes
I Introduction
Although the use of video laryngoscopy for teaching the routine laryngoscopic technique of endotracheal intubation and for managing a difficult airway have been known for some years, anesthesiologists have been slow to recognize these advantages. Video-assisted techniques have been successfully used for decades in many surgical disciplines and have largely replaced open approaches in areas such as arthroscopy and laparoscopy (Box 25-1).The magnified and detailed view of the surgical site on a monitor makes it easier to coordinate the work of the surgical team and provides an effective teaching tool for novices. Anesthesiologists have observed this development with interest but without realizing its potential for their own specialty. For years, anesthesiologists have applied video technology almost exclusively for imaging in bronchoscopy and fiberoptic intubation, but the past decade has witnessed some important innovations in the field of video-assisted airway management.
Another principle forms the basis for development of modern video laryngoscopes (VLs). By integrating optical image guides and video cameras into standard laryngoscopes, a magnified and detailed view can be displayed on an external monitor while conventional direct laryngoscopy is performed. Various investigators made an effort to advance this principle and integrated rigid or flexible fiberoptics into laryngoscopes with different shapes, such as the WuScope,1 Bullard,2 and UpsherScope.3 Henthorn and coworkers reported the combination of a flexible fiberoptic cable with a conventional Miller laryngoscope blade,4 which they used for student education. Instructors and trainees found this forerunner of modern VLs to be helpful in identifying the anatomy of the upper airways and successfully performing the intubation.
In 2001, Weiss and associates described a Macintosh laryngoscope, the angulated video-intubation laryngoscope (AVIL), in which a thin fiberoptic cable can be advanced through a guide channel in the laryngoscope handle and blade to a point very close to the blade tip.5 Adapters can be used to connect the fiberoptic cable to an external video unit, enabling a close-up view of the larynx to be displayed on an external monitor. Another option is to introduce the video scope into the endotracheal tube (ETT). However, there have been no other publications on this device from other users, and it apparently has not found wide application.
In 2004, Kaplan and Berci introduced a further improvement of a Macintosh VL, a direct coupled interface VL (DCI, Karl Storz, Tuttlingen, Germany), also known as the VMS or V-MAC.6 The DCI has an integrated camera and connectable blades equipped with a fiberoptic light and image guide, and the handle and blade are combined in a fixed unit.
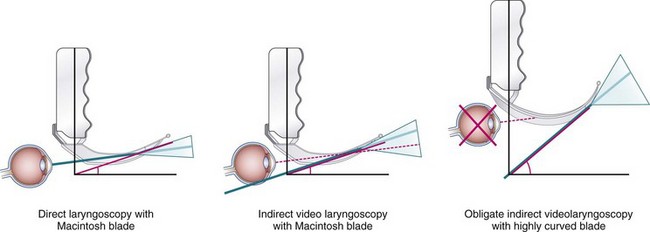
Miniaturization of camera chip technology; improved, rechargeable battery power and light output; and affordable, small liquid crystal display (LCD) monitors made video laryngoscopy a booming technology, which led to the introduction of different types of VLs. Because VLs have different shapes, technical equipment, and applications, further classification of these devices is justified.7 The main difference in VLs arises from the type of blade that is incorporated into the system. VLs that are based on a conventional, established blade shape, such as the Macintosh blade, have the option of visualizing the glottic entrance by direct laryngoscopy. Users are familiar with the handling of this blade type. Other VLs are designed with highly curved or angled blades that pass around the tongue and allow a “look around the corner” to the glottic opening. These VLs allow the best visualization of the glottis, although a direct view of the glottic entrance usually is impossible (i.e., obligatory indirect visualization). Because of the high degree of blade angulation, they must be used with a malleable or rigid styletted tube in most cases.
II Video Laryngoscopes Using Macintosh-Based Blades
A A.P. Advance
3 Clinical Experience
No clinical experience has been published for the A.P. Advance, but in two mannequin studies, medical professionals used it in normal and difficult airway scenarios and reported good visualization and intubation success.8,9 In another mannequin study, paramedics who had not previously used video laryngoscopy achieved earlier intubation and fewer unplanned advances of the tube compared with use of the GlideScope Ranger.10
B Direct Coupled Interface (DCI) Video Laryngoscope System
1 Description
The DCI video laryngoscope was designed using a modified Macintosh blade with the same curvature as the original 1943 version and a laryngoscope handle. The batteries in the handle are replaced with a small video camera (i.e., DCI camera) and a combined image-light bundle that inserts into the Macintosh blade.6 The DCI video laryngoscope system allows interchange of different devices, such as laryngoscopes (e.g., Macintosh, Dörges, Miller, D-Blade) and rigid (e.g., Bonfils intubation endoscope) and flexible fiberscopes (Fig. 25-1); however, mobility of the fiberoptic-based system is limited. The DCI system has been displaced by the mobile C-MAC video intubation system.
3 Clinical Experience
Kaplan and associates reported a series of 235 patients in whom they used the DCI video laryngoscope system.6 Of these cases, 217 were predicted to be straightforward, and in all but one, the DCI video laryngoscope system was successfully used, with 10% requiring external laryngeal manipulation. A second group of 18 patients had anatomic predictors of difficult laryngoscopy; all in this group required external laryngeal manipulation but were successfully intubated with the DCI video laryngoscope system. In another study, Kaplan and colleagues compared the view obtained using DCI by direct vision with that obtained on the monitor and found that the image on the monitor was the same as or better than the direct line-of-sight view in most patients undergoing routine anesthesia.11 Hagberg and colleagues describe the successful use in a patient who previously had an unexpected difficult laryngoscopy and impossible intubation and who was subsequently intubated with the DCI system after the first attempt.12
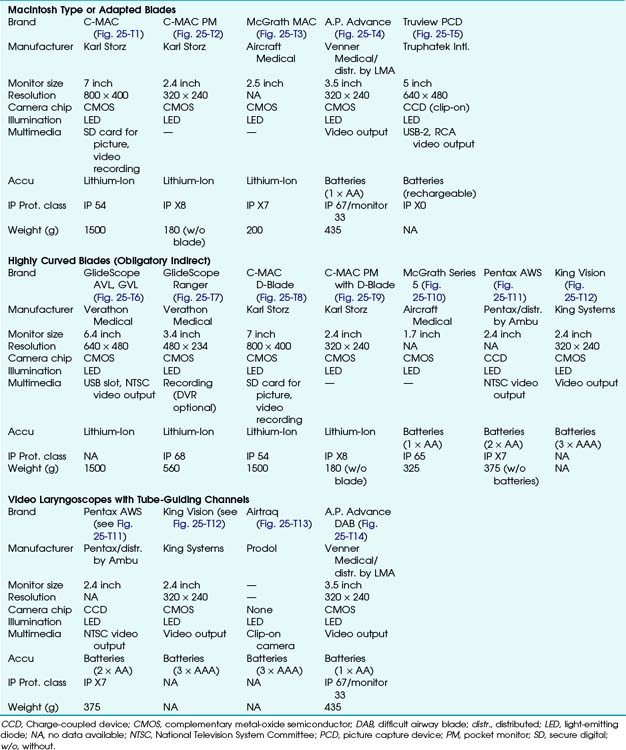
C C-MAC Video Laryngoscope System
1 Description
The C-MAC (Karl Storz, Tuttlingen, Germany) video laryngoscope system is a modification of the Storz DCI system. The C-MAC VL can provide a useful alternative during routine induction of general anesthesia and in securing a difficult airway. The C-MAC is based on a modified Macintosh blade that has the same curvature as the original 1943 version,13 but it is different from the original Macintosh blade in its thinner profile (maximum of 14 mm) and its beveled shoulder, which reduces the risk of oral and dental injury and facilitates insertion in patients with limited mouth opening. Optionally, the blade may be equipped with a guide channel for introducing a suction catheter to help maintain a clear visual field during laryngoscopy. The C-MAC system is compatible with various blades. The electronic module (E-module) fits into the blade handle and allows a rapid exchange of Macintosh stainless steel blade sizes 2, 3, and 4, Miller sizes 0 and 1, and the D-Blade. A clip-on camera (C-CAM) can link the C-MAC system with rigid or flexible fiberoptics. The combined optical system of the C-MAC consists of a complementary metal-oxide semiconductor (CMOS) chip set (320 × 240 pixels), an optical lens with an aperture angle of 80 degrees, and a high-power, light-emitting diode (LED) at the distal third of the blade with effective antifogging properties. The blade handle with the E-module and the external, 7-inch LCD color monitor have push buttons that allow the operator to capture images from the screen and record video sequences, which are storable on standard SD memory cards, which have a 2-GB capacity. In the rare case that visualization of the glottic opening is still difficult, the D-Blade may be attached to the system within seconds. The higher curvature of the D-Blade allows a better look around the corner, and the low blade profile may permit use even in patients with limited mouth opening (e.g., 15 mm); however, direct laryngoscopy is not possible in most cases.
3 Clinical Experience
Several investigators showed superior visualization of the glottis with the C-MAC compared with conventional direct laryngoscopy.14–17 Even if the application of a stylet cannot be eliminated completely, most intubations using a C-MAC VL can be performed without stylet use.18,19 In a preliminary study by Cavus and associates of patients in whom conventional Macintosh laryngoscopy failed, use of the C-MAC D-Blade provided better glottic visualization and intubation success in all patients.20 An observational study of 80 patients with the need for out-of-hospital emergency intubation (e.g. trauma, cardiopulmonary resuscitation) performed by physicians showed good handling and intubation success with the C-MAC VL. In a few cases, video laryngoscopic intubation was impossible due to VL problems such as bright surrounding light, and only direct laryngoscopy with the same device resulted in fast, successful intubation.17
F Truview Picture Capture Device
3 Clinical Experience
The glottic view may be improved by use of the Truview compared with conventional laryngoscopy with a Macintosh blade, and this may result in a higher intubation success rate in difficult-to-manage airways.22–25 Compared with conventional laryngoscopy with a Macintosh laryngoscope, intubation with the Truview may take more time, but intubation success rates may be comparable; however, rates of airway morbidity related to laryngoscopy may be lower.23 In a study by Carlino and colleagues using the Truview as a teaching tool for anesthesiology residents, intubation success after the first attempt was almost doubled compared with that for conventional Macintosh laryngoscopy.26 In patients with cervical spine immobilization, Malik and colleagues experienced inferior visualization and intubation compared with other VLs. The handling may be cumbersome, and fogging may impair visualization process.22
III Video Laryngoscopes Using Highly Curved Blades
High curvature of the blade typically makes it impossible to perform direct laryngoscopy; tracheal intubation requires indirect visualization. To follow the high curvature of the blade with an ETT, a tube guide or malleable stylet is necessary.18,19 Although there is a tendency to focus on the video monitor, it is important to directly visualize the tube going into the mouth and advancing beyond the tongue before it becomes visible on the monitor. Perforations of the pharynx and hypopharynx have occurred with the GlideScope and the McGrath when operators have blindly inserted styletted tubes while focusing only on the video monitor.27,28 Highly curved, indirect VLs can be used with almost no forces applied to tongue and pharyngeal structures, and these devices can be used in awake video laryngoscopic intubation as an alternative to awake fiberoptic intubation, assuming that attention is paid to possible contraindications for video laryngoscopy (e.g., mouth opening <15 mm, subglottic stenosis, tumor masses). Several case reports describe safe application of this technique.29–35
A GlideScope
2 Instrument Use
Preparation for use of the GlideScope is limited to ensuring that the power is connected and turned on. After the instrument has been on for a few minutes, no additional defogging maneuver is needed. A styletted ETT is needed with distal curvature of 60 to 90 degrees to aid access to the glottic opening (i.e., “hockey-stick” formation). The blade is inserted as done with a Macintosh blade, although in this indirect technique, the blade tip does not need to be advanced to the vallecula, and a lift does not need to be performed to the same extent as with a conventional Macintosh blade. When the best view of the glottis is achieved on the video monitor with or without external laryngeal manipulation, the ETT is advanced alongside and posterior to the blade. Because advancement of the styletted tube cannot directly be observed due to the blade curvature, caution is needed during advancement of the tube to avoid injury of pharyngeal structures.27,36–38 Intubation can be achieved by positioning the ETT at the glottic opening and then advancing it off the stylet through the cords. If tube passage is difficult, relaxation of any upward tongue lift should be attempted; alternatively, backing away slightly from the laryngeal inlet with the scope may help. Good visualization of the process should be available throughout on the monitor.
3 Clinical Experience
The GlideScope is the prototype of modern obligate indirect VLs. Since its introduction in 2001, it has been studied in the operating room,39–43 used in normal and difficult intubation scenarios,38,44–49 and compared with other VLs.16,18,22,50–55 In most patients, use of the GlideScope resulted in improved glottic visualization according to the Cormack-Lehane classification,56 and it has provided successful intubation of difficult airways.48,57 Aziz and colleagues analyzed 2004 GlideScope intubations and reported an overall intubation success rate of 97%. However, 3% could not be intubated with the GlideScope, and the investigators concluded that maintenance of competency with alternative methods of intubation was mandatory.38 Intubation difficulties have changed from impaired visualization to difficult tube advancement. Despite optimal glottic visualization, the most difficult part of indirect video laryngoscopy is placing the curved tube in the glottic entrance and advancing it into the trachea.58
Use of the portable GlideScope Ranger has been studied predominantly in out-of-hospital settings and in emergency departments.59–62 GlideScope Ranger use in an emergency setting improved glottic visualization and reduced the number of intubation attempts compared with conventional laryngoscopy.57,63 However, Choi and colleagues reported some cases of unsuccessful intubation despite excellent visualization, which highlights the need for training on the device outside of emergency situations.64
B McGrath Series 5
3 Clinical Experience
Most clinical data show improved visualization and intubation success compared with conventional laryngoscopy with the Macintosh and Henderson straight blades.65–68 Similar to the GlideScope, advancement of the styletted tube cannot directly be observed because of the blade’s shape, and caution is needed during advancement of the tube to avoid injuries.28
IV Video Laryngoscopes with Tube-Guiding Channels
B Pentax Airway Scope AWS-S100
3 Clinical Experience
Because of the high angulation of the blade, the AWS has shown superior glottic visualization and intubation success compared with conventional laryngoscopy in patients with immobilization of the cervical spine.22,69 In contrast, in a study of morbidly obese patients, Abdallah and colleagues showed faster intubation and higher first-pass success rates with a conventional Macintosh size 4 blade compared with the Pentax-AWS, despite inferior glottic visualization.70 Several case reports describe the Pentax AWS VL for successful intubation of awake, spontaneously breathing patients.31–33
In morbidly obese patients, the relatively bulky design may cause difficulties during insertion in the mouth.71 Problems with the guiding channel may arise if the cervical spine has a fixed rotation72 or if otherwise the tube may not be redirected from the channel.73 In principle, these problems may arise with all channeled-blade VLs.
C Airtraq
3 Clinical Experience
Compared with conventional Macintosh laryngoscopy, the Airtraq has demonstrated promising results in patients at low or higher risk for difficult tracheal intubation and in patients with immobilization of the cervical spine.74–76 McElwain and colleagues found that the Airtraq laryngoscope performed better than the C-MAC (with a Macintosh blade) and conventional Macintosh laryngoscopes in patients undergoing tracheal intubation with manual in-line stabilization of the cervical spine.77 However, Trimmel and colleagues showed that the Airtraq laryngoscope had no benefit over conventional direct laryngoscopy in the prehospital setting if used by untrained physicians, and they could not recommend it in the prehospital setting without significant clinical experience obtained in the operation room.78
V Fields of Application
Video laryngoscopy has many nontraditional but useful applications in anesthesiology (Table 25-1). Suitable devices should be available when anesthesia is administered, and all airway practitioners should be skilled in their use. Although VLs can provide important savings in time and decreased patient morbidity, equipment cannot substitute for clinical proficiency, and traditional intubation skills should be maintained.
VI Difficult Airway
At one time, the use of video laryngoscopy for managing the unexpected difficult airway was limited by restricted mobility and extended preparation time. This is no longer the case because current VLs are mobile and quick to set up. Serocki and colleagues found that video laryngoscopy was helpful in many clinical conditions with an expected difficult airway, including limited neck mobility, reduced thyromental distance, reduced inter-incisor distance, and retrognathia.48 Their data confirmed that the DCI VL with a Macintosh blade and the GlideScope enhanced glottic visualization in patients with difficult conventional laryngoscopy.
Video laryngoscopy cannot replace awake fiberoptic intubation in many cases of predictable difficult airway. Nonetheless, in an expected difficult airway, video laryngoscopy may be a worthy addition as an awake intubation technique.32,34,79 Although the American Society of Anesthesiologists (ASA) difficult airway guidelines highlight the approach of awake intubation as the preferred method to manage expected difficult airways, video laryngoscopy under general anesthesia should be considered for intubation if difficulty with intubation, but not mask ventilation, is expected.80 Video laryngoscopy has successfully been applied for the management of the difficult airway in otonasolaryngologic and maxillofacial surgery,48 neurosurgery,81 obstetrics,82 traumatology, pediatrics,83 the intensive care unit,84 the emergency department,64 and in physician-based, out-of-hospital emergency medicine.17
VL systems may be advantageous over direct laryngoscopy for the exchange of one airway device for another. A case report demonstrated the use of video laryngoscopy to exchange a Combitube, which was placed by paramedics after failed direct vision intubation, for an ETT to establish a definitive airway.12 It is not unusual for a supraglottic airway device, such as a Laryngeal Tube or Combitube, to be placed in the prehospital setting when direct laryngoscopy is unsuccessful and the patient’s airway is difficult; exchanging this device for an ETT may be demanding. Anesthesiologists use VLs in routine cases without any suspicion of difficult airway management or before any attempt of direct laryngoscopy is performed, because VLs are simple to use and have a high rate of intubation success.
VLs have the advantage in the unanticipated situation because their rigidity facilitates rapid control of the position of the laryngoscope tip, and they can be ready for immediate use. These devices allow retraction of soft tissues so that there is a line of sight from the lens to the distal structures, without the necessity of aligning the oral and laryngotracheal axes with the naked eye. Even with a Macintosh VL that is used in the traditional Macintosh fashion (i.e., tip of blade in vallecula), the epiglottis may be directly elevated; the straight-blade technique offers improved viewing. This type of positioning is often performed for difficult airways. In a study of 60 patients by Cavus and associates,15 a size 4 rather than a size 3 C-MAC blade was used in three patients with unexpected intubation difficulties. The Macintosh size 4 blade is more curved than the size 3, resulting in a higher angulation with a wider view of the glottis. In all three of these patients, the Cormack-Lehane score improved by two classes using this technique. Some practitioners position the tip over the dorsum of the tongue, proximal to the epiglottis, achieving indirect elevation of the epiglottis without conventional tensioning of the hyoepiglottic ligament.
Because of their optics, these devices allow the operator to visualize structures that may not be seen with the direct line-of-sight view available to the naked eye. When glottic visualization is difficult despite the use of a Macintosh-based VL, an obligate indirect VL such as the GlideScope or the C-MAC D-Blade may be used.20,39 A direct view on the glottis is impossible with an obligate indirect VL in most patients. If secretions (e.g., blood, vomit), surrounding light, and battery failure impede the glottic view on the monitor, direct glottic visualization can be an important fall-back strategy.17
It may be advantageous to use a system in which different types of blades can be changed with minimal delay, such as C-MAC system or A.P. Advance.9 In a stepwise approach, airway management can be changed from direct laryngoscopy by video laryngoscopy with a Macintosh blade to obligate indirect video laryngoscopy with a more highly curved blade (Fig. 25-2). Most VLs provide an output socket to an external monitor. Some offer video capture capabilities to record airway procedures for educational or documentation purposes (e.g., C-MAC, GlideScope). Control buttons are located on the handle or the monitor for recording videos and captured images.
VII Teaching
VLs based on Macintosh blades offer the possibility for conventional direct laryngoscopy attempts by the trainee, and at the same time, the faculty member is able to analyze the airway on the monitor and make better-informed decisions about the prudence of allowing the trainee to continue. A study using video laryngoscopy to provide feedback for instructor showed that the student’s success of intubation is increased and the rate of esophageal intubations was markedly decreased compared with instructor assistance based on standard cues.85 In the absence of a VL system, the faculty member is more likely to take over the procedure earlier if a problem is encountered, reducing the experience afforded to the trainee.
VIII Documentation
VLs with external monitors can record and save video sequences and image captures from the screen. Video recordings of professional laryngoscopic attempts can be educational, and recordings of intubation attempts by students can be used as a teaching tool. Airway pathologies such as edema of the glottic opening and erythema after a burn injury can be documented. In newborns, the enlarged panoramic view and recordings of video laryngoscopy have assisted in correctly diagnosing vocal cord paralysis.83
Direct visualization of tube insertion with video recording can confirm correct tube placement and can detect esophageally misplaced ETTs quickly. Use of video laryngoscopy for routine intubations in the operating room, intensive care unit, emergency department, and prehospital emergency settings can increase intubation success rates and reduce the incidence of critical situations in airway management.86
X Clinical Pearls
• The main indication for video laryngoscopy is an unpredicted difficult intubation.
• If oxygenation of the patient can be ensured (e.g., by bag-mask ventilation), video laryngoscopy may be considered for some cases of predicted difficult intubation.
• Video laryngoscopes (VLs) have different technical requirements and handling conditions. Training with each device in elective situations is mandatory before use in airway emergencies.
• VLs with highly curved blades provide obligate indirect glottic visualization. In most cases, a tube stylet must be used. Despite optimal visualization of the glottic entrance, tube advancement into the trachea may be difficult due to the steep angle of the styletted, curved tube.
• VLs with Macintosh-type blades provide direct and indirect glottic views. The option of direct visualization may be particularly important in airway emergencies outside of the hospital.
• Ideally, VLs are available to cover a broad range of applications in patients of different ages and sizes (e.g., newborns, obese patients).
• Reusable, stainless steel blades have lower blade profiles, but disposable blades also should be available for hygienic reasons. Disposable blades are mandatory in some countries.
• Video laryngoscopy allows for image capture and video documentation that may be useful in a variety of settings (e.g., oropharyngeal pathologies, correct tube placement).
• Video laryngoscopy may be used for awake orotracheal intubation, but awake fiberoptic intubation remains the gold standard for patients with a predicted difficult airway, and skill in performing fiberoptic intubation must be maintained.
• Because VLs, especially those with interchangeable blades for direct laryngoscopy and obligate indirect laryngoscopy, aid education in conventional laryngoscopy and reduce patient morbidity, they may become the standard for routine intubation in the operating room, intensive care unit, emergency department, and prehospital emergency settings.
All references can be found online at expertconsult.com.
11 Kaplan MB, Hagberg CA, Ward DS, et al. Comparison of direct and video-assisted views of the larynx during routine intubation. J Clin Anesth. 2006;18:357–362.
15 Cavus E, Kieckhaefer J, Doerges V, et al. The C-MAC videolaryngoscope: First experiences with a new device for videolaryngoscopy-guided intubation. Anesth Analg. 2010;110:473–477.
18 Maassen R, Lee R, Hermans B, et al. A comparison of three videolaryngoscopes: The Macintosh laryngoscope blade reduces, but does not replace, routine stylet use for intubation in morbidly obese patients. Anesth Analg. 2009;109:1560–1565.
34 Doyle DJ. Awake intubation using the GlideScope video laryngoscope: Initial experience in four cases. Can J Anaesth. 2004;51:520–521.
38 Aziz MF, Healy D, Kheterpal S, et al. Routine clinical practice effectiveness of the GlideScope in difficult airway management: an analysis of 2,004 GlideScope intubations, complications, and failures from two institutions. Anesthesiology. 2011;114:34–41.
39 Cooper RM, Pacey JA, Bishop MJ, et al. Early clinical experience with a new videolaryngoscope (GlideScope) in 728 patients. Can J Anaesth. 2005;52:191–198.
58 Levitan RM, Heitz JW, Sweeney M, et al. The complexities of tracheal intubation with direct laryngoscopy and alternative intubation devices. Ann Emerg Med. 2011;57:240–247.
64 Choi HJ, Kang HG, Lim TH, et al. Endotracheal intubation using a GlideScope video laryngoscope by emergency physicians: A multicentre analysis of 345 attempts in adult patients. Emerg Med J. 2010;27:380–382.
73 Asai T, Liu EH, Matsumoto S, et al. Use of the Pentax-AWS in 293 patients with difficult airways. Anesthesiology. 2009;110:898–904.
85 Howard-Quijano KJ, Huang YM, Matevosian R, et al. Video-assisted instruction improves the success rate for tracheal intubation by novices. Br J Anaesth. 2008;101:568–572.
1 Wu TL, Chou HC. A new laryngoscope: The combination intubating device. Anesthesiology. 1994;81:1085–1087.
2 Borland LM, Casselbrant M. The Bullard laryngoscope: A new indirect oral laryngoscope (pediatric version). Anesth Analg. 1990;70:105–108.
3 Pearce AC, Shaw S, Macklin S. Evaluation of the Upsherscope: A new rigid fibrescope. Anaesthesia. 1996;51:561–564.
4 Henthorn RW, Reed J, Szafranski JS, Ganta R. Combining the fiberoptic bronchoscope with a laryngoscope blade aids teaching direct laryngoscopy. Anesth Analg. 1995;80:433.
5 Weiss M, Hartmann K, Fischer JE, Gerber AC. Use of angulated video-intubation laryngoscope in children undergoing manual in-line neck stabilization. Br J Anaesth. 2001;87:453–458.
6 Kaplan MB, Ward DS, Berci G. A new video laryngoscope: An aid to intubation and teaching. J Clin Anesth. 2002;14:620–626.
7 Cavus E, Bein B, Doerges V. Airway management: Video-assisted airway management [in German]. Anasthesiol Intensivmed Notfallmed Schmerzther. 2011;46:588–596.
8 Burdett E, Ross-Anderson DJ, Makepeace J, et al. Randomized controlled trial of the A.P. Advance, McGrath, and Macintosh laryngoscopes in normal and difficult intubation scenarios: A manikin study. Br J Anaesth. 2011;107:983–988.
9 Hodd JA, Doyle DJ, Gupta S, et al. A mannequin study of intubation with the AP Advance and GlideScope Ranger videolaryngoscopes and the Macintosh laryngoscope. Anesth Analg. 2011;113:791–800.
10 Butchart AG, Tjen C, Garg A, Young P. Paramedic laryngoscopy in the simulated difficult airway: Comparison of the Venner A.P. Advance and GlideScope Ranger video laryngoscopes. Acad Emerg Med. 2011;18:692–698.
11 Kaplan MB, Hagberg CA, Ward DS, et al. Comparison of direct and video-assisted views of the larynx during routine intubation. J Clin Anesth. 2006;18:357–362.
12 Hagberg CA, Vogt-Harenkamp CC, Iannucci DG. Successful airway management of a patient with a known difficult airway with the Direct Coupler Interface Video Laryngoscope. J Clin Anesth. 2007;19:629–631.
13 Macintosh RR. A new laryngoscope. Lancet. 1943;1:205.
14 Byhahn C, Iber T, Zacharowski K, et al. Tracheal intubation using the mobile C-MAC video laryngoscope or direct laryngoscopy for patients with a simulated difficult airway. Minerva Anestesiol. 2010;76:577–583.
15 Cavus E, Kieckhaefer J, Doerges V, et al. The C-MAC videolaryngoscope: First experiences with a new device for videolaryngoscopy-guided intubation. Anesth Analg. 2010;110:473–477.
16 Teoh WH, Saxena S, Shah MK, Sia AT. Comparison of three videolaryngoscopes: Pentax Airway Scope, C-MAC, GlideScope vs the Macintosh laryngoscope for tracheal intubation. Anaesthesia. 2010;65:1126–1132.
17 Cavus E, Callies A, Doerges V, et al. The C-MAC videolaryngoscope for prehospital emergency intubation: A prospective, multicentre, observational study. Emerg Med J. 2011;28:650–653.
18 Maassen R, Lee R, Hermans B, et al. A comparison of three videolaryngoscopes: The Macintosh laryngoscope blade reduces, but does not replace, routine stylet use for intubation in morbidly obese patients. Anesth Analg. 2009;109:1560–1565.
19 van Zundert A, Maassen R, Lee R, et al. A Macintosh laryngoscope blade for videolaryngoscopy reduces stylet use in patients with normal airways. Anesth Analg. 2009;109:825–831.
20 Cavus E, Neumann T, Doerges V, et al. First clinical evaluation of the C-MAC D-Blade videolaryngoscope during routine and difficult intubation. Anesth Analg. 2011;112:382–385.
21 Purugganan RV, Jackson TA, Heir JS, et al. Video laryngoscopy versus direct laryngoscopy for double-lumen endotracheal tube intubation: A retrospective analysis. J Cardiothorac Vasc Anesth. 2012 Feb 21. [Epub ahead of print]
22 Malik MA, Maharaj CH, Harte BH, Laffey JG. Comparison of Macintosh, Truview EVO2, GlideScope, and Airwayscope laryngoscope use in patients with cervical spine immobilization. Br J Anaesth. 2008;101:723–730.
23 Barak M, Philipchuck P, Abecassis P, Katz Y. A comparison of the Truview blade with the Macintosh blade in adult patients. Anaesthesia. 2007;62:827–831.
24 Li JB, Xiong YC, Wang XL, et al. An evaluation of the TruView EVO2 laryngoscope. Anaesthesia. 2007;62:940–943.
25 Matsumoto S, Asai T, Shingu K. Truview video laryngoscope in patients with difficult airways. Anesth Analg. 2006;103:492–493.
26 Carlino C, Pastore JC, Battistini GM, et al. Training resident anesthesiologists in adult challenging intubation comparing Truview EVO2 and Macintosh laryngoscope: A preliminary study. Minerva Anestesiol. 2009;75:563–567.
27 Cooper RM. Complications associated with the use of the GlideScope videolaryngoscope. Can J Anaesth. 2007;54:54–57.
28 Williams D, Ball DR. Palatal perforation associated with McGrath videolaryngoscope. Anaesthesia. 2009;64:1144–1145.
29 Uslu B, Damgaard Nielsen R, Kristensen BB. McGrath videolaryngoscope for awake tracheal intubation in a patient with severe ankylosing spondylitis. Br J Anaesth. 2010;104:118–119.
30 Thong SY, Shridhar IU, Beevee S. Evaluation of the airway in awake subjects with the McGrath videolaryngoscope. Anaesth Intensive Care. 2009;37:497–498.
31 Suzuki A, Terao M, Aizawa K, et al. Pentax-AWS Airway Scope as an alternative for awake flexible fiberoptic intubation of a morbidly obese patient in the semi-sitting position. J Anesth. 2009;23:162–163.
32 Asai T. Pentax-AWS videolaryngoscope for awake nasal intubation in patients with unstable necks. Br J Anaesth. 2010;104:108–111.
33 Jeyadoss J, Nanjappa N, Nemeth D. Awake intubation using Pentax AWS videolaryngoscope after failed fibreoptic intubation in a morbidly obese patient with a massive thyroid tumour and tracheal compression. Anaesth Intensive Care. 2011;39:311–312.
34 Doyle DJ. Awake intubation using the GlideScope video laryngoscope: Initial experience in four cases. Can J Anaesth. 2004;51:520–521.
35 Jones PM, Harle CC. Avoiding awake intubation by performing awake GlideScope laryngoscopy in the preoperative holding area. Can J Anaesth. 2006;53:1264–1265.
36 Hirabayashi Y. Pharyngeal injury related to GlideScope videolaryngoscope. Otolaryngol Head Neck Surg. 2007;137:175–176.
37 Hsu WT, Hsu SC, Lee YL, et al. Penetrating injury of the soft palate during GlideScope intubation. Anesth Analg. 2007;104:1609–1610. discussion 1611
38 Aziz MF, Healy D, Kheterpal S, et al. Routine clinical practice effectiveness of the GlideScope in difficult airway management: An analysis of 2,004 GlideScope intubations, complications, and failures from two institutions. Anesthesiology. 2011;114:34–41.
39 Cooper RM, Pacey JA, Bishop MJ, McCluskey SA. Early clinical experience with a new videolaryngoscope (GlideScope) in 728 patients. Can J Anaesth. 2005;52:191–198.
40 Rai MR, Dering A, Verghese C. The GlideScope system: A clinical assessment of performance. Anaesthesia. 2005;60:60–64.
41 Sun DA, Warriner CB, Parsons DG, et al. The GlideScope Video Laryngoscope: Randomized clinical trial in 200 patients. Br J Anaesth. 2005;94:381–384.
42 Teoh WH, Shah MK, Sia AT. Randomised comparison of Pentax AirwayScope and GlideScope for tracheal intubation in patients with normal airway anatomy. Anaesthesia. 2009;64:1125–1129.
43 Jones PM, Turkstra TP, Armstrong KP, et al. Comparison of a single-use GlideScope Cobalt videolaryngoscope with a conventional GlideScope for orotracheal intubation. Can J Anaesth. 2010;57:18–23.
44 Agro F, Barzoi G, Montecchia F. Tracheal intubation using a Macintosh laryngoscope or a GlideScope in 15 patients with cervical spine immobilization. Br J Anaesth. 2003;90:705–706.
45 Lim Y, Yeo SW. A comparison of the GlideScope with the Macintosh laryngoscope for tracheal intubation in patients with simulated difficult airway. Anaesth Intensive Care. 2005;33:243–247.
46 Turkstra TP, Craen RA, Pelz DM, Gelb AW. Cervical spine motion: A fluoroscopic comparison during intubation with lighted stylet, GlideScope, and Macintosh laryngoscope. Anesth Analg. 2005;101:910–915.
47 Malik MA, Subramaniam R, Maharaj CH, et al. Randomized controlled trial of the Pentax AWS, GlideScope, and Macintosh laryngoscopes in predicted difficult intubation. Br J Anaesth. 2009;103:761–768.
48 Serocki G, Bein B, Scholz J, Dorges V. Management of the predicted difficult airway: a comparison of conventional blade laryngoscopy with video-assisted blade laryngoscopy and the GlideScope. Eur J Anaesthesiol. 2010;27:24–30.
49 Armstrong J, John J, Karsli C. A comparison between the GlideScope Video Laryngoscope and direct laryngoscope in paediatric patients with difficult airways: A pilot study. Anaesthesia. 2010;65:353–357.
50 Savoldelli GL, Schiffer E, Abegg C, et al. Comparison of the GlideScope, the McGrath, the Airtraq and the Macintosh laryngoscopes in simulated difficult airways. Anaesthesia. 2008;63:1358–1364.
51 McElwain J, Malik MA, Harte BH, et al. Comparison of the C-MAC videolaryngoscope with the Macintosh, GlideScope, and Airtraq laryngoscopes in easy and difficult laryngoscopy scenarios in manikins. Anaesthesia. 2010;65:483–489.
52 Powell L, Andrzejowski J, Taylor R, Turnbull D. Comparison of the performance of four laryngoscopes in a high-fidelity simulator using normal and difficult airway. Br J Anaesth. 2009;103:755–760.
53 Maassen R, van Zundert A. Comparison of the C-MAC videolaryngoscope with the Macintosh, GlideScope and Airtraq laryngoscopes in easy and difficult laryngoscopy scenarios in manikins. Anaesthesia. 2010;65:955. author reply 956
54 Jeon WJ, Kim KH, Yeom JH, et al. A comparison of the GlideScope(R) to the McGrath(R) videolaryngoscope in patients. Korean J Anesthesiol. 2011;61:19–23.
55 Piepho T, Weinert K, Heid FM, et al. Comparison of the McGrath(R) Series 5 and GlideScope(R) Ranger with the Macintosh laryngoscope by paramedics. Scand J Trauma Resusc Emerg Med. 2011;19:4.
56 Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia. 1984;39:1105–1111.
57 Griesdale DE, Liu D, McKinney J, Choi PT. GlideScope((R)) video-laryngoscopy versus direct laryngoscopy for endotracheal intubation: A systematic review and meta-analysis. Can J Anaesth. 2011;59:41–52.
58 Levitan RM, Heitz JW, Sweeney M, Cooper RM. The complexities of tracheal intubation with direct laryngoscopy and alternative intubation devices. Ann Emerg Med. 2011;57:240–247.
59 Lim HC, Goh SH. Utilization of a GlideScope videolaryngoscope for orotracheal intubations in different emergency airway management settings. Eur J Emerg Med. 2009;16:68–73.
60 Platts-Mills TF, Campagne D, Chinnock B, et al. A comparison of GlideScope video laryngoscopy versus direct laryngoscopy intubation in the emergency department. Acad Emerg Med. 2009;16:866–871.
61 Wayne MA, McDonnell M. Comparison of traditional versus video laryngoscopy in out-of-hospital tracheal intubation. Prehosp Emerg Care. 2010;14:278–282.
62 Sakles JC, Mosier JM, Chiu S, Keim SM. Tracheal intubation in the emergency department: A comparison of GlideScope(R) video laryngoscopy to direct laryngoscopy in 822 intubations. J Emerg Med. 2011;42:400–405.
63 Struck MF, Wittrock M, Nowak A. Prehospital GlideScope video laryngoscopy for difficult airway management in a helicopter rescue program with anaesthetists. Eur J Emerg Med. 2011;18:282–284.
64 Choi HJ, Kang HG, Lim TH, et al. Endotracheal intubation using a GlideScope video laryngoscope by emergency physicians: A multicentre analysis of 345 attempts in adult patients. Emerg Med J. 2010;27:380–382.
65 Walker L, Brampton W, Halai M, et al. Randomized controlled trial of intubation with the McGrath Series 5 videolaryngoscope by inexperienced anaesthetists. Br J Anaesth. 2009;103:440–445.
66 Shippey B, Ray D, McKeown D. Use of the McGrath videolaryngoscope in the management of difficult and failed tracheal intubation. Br J Anaesth. 2008;100:116–119.
67 Noppens RR, Mobus S, Heid F, et al. Evaluation of the McGrath Series 5 videolaryngoscope after failed direct laryngoscopy. Anaesthesia. 2010;65:716–720.
68 Ng I, Sim XL, Williams D, Segal R. A randomised controlled trial comparing the McGrath((R)) videolaryngoscope with the straight blade laryngoscope when used in adult patients with potential difficult airways. Anaesthesia. 2011;66:709–714.
69 Enomoto Y, Asai T, Arai T, et al. Pentax-AWS, a new videolaryngoscope, is more effective than the Macintosh laryngoscope for tracheal intubation in patients with restricted neck movements: A randomized comparative study. Br J Anaesth. 2008;100:544–548.
70 Abdallah R, Galway U, You J, et al. A randomized comparison between the Pentax AWS video laryngoscope and the Macintosh laryngoscope in morbidly obese patients. Anesth Analg. 2011;113:1082–1087.
71 Suzuki A, Terao M, Fujita S, Henderson JJ. Tips for intubation with the Pentax-AWS Rigid Indirect Laryngoscope in morbidly obese patients. Anaesthesia. 2008;63:442–444.
72 Sasano N, Sasano H, Sobue K. Failure of the Airway Scope to visualize the glottis: Two case reports. J Anesth Clin Res. 2011;2:137–138.
73 Asai T, Liu EH, Matsumoto S, et al. Use of the Pentax-AWS in 293 patients with difficult airways. Anesthesiology. 2009;110:898–904.
74 Maharaj CH, O’Croinin D, Curley G, et al. A comparison of tracheal intubation using the Airtraq or the Macintosh laryngoscope in routine airway management: A randomised, controlled clinical trial. Anaesthesia. 2006;61:1093–1099.
75 Maharaj CH, Costello JF, Harte BH, Laffey JG. Evaluation of the Airtraq and Macintosh laryngoscopes in patients at increased risk for difficult tracheal intubation. Anaesthesia. 2008;63:182–188.
76 Maharaj CH, Buckley E, Harte BH, Laffey JG. Endotracheal intubation in patients with cervical spine immobilization: A comparison of Macintosh and Airtraq laryngoscopes. Anesthesiology. 2007;107:53–59.
77 McElwain J, Laffey JG. Comparison of the C-MAC(R), Airtraq(R), and Macintosh laryngoscopes in patients undergoing tracheal intubation with cervical spine immobilization. Br J Anaesth. 2011;107:258–264.
78 Trimmel H, Kreutziger J, Fertsak G, et al. Use of the Airtraq laryngoscope for emergency intubation in the prehospital setting: A randomized control trial. Crit Care Med. 2011;39:489–493.
79 McGuire BE. Use of the McGrath video laryngoscope in awake patients. Anaesthesia. 2009;64:912–914.
80 Practice guidelines for management of the difficult airway: An updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2003;98:1269–1277.
81 Nishikawa K, Matsuoka H, Saito S. Tracheal intubation with the Pentax-AWS (Airway scope) reduces changes of hemodynamic responses and bispectral index scores compared with the Macintosh laryngoscope. J Neurosurg Anesthesiol. 2009;21:292–296.
82 Turkstra TP, Armstrong PM, Jones PM, Quach T. GlideScope use in the obstetric patient. Int J Obstet Anesth. 2010;19:123–124.
83 Vanderhal AL, Berci G, Simmons CF, Jr., Hagiike M. A videolaryngoscopy technique for the intubation of the newborn: Preliminary report. Pediatrics. 2009;124:e339–e346.
84 Mort TC. Tracheal tube exchange: Feasibility of continuous glottic viewing with advanced laryngoscopy assistance. Anesth Analg. 2009;108:1228–1231.
85 Howard-Quijano KJ, Huang YM, Matevosian R, et al. Video-assisted instruction improves the success rate for tracheal intubation by novices. Br J Anaesth. 2008;101:568–572.
86 Peterson GN, Domino KB, Caplan RA, et al. Management of the difficult airway: A closed claims analysis. Anesthesiology. 2005;103:33–39.