Chapter 33 Prehospital Airway Management
I Introduction
The variability in EMS systems throughout North America is dictated by several factors, including historical system design, state laws, system size, volunteer versus paid provider status, physicians’ preferences, and economic issues. For example, in large urban systems, a lack of high-quality medical direction and monitoring may make medication-assisted intubation difficult to successfully implement and sustain. In rural systems, the frequency of intubation may be low, making it difficult to acquire and maintain the necessary skill levels. Prehospital intubation can be challenging compared with the in-hospital environment. EMS providers work in a variety of conditions that complicate the task of airway management, ventilation, and oxygenation. Extreme weather, enclosed working spaces (e.g., cars, small rooms, hallways), bystander distractions, and a variety of other challenging situations face the EMT and paramedic.1
Some aspects of an EMS system design are essential for maximizing provider competency. The frequency with which any provider performs advanced airway management is critical for maintaining skill competency.2,3 Some systems have reported very low rates of intubation, especially for pediatric patients.4–6 How can competency be maintained when providers intubate three or four times per year?2,7–9 Should they intubate when the frequency is so low? System medical directors must answer these questions when designing, evaluating, or refining an EMS system. Physicians must be artful in selecting airway strategies, training providers, monitoring interventions, and maintaining quality.7
II History of Airway Management by Emergency Medical Services
Before the 1950s, prehospital airway management was provided by relatively unskilled providers in most EMS systems throughout the United States. Progressive systems of the time provided bag-mask ventilation with an oropharyngeal or nasopharyngeal airway. In some cases, training was limited to basic first aid without training in airway adjuncts.10–12
In the 1960s, the quality of prehospital care came into focus with publication of Accidental Death and Disability: The Neglected Disease of Modern Society by the National Research Council and development of a national standards curriculum for EMTs that defined minimal training and equipment.13 Standards included training in the use of basic equipment such as bag-mask ventilation, oropharyngeal and nasopharyngeal airways, and suction.
In the 1970s, some paramedic systems began to use neuromuscular blocking drugs to manage patients’ airways with great success. These programs provided significant medical oversight that included monitoring successful outcomes and complications associated with endotracheal intubations.14 System medical directors had concerns about the use of medication-assisted intubation, including the issue of increased time at the scene by paramedics and complications such as unrecognized esophageal intubation.15–17
Drug-assisted intubation is a relatively new idea that is used on a limited basis in EMS systems in North America. Because success rates for drug-assisted endotracheal intubation vary greatly among EMS groups, it is not routinely recommended.8,9 However, the National Association of EMS Physicians has developed guidelines for implementing drug-assisted intubation programs that include provider training, patient selection, use of standardized protocols and resources for storage and delivery of medications, training in verification and monitoring of end-tidal carbon dioxide, a continuous quality improvement program, and research on a system level to verify effectiveness of the program.18
Alternative airway devices have been used in prehospital care since the advent of prehospital advanced life support. Devices include the esophageal obturator, gastric tube airway, esophageal-tracheal Combitube, and King laryngeal tube (LT) airway. Many studies have demonstrated their relative effectiveness compared with bag-mask ventilation and endotracheal intubation (ETI) ventilation.19–21
III Prehospital Care of Airway Patients
Prehospital care of airway patients addresses the spectrum of clinical conditions faced in emergency departments, critical care units, and operating rooms. In the ideal world, providers would be prepared to deal with airway management and ventilation for all possible conditions, but the scope of practice and provider skill levels vary in North America. In other parts of the world, where physicians staff EMS vehicles, skill levels may be more uniform. At the entry level of emergency medical response (EMT-Basic), forced positive pressure with bag-mask ventilation and rapid transport may be the only options available. ETI has been considered the gold standard for definitive airway management, but the diverse skill levels found in prehospital care and the use of extraglottic airway devices in EMS have challenged this idea. High rates of unrecognized esophageal or hypopharyngeal placement or dislodgement have raised concerns about ETI as a default strategy for EMS providers.16,17
A Basic Airway Management
Most EMS providers are equipped to manage the patient who is unresponsive or in respiratory or cardiac arrest. Since the late 1960s, EMT-Basic training has included the use of oropharyngeal and nasopharyngeal airways, bag-mask ventilation, and suctioning. Training has emphasized appropriate mask seal, controlled volumes and inspiratory times, and the avoidance of hyperventilation in cardiac arrest and shock states.11,22–24
B Extraglottic Airway Devices
Use of the King LT as a primary and alternative airway device has been an effective prehospital airway strategy.17,25,26 Because alternative airway devices do not provide definitive protection against aspiration, they typically are used temporarily until ETI can be achieved in the field or in the emergency department. In one case report, the King LT resulted in tongue engorgement when left in place for approximately 3 hours.27
The double-lumen esophageal-tracheal Combitube is an alternative airway device commonly used in EMS. It has been used by Basic and Advanced EMTs as a primary airway device and by paramedics as a rescue device. Effectiveness of the Combitube has varied among studies in prehospital care. Cady and colleagues found it had no effect on patient outcomes compared with ETI.28 In a study of prehospital physicians, the Combitube was superior to ETI in the management of cardiopulmonary arrest.29 When the King LT and Combitube were compared in a study of EMS providers, nurses, and physicians, the King LT was inserted faster and preferred by 96% of the participants.30
For patients with acute respiratory distress and acute pulmonary edema, continuous positive airway pressure (CPAP) has significantly improved outcomes and reduced the need for intubation in prehospital care.31 CPAP has also proved to be cost-effective in the prehospital environment.32
Some studies have shown increased morbidity rates with prehospital intubation. Others have demonstrated no increase in mortality rates despite significant errors such as esophageal intubation, dislodgement, or failed ETI.33 A study of patients with acute respiratory distress showed a decrease in mortality rates when advanced interventions such as ETI were used in the prehospital environment.33
Some investigators think that ETI should not be standard operating procedure for EMS systems. Variables cited as key factors in determining whether a given EMS system should use ETI include low case exposure and inadequate operating room training for paramedics and paramedic students. However, it has been shown that if a minimum number of intubations is used as the criterion to permit ETI in the field, the overall numbers of ETI performed in the field decrease because fewer providers meet the minimum number needed to permit continued performance of the skill.2 Additionally, supraglottic devices have demonstrated equivalency to ETI in many studies, and many advocate using alternative strategies for ensuring the success rates for intubations, such as simulation and cadaver training.21,34,35 When time in the operating room is made available to paramedics, it can be a significant training adjunct for clinical practice.
The U.S. National Highway Traffic Safety Administration (NHTSA) requires only five intubations to be eligible for paramedic certification.22–24 This level is well below the recommended level of 35 ETIs for emergency medicine residents. Anesthesiology residents must perform between 45 and 60 ETIs to achieve at least a 90% success rate in the controlled setting of the operating room.36 Wang and colleagues calculated the learning curves for paramedic students performing ETI and found that at 20 to 25 ETIs in live subjects must be performed to achieve success rates of at least 90%.2 This finding argues that paramedics with only five ETIs during training may have little skill in performing intubations.
Medical oversight is a critical part of any EMS airway program. Direction by physicians has enhanced the cognitive (though not the technical) skills of paramedics and improved patient selection.7
IV System Structure and Types of Providers
The foundation for any EMS program is provided by system-wide protocols. Almost every system in North America has protocols that delineate the specific steps of care, types and dosages of medications, and other special considerations needed to rescue patients. Protocols usually are designed by a group of physicians, an EMS medical advisory committee, or an EMS medical director. In the case of advanced airway management in the United States, protocols relating respiratory failure, cardiac arrest, and airway obstruction are derived from the National EMS Education Standards and from guidelines for CPR and emergency cardiac care by the American Heart Association (AHA), International Liaison Committee on Resuscitation (ILCOR), and other reputable bodies.37–39
The guidelines for airway management have significantly changed over the past decade. The most striking modification is incorporation of waveform capnography as the gold standard for endotracheal tube confirmation and continuous verification of intratracheal positioning. In some EMS jurisdictions, waveform capnography has become a requirement for all intubations. The value of this strategy was established by Silvestri and colleagues, who demonstrated no unrecognized esophageal intubations when capnography was used in their EMS system.16
V Physician Oversight and Continuous Quality Assurance
Physician oversight of prehospital care has been an essential component since the earliest EMS advance life support programs.10 It has included training and evaluation, protocol development, radio communications with providers in the field, review and observation of patient care delivery, and continuous quality assurance programs. Airway management has been a central issue in advanced EMT and paramedic training since the early 1970s.
B Continuous Quality Improvement
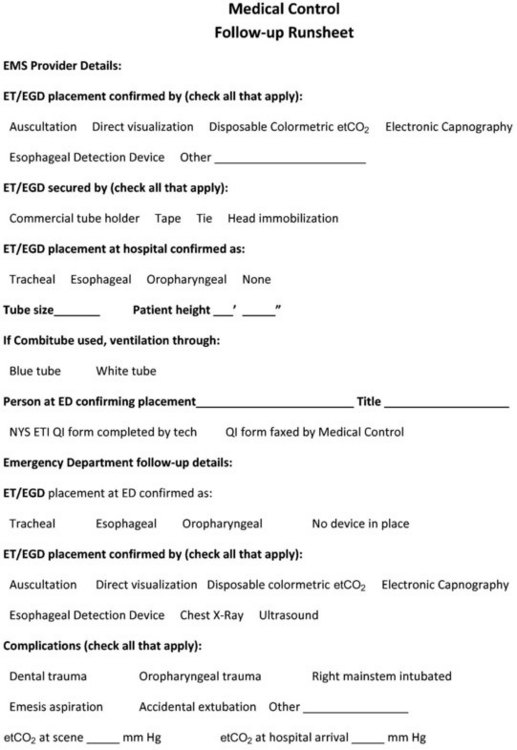
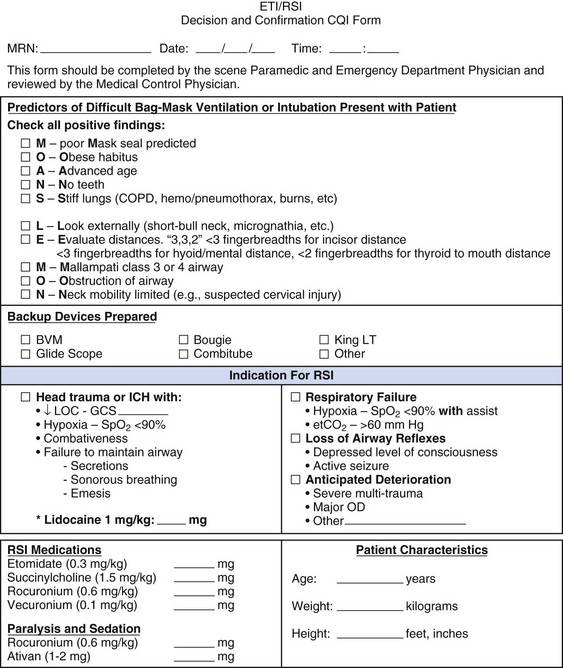
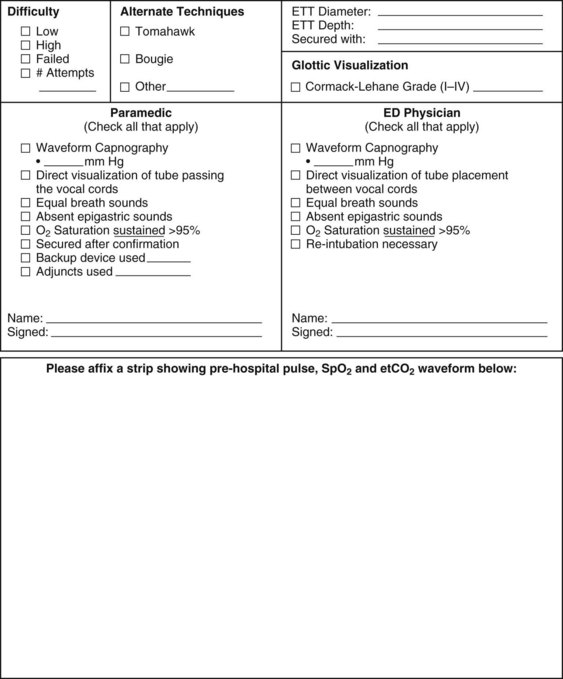
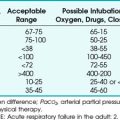
The most important role for a physician in prehospital care is continuous quality improvement. Poor airway management in prehospital care can result in brain injury and death. Every case of airway management and ventilation should be reviewed by the medical director’s staff. At a minimum, this includes tracking success rates for intubation and alternative airway devices and documenting end-tidal carbon dioxide values at the scene, during transport, and on arrival at the hospital. The receiving emergency department should be routinely contacted by the medical director’s staff for confirmation of airway device placement on arrival. Figure 33-1 is a review form that might be used for this purpose. Figure 33-2 is a more comprehensive form used by a hospital-based program using RSI.
VII Clinical Pearls
• Emergency medical services (EMS) provide a variety of prehospital care, including airway management.
• Emergency medical technicians (EMTs) work in many environments that complicate the task of airway management, including extreme weather, small, enclosed working spaces, and bystander distractions.
• EMS programs and EMT training are based on established protocols that delineate the specific steps of care, types and dosages of medications, and other special considerations needed to rescue patients. Protocols usually are designed by a group of physicians, an EMS medical advisory committee, or an EMS medical director and are based on national standards and curricula.
• EMTs are trained to assess a patient’s condition and to perform the procedures needed to maintain a patent airway with adequate breathing and cardiovascular circulation until the patient can be transported to a hospital for definitive medical care.
• EMTs can mange the patient who is unresponsive or in cardiorespiratory arrest. Depending on the level of training and local protocols, they can use bag-mask ventilation, suctioning, drug-assisted intubation, oropharyngeal and nasopharyngeal airways, and alternative devices such as the Combitube and King laryngeal tube (LT) airway.
• The most important role for a physician in prehospital care is continuous quality improvement, because poor airway management can result in brain injury and death.
All references can be found online at expertconsult.com.
2 Wang HE, Abo BN, Lave JR, et al. How would minimum experience standards affect the distribution of out-of-hospital endotracheal intubations? Ann Emerg Med. 2007;50:246–252.
4 Gausche M, Lewis RJ, Stratton SJ, et al. Effect of out-of-hospital pediatric endotracheal intubation on survival and neurological outcome: A controlled clinical trial. JAMA. 2000;283:783–790.
7 Cushman JT, Zachary Hettinger A, Farney A, Shah MN. Effect of intensive physician oversight on a prehospital rapid-sequence intubation program. Prehosp Emerg Care. 2010;14:310–316.
16 Silvestri S, Ralls GA, Krauss B, et al. The effectiveness of out-of-hospital use of continuous end-tidal carbon dioxide monitoring on the rate of unrecognized misplaced intubation within a regional emergency medical services system. Ann Emerg Med. 2005;45:497–503.
18 National Association of EMS Physicians (NAEMSP). Drug-assisted intubation in the prehospital setting: Position statement of the National Association of Emergency Physicians. Prehosp Emerg Care. 2006;10:260.
23 National Highway Traffic Safety Administration (NHTSA). National emergency medical services education standards. http://www.ems.gov/education/overview.html, 2010. Available at (accessed March 2012)
33 Wang HE, Cook LJ, Chang CC, et al. Outcomes after out-of-hospital endotracheal intubation errors. Resuscitation. 2009;80:50–55.
37 Hinchey PR, Myers JB, Lewis R, et al. Improved out-of-hospital cardiac arrest survival after the sequential implementation of 2005 AHA guidelines for compressions, ventilations, and induced hypothermia: The Wake County experience. Ann Emerg Med. 2010;56:348–357.
38 Brain Trauma Foundation. Prehospital severe traumatic brain injury guidelines. Available at http://tbiguidelines.org/glHome.aspx (accessed March 2012)
39 Walls R, Murphy M. Manual of emergency airway management, ed 3. Philadelphia: Lippincott, Williams & Wilkins; 2008. pp 303–325
1 Garza AG, Gratton MC, McElroy J, et al. Environmental factors encountered during out-of-hospital intubation attempts. Prehosp Emerg Care. 2008;12:286–289.
2 Wang HE, Abo BN, Lave JR, et al. How would minimum experience standards affect the distribution of out-of-hospital endotracheal intubations? Ann Emerg Med. 2007;50:246–252.
3 Ruetzler K, Roessler B, Potura L, et al. Performance and skill retention of intubation by paramedics using seven different airway devices—A manikin study. Resuscitation. 2011;82:593–597.
4 Gausche M, Lewis RJ, Stratton SJ, et al. Effect of out-of-hospital pediatric endotracheal intubation on survival and neurological outcome: A controlled clinical trial. JAMA. 2000;283:783–790.
5 Chen L, Hsiao AL. Randomized trial of endotracheal tube versus laryngeal mask airway in simulated prehospital pediatric arrest. Pediatrics. 2008;122:294–297.
6 Gerritse BM, Draaisma JM, Schalkwijk A, et al. Should EMS-paramedics perform paediatric tracheal intubation in the field? Resuscitation. 2008;79:225–229.
7 Cushman JT, Zachary Hettinger A, Farney A, Shah MN. Effect of intensive physician oversight on a prehospital rapid-sequence intubation program. Prehosp Emerg Care. 2010;14:310–316.
8 Tam RK, Maloney J, Gaboury I, et al. Review of endotracheal intubations by Ottawa advanced care paramedics in Canada. Prehosp Emerg Care. 2009;13:311–315.
9 Denver Metro Airway Study Group. A prospective multicenter evaluation of prehospital airway management performance in a large metropolitan region. Prehosp Emerg Care. 2009;13:304–310.
10 Mecham C. Emergency medical services. Tintinalli JE, ed. Tintinalli’s emergency medicine: A comprehensive study guide, ed 7, New York: McGraw-Hill, 2011.
11 U.S. Department of Transportation, National Highway Traffic Safety Administration (NHTSA). EMT-paramedic national standard curriculum, 1994. Available at http://www.health.ny.gov/nysdoh/ems/original/intro/intro.pdf (accessed March 2012)
12 Bell RC. The ambulance: A history. Jefferson, NC: McFarland; 2009.
13 National Research Council. Accidental death and disability: The neglected disease of modern society. Washington, DC: National Academy of Sciences; 1966.
14 Hedges JR, Dronen SC, Feero S, et al. Succinylcholine-assisted intubations in prehospital care. Ann Emerg Med. 1988;17:469–472.
15 Hedges JR, Feero S, Moore B, et al. Factors contributing to paramedic onscene time during evaluation and management of blunt trauma. Am J Emerg Med. 1988;6:443–448.
16 Silvestri S, Ralls GA, Krauss B, et al. The effectiveness of out-of-hospital use of continuous end-tidal carbon dioxide monitoring on the rate of unrecognized misplaced intubation within a regional emergency medical services system. Ann Emerg Med. 2005;45:497–503.
17 Wirtz DD, Ortiz C, Newman DH, et al. Unrecognized misplacement of endotracheal tubes by ground prehospital providers. Prehosp Emerg Care. 2007;11:213–218.
18 National Association of EMS Physicians (NAEMSP). Drug-assisted intubation in the prehospital setting: Position statement of the National Association of Emergency Physicians. Prehosp Emerg Care. 2006;10:260.
19 Garvin JM. The esophageal obturator airway—An improved model. Emerg Med Serv. 1979;8(48):50–51.
20 Frass M, Frenzer R, Rauscha F, et al. Evaluation of esophageal tracheal Combitube in cardiopulmonary resuscitation. Crit Care Med. 1987;15:609–611.
21 Braude D, Richards M. Rapid sequence airway (RSA): a novel approach to prehospital airway management. Prehosp Emerg Care. 2007;11:250–252.
22 National Highway Traffic Safety Administration (NHTSA). National emergency medical services scope of practice model. http://www.soundrock.com/sop/statement.html, 2005. Available at (accessed March 2012)
23 National Highway Traffic Safety Administration (NHTSA). National emergency medical services education standards. http://www.ems.gov/education/overview.html, 2010. Available at (accessed March 2012)
24 National Highway Traffic Safety Administration (NHTSA). National emergency medical services (EMS) core content. Available at http://www.nhtsa.gov/people/injury/ems/emscorecontent/images/EMSCoreContent.pdf (accessed March 2012)
25 Burns JB, Jr., Branson R, Barnes SL, et al. Emergency airway placement by EMS providers: Comparison between the King LT supralaryngeal airway and endotracheal intubation. Prehosp Disaster Med. 2010;25:92–95.
26 Warner GS. Evaluation of the effect of prehospital application of continuous positive airway pressure therapy in acute respiratory distress. Prehosp Disaster Med. 2010;25:87–91.
27 Gaither JB, Matheson J, Eberhardt A, et al. Tongue engorgement associated with prolonged use of the King-LT laryngeal tube device. Ann Emerg Med. 2010;55:367–369.
28 Cady CE, Weaver MD, Pirrallo RG, et al. Effect of emergency medical technician–placed Combitubes on outcomes after out-of-hospital cardiopulmonary arrest. Prehosp Emerg Care. 2009;13:495–499.
29 Rabitsch W, Schellongowski P, Staudinger T, et al. Comparison of a conventional tracheal airway with the Combitube in an urban emergency medical services system run by physicians. Resuscitation. 2003;57:27–32.
30 Tumpach EA, Lutes M, Ford D, Lerner EB. The King LT versus the Combitube: Flight crew performance and preference. Prehosp Emerg Care. 2009;13:324–328.
31 Warner GS. Evaluation of the effect of prehospital application of continuous positive airway pressure therapy in acute respiratory distress. Prehosp Disaster Med. 2010;25:87–91.
32 Hubble MW, Richards ME, Wilfong DA. Estimates of cost-effectiveness of prehospital continuous positive airway pressure in the management of acute pulmonary edema. Prehosp Emerg Care. 2008;12:277–285.
33 Wang HE, Cook LJ, Chang CC, et al. Outcomes after out-of-hospital endotracheal intubation errors. Resuscitation. 2009;80:50–55.
34 Kory PD, Eisen LA, Adachi M, et al. Initial airway management skills of senior residents: Simulation training compared with traditional training. Chest. 2007;132:1927–1931.
35 Okuda Y, Byson EO, DeMaria S, et al. The utility of simulation in medical education: What is the evidence? Mt Sinai J Med. 2009;76:330–343.
36 Mulcaster JT, Mills J, Hung OR, et al. Laryngoscopic intubation: Learning and performance. Anesthesiology. 2003;98:23–27.
37 Hinchey PR, Myers JB, Lewis R, et al. Improved out-of-hospital cardiac arrest survival after the sequential implementation of 2005 AHA guidelines for compressions, ventilations, and induced hypothermia: The Wake County experience. Ann Emerg Med. 2010;56:348–357.
38 Brain Trauma Foundation. Prehospital severe traumatic brain injury guidelines. Available at http://tbiguidelines.org/glHome.aspx (accessed March 2012)
39 Walls R, Murphy M. Manual of emergency airway management, ed 3. Philadelphia: Lippincott, Williams & Wilkins; 2008. pp 303–325