28
Vesiculopustular and Erosive Disorders in Newborns and Infants
This chapter covers classic transient neonatal eruptions as well as several infectious diseases and other disorders that present with vesiculopustules in the neonatal period or early infancy. Table 28.1 provides a more complete differential diagnosis of vesiculopustules, bullae, erosions, and ulcerations in neonates.
Common Transient Conditions
Erythema Toxicum Neonatorum (‘e tox’)
• Affects approximately half of full-term neonates; less common in premature infants.
• Various combinations of erythematous macules, wheals, and small (≤2 mm) papules, pustules, and vesicles surrounded by a larger erythematous flare (Fig. 28.1); lesions may be grouped at sites of mechanical irritation.


Fig. 28.1 Erythema toxicum neonatorum. Scattered papulovesicles and pustules with an erythematous flare on the abdomen (A) and upper extremity (B). Courtesy, Deborah S. Goddard, MD, Amy E. Gilliam, MD, and Ilona J. Frieden, MD.
• Wright’s stain of pustular contents shows numerous eosinophils.
Transient Neonatal Pustular Melanosis
• Lesions are almost always present at birth.
• Three stages, any of which may be present at a given time (Fig. 28.2).
– 2- to 10-mm superficial vesiculopustules with little or no surrounding erythema.
– Collarettes of scale at sites of ruptured vesiculopustules.
– Residual brown macules representing post-inflammatory hyperpigmentation, which may persist for several months.


Fig. 28.2 Transient neonatal pustular melanosis in an African-American neonate. A One hour after birth, flaccid vesiculopustules and superficial erosions with minimal surrounding erythema are present in the groin. B On the 8th day of life, hyperpigmented macules and a few collarettes of scale are evident on the lower leg.
• Any region can be affected, but favors the forehead, chin, neck, lower back, and shins.
• Wright’s stain of pustular contents shows neutrophils > eosinophils.
Miliaria (Heat Rash)
• Caused by blockage of eccrine sweat ducts.
– Small clear vesicles (likened to ‘dew drops’) without surrounding erythema (Fig. 28.3); they are fragile and therefore short-lived.
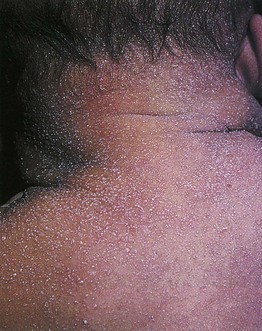
Fig. 28.3 Miliaria crystallina. Tiny, superficial vesicles, seen on the back and neck of this newborn, are characteristic of miliaria crystallina. From Eichenfield L.F., Frieden I.J., Esterly N.B., et al. (Eds.). Textbook of Neonatal Dermatology. © 2001 Saunders.
– Most often on the forehead, upper trunk, and arms.
– Usually develops at ≥1 week of age.
– Small erythematous papules, sometimes with a tiny central pustule or vesicle.
– Favors the neck, upper trunk, and occluded areas.
• Rx: avoid overheating and occlusion; bathing with lukewarm water.
Neonatal Cephalic Pustulosis (Neonatal Acne)
• Onset usually at 2–3 weeks of life, with spontaneous resolution by 2–3 months of age.
• Papulopustular eruption on the face (cheeks > forehead, chin, eyelids) (Fig. 28.4) > neck, upper chest, and scalp.

Fig. 28.4 Neonatal cephalic pustulosis. Papulopustules on the forehead and cheeks of a 3-week-old infant. Courtesy, Julie V. Schaffer, MD.
• An absence of comedones in neonatal cephalic pustulosis distinguishes it from infantile acne, which typically develops at 3–12 months of age and is more persistent (see Chapter 29).
• Rx: usually not required; topical imidazoles (e.g. ketoconazole cream) may be helpful.
Infectious Diseases
Cutaneous Candidiasis
– Evident at birth or during the first few days of life.
– Findings range from erythematous papules and pustules with fine scaling in full-term neonates to diffuse, ‘burn-like’ erythema and erosions in premature infants (Fig. 28.5A,B).



Fig. 28.5 Congenital candidiasis and bullous impetigo. A Numerous pink papules admixed with small superficial pustules and desquamation due to congenital candidiasis in a full-term neonate. Note the plantar involvement. B Widespread ‘burn-like’ erosions due to congenital candidiasis in a premature neonate born at 24 weeks’ gestation. C Multiple superficial erosions with collarettes of scale in the diaper area of an infant with bullous impetigo. Note the scattered vesiculopustules. A, B, Courtesy, Julie V. Schaffer, MD.
• Neonatal candidiasis (see Chapter 64).
– Common condition that presents at ≥1 week of age as intense erythema with desquamation and satellite papulopustules, favoring the diaper area > other intertriginous sites (see Fig. 13.4); patients may also have oral thrush.
Bullous Impetigo (See Chapter 61)
• Presents as early as a few days of age with flaccid bullae, vesiculopustules, and superficial shiny red erosions with collarettes of scale (Fig. 28.5C).
• Favors the diaper area and other intertriginous sites (see Fig. 13.4).
• DDx: Gram stain shows gram-positive cocci in clusters, and culture grows Staphylococcus aureus.
Neonatal Herpes Simplex Virus (HSV) Infection (See Chapter 67)
• Onset from birth to 2 weeks, but usually ≥5 days of age.
• Localized (favoring the scalp and trunk) or disseminated vesicles (Fig. 28.6), pustules, and crusts; lesions are often grouped and may progress to bullae and erosions with scalloped borders.
• Involvement of the oral mucosa, eye, CNS, and other internal organs can occur.
Uncommon Conditions
Eosinophilic Pustular Folliculitis in Infancy
• Onset often in the first few months of life, with cyclical recurrences for several months to years.
• Pruritic perifollicular pustules and crusts favoring the scalp (Fig. 28.7) and forehead.

Fig. 28.7 Eosinophilic pustular folliculitis in infancy. Crusted papules and pustules on the scalp of a 1-year-old boy. Courtesy, Deborah S. Goddard, MD, Amy E. Gilliam, MD, and Ilona J. Frieden, MD.
• Rx: potent topical CS (intermittently for flares), oral antihistamines.
Infantile Acropustulosis (Acropustulosis of Infancy)
• Onset usually between 3 and 6 months of age; occasionally develops in newborns.
• Pruritic vesicles and pustules on the hands and feet (including palms/soles) (Fig. 28.8) > wrists and ankles.

Fig. 28.8 Infantile acropustulosis. Multiple vesiculopustules with an erythematous base on the medial ankle of an infant. Courtesy, Deborah S. Goddard, MD, Amy E. Gilliam, MD, and Ilona J. Frieden, MD.
• Outbreaks last 1–2 weeks, with cyclical recurrences until 2–3 years of age.
• Rx: potent topical CS (intermittently for flares), oral antihistamines.
Incontinentia Pigmenti (IP) (See Chapter 51)
• Typically presents in the first 2 weeks of life with vesicles on an inflammatory base in linear streaks that favor the extremities (Fig. 28.9); in subsequent weeks, verrucous streaks may develop, followed by more widespread linear and whorled grayish-brown hyperpigmentation.
Differential diagnosis of neonatal vesiculopustules, bullae, erosions, and ulcers.
This list is not exhaustive, as other rare diseases such as deficiency of the interleukin-1 receptor antagonist (DIRA), ankyloblepharon–ectodermal dysplasia–clefting (AEC) syndrome, and congenital Behçet’s disease can have vesiculopustular and erosive presentations.
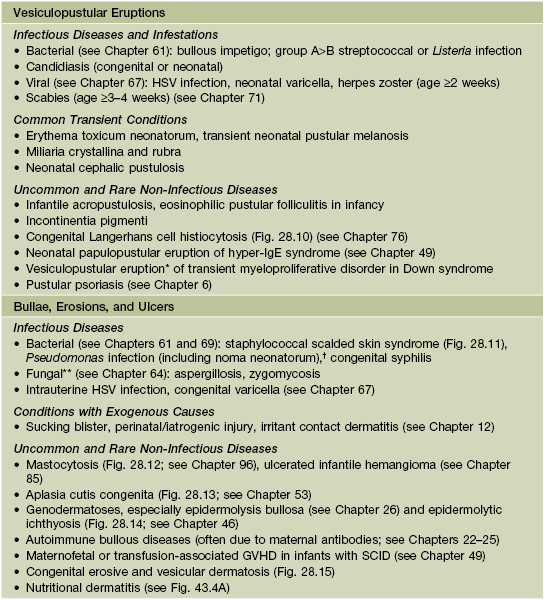
* Favors the cheeks.
** Evolves into necrotic ulcers; risk factors include prematurity and occlusion.
† Evolves into necrotic ulcers that favor the groin; risk factors include prematurity, immunodeficiency, and (especially for noma) malnutrition.
SCID, severe combined immunodeficiency.

Fig. 28.10 Congenital Langerhans cell histiocytosis. Numerous erosions with crusting on the face and trunk of a newborn. Courtesy, Deborah S. Goddard, MD, Amy E. Gilliam, MD, and Ilona J. Frieden, MD.

Fig. 28.11 Staphylococcal scalded skin syndrome. Radiating perioral scale-crusts due to exfoliative toxins.


Fig. 28.12 Bullous mastocytosis. A Tense bulla on the wrist and flaccid bullae on the dorsal hand as well as pink plaques on the trunk in a 1-month-old infant. B Second infant with erosions and diffuse infiltration of the skin with mast cells, leading to a thickened leathery appearance. A, Courtesy, Deborah S. Goddard, MD, Amy E. Gilliam, MD, and Ilona J. Frieden, MD.

Fig. 28.13 Aplasia cutis congenita. Ulcerations on the vertex of the scalp may be misdiagnosed as an HSV infection. The angulated appearance of the larger ulceration would not be characteristic of HSV infection.

Fig. 28.14 Epidermolytic ichthyosis (bullous congenital ichthyosiform erythroderma). Diffuse scaling and a large erosion with scale-crust in a neonate.


Fig. 28.15 Congenital erosive and vesicular dermatosis. A Bright red, irregularly shaped erosions on the buttocks of a 2-week-old infant. B Residual supple and reticulate scarring in a 9-month-old child. A, Courtesy, Anthony J. Mancini, MD; B, Courtesy, Julie V. Schaffer, MD.
For further information see Ch. 34. From Dermatology, Third Edition.










