Venous system
Peripheral venography
Lower limb
Patient preparation
The leg should be elevated overnight to lessen oedema if leg swelling is severe.
Technique
1. The patient is supine and tilted 40° head up, to delay the transit time of the contrast medium.
2. A tourniquet is applied tightly just above the ankle to occlude the superficial venous system. The compression may also occlude the anterior tibial veins, and so their absence should not automatically be interpreted as due to venous thrombosis.
3. A 19G butterfly needle (smaller if necessary) is inserted into a vein on the dorsum of the foot. If the needle is too near the ankle, the contrast medium may bypass the deep veins and so give the impression of deep venous occlusion.
4. 40 ml of contrast medium is injected by hand. The first series of spot films is then taken.
5. A further 20 ml bolus is injected quickly whilst the patient performs a Valsalva manoeuvre to delay the transit of contrast medium into the upper thigh and pelvic veins. The patient is tilted quickly into a slightly head down position and the Valsalva manoeuvre is relaxed. Alternatively, if the patient is unable to comply, direct manual pressure over the femoral vein whilst the table is being tilted into the head-down position will achieve the same effect. Films are taken 2–3 s after releasing pressure.
6. At the end of the procedure the needle should be flushed with 0.9% saline to lessen the chance of phlebitis due to contrast medium.
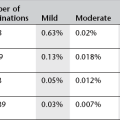
Complications
Due to the contrast medium
Upper limb
Technique
2. An 18G butterfly needle is inserted into the median cubital vein at the elbow. The cephalic vein is not used, as this bypasses the axillary vein
3. Spot films are taken of the region of interest during a hand injection of 30 ml of contrast medium. Alternatively a digital subtraction angiographic run can be performed at 1 frame sec−1.
Central venography
Superior vena cavography
Technique
2. 18G butterfly needles are inserted into the median antecubital vein of both arms
3. Hand injections of contrast medium 30 ml per side are made simultaneously, as rapidly as possible, by two operators. The injection is recorded by rapid serial radiography (see ‘Films’ below). The film sequence is commenced after about two-thirds of the contrast medium has been injected.
N.B. If the study is to demonstrate a congenital abnormality, or on the rare occasion that the opacification obtained by the above method is too poor, a 5-F catheter with side holes, introduced by the Seldinger technique, may be used.
Inferior vena cavography
Technique
1. With the patient supine, the catheter is inserted into the femoral vein using the Seldinger technique (see Chapter 9). A Valsalva manoeuvre may facilitate venepuncture by distending the vein. The vein can be punctured blindly by palpating the femoral artery pulsation and aiming to its medial side, but it is preferable to puncture the vein under direct US guidance.
2. Any obstruction to the passage of the catheter may indicate thrombus in the iliac veins or that the catheter and wire have entered an ascending lumbar vein. Fluoroscopy and gentle hand injection of contrast will clarify.
3. An injection of 40 ml of contrast medium is made at 20 ml s–1 by a pump injector, and recorded by rapid serial radiography or as a digital subtraction run at 2 frames s–1.
Portal venography
Technique
For trans-splenic approach
1. With the patient supine, the position of the spleen is percussed or identified with US. The access point is as low as possible in the midaxillary line, usually at the level of the tenth or eleventh intercostal space.
2. The region is anaesthetized using a sterile procedure.
3. The patient is asked to hold their breath in mid-inspiration, and the needle is then inserted inwards and upwards into the spleen (about three-quarters of the length of the needle is inserted, i.e. 7.5 cm). The needle and stilette are then withdrawn, leaving the plastic cannula in situ. Blood will flow back easily if the cannula is correctly sited. The patient is then asked to breathe as shallowly as possible to avoid trauma to the spleen from excessive movement of the cannula.
4. A test injection of a small volume of contrast medium under screening control can be made to ensure correct siting of the cannula. If it has transfixed the spleen, simple withdrawal into the body of the spleen is not acceptable, as any contrast medium subsequently injected would follow the track created by the withdrawal. A new puncture is necessary.
5. When the cannula is in a satisfactory position, the splenic pulp pressure may be measured with a sterile manometer (normally 10–15 cmH2O).
6. A hand injection of 50 ml of contrast medium is made over 5 s and recorded by rapid serial radiography/digital subtraction angiography. The cannula should be removed as soon as possible after the injection to minimize trauma to the spleen.
7. Occasionally a patent portal vein will fail to opacify, owing to major portosystemic collaterals causing reversed flow in the portal vein. The final arbiter of portal vein patency is direct mesenteric venography performed at operation. The maximum width of a normal portal vein is said to be 2 cm.
Transhepatic portal venous catheterization
Technique
1. 5-ml samples of blood are taken at points along the splenic vein, superior mesenteric vein and first part of the portal vein. The samples are numbered sequentially, and the site from which each was taken is marked on a sketch map of the portal drainage system. Simultaneous peripheral blood samples should be obtained at the same time as each portal sample to assess changing blood levels.
2. The accuracy of sampling can be improved by selective catheterization of pancreatic veins using varying shapes of catheter.1
Ultrasound
3. Abdominal veins including renal veins, hepatic and portal veins, and inferior vena cava
4. Venous anatomy to assist in central venous line placement, e.g. for the internal jugular or subclavian vein.
US is most commonly used for assessment of patients with suspected venous thrombosis, particularly of the lower limb. It is also useful to assess arterio-venous fistulae; both therapeutic fistulae created for haemodialysis and those occurring as a complication of interventional vascular procedures, and for pre-surgical planning in patients with varicose veins. Both duplex and colour Doppler techniques are utilized.
Lower limb venous ultrasound
Technique
1. Patient supine with foot-down tilt. The popliteal and calf veins can easily be examined with the patient sitting with legs dependent or lying on a tilted couch with flexed knees and externally rotated hips. The femoral veins and external iliac veins are examined supine. The popliteal veins may be examined with the patient prone.
2. Longitudinal and transverse scans for external iliac, femoral and popliteal veins. For tibial and peroneal veins, these may be supplemented by oblique coronal scans.
3. Each vein may be identified by real-time scanning and colour Doppler. If in any doubt it may be confirmed as a vein by the spectral Doppler tracing. A normal patent vein should be completely occluded in real time by directly applied transducer pressure (though this is not always possible for the superficial femoral vein at the adductor canal).
4. The normal venous signal is phasic and in the larger veins varies with respiration. Flow can be stopped by a Valsalva manoeuvre and is transiently augmented by distal compression of the foot or calf. Acute thrombus may be non-echogenic but the vein should not be completely compressible nor fill with colour Doppler. Thrombus tends to become echogenic after a few days.
5. Although this technique is less well established for the exclusion of thrombus in the calf vessels, it has been shown to have a sensitivity and specificity close to that of venography. Cannulation of a vein and injection of contrast medium can thus be avoided.
Upper limb venous ultrasound
Technique
1. The patient should be recumbent on a couch wide enough to support the upper limb and trunk comfortably.
2. With the arm in a neutral position at the patient’s side, the subclavian vein is assessed either from above or below the clavicle. The image plane is parallel to the long axis of the vein. Diagnostic criteria for upper limb thrombosis are the same as those used for the lower limb, but the Doppler waveform in the upper limb venous system is more pulsatile because of proximity to the heart. The upper limb also has a much more extensive network of potential collateral venous pathways and care should be taken to avoid confusion of a patent collateral vein with the potentially occluded deep venous structure under examination.
3. The arm is then abducted and the axillary and brachial veins examined. The transducer should be placed high in the axilla to identify the proximal axillary vein and the Doppler characteristics of the axillary and brachial veins followed to assess for spontaneous and phasic flow, and appropriate response to augmentation and Valsalva manoeuvre. Both transverse and longitudinal imaging planes should be used, including assessment of response to compression.
The examination can be extended to include the cephalic, basilic and forearm veins.
Impedance plethysmography
This technique depends on the principle of the capacity of the veins to fill and empty in response to temporary obstruction to venous outflow by occlusion of the thigh veins with a pneumatic cuff. Changes in calf volume produce changes in impedance measured by electrodes applied to the calf. The technique is demanding and requires skilled personnel. Clinical states that impair venous return, such as cardiac failure and pelvic pathology and also arterial insufficiency, produce abnormal results. Many centres use impedance plethysmography in conjunction with clinical pretest probability scoring and/or plasma D-dimer assay to identify patients who do not need to proceed to US or venography.1
Computed tomography
Multidetector CT (MDCT) with standard i.v. contrast and scan delay protocols for the chest or abdomen/pelvis (see Chapter 1) is very effective for detection of compression or thrombosis of major veins including the superior and inferior vena cavae, iliac and renal veins.
In a group of selected patients with suspected pulmonary embolus (PE), MDCT of the lower limbs from iliac crest to popliteal fossa, 2 min after completion of CT pulmonary angiography (indirect CT venography), may be used as an alternative to US for detection of lower limb deep venous thrombosis. However, there is a significant associated radiation dose and there is no diagnostic advantage over US.1 Indirect CT venography is not recommended in patients with suspected deep vein thrombosis, but without suspected PE. It should only be used as an alternative to US in patients undergoing CT for suspected PE for whom identification of DVT is considered necessary2 or those with a high probability of PE, including patients with history of previous venous thrombo-embolism and possible malignancy.3
References
1. Goodman, LR, Stein, PD, Matta, F, et al. CT venography and compression sonography are diagnostically equivalent: data from PIOPED II. Am J Roentgenol. 2007; 189(5):1071–1076.
2. Thomas, SM, Goodacre, SW, Sampson, FC, et al. Diagnostic value of CT for deep vein thrombosis; results of a systematic review and meta-analysis. Clin Radiol. 2008; 63(3):299–304.
3. Hunsaker, AR, Zou, KH, Poh, AC, et al. Routine pelvic and lower extremity CT venography in patients undergoing pulmonary CT angiography. Am J Roentgenol. 2008; 190(2):322–326.
Magnetic resonance
Standard guidance applies on selection of patients suitable for MRI examination (see Chapter 1).
MRI is well suited to imaging the venous system, but because of cost and limited availability it is used infrequently. Peripheral MR venography (MRV)1 is currently used in selected cases of venous thrombosis in pregnant subjects and where fractured limbs are immobilized in casts. It is useful in evaluation of congenital abnormalities of peripheral venous anatomy and venous malformations.
MR venography offers unique diagnostic possibilities for abdominal, pelvic and thoracic veins,2 and development of blood pool contrast agents (see Chapter 2) will further improve clinical usefulness of these procedures.3
References
1. Sampson, FC, Goodacre, SW, Thomas, SM, et al. The accuracy of MRI in diagnosis of suspected deep vein thrombosis: systematic review and meta-analysis. Eur Radiol. 2007; 17(1):175–181.
2. Butty, S, Hagspiel, KD, Leung, DA, et al. Body MR venography. Radiol Clin North Am. 2002; 40(4):899–919.
3. Prince, MR, Sostman, HD. MR venography: unsung and underutilized. Radiology. 2003; 226(3):630–632.