Use of ultrasound in war zones
Overview
During previous conflicts, as recently as the late 20th century, medical diagnostic imaging on the battlefield was mostly limited to sparsely available plain radiography. The introduction of ruggedized handheld ultrasound devices in the late 1990s transformed the diagnostic capability on the modern battlefield.1,2 Although still vulnerable to the harsh environment of war zones, these lightweight portable units now enhance medical care for diverse battlefield settings and medical providers. The use of ultrasound in war zones often reflects its use in traditional hospital environments; however, the unique challenges and constraints of the battlefield give rise to unique applications.
Deployable ultrasound devices and technology
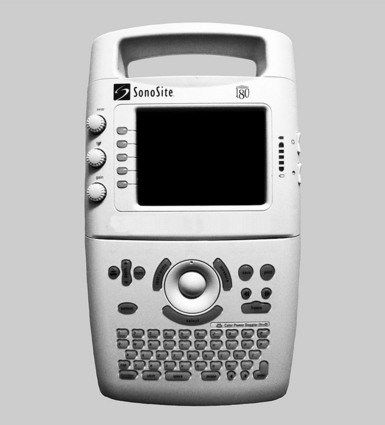
Ultrasound imaging for field military use became feasible in 1999 with the release of the SonoSite 180 machine (SonoSite, Bothell, WA), which was developed with a grant from the United States government for military use, with specifications that it be “a field device, hand-held by soldiers or medics, producing high quality images which could be downloaded via satellite to physicians at base hospitals” (Figure 49-1).1,2 To achieve these goals and be practical for field use, designers of this and subsequent ultrasound machines have sought to be lightweight and easy to transport, rugged, and versatile in their power source.
War zone ultrasonographers may be equipped with capable technology and basic image acquisition and interpretation training but may lack the expertise to interpret some aspects of the images obtained. Via telesonography, electronic communication tools allow the transmission of ultrasound images from the point of care to specialists for further image interpretation. Several battlefield methods have been described.2–5 Image file capture can be achieved by the ultrasound machine or a secondary device, such as a camera or camera-equipped phone. Image file transmission has been described by phone, landline, and by wireless relay from a portable vest-mounted transmitter to a receiving antenna and then to a satellite.6 The clinical impact of telesonography depends on the speed of image transmission, clarity of the final received image, and the timeliness of pertinent image interpretation.
Settings of patient care during war
Medical care is delivered to battlefield casualties in several unique settings, from the point of injury to care during evacuation out of the war zone. Each of these settings can pose exceptional challenges to a unique combination of care providers with varying medical skills and familiarity with ultrasound (Table 49-1). These variations allow diverse opportunities for ultrasound to impact the care of injured or ill patients.
TABLE 49-1
Characteristics of Different Settings of Care in the War Zone
| Setting | Potential Ultrasonographers Providing Care | Challenges to Medical Care |
| Point of injury | Medics Soldiers |
Enemy fire Noise Lack of resources Lack of medical expertise Mass casualty events |
| Prehospital transport | Medics | Enemy fire Noise Uncertainty of injuries |
| Field aid station | Medics Physicians Midlevel providers, such as physician assistants |
Enemy fire Uncertainty of injuries Lack of resources Lack of medical specialists |
| Field hospital | Physicians Midlevel providers, such as physician assistants Nurses Medics |
Mass casualty events Variable resources and medical specialists |
| War zone evacuation | Physicians Nurses Medics |
Noise Long transport times |
During war, the prehospital medical setting is typically characterized by simple and unpredictable resources amidst exposure to harsh environmental conditions and the danger of enemy engagements. Patient care may take place without shelter, while under enemy fire, and with limited oversight. In such situations, ultrasound imaging can be used by soldiers, typically combat medics, to guide patient care. Ultrasound imaging can act as a triage tool to identify those most needing evacuation to a combat hospital or those patients who can be adequately cared for in smaller rapidly deployed and highly mobile aid stations.7 In this dynamic environment, ultrasound imaging may be the only method of diagnostic imaging available. Ultrasonographers in this field setting may rely only on prior ultrasound instruction or may also have telesonography resources available to assist in image interpretation and patient care.
Current uses and applications
Although portable ultrasound devices were partly developed for use by the United States military in the battlefield, the applications used there are not generally novel. However, the use of and unique reliance on ultrasonography in war zones often reflects the exceptional constraints and needs of providing medical care during combat. These limitations and the extreme circumstances experienced by field ultrasonographers have resulted in some highly effective and well-described applications of ultrasound imaging in a war zone (Table 49-2).
TABLE 49-2
Commonly Reported and Less Frequently Described Uses of Ultrasound in War Zones
| Well-Described Uses of Ultrasound | Other Reported Uses of Ultrasound |
| FAST (and e-FAST) Fracture detection Abdominal Foreign body detection or related soft tissue applications Pelvic ultrasound for female abdominal pain and first trimester bleeding Echo Procedural ultrasound |
Optic nerve sheath diameter assessment after head injury Thoracic ultrasound to detect pneumonia Assistance of peripheral and regional nerve blocks DVT Renal Assistance of intubation confirmation and cricothyroidotomy |
Combat casualties are often critically ill and occur in multicasualty or mass casualty incidents, with hemorrhage being the most common cause of death.8 The FAST (focused assessment with sonography in trauma) examination evaluating for potential blood in the peritoneal, thorax, and pericardial space, and the e-FAST (extended focused assessment with sonography in trauma) examination, which includes an additional thoracic window to evaluate for a pneumothorax, are frequently used as a triage tools during combat casualty arrival.2,4,5,9 Operating room capabilities are often limited, and advanced imaging, such as computed tomography, may be absent in a war zone; a portable ultrasound device can triage patients in these resource-scarce zones. Both the FAST and e-FAST examinations also provide an ability to assess and reassess for life-threatening injuries during periods of loud and otherwise challenging helicopter or armored vehicle patient evacuation.10
Lack of advanced or alternative methods of diagnostic imaging in the presence of a portable ultrasound device has produced a number of case reports describing additional ultrasound applications, such as ultrasonographic fracture detection, soft tissue foreign-body detection, and ultrasonographic ocular assessment of the optic nerve sheath diameter for evidence of increased intracranial pressure.2,11–13 Radiography machines, which are significantly easier to transport than computed tomography, are not easily portable compared with handheld ultrasound devices, which can be transported in a medic’s equipment bag without location barriers. In the absence of radiography, combat medics and physicians have relied on ultrasound to detect, with high accuracy, the presence of underlying pathology requiring limited transportation resources to transfer patients to a higher level of medical care or evacuation from the war theater.
In the war zone, ultrasound (often used by nonradiologist physicians) is frequently used for nontraumatic and procedural indications. Abdominal imaging for medical complaints, such as gallbladder pathology, is common, and female pelvic and obstetrical/gynecologic ultrasound imaging for applications such as ovarian and pregnancy-related pathology is prevalent.2,4,9,14 Simple procedural applications, such as assistance with central line insertion, are used in a similar manner as in nonwar settings. More advanced ultrasonographic procedural applications, such as imaging of fracture reduction and assistance with complicated regional and peripheral nerve blocks, are also used when operator expertise is sufficient.15,16 The use of complex nerve blocks in the combat hospital setting can be a particularly valuable method of achieving excellent and long-lasting anesthesia and pain control in patients with complex traumatic injuries.
Pearls and highlights
• The needs of medical care on the modern battlefield have influenced advancements in ultrasound technology through the development of the first portable ultrasound units.
• To be feasible for use in war zones, ultrasound devices must be portable and lightweight, small, rugged, and able to be safely transported in varying environmental conditions, locations, and settings. Ultrasound kits must possess enough battery power to sustain use between anticipated electrical sources and have a variety of transducers to facilitate desired field applications.
• Battlefield ultrasound imaging can achieve clinical impact when performed by ultrasonographers of varying skills—from soldiers with little medical background to medics to physicians. Targeted training can facilitate the ability of novice ultrasonographers, and telesonography can enable accurate interpretation of images when specialists are not available for image interpretation at the point of care.
• Medical care in war zones occurs in unique locales and situations, such as in the battlefield, during medical evacuation in an armored vehicle or helicopter, in field aid stations, the combat hospital, and during evacuation from the war zone. Environmental conditions, enemy fire and noise, special constraints, and unpredictable resources and access to specialty medical care are some challenges that ultrasonographers face in these settings.
• Portable ultrasound has proven to be uniquely adaptable in war zones as an imaging modality and adjunct to patient care. Although most applications are similar to the noncombat setting, ultrasonography in combat is often heavily relied upon as the only diagnostic tool to guide patient triage, patient treatment, and evacuation to higher levels of patient care.
References
1. Hwang, J, Quistgaard, J, Souquet, J, et al. Portable ultrasound device for battlefield trauma,. Proc IEEE Ultrasonics Symp. 1998; 2:1663–1667.
2. Langlois Sle, P, Portable ultrasound on deployment. ADF Health. 2003;4(2):77–80.
3. Strode, CA, Rubal, BJ, Gerhardt, RT, et al. Satellite and mobile wireless transmission of focused assessment with sonography in trauma. Acad Emerg Med. 2003; 10(12):1411.
4. Rozanski, TA, Edmondson, JM, Jones, SB, Ultrasonography in a forward-deployed military hospital. Mil Med. 2005;170(2):99–102.
5. Harcke, HT, Statler, JD, Montilla, J, Radiology in a hostile environment: experience in Afghanistan. Mil Med. 2006;171(3):194–199.
6. Nations, JA, Browning, RF. Battlefield applications for handheld ultrasound. US Quart. 2011; 27(3):171–176.
7. Whitfield, DA, Portouw, SJ, Retinal detachment due to facial gunshot wound: the utility of ultrasonography in medically austere environment. J Emerg Med. 2012;42(6):678–681.
8. Bellamy, RF, The causes of death in conventional land warfare: implications for combat casualty care research. Mil Med. 1984;149(2):55–62.
9. Peoples, GE, Gerlinger, T, Craig, R, et al. Combat casualties in Afghanistan cared for by a single Forward Surgical Team during the initial phases of Operation Enduring Freedom. Mil Med. 2005; 170(6):462–468.
10. Madill, JJ. In-flight thoracic ultrasound detection of pneumothorax in combat. J Emerg Med. 2010; 39(2):194–197.
11. McNeil, CR, McManus, J, Mehta, S. The accuracy of portable ultrasonography to diagnose fractures in an austere environment. Prehosp Emerg Care. 2009; 13(1):50–52.
12. Vasios, WN, Hubler, DA, Lopez, RA, et al, Fracture detection in a combat theater: four cases comparing ultrasound to conventional radiography. J Spec Oper Med. 2010;10(2):11–15.
13. Hightower, S, Chin, EJ, Heiner, JD. Detection of increased intracranial pressure by ultrasound. J Spec Oper Med. 2012; 12(3):19–22.
14. Albright, TS, Gehrich, AP, Wright, J, Jr., et al, Utility of ultrasound in the combat theater: experiences of a gynecologist during Operation Iraqi Freedom/Operation Enduring Freedom. Mil Med. 2007;172(5):507–510.
15. Plunkett, AR, Brown, DS, Rogers, JM, et al, Supraclavicular continuous peripheral nerve block in a wounded soldier: when ultrasound is the only option. Br J Anaesth. 2006;97(5):715–717.
16. Allcock, E, Spencer, E, Frazer, R, et al. Continuous transversus abdominis plane (TAP) block catheters in a combat surgical environment. Pain Med. 2010; 11(9):1426–1429.