Chapter 97 Upper respiratory tract obstruction in children
Upper respiratory tract obstruction (URTO) is a common cause of respiratory failure in infants and children. This reflects the frequency of upper respiratory tract abnormalities and disorders, the presence of narrow airways and the structural inefficiencies of the lung and chest wall. The majority of children with critical airway obstruction are otherwise healthy, and expert management results in a normal life expectancy. Poor management can lead to cardiopulmonary arrest and hypoxic cerebral damage.
ANATOMICAL DIFFERENCES AND CLINICAL RELEVANCE
Differences in the anatomy and function of the airway are important considerations in airway maintenance, laryngoscopy and intubation. In the newborn, the nose contributes approximately 42% of total airways resistance, which is considerably less than the adult’s 63%. Thus, infants are obligatory nose-breathers. The epiglottis is longer, U-shaped and floppy, and may need to be lifted with a straight-bladed laryngoscope for visualisation of the larynx and intubation. The larynx is higher in the neck (C3–4) in the neonate, and has an anterior inclination.1 It descends over the first 3 years of life, and again at puberty, to ultimately lie opposite C6. The length of the trachea varies from 3.2 to 7.0 cm in babies weighing less than 6 kg. Accurate positioning of the tracheal tubes is required to prevent accidental extubation or endobronchial intubation. The narrowest part of the airway until puberty is the cricoid ring. This part of the airway is most vulnerable to trauma and swelling. The narrow cricoid ring also dictates tube size, and allows use of uncuffed tubes in infants and children.
PATHOPHYSIOLOGY
Although the ratio of airway diameter to body weight is relatively large in the infant, in absolute terms airway diameter is small, and a minimal reduction causes a devastating increase in airway resistance. For example, the diameter of the newborn’s cricoid ring is 5 mm. A 50% reduction in radius will result in turbulent flow, and increases the pressure (and work) required to maintain breathing 32-fold.2
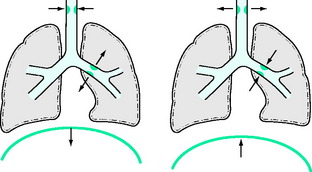
Symptoms and signs vary with the level of obstruction, the aetiology and the age of the child. Airway obstruction may be extrathoracic, intrathoracic or a combination. Extrathoracic obstruction is more pronounced during inspiration and is characterised by inspiratory stridor and prolongation of inspiration. Intrathoracic obstruction affecting either large or small airways is more pronounced during expiration and is characterised by expiratory stridor, prolonged expiration, wheeze and air trapping. Biphasic stridor is characteristic of mid tracheal lesions. These features mirror the intrapleural and airway pressure changes of the respiratory cycle (Figure 97.1). Retraction of the chest wall, an important sign of respiratory distress, reflects the negative intrapleural pressures generated combined with the compliance of the chest wall. Large negative intrapleural pressures are also transmitted to the interstitium of the lung, and may result in pulmonary oedema.3,4 Cor pulmonale may develop secondary to chronic obstruction, hypoxia and pulmonary hypertension.5,6
CLINICAL PRESENTATION
Retraction of the chest wall develops as obstruction progresses. Retraction is less prominent in older children, as the chest wall is more stable. As obstruction worsens, the work of breathing increases and the accessory muscles become active. The alae nasi (vestigial muscles of ventilation) begin to flare. Fever increases minute volume and magnifies any degree of obstruction. Whereas infants and older children can maintain an increased work of breathing, premature infants and neonates rapidly fatigue, and may develop apnoeic episodes.7,8
Auscultation over the neck and larynx may identify the site of obstruction. A foreign body in the airway may produce a mechanical or slapping sound. Decreased or absent breath sounds may occur with greater degrees of obstruction. Chronic URTO is a cause of failure to thrive, chest deformity (pectus excavatum) and cor pulmonale.5,6 Some infants present with recurrent chest infections. Abnormal posturing (head retraction) may also be a feature, particularly in infants.
AETIOLOGY
A classification of the causes of URTO is presented in Table 97.1. The neonatal causes are predominantly due to congenital structural lesions. Acute inflammatory lesions, foreign bodies and trauma predominate in older infants and children.
| Level | Newborn | Older infant and child |
|---|---|---|
| Nasal | Choanal atresia | |
| Oropharyngeal | Facial malformations (e.g. Pierre Robin syndrome, Treacher Collins syndrome) | Macroglossia/postglossectomyAngioedema |
| Macroglossia | Retropharyngeal abscess | |
| Cystic hygroma | Tonsillar and adenoidal hypertrophy | |
| Vallecular cyst | Obstructive sleep apnoea | |
| Laryngeal | Infantile larynx | Acute laryngotracheobronchitis (croup) |
| Bilateral vocal cord palsy | Bacterial tracheitis | |
| Congenital subglottic stenosis | Acute epiglottitis | |
| Subglottic haemangioma | Postintubation oedema and stenosis | |
| Laryngeal web | Laryngeal papillomata | |
| Laryngeal cysts | Laryngeal foreign body | |
| Inhalation burns | ||
| Caustic ingestion | ||
| External trauma | ||
| Tracheal | Tracheomalacia | Foreign body |
| Vascular ring | Anterior mediastinal tumours (e.g. lymphoma) | |
DIAGNOSIS
The cause of URTO can often be determined from the history and clinical features. Radiographic examination of the upper and lower airways with anteroposterior and lateral views may show soft-tissue swelling or the presence of foreign bodies.9 Air shadows may indicate fixed stenotic or compressive lesions. In children with significant respiratory distress, these investigations should be undertaken in the intensive care unit (ICU) rather than the radiology department.
Previously, barium swallow and aortography have been used to confirm the diagnosis of vascular compression of the trachea. Computed tomography (CT) has assumed importance in the assessment of fixed lesions such as intrinsic stenosis and extrinsic compression. Echocardiography, magnetic resonance imaging (MRI) and CT with contrast are useful to assess vascular anomalies.10 Tracheobronchography may provide excellent anatomical delineation of the proximal tracheobronchial tree and allow dynamic assessment of airway calibre.
Direct visualisation of the airway may be necessary, and may also prove therapeutic (e.g. removal of a foreign body). Nasoscopy, flexible fibreoptic and rigid laryngoscopy and bronchoscopy all have a place in assessing the paediatric airway. Investigation of the child’s airway should only be undertaken in specialised centres by experienced endoscopists, radiologists and anaesthetists.
SPECIFIC AIRWAY OBSTRUCTION
MANAGEMENT
RELIEF OF AIRWAY OBSTRUCTION
All but the mildest cases require insertion of an artificial airway under anaesthesia (see below). Nasotracheal intubation is the optimal management,11 although, depending on the available personnel, tracheostomy is a satisfactory alternative. Anaesthesia for relief of airway obstruction is described below. A tube of size appropriate for age is chosen (see Chapter 104). Extubation can be undertaken when fever subsides and the child no longer appears toxic. Most cases can be extubated in less than 18 hours. Only those complicated by pulmonary oedema, pneumonia or cerebral hypoxia (from delayed therapy) will require intubation for longer than 24 hours. It is not necessary to re-examine the larynx prior to extubation. Nebulised adrenaline (epinephrine) is of no benefit in this condition and may aggravate the situation.12 Pulmonary oedema, when it occurs, is due to airway obstruction, septicaemia and increased lung capillary permeability.3,13,14 It is managed according to conventional principles.
CROUP
Three subgroups are recognised: viral croup, spasmodic croup and bacterial tracheitis.
VIRAL CROUP
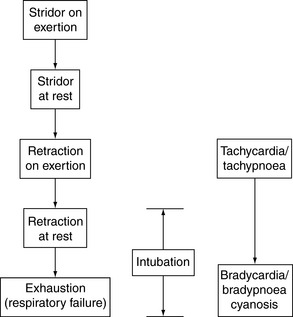
Viral croup, most commonly due to parainfluenza virus, respiratory syncytial virus and rhinovirus, is characterised by a coryzal prodrome, low-grade fever, harsh barking (croupy) cough and hoarse voice. Progression of airway obstruction in severe cases is shown in Figure 97.2.
SPASMODIC CROUP
Spasmodic or recurrent croup occurs in children with an allergic predisposition.15,16 It usually develops suddenly, often at night, and without prodromal symptoms. Endoscopy reveals pale, watery oedema of the subglottic mucosa. Such children probably represent part of the asthma spectrum, and wheeze, due to small airway flow limitation, may be a feature.
BACTERIAL TRACHEITIS
Bacterial tracheitis is uncommon but should be suspected in children exhibiting the usual features of croup, but accompanied by high fever, leukocytosis and copious purulent secretions.17 There is a greater risk of sudden, severe obstruction from purulent secretions. Staphylococcus aureus is usually the cause, although H. influenzae and group A Streptococcus have also been isolated in some cases.
MANAGEMENT
Corticosteroids have dramatically reduced the need for intubation in children with croup. They are effective in both viral and spasmodic croup.18,19 Steroids will also shorten the duration of intubation and increase the success rate of extubation.20,21 The dose of dexamethasone is 0.6 mg/kg statim (maximum dose 10 mg) followed, if necessary, by 0.15 mg/kg 6-hourly. In very distressed children, it is best administered i.m. or i.v. to ensure absorption. Inhaled steroids are also effective in milder cases.22
Humidification of inspired gases was the mainstay of supportive care for decades. Controlled studies showing efficacy are lacking. A study by Bourchier et al. failed to demonstrate benefit and its use has been abandoned in many centres.23
Nebulised adrenaline will usually provide temporary relief of acute obstruction.24 Historically, racemic adrenaline (2.25% solution, i.e. 1:88 L-adrenaline), developed for use in asthma, was employed. Indications for adrenaline nebulisation are:
Mechanical relief of airway obstruction: this requirement has been greatly reduced by early use of steroids. Increasing tachycardia, tachypnoea and restlessness indicate the need for tracheal intubation. An SaO2 persistently less than 90% is another reason for concern. It is important not to wait for the development of bradycardia, bradypnoea, cyanosis, exhaustion and respiratory failure. Blood gases are not a useful guide for intubation. Nasotracheal intubation is preferred. An orotracheal tube, size (inner diameter) 1 mm less than that predicted by age (Table 97.2) is first inserted under anaesthesia (see below). A stylet through the tube is recommended to overcome the resistance of the subglottic region. The tube is changed to a nasotracheal tube immediately after clearance of secretions.
| Age | Size |
|---|---|
| Less than 6 months | 3.0 mm |
| 6 months to 2 years | 3.5 mm |
| 2–5 years | 4.0 mm |
| Over 5 years | 4.5 mm |
TONSILLAR AND ADENOIDAL AIRWAY OBSTRUCTION
The contemporary conservative surgical approach to tonsillectomy and adenoidectomy has led to an increased incidence of hypertrophy and untreated chronic upper-airway obstruction.25 Such children may present with severe, acute exacerbations due to intercurrent infection (e.g. tonsillitis). They may present in a toxic state with drooling, thereby mimicking acute epiglottitis. Obstruction is most marked during sleep. In the most severe cases, it may be necessary to relieve the obstruction with a nasotracheal tube or a nasopharyngeal tube positioned beyond the tonsillar bed. Tonsillectomy and adenoidectomy are generally contraindicated in the acute phase, because of increased risk of bleeding, but are performed when infection has settled.
OBSTRUCTIVE SLEEP APNOEA SYNDROME
Obstructive sleep apnoea (OSA) syndrome is characterised by intermittent upper-airway obstruction during sleep, with heavy snoring, stertorous breathing and an abnormal, irregular respiratory pattern.26 Frequent episodes of chest-wall motion with inadequate airflow (hypopnoea) or absent airflow (obstructive apnoea) are a feature. These episodes are most frequent during rapid eye movement sleep. They are accompanied by variable degrees of oxygen desaturation. OSA may be associated with enlarged tonsils and adenoids, a large uvula or long soft palate, macroglossia, retrognathia or various neurological disorders. Obesity is a common finding.
If OSA is severe and protracted, cardiac and pulmonary decompensation may occur. Chronic hypoxia and hypercarbia lead to pulmonary hypertension and cor pulmonale.5,6 There may also be evidence of left ventricular failure and pulmonary oedema. Urgency of treatment is dictated by the mode of presentation. Critically ill children may require immediate relief of airway obstruction (nasopharyngeal or nasotracheal tube), oxygen therapy and diuretics. Antibiotics are indicated if there is bacterial superinfection. Surgical intervention is required after stabilisation. Tonsillectomy and adenoidectomy are often dramatically beneficial. They are best removed even when not grossly enlarged. Postoperative observation in a paediatric ICU or high-dependency unit is required for those with severe OSA. Other surgical procedures, such as uvulopalatopharyngoplasty or tracheostomy, may be required when this fails. The use of nocturnal continuous positive airway pressure (CPAP) is an option in long-standing, refractory conditions, e.g. neurological disorders. It is often not feasible because it is difficult to interface CPAP masks in young and uncooperative children.
PIERRE ROBIN SYNDROME
This sequence consists of a posterior cleft palate, retrognathia and relative macroglossia. It is the cause of airway obstruction, feeding difficulties and failure to thrive in the newborn. Differential growth eventually reduces the significance of the deformity. Acute airway obstruction may be relieved by nursing the infant in the prone position, by passage of a nasopharyngeal tube or insertion of a laryngeal mask airway.27 Occasionally, nasotracheal intubation or tracheostomy is required. Tongue–lip anastomosis has been used in the past but is now rarely performed.
CYSTIC HYGROMA
Although often conspicuous at birth, cystic hygroma is a relatively rare cause of upper-airway obstruction in infancy. The tumours consist of masses of dilated lymphatic channels. They usually occur in the neck and may involve tissues of the tongue and larynx. Occasionally, extension into the mediastinum occurs. Airway obstruction may be due to infection or haemorrhage into the lesion. Surgical excision has been the mainstay of treatment, although complete removal is difficult and recurrence is common. Treatment using sclerosing therapy is now used. Compounds used include bleomycin emulsion or OK 432.28,29 OK 432 is produced by lyophilisation of cultures of a low virulent strain of group A Streptococcus pyogenes (human origin). In severe cases, long-term tracheostomy is required.
FOREIGN BODY OR CHOKING
The technique for removal of a pharyngolaryngeal foreign body without equipment in infants and children is controversial and difficult. The American Academy of Paediatrics has made recommendations to cover various ages.30 Gravity should be utilised by placing the child prone, straddled over the arm with the head down and a hand supporting the jaw. Four back blows between the shoulder blades should be administered. If this fails, chest thrusts or finger sweep across the pharynx should be attempted. There is some risk that the latter manoeuvre may impact the foreign body in the larynx. Abdominal thrusts (the Heimlich manoeuvre) are not recommended in infants but may be useful in children older than 1 year. Expired air resuscitation should be attempted in an emergency, although the risk of gastric distension is great. The best method of removal is extraction under direct vision using a laryngoscope, forceps, suction or a finger.
ANTERIOR MEDIASTINAL TUMOURS
Anterior mediastinal tumours, such as lymphoma, may compress the trachea or bronchi, causing symptoms such as dry cough, stridor or wheeze. Airway compression may become severe enough to cause hyperinflation or atelectasis. Pleural effusions are common and may add to the respiratory distress. This is a high-risk situation. Symptoms may be aggravated by the supine position, especially during anaesthesia for a biopsy procedure. This is likely in patients with superior vena caval syndrome. Postural symptoms or findings on flow–volume loops may allude to this risk. Echocardiography may also provide evidence of cardiac compression which increases the risks associated with anaesthesia. Sudden complete obstruction that cannot be bypassed by a standard tracheal tube has been described. The use of armoured tubes or a rigid bronchoscope may be required. Consideration should be given to leaving the tracheal tube in situ postoperatively until corticosteroids and chemotherapy reduce the tumour mass.
ANAESTHESIA FOR RELIEF OF AIRWAY OBSTRUCTION
CRICOTHYROTOMY
A wide-bore plastic i.v. cannula (14- or 16-gauge) passed into the trachea via the cricothyroid membrane may be life-saving if alternative procedures are unavailable. This should be performed with the neck extended as for tracheostomy. A system of connection to a low-pressure oxygen supply must be planned in advance. One method is to attach the hub of the cannula to the sleeve of a plastic 2–3 ml syringe (without plunger) to an adaptor from a 7.5 mm outer diameter tracheal tube, and then to a breathing circuit (e.g. Jackson Rees modification of Ayres T-piece). Jet ventilation has also been performed through a narrow cannula in this situation.
1 Westhorpe RN. The position of the larynx in children and its relationship to the ease of intubation. Anaesth Intensive Care. 1987;15:384-388.
2 Badgwell JM, McLeod ME, Friedberg J. Airway obstruction in infants and children. Can J Anaesth. 1987;34:90-98.
3 Sofer S, Bar-Ziv J, Scharf SM. Pulmonary edema following relief of upper airway obstruction. Chest. 1984;86:401-403.
4 Stalcup SA, Mellins RB. Mechanical forces producing pulmonary edema in acute asthma. N Engl J Med. 1977;297:592-596.
5 Cox MA, Schiebler GL, Taylor WJ, et al. Reversible pulmonary hypertension in a child with respiratory obstruction and cor pulmonale. J Pediatr. 1965;67:192-197.
6 Luke MJ, Mehrizi A, Folger GM, et al. Chronic nasopharyngeal obstruction as a cause of cardiomegaly, cor pulmonale, and pulmonary oedema. Paediatrics. 1966;37:762-768.
7 Keens TG, Bryan AC, Levinson H, et al. Development pattern of muscle fibre types in human ventilatory muscles. J Appl Physiol Respir Environ Exercise Physiol. 1978;44:909-913.
8 Muller NL, Bryan AC. Chest wall mechanics and respiratory muscles in infants. Pediatr Clin North Am. 1979;26:503-516.
9 Kushner DC, Harris GBC. Obstructing lesions of the larynx and trachea in infants and children. Radiol Clin North Am. 1978;16:181-194.
10 Siegel MJ, Nadel SN, Glazer HS, et al. Mediastinal lesions in children. Comparison of CT and MR. Radiology. 1986;160:241-244.
11 Butt W, Shann F, Walker C, et al. Acute epiglottitis: a different approach to management. Crit Care Med. 1988;16:43-47.
12 Kissoon N, Mitchell I. Adverse effects of racemic epinephrine in epiglottitis. Pediatr Emerg Care. 1985;1:143-144.
13 Soliman MG, Richer P. Epiglottitis and pulmonary oedema in children. Can Anaesth Soc J. 1978;25:270-275.
14 Travis KW, Todres DI, Shannon DC. Pulmonary edema associated with croup and epiglottitis. Pediatrics. 1978;59:695-698.
15 Zach M, Erben E, Olinsky A. Croup, recurrent croup, allergy and airways hyper-reactivity. Arch Dis Child. 1981;56:336-341.
16 Zach MS, Schnall RP, Landau LI. Upper and lower airway hyper-reactivity in recurrent croup. Am Rev Respir Dis. 1980;121:979-983.
17 Jones R, Santos JI, Overall JC. Bacterial tracheitis. JAMA. 1979;242:721-726.
18 Super DM, Cartelli NA, Brooks LJ, et al. A prospective randomized double-blind study to evaluate the effect of dexamethasone in acute laryngo-tracheitis. J Pediatr. 1989;115:323-329.
19 Koren G, Frand M, Barzilay Z, et al. Corticosteroid treatment of laryngotracheitis in spasmodic croup in children. Am J Dis Child. 1983;137:941-944.
20 Tibballs J, Shann FA, Landau FI. Placebo controlled trial of prednisolone in children intubated for croup. Lancet. 1992;340:745-748.
21 Freezer N, Butt W, Phelan P. Steroids in croup: do they increase the incidence of successful extubation? Anaesth Intensive Care. 1990;18:224-228.
22 Klassen TP, Feldman ME, Watters LK, et al. Nebulized budesonide for children with mild to moderate croup. N Engl J Med. 1994;331:285-289.
23 Bourchier D, Dawson KP, Fergusson DM. Humidification in viral croup: a controlled trial. Aust Paediatr. 1984;20:289-291.
24 Jordan WS, Graves CL, Elwyn RA. New therapy for postintubation laryngeal edema and tracheitis in children. JAMA. 1970;212:585-588.
25 Check WA. Does drop in tonsillectomies and adenoidectomies pose new issue of adeno-tonsillar hypertrophy? JAMA. 1982;247:1229-1230.
26 Guilleminault C, Tilkian A, Dement WA. The sleep apnea syndromes. Ann Rev Med. 1976;27:465-484.
27 Heaf DP, Helms PJ, Dinwiddie MB, et al. Nasopharyngeal airways in Pierre Robin syndrome. J Pediatr. 1982;100:698-703.
28 Tanaka K, Inomata Y, Utsunomiya H, et al. Sclerosing therapy with bleomycin emulsion for lymphangioma in children. Pediatr Surg Int. 1990;5:270-273.
29 Samuel M, McCarthy L, Boddy SA. Efficacy and safety of OK-432 sclerotherapy for giant cystic hygroma in a newborn. Fetal Diagnosis Ther. 2000;15:93-96.
30 American Academy of Pediatrics Committee on Accident and Poison Prevention. First aid for the choking child. Pediatrics, 81. 1988, 740-742.