7
Upper Limb
Gateways to the posterior scapular region
Gateways in the posterior wall
Anterior compartment of the forearm
Posterior compartment of forearm
Carpal tunnel and structures at the wrist
ADDITIONAL LEARNING RESOURCES FOR CHAPTER 7, UPPER LIMB, ON STUDENT CONSULT (www.studentconsult.com)
 Image Library—illustrations of upper limb anatomy, Chapter 7
Image Library—illustrations of upper limb anatomy, Chapter 7
 Self-Assessment (scored)—National Board style multiple-choice questions, Chapter 7
Self-Assessment (scored)—National Board style multiple-choice questions, Chapter 7
 Short Questions (not scored)—National Board style multiple-choice questions, Chapter 7
Short Questions (not scored)—National Board style multiple-choice questions, Chapter 7
 Interactive Surface Anatomy—interactive surface animations, Chapter 7
Interactive Surface Anatomy—interactive surface animations, Chapter 7
Upper quarter screening examination
See more PT Case Studies online
Extensor tendon injury of the hand
See more Medical Clinical Case Studies online
Regional anatomy
Based on the position of its major joints, the upper limb is divided into shoulder, arm, forearm, and hand (Fig. 7.1):
 The arm is between the shoulder and the elbow joint. The bone of the arm is the humerus.
The arm is between the shoulder and the elbow joint. The bone of the arm is the humerus.
Fig. 7.1 Anterior view of the upper limb.
The major function of the upper limb is to position the hand in space for use as a mechanical and sensory tool.
Unlike the lower limb, which is used for support, stability, and locomotion, the upper limb is designed to be flexible. The shoulder is suspended from the trunk predominantly by muscles and can therefore be moved relative to the body. Sliding (protraction and retraction) and rotating the scapula on the thoracic wall changes the position of the glenohumeral joint (shoulder joint) and extends the reach of the hand (Fig. 7.2). The glenohumeral joint allows the arm to move around three axes with a wide range of motion. Movements of the arm at this joint are flexion, extension, abduction, adduction, medial rotation (internal rotation), lateral rotation (external rotation), and circumduction (Fig. 7.3).
Fig. 7.2 Movements of the scapula. A. Rotation. B. Protraction and retraction.
Fig. 7.3 Movements of the arm at the glenohumeral joint.
The major movements at the elbow joint are flexion and extension of the forearm (Fig. 7.4A). At the other end of the forearm, the distal end of the lateral bone, the radius, can be flipped over the adjacent head of the medial bone, the ulna. Because the hand is articulated with the radius, it can be efficiently moved from a palm-anterior position to a palm-posterior position simply by crossing the distal end of the radius over the ulna (Fig. 7.4B). This movement, termed pronation, occurs solely in the forearm. Supination returns the hand to the anatomical position.
Fig. 7.4 Movements of the forearm. A. Flexion and extension at the elbow joint. B. Pronation and supination.
At the wrist joint, the hand can be abducted, adducted, flexed, extended, and circumducted (Fig. 7.5). These movements, combined with those of the shoulder, arm, and forearm, enable the hand to be placed in a wide range of positions relative to the body.
Fig. 7.5 Movements of the hand at the wrist joint.
The thumb is positioned at right angles to the orientation of the index, middle, ring, and little fingers (Fig. 7.6). As a result, movements of the thumb occur at right angles to those of the other digits. For example, flexion brings the thumb across the palm, whereas abduction moves it away from the fingers at right angles to the palm (Fig. 7.6A,B).
Fig. 7.6 A–C. Movements of the thumb.
Importantly, with the thumb positioned at right angles to the palm. Only a slight rotation of the thumb brings it into a position directly facing the other fingers (Fig. 7.6C). This opposition of the thumb is essential for normal hand function.
SHOULDER
The bone framework of the shoulder consists of:
 the clavicle and scapula, which form the pectoral girdle (shoulder girdle), and
the clavicle and scapula, which form the pectoral girdle (shoulder girdle), and
 the proximal end of the humerus.
the proximal end of the humerus.
The superficial muscles of the shoulder consist of the trapezius and deltoid muscles, which together form the smooth muscular contour over the lateral part of the shoulder. These muscles connect the scapula and clavicle to the trunk and to the arm, respectively.
Bones
Clavicle
The clavicle is the only bony attachment between the trunk and the upper limb. It is palpable along its entire length and has a gentle S-shaped contour, with the forward-facing convex part medial and the forward-facing concave part lateral. The acromial (lateral) end of the clavicle is flat, whereas the sternal (medial) end is more robust and somewhat quadrangular in shape (Fig. 7.7).
Fig. 7.7 Right clavicle.
The acromial end of the clavicle has a small oval facet on its surface for articulation with a similar facet on the medial surface of the acromion of the scapula.
The sternal end has a much larger facet for articulation mainly with the manubrium of the sternum, and to a lesser extent, with the first costal cartilage.
The inferior surface of the lateral third of the clavicle possesses a distinct tuberosity consisting of a tubercle (the conoid tubercle) and lateral roughening (the trapezoid line), for attachment of the important coracoclavicular ligament.
In addition, the surfaces and margins of the clavicle are roughened by the attachment of muscles that connect the clavicle to the thorax, neck, and upper limb. The superior surface is smoother than the inferior surface.
Scapula
The scapula is a large, flat triangular bone with (Fig. 7.8):
 three angles (lateral, superior, and inferior);
three angles (lateral, superior, and inferior);
 three borders (superior, lateral, and medial);
three borders (superior, lateral, and medial);
 two surfaces (costal and posterior); and
two surfaces (costal and posterior); and
 three processes (acromion, spine, and coracoid process)
three processes (acromion, spine, and coracoid process)
Fig. 7.8 Scapula. A. Posterior view of right scapula. B. Anterior view of costal surface. C. Lateral view.
The lateral angle of the scapula is marked by a shallow, somewhat comma-shaped glenoid cavity, which articulates with the head of the humerus to form the glenohumeral joint (Fig. 7.8B,C).
A large triangular-shaped roughening (the infraglenoid tubercle) inferior to the glenoid cavity is the site of attachment for the long head of the triceps brachii muscle (Fig. 7.8B,C).
A less distinct supraglenoid tubercle is located superior to the glenoid cavity and is the site of attachment for the long head of the biceps brachii muscle (Fig. 7.8C).
A prominent spine subdivides the posterior surface of the scapula into a small, superior supraspinous fossa and a much larger, inferior infraspinous fossa (Fig. 7.8A).
The acromion, which is an anterolateral projection of the spine, arches over the glenohumeral joint and articulates, via a small oval facet on its distal end, with the clavicle (Fig. 7.8B).
The region between the lateral angle of the scapula and the attachment of the spine to the posterior surface of the scapula is the greater scapular notch (spinoglenoid notch) (Fig. 7.8A).
Unlike the posterior surface, the costal surface of the scapula is unremarkable, being characterized by a shallow concave subscapular fossa over much of its extent (Fig. 7.8B). The costal surface and margins provide for muscle attachment, and the costal surface, together with its related muscle (subscapularis), moves freely over the underlying thoracic wall.
The lateral border of the scapula is strong and thick for muscle attachment, whereas the medial border and much of the superior border is thin and sharp.
The superior border is marked on its lateral end by:
 the coracoid process (Fig. 7.8B,C), a hooklike structure that projects anterolaterally and is positioned directly inferior to the lateral part of the clavicle; and
the coracoid process (Fig. 7.8B,C), a hooklike structure that projects anterolaterally and is positioned directly inferior to the lateral part of the clavicle; and
 the small but distinct suprascapular notch (Fig. 7.8A), which lies immediately medial to the root of the coracoid process.
the small but distinct suprascapular notch (Fig. 7.8A), which lies immediately medial to the root of the coracoid process.
The spine and acromion can be readily palpated on a patient, as can the tip of the coracoid process, the inferior angle, and much of the medial border of the scapula.
Proximal humerus
The proximal end of the humerus consists of the head, the anatomical neck, the greater and lesser tubercles, the surgical neck, and the superior half of the shaft of humerus (Fig. 7.9).
Fig. 7.9 Proximal end of right humerus.
The head is half-spherical in shape and projects medially and somewhat superiorly to articulate with the much smaller glenoid cavity of the scapula.
The anatomical neck is very short and is formed by a narrow constriction immediately distal to the head. It lies between the head and the greater and lesser tubercles laterally, and between the head and the shaft more medially.
Greater and lesser tubercles
The greater and lesser tubercles are prominent landmarks on the proximal end of the humerus and serve as attachment sites for the four rotator cuff muscles of the glenohumeral joint (Fig. 7.9).
The greater tubercle is lateral in position. Its superior surface and posterior surface are marked by three large smooth facets for muscle tendon attachment (Fig. 7.9):
 The superior facet is for attachment of the supraspinatus muscle.
The superior facet is for attachment of the supraspinatus muscle.
 The middle facet is for attachment of infraspinatus.
The middle facet is for attachment of infraspinatus.
 The inferior facet is for attachment of teres minor.
The inferior facet is for attachment of teres minor.
The lesser tubercle is anterior in position and its surface is marked by a large smooth impression for attachment of the subscapularis muscle.
A deep intertubercular sulcus (bicipital groove) separates the lesser and greater tubercles and continues inferiorly onto the proximal shaft of the humerus (Fig. 7.9). The tendon of the long head of the biceps brachii passes through this sulcus.
Roughenings on the lateral and medial lips and on the floor of the intertubercular sulcus mark sites for the attachment of the pectoralis major, teres major, and latissimus dorsi muscles, respectively.
The lateral lip of the intertubercular sulcus is continuous inferiorly with a large V-shaped deltoid tuberosity on the lateral surface of the humerus midway along its length (Fig. 7.9), which is where the deltoid muscle inserts onto the humerus.
In approximately the same position, but on the medial surface of the bone, there is a thin vertical roughening for attachment of the coracobrachialis muscle.
Surgical neck
One of the most important features of the proximal end of the humerus is the surgical neck (Fig. 7.9). This region is oriented in the horizontal plane between the expanded proximal part of the humerus (head, anatomical neck, and tubercles) and the narrower shaft. The axillary nerve and the posterior circumflex humeral artery, which pass into the deltoid region from the axilla, do so immediately posterior to the surgical neck. Because the surgical neck is weaker than more proximal regions of the bone, it is one of the sites where the humerus commonly fractures.
Clinical app
Fracture of the proximal humerus
Typically, fractures occur around the surgical neck of the humerus. Although the axillary nerve and posterior circumflex humeral artery may be damaged with this type of fracture, this rarely happens. However, it is important that the axillary nerve is tested to be sure that the injury has not damaged the nerve and that the treatment itself does not cause a neurological deficit.
Joints
The three joints in the shoulder complex are the sternoclavicular, acromioclavicular, and glenohumeral joints.
The sternoclavicular joint and the acromioclavicular joint link the two bones of the pectoral girdle to each other and to the trunk. The combined movements at these two joints enable the scapula to be positioned over a wide range on the thoracic wall, substantially increasing “reach” by the upper limb.
The glenohumeral joint (shoulder joint) is the articulation between the humerus of the arm and the scapula.
Sternoclavicular joint
The sternoclavicular joint occurs between the proximal end of the clavicle and the clavicular notch of the manubrium of sternum together with a small part of the first costal cartilage (Fig. 7.10, 7.11). It is synovial and saddle-shaped. The articular cavity is completely separated into two compartments by an articular disc. The sternoclavicular joint allows movement of the clavicle, predominantly in the anteroposterior and vertical planes, although some rotation also occurs.
Fig. 7.10 Sternoclavicular joint.
Imaging app
Visualizing the sternoclavicular joint
Fig. 7.11 Anterior view of normal sternoclavicular joints. Volume-rendered reconstruction using multidetector computed tomography.
The sternoclavicular joint is surrounded by a joint capsule and is reinforced by four ligaments (Fig. 7.10):
Acromioclavicular joint
The acromioclavicular joint is a small synovial joint between an oval facet on the medial surface of the acromion and a similar facet on the acromial end of the clavicle (Figs. 7.12; 7.13). It allows movement in the anteroposterior and vertical planes together with some axial rotation.
Fig. 7.12 Right acromioclavicular joint.
Imaging app
Visualizing the acromioclavicular joint
Fig. 7.13 Radiograph of a normal right acromioclavicular joint (anteroposterior view).
The acromioclavicular joint is surrounded by a joint capsule and is reinforced by (Fig. 7.12):
Glenohumeral joint
The glenohumeral joint is a synovial ball and socket articulation between the head of the humerus and the glenoid cavity of the scapula (Fig. 7.14; see Fig. 7.15). It is multiaxial with a wide range of movements provided at the cost of skeletal stability. Joint stability is provided instead by the rotator cuff muscles, the long head of the biceps brachii muscle, related bony processes, and extracapsular ligaments.
Fig. 7.14 Articular surfaces of right glenohumeral joint.
The articular surfaces of the glenohumeral joint are the large spherical head of the humerus and the small glenoid cavity of the scapula (Fig. 7.14).
The glenoid cavity is deepened and expanded peripherally by a fibrocartilaginous collar (the glenoid labrum), which attaches to the margin of the fossa (Fig. 7.14). Superiorly, this labrum is continuous with the tendon of the long head of the biceps brachii muscle, which attaches to the supraglenoid tubercle and passes through the articular cavity superior to the head of the humerus.
The synovial membrane attaches to the margins of the articular surfaces and lines the fibrous membrane of the joint capsule (Fig. 7.16). The synovial membrane is loose inferiorly. This redundant region of synovial membrane and related fibrous membrane accommodates abduction of the arm.
Fig. 7.16 Synovial membrane and joint capsule of right glenohumeral joint.
The synovial membrane protrudes through apertures in the fibrous membrane to form bursae, which lie between the tendons of surrounding muscles and the fibrous membrane. The most consistent of these is the subtendinous bursa of subscapularis (Figs. 7.16, 7.17), which lies between the subscapularis muscle and the fibrous membrane. The synovial membrane also folds around the tendon of the long head of the biceps brachii muscle in the joint and extends along the tendon as it passes into the intertubercular sulcus (Figs. 7.16, 7.18). All these synovial structures reduce friction between the tendons and adjacent joint capsule and bone.
Fig. 7.18 Capsule of right glenohumeral joint.
In addition to bursae that communicate with the articular cavity through apertures in the fibrous membrane, other bursae are associated with the joint but are not connected to it. These occur:
 between the acromion (or deltoid muscle) and supraspinatus muscle (or joint capsule) (the subacromial or subdeltoid bursa) (Fig. 7.17);
between the acromion (or deltoid muscle) and supraspinatus muscle (or joint capsule) (the subacromial or subdeltoid bursa) (Fig. 7.17);
 between the acromion and skin;
between the acromion and skin;
 between the coracoid process and the joint capsule; and
between the coracoid process and the joint capsule; and
The fibrous membrane of the joint capsule attaches to the margin of the glenoid cavity, outside the attachment of the glenoid labrum and the long head of the biceps brachii muscle, and to the anatomical neck of the humerus (Fig. 7.18).
Openings in the fibrous membrane provide continuity of the articular cavity with bursae that occur between the joint capsule and surrounding muscles and around the tendon of the long head of the biceps brachii muscle in the intertubercular sulcus.
The fibrous membrane of the joint capsule is thickened (Fig. 7.18):
Joint stability is provided by surrounding muscle tendons and a skeletal arch formed superiorly by the coracoid process and acromion and the coraco-acromial ligament (Fig. 7.17).
Imaging app
Visualizing the rotator cuff muscles
Fig. 7.19 Magnetic resonance image (T1-weighted) of a normal glenohumeral joint in the sagittal plane.
Tendons of the rotator cuff muscles (the supraspinatus, infraspinatus, teres minor, and subscapularis muscles) blend with the joint capsule and form a musculotendinous collar that surrounds the posterior, superior, and anterior aspects of the glenohumeral joint (see Figs. 7.17; 7.19). This cuff of muscles stabilizes and holds the head of the humerus in the glenoid cavity of the scapula without compromising the arm’s flexibility and range of motion. The tendon of the long head of the biceps brachii muscle passes superiorly through the joint and restricts upward movement of the humeral head on the glenoid cavity.
Vascular supply to the glenohumeral joint is predominantly through branches of the anterior and posterior circumflex humeral and suprascapular arteries.
The glenohumeral joint is innervated by branches from the posterior cord of the brachial plexus, and from the suprascapular, axillary, and lateral pectoral nerves.
Clinical app
Fractures of the clavicle and dislocations of the acromioclavicular and sternoclavicular joints
The clavicle is often fractured because of its small size and the large forces that it often transmits from the upper limb to the trunk. The typical site of fracture is the middle third (Fig. 7.20), proximal to the attachment of the coracoclavicular ligament.
Fig. 7.20 Radiograph showing an oblique fracture of the middle third of the right clavicle.
The acromial end of the clavicle tends to dislocate at the acromioclavicular joint with trauma (Fig. 7.21). A minor injury tends to tear the fibrous joint capsule and ligaments of the acromioclavicular joint, resulting in acromioclavicular separation on a plain radiograph. More severe trauma will disrupt the conoid and trapezoid ligaments of the coracoclavicular ligament, which results in elevation and upward subluxation of the clavicle.
Fig. 7.21 Radiograph of dislocated right acromioclavicular joint.
The typical injury at the medial end of the clavicle is an anterior or posterior dislocation of the sternoclavicular joint. Importantly, a posterior dislocation of the clavicle may impinge on the great vessels and compress or disrupt them.
Clinical app
Dislocations of the glenohumeral joint
The glenohumeral joint is extremely mobile, providing a wide range of movement at the expense of stability. The relatively small bony glenoid cavity, supplemented by the less robust fibrocartilaginous glenoid labrum and the ligamentous support, make it susceptible to dislocation.
Anteroinferior dislocation (Fig. 7.22) occurs most frequently and is usually associated with an isolated traumatic incident (clinically, all anterior dislocations are anteroinferior). In some cases, the anteroinferior glenoid labrum is torn with or without a small bony fragment. Once the joint capsule and cartilage are disrupted, the joint is susceptible to further (recurrent) dislocations. When an anteroinferior dislocation occurs, the axillary nerve may be injured by direct compression of the humeral head on the nerve inferiorly as it passes through the quadrangular space. Furthermore, the “lengthening” effect of the humerus may stretch the radial nerve, which is tightly bound within the radial groove, and produce a radial nerve paralysis. Occasionally, an anteroinferior dislocation is associated with a fracture. Posterior dislocation is extremely rare.
Fig. 7.22 Radiograph showing an anteroinferior dislocation of the shoulder joint.
Clinical app
Rotator cuff disorders
The two main disorders of the rotator cuff are impingement and tendinopathy. The muscle most commonly involved is supraspinatus as it passes beneath the acromion and the acromioclavicular ligament. This space, beneath which the supraspinatus tendon passes, is of fixed dimensions. Swelling of the supraspinatus muscle, excessive fluid within the subacromial/subdeltoid bursa, or subacromial bony spurs may produce significant impingement when the arm is abducted.
The blood supply to the supraspinatus tendon is relatively poor. Repeated trauma, in certain circumstances, makes the tendon susceptible to degenerative change, which may result in calcium deposition, producing extreme pain.
When the supraspinatus tendon has undergone significant degenerative change, it is further susceptible to trauma and partial- or full-thickness tears may develop (Fig. 7.23). These tears are most common in older patients and may result in considerable difficulty in carrying out normal activities of daily living such as combing hair. However, complete tears may be entirely asymptomatic.
Muscles
The two most superficial muscles of the shoulder are the trapezius and deltoid muscles (Table 7.1, Fig. 7.24). Together, they provide the characteristic contour of the shoulder:
 The trapezius attaches the scapula and clavicle to the trunk.
The trapezius attaches the scapula and clavicle to the trunk.
 The deltoid attaches the scapula and clavicle to the humerus.
The deltoid attaches the scapula and clavicle to the humerus.
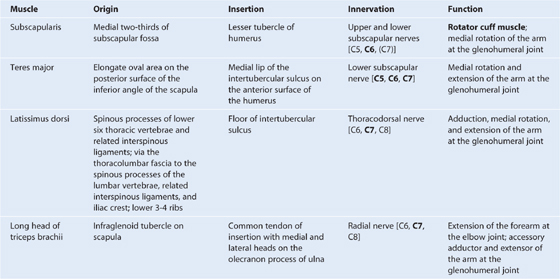
Table 7.1 Muscles of the shoulder (spinal segments indicated in bold are the major segments innervating the muscle)
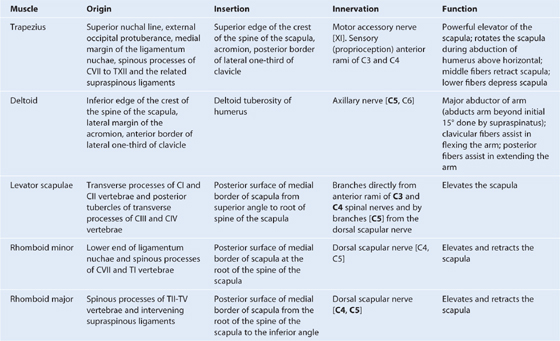
Fig. 7.24 Attachment and neurovascular supply of the trapezius and deltoid muscles.
Both the trapezius and deltoid are attached to opposing surfaces and margins of the spine of the scapula, the acromion, and the clavicle and these structures can be palpated between the attachments of trapezius and deltoid.
Deep to the trapezius the scapula is attached to the vertebral column by three muscles—the levator scapulae, rhomboid minor, and rhomboid major (Table 7.1, Fig. 7.24). These three muscles work with the trapezius (and with muscles found anteriorly) to position the scapula on the trunk.
POSTERIOR SCAPULAR REGION
The posterior scapular region occupies the posterior aspect of the scapula and is located deep to the trapezius and deltoid muscles. It contains four muscles, which pass between the scapula and proximal end of the humerus: the supraspinatus, infraspinatus, teres minor, and teres major muscles (Table 7.2, Fig. 7.25).
Table 7.2 Muscles of the posterior scapular region (spinal segments indicated in bold are the major segments innervating the muscle)
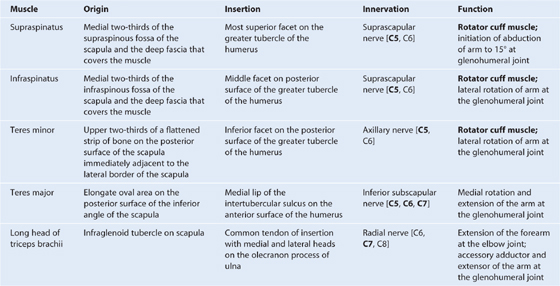
Fig. 7.25 Right posterior scapular region.
The posterior scapular region also contains part of one additional muscle, the long head of the triceps brachii, which passes between the scapula and the proximal end of the arm (Fig. 7.25). The importance of the triceps brachii in the posterior scapular region is that its vertical course between the teres minor and teres major, together with these muscles and the humerus, forms spaces through which nerves and vessels pass between regions.
The supraspinatus, infraspinatus, and teres minor muscles are three of the four components of the rotator cuff, which stabilizes the glenohumeral joint. The other component is subscapularis that is on the anterior aspect of the scapula.
Gateways to the posterior scapular region
Suprascapular foramen
The suprascapular foramen is the route through which structures pass between the base of the neck and the posterior scapular region. It is formed by the suprascapular notch of the scapula and the superior transverse scapular (suprascapular) ligament, which converts the notch into a foramen (Fig. 7.26).
Fig. 7.26 Arteries and nerves associated with gateways in the posterior scapular region.
The suprascapular nerve passes through the suprascapular foramen; the suprascapular artery and the suprascapular vein follow the same course as the nerve, but normally pass immediately superior to the superior transverse scapular ligament and not through the foramen (Fig. 7.26).
Quadrangular space (from posterior)
The quadrangular space provides a passageway for nerves and vessels passing between more anterior regions (the axilla) and the posterior scapular region (Figs. 7.25, 7.26). In the posterior scapular region, its boundaries are formed by:
 the inferior margin of the teres minor,
the inferior margin of the teres minor,
 the surgical neck of the humerus,
the surgical neck of the humerus,
 the superior margin of the teres major, and
the superior margin of the teres major, and
 the lateral margin of the long head of triceps brachii.
the lateral margin of the long head of triceps brachii.
The axillary nerve and the posterior circumflex humeral artery and vein pass through this space (Fig. 7.26).
Clinical app
Quadrangular space syndrome
Hypertrophy of the muscles around the quadrangular space or fibrosis of the muscle edges may impinge on the axillary nerve. This may produce weakness of the deltoid muscle. It may also produce atrophy of the teres minor muscle, which may affect the control that the rotator cuff muscles exert on shoulder movement.
Triangular space
The triangular space is an area of communication between the axilla and the posterior scapular region (see Fig. 7.25). When viewed from the posterior scapular region, the triangular space is formed by:
 the medial margin of the long head of triceps brachii,
the medial margin of the long head of triceps brachii,
 the superior margin of the teres major, and
the superior margin of the teres major, and
 the inferior margin of the teres minor.
the inferior margin of the teres minor.
The circumflex scapular artery and vein pass through this gap (see Fig. 7.26).
Triangular interval
The triangular interval is formed by (see Fig. 7.25):
 the lateral margin of the long head of triceps brachii,
the lateral margin of the long head of triceps brachii,
 the inferior margin of the teres major.
the inferior margin of the teres major.
Because this space is below the inferior margin of the teres major, which defines the inferior boundary of the axilla, the triangular interval serves as a passageway between the anterior and posterior compartments of the arm and between the posterior compartment of the arm and the axilla. The radial nerve, the profunda brachii artery (deep artery of arm), and associated veins pass through it (see Fig. 7.26).
Nerves
The two major nerves of the posterior scapular region are the suprascapular and axillary nerves (see Fig. 7.25), both of which originate from the brachial plexus in the axilla.
Suprascapular nerve
The suprascapular nerve originates in the base of the neck from the superior trunk of the brachial plexus. It passes posterolaterally from its origin, through the suprascapular foramen to reach the posterior scapular region, where it lies in the plane between bone and muscle (see Fig. 7.26).
It innervates the supraspinatus muscle, then passes through the greater scapular (spinoglenoid) notch, between the root of the spine of the scapula and the glenoid cavity, to terminate in and innervate the infraspinatus muscle.
Generally, the suprascapular nerve has no cutaneous branches.
Axillary nerve
The axillary nerve originates from the posterior cord of the brachial plexus. It exits the axilla by passing through the quadrangular space in the posterior wall of the axilla, and enters the posterior scapular region (see Fig. 7.26). Together with the posterior circumflex humeral artery and vein, it is directly related to the posterior surface of the surgical neck of the humerus.
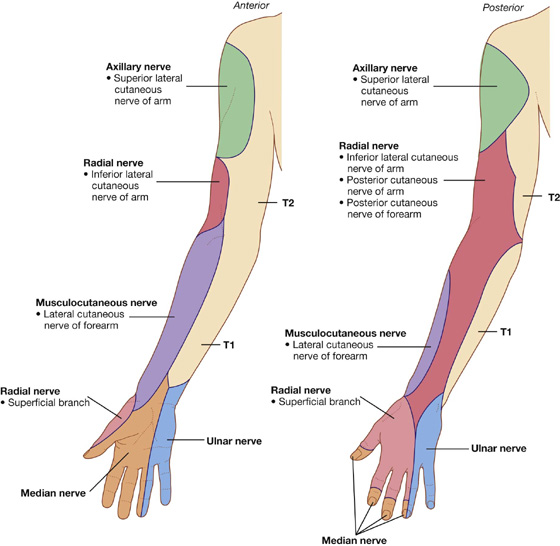
The axillary nerve innervates the deltoid and teres minor muscles. In addition, it has a cutaneous branch, the superior lateral cutaneous nerve of the arm, which carries general sensation from the skin over the inferior part of the deltoid muscle.
Arteries and veins
Three major arteries are found in the posterior scapular region: the suprascapular, posterior circumflex humeral, and circumflex scapular arteries. These arteries contribute to an interconnected vascular network around the scapula (Fig. 7.27).
Fig. 7.27 Arterial anastomoses around the shoulder.
Suprascapular artery
The suprascapular artery originates in the base of the neck as a branch of the thyrocervical trunk, which in turn, is a major branch of the subclavian artery (Fig. 7.27). The vessel may also originate directly from the third part of the subclavian artery.
The suprascapular artery normally enters the posterior scapular region superior to the suprascapular foramen, whereas the nerve passes through the foramen. In the posterior scapular region, the vessel runs with the suprascapular nerve (see Fig. 7.26).
In addition to supplying the supraspinatus and infraspinatus muscles, the suprascapular artery contributes branches to numerous structures along its course.
Posterior circumflex humeral artery
The posterior circumflex humeral artery originates from the third part of the axillary artery in the axilla (Figs. 7.26, 7.27).
The posterior circumflex humeral artery and axillary nerve leave the axilla through the quadrangular space in the posterior wall and enter the posterior scapular region. The vessel supplies the related muscles and the glenohumeral joint.
Circumflex scapular artery
The circumflex scapular artery is a branch of the subscapular artery that also originates from the third part of the axillary artery in the axilla (Fig. 7.27; also see Fig. 7.26). The circumflex scapular artery leaves the axilla through the triangular space and enters the posterior scapular region, passes through the origin of the teres minor muscle, and forms anastomotic connections with other arteries in the region.
Veins
Veins in the posterior scapular region generally follow the arteries and connect with vessels in the neck, back, arm, and axilla.
AXILLA
The axilla is the gateway to the upper limb, providing an area of transition between the neck and the arm (Fig. 7.28A). Formed by the clavicle, the scapula, the upper thoracic wall, the humerus, and related muscles, the axilla is an irregularly shaped pyramidal space with (Fig. 7.28A,B):
Fig. 7.28 Axilla. A. Walls and transition between neck and arm. B. Boundaries. C. Continuity with the arm.
The axillary inlet is continuous superiorly with the neck, and the lateral part of the floor opens into the arm.
All major structures passing into and out of the upper limb pass through the axilla (Fig. 7.28C). Apertures formed between muscles in the anterior and posterior walls enable structures to pass between the axilla and immediately adjacent regions (the posterior scapular, pectoral, and deltoid regions).
Axillary inlet
The axillary inlet is oriented in the horizontal plane and is somewhat triangular in shape, with its apex directed laterally (Fig. 7.28). The margins of the inlet are completely formed by bone:
 The medial margin is the lateral border of rib I.
The medial margin is the lateral border of rib I.
 The anterior margin is the posterior surface of the clavicle.
The anterior margin is the posterior surface of the clavicle.
 The posterior margin is the superior border of the scapula up to the coracoid process.
The posterior margin is the superior border of the scapula up to the coracoid process.
Major vessels and nerves pass between the neck and the axilla by crossing over the lateral border of rib I and through the axillary inlet (Fig. 7.28,A).
The subclavian artery, the major blood vessel supplying the upper limb, becomes the axillary artery as it crosses the lateral margin of rib I and enters the axilla. Similarly, the axillary vein becomes the subclavian vein as it passes over the lateral margin of rib I and leaves the axilla to enter the neck.
At the axillary inlet, the axillary vein is anterior to the axillary artery, which, in turn, is anterior to the trunks of the brachial plexus (Fig. 7.28,A)
The inferior trunk (lower trunk) of the brachial plexus lies directly on rib I in the neck, as does the subclavian artery and vein. As they pass over rib I, the vein and artery are separated by the insertion of the anterior scalene muscle (Fig. 7.28,A).
Anterior wall
The anterior wall of the axilla is formed by the lateral part of the pectoralis major muscle, the underlying pectoralis minor and subclavius muscles, and the clavipectoral fascia (Table 7.3, Figs. 7.28B, 7.29).
Table 7.3 Muscles of the anterior wall of the axilla (spinal segments indicated in bold are the major segments innervating the muscle)
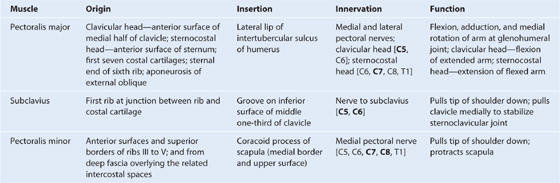
Fig. 7.29 Pectoralis major muscle.
Clavipectoral fascia
The clavipectoral fascia is a thick sheet of connective tissue that connects the clavicle to the floor of the axilla (Fig. 7.30). It encloses the subclavius and pectoralis minor muscles and spans the gap between them.
Fig. 7.30 Pectoralis minor and subclavius muscles and clavipectoral fascia.
Structures travel between the axilla and the anterior wall of the axilla by passing through the clavipectoral fascia either between the pectoralis minor and subclavius muscles or inferior to the pectoralis minor muscle.
Important structures that pass between the subclavius and pectoralis minor muscles include the cephalic vein, the thoraco-acromial artery, and the lateral pectoral nerve.
The lateral thoracic artery leaves the axilla by passing through the fascia inferior to the pectoralis minor muscle.
The medial pectoral nerve leaves the axilla by penetrating directly through the pectoralis minor muscle to supply this muscle and to reach the pectoralis major muscle. Occasionally, branches of the medial pectoral nerve pass around the lower margin of the pectoralis minor to reach and innervate the overlying pectoralis major muscle.
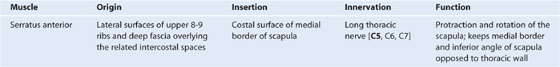
Medial wall
The medial wall of the axilla consists of the upper thoracic wall (the ribs and related intercostal tissues) and the serratus anterior muscle (Table 7.4, Fig. 7.31; see Fig. 7.28B).
Table 7.4 Muscles of the medial wall of the axilla (spinal segments indicated in bold are the major segments innervating the muscle)
The only major structure that passes directly through the medial wall and into the axilla is the intercostobrachial nerve (Fig. 7.31C). This nerve is the lateral cutaneous branch of the second intercostal nerve (anterior ramus of T2). It communicates with a branch of the brachial plexus (the medial cutaneous nerve of the arm) in the axilla and supplies skin on the upper posteromedial side of the arm, which is part of the T2 dermatome.
Clinical app
“Winging” of the scapula
Because the long thoracic nerve passes down the lateral thoracic wall on the external surface of the serratus anterior muscle, just deep to skin and subcutaneous fascia, it is vulnerable to damage (see Fig. 7.31C). Loss of function of this muscle causes the medial border, and particularly the inferior angle, of the scapula to elevate away from the thoracic wall, resulting in characteristic “winging” of the scapula, on pushing forward with the arm. Furthermore, normal elevation of the arm is no longer possible.
Lateral wall
The lateral wall of the axilla is narrow and formed entirely by the intertubercular sulcus of the humerus (Fig. 7.32). The pectoralis major muscle of the anterior wall attaches to the lateral lip of the intertubercular sulcus. The latissimus dorsi and teres major muscles of the posterior wall attach to the floor and medial lip of the intertubercular sulcus, respectively (Table 7.5, Fig. 7.32).
Fig. 7.32 Lateral wall of the axilla.
Table 7.5 Muscles of the lateral and posterior wall of the axilla (spinal segments indicated in bold are the major segments innervating the muscle; spinal segments enclosed in parentheses do not consistently innervate the muscle)
Posterior wall
The posterior wall of the axilla is complex (Table 7.5, Figs. 7.28B, 7.33). Its bone framework is formed by the costal surface of the scapula. Muscles of the wall are:
 the subscapularis muscle (associated with the costal surface of the scapula),
the subscapularis muscle (associated with the costal surface of the scapula),
 the proximal part of the long head of the triceps brachii muscle (which passes vertically down the wall and into the arm).
the proximal part of the long head of the triceps brachii muscle (which passes vertically down the wall and into the arm).
Fig. 7.33 Posterior wall of the axilla.
Gaps between the muscles of the posterior wall form apertures through which structures pass between the axilla, posterior scapular region, and posterior compartment of the arm (Fig. 7.33).
Together with three muscles of the posterior scapular region (the supraspinatus, infraspinatus, and teres minor muscles), the subscapularis is a member of the rotator cuff muscles, which stabilize the glenohumeral joint.
The long head of the triceps brachii muscle passes vertically through the posterior wall of the axilla, and, together with surrounding muscles and adjacent bones, results in the formation of three apertures through which major structures pass through the posterior wall (Fig. 7.33):
Gateways in the posterior wall
(See also “Gateways to the posterior scapular region,” p. 351, and Fig. 7.25.)
Quadrangular space
The quadrangular space provides a passageway for nerves and vessels passing between the axilla and the more posterior scapular and deltoid regions (Fig. 7.33). When viewed from anteriorly, its boundaries are formed by:
 the inferior margin of the subscapularis muscle;
the inferior margin of the subscapularis muscle;
 the surgical neck of the humerus;
the surgical neck of the humerus;
 the superior margin of the teres major muscle; and
the superior margin of the teres major muscle; and
 the lateral margin of the long head of the triceps brachii muscle.
the lateral margin of the long head of the triceps brachii muscle.
Passing through the quadrangular space are the axillary nerve and the posterior circumflex humeral artery and vein (see Fig. 7.26).
Triangular space
The triangular space is an area of communication between the axilla and the posterior scapular region (Fig. 7.33). When viewed from anteriorly, it is formed by:
 the medial margin of the long head of the triceps brachii muscle,
the medial margin of the long head of the triceps brachii muscle,
 the superior margin of the teres major muscle; and
the superior margin of the teres major muscle; and
 the inferior margin of the subscapularis muscle.
the inferior margin of the subscapularis muscle.
The circumflex scapular artery and vein pass into this space (see Fig. 7.26).
Triangular interval
This triangular interval is formed by (Fig. 7.33):
 the lateral margin of the long head of the triceps brachii muscle,
the lateral margin of the long head of the triceps brachii muscle,
 the inferior margin of the teres major muscle.
the inferior margin of the teres major muscle.
The radial nerve passes out of the axilla traveling through this interval to reach the posterior compartment of the arm (see Fig. 7.26).
Floor
The floor of the axilla (Fig. 7.34; also see Fig 7.28B) is formed by fascia and a dome of skin that spans the distance between the inferior margins of the walls. It is supported by the clavipectoral fascia.
Fig. 7.34 Floor of the axilla.
Inferiorly, structures pass into and out of the axilla immediately lateral to the floor where the anterior and posterior walls of the axilla converge and where the axilla is continuous with the anterior compartment of the arm.
Contents of the axilla
Passing through the axilla are the major vessels, nerves, and lymphatics of the upper limb. The space also contains the proximal parts of two muscles (biceps brachii and coracobrachialis muscles; Table 7.6) of the arm, the axillary process of the breast, and collections of lymph nodes, which drain the upper limb and chest wall.
Table 7.6 Muscles having parts that pass through the axilla (spinal segments indicated in bold are the major segments innervating the muscle)
Axillary artery
The axillary artery supplies the walls of the axilla and related regions, and continues as the major blood supply to the more distal parts of the upper limb (Fig. 7.35).
Fig. 7.35 Contents of the axilla: the axillary artery.
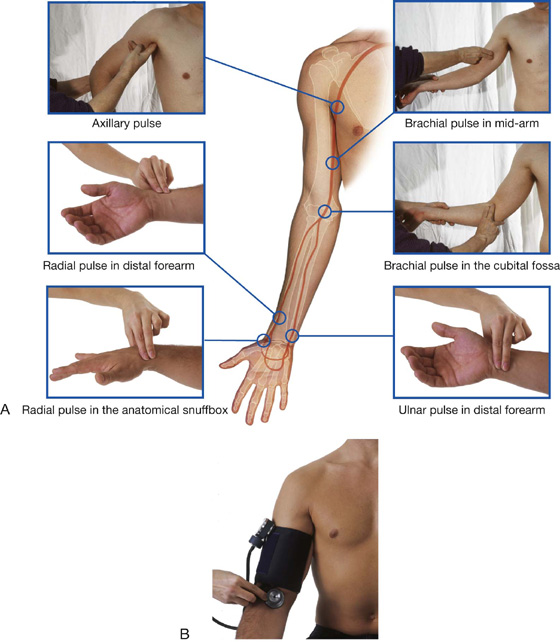
The subclavian artery in the neck becomes the axillary artery at the lateral margin of rib I and passes through the axilla, becoming the brachial artery at the inferior margin of the teres major muscle.
The axillary artery is separated into three parts by the pectoralis minor muscle, which crosses anteriorly to the vessel (Fig. 7.35):
 The first part is proximal to pectoralis minor.
The first part is proximal to pectoralis minor.
 The second part is posterior to pectoralis minor.
The second part is posterior to pectoralis minor.
 The third part is distal to pectoralis minor.
The third part is distal to pectoralis minor.
Generally, six branches arise from the axillary artery (Fig. 7.36):
 One branch, the superior thoracic artery, originates from the first part.
One branch, the superior thoracic artery, originates from the first part.
Fig. 7.36 Branches of the axillary artery.
Superior thoracic artery
The superior thoracic artery is small and originates from the anterior surface of the first part of the axillary artery (Fig. 7.36). It supplies upper regions of the medial and anterior axillary walls.
Thoracoacromial artery
The thoracoacromial artery is short and originates from the anterior surface of the second part of the axillary artery just posterior to the medial (superior) margin of the pectoralis minor muscle (Fig. 7.36). It curves around the superior margin of the muscle, penetrates the clavipectoral fascia, and immediately divides into four branches—the pectoral, deltoid, clavicular, and acromial branches, which supply the anterior axillary wall and related regions.
Additionally, the pectoral branch contributes vascular supply to the breast, and the deltoid branch passes into the clavipectoral triangle where it accompanies the cephalic vein and supplies adjacent structures (see Fig. 7.30).
Lateral thoracic artery
The lateral thoracic artery arises from the anterior surface of the second part of the axillary artery posterior to the lateral (inferior) margin of pectoralis minor (Fig. 7.36). It follows the margin of the muscle to the thoracic wall and supplies the medial and anterior walls of the axilla. In women, branches emerge from around the inferior margin of the pectoralis major muscle and contribute to the vascular supply of the breast.
Subscapular artery
The subscapular artery is the largest branch of the axillary artery and is the major blood supply to the posterior wall of the axilla (Fig. 7.36). It also contributes to the blood supply of the posterior scapular region.
The subscapular artery originates from the posterior surface of the third part of the axillary artery, follows the inferior margin of the subscapularis muscle for a short distance, then divides into its two terminal branches, the circumflex scapular artery and the thoracodorsal artery (Fig. 7.36).
The circumflex scapular artery passes through the triangular space between the subscapularis, teres major, and long head of the triceps muscles. Posteriorly, it passes inferior to, or pierces, the origin of the teres minor muscle to enter the infraspinous fossa. It anastomoses with the suprascapular artery and the deep branch (dorsal scapular artery) of the transverse cervical artery, thereby contributing to an anastomotic network of vessels around the scapula.
The thoracodorsal artery approximately follows the lateral border of the scapula to the inferior angle. It contributes to the vascular supply of the posterior and medial walls of the axilla.
Anterior circumflex humeral artery
The anterior circumflex humeral artery is small compared to the posterior circumflex humeral artery, and originates from the lateral side of the third part of the axillary artery (Fig. 7.36). It passes anterior to the surgical neck of the humerus and anastomoses with the posterior circumflex humeral artery.
This anterior circumflex humeral artery supplies branches to surrounding tissues, which include the glenohumeral joint and the head of the humerus.
Posterior circumflex humeral artery
The posterior circumflex humeral artery originates from the lateral surface of the third part of the axillary artery immediately posterior to the origin of the anterior circumflex humeral artery (Fig. 7.36). With the axillary nerve, it leaves the axilla by passing through the quadrangular space between the teres major, teres minor, and the long head of the triceps brachii muscle and the surgical neck of the humerus (see Fig. 7.26).
The posterior circumflex humeral artery curves around the surgical neck of the humerus and supplies the surrounding muscles and the glenohumeral joint. It anastomoses with the anterior circumflex humeral artery, and with branches from the profunda brachii, suprascapular, and thoracoacromial arteries.
Axillary vein
The axillary vein begins at the lower margin of the teres major muscle and is the continuation of the basilic vein (Fig. 7.37), which is a superficial vein that drains the posteromedial surface of the hand and forearm and penetrates the deep fascia in the middle of the arm.
Fig. 7.37 Axillary vein.
The axillary vein passes through the axilla medial and anterior to the axillary artery and becomes the subclavian vein as the vessel crosses the lateral border of rib I at the axillary inlet. Tributaries of the axillary vein generally follow the branches of the axillary artery. Other tributaries include brachial veins that follow the brachial artery, and the cephalic vein (Fig. 7.37).
The cephalic vein is a superficial vein that drains the lateral and posterior parts of the hand, the forearm, and the arm. In the area of the shoulder, it passes into an inverted triangular cleft (the clavipectoral triangle) between the deltoid muscle, pectoralis major muscle, and the clavicle. In the superior part of the clavipectoral triangle, the cephalic vein passes deep to the clavicular head of the pectoralis major muscle and pierces the clavipectoral fascia to join the axillary vein.
Clinical app
Trauma to the arteries in and around the axilla
As the subclavian artery passes out of the neck and into the axilla, it is fixed in position by the surrounding muscles to the superior surface of rib I. A rapid deceleration injury involving upper thoracic trauma may cause a first rib fracture, which may significantly compromise the distal part of the subclavian artery or the first part of the axillary artery. Fortunately, there are anastomotic connections between branches of the subclavian artery and the axillary artery, which form a network around the scapula and proximal end of the humerus; therefore, even with complete vessel transection, the arm is rarely rendered completely ischemic (ischemia is poor blood supply to an organ or a limb).
Anterior dislocation of the humeral head
Anterior dislocation of the humeral head may compress the axillary artery resulting in vessel occlusion. This is unlikely to render the upper limb completely ischemic, but it may be necessary to surgically reconstruct the axillary artery to obtain pain-free function. Importantly, the axillary artery is intimately related to the brachial plexus, which also may be damaged at the time of anterior dislocation.
Clinical app
Central venous access via the subclavian/axillary vein
There are a number of routes through which central venous access may be obtained. The “subclavian route” and the “jugular route” are commonly used by clinicians. The subclavian route is a misnomer that remains the preferred term in clinical practice. In fact, most clinicians enter the first part of the axillary vein.
Brachial plexus
The brachial plexus is a somatic plexus formed by the anterior rami of C5 to C8, and most of the anterior ramus of T1 (Fig. 7.38). It originates in the neck, passes laterally and inferiorly over rib I, and enters the axilla.
The parts of the brachial plexus, from medial to lateral, are roots, trunks, divisions, and cords. All major nerves that innervate the upper limb originate from the brachial plexus, mostly from the cords. Proximal parts of the brachial plexus are posterior to the subclavian artery in the neck, while more distal regions of the plexus surround the axillary artery.
Roots
The roots of the brachial plexus are the anterior rami of C5 to C8, and most of T1. Close to their origin, the roots receive gray rami communicantes from the sympathetic trunk (Fig. 7.38). These carry postganglionic sympathetic fibers onto the roots for distribution to the periphery. The roots and trunks enter the posterior triangle of the neck by passing between the anterior scalene and middle scalene muscles and lie superior and posterior to the subclavian artery.
Trunks
The three trunks of the brachial plexus originate from the roots, pass laterally over rib I, and enter the axilla (Fig. 7.38):
 The superior trunk is formed by the union of C5 and C6 roots.
The superior trunk is formed by the union of C5 and C6 roots.
 The middle trunk is a continuation of the C7 root.
The middle trunk is a continuation of the C7 root.
 The inferior trunk is formed by the union of the C8 and T1 roots.
The inferior trunk is formed by the union of the C8 and T1 roots.
The inferior trunk lies on rib I posterior to the subclavian artery; the middle and superior trunks are more superior in position.
Divisions
Each of the three trunks of the brachial plexus divides into an anterior and a posterior division (Fig. 7.38):
Cords
The three cords of the brachial plexus originate from the divisions and are related to the second part of the axillary artery (Fig. 7.38):
Most of the major peripheral nerves of the upper limb originate from the cords of the brachial plexus. Generally, nerves associated with the anterior compartments of the upper limb arise from the medial and lateral cords and nerves associated with the posterior compartments originate from the posterior cord.
Branches (Table 7.7)
In addition to small segmental branches from C5 to C8 to muscles of the neck and a contribution of C5 to the phrenic nerve, the roots of the brachial plexus give rise to the dorsal scapular and long thoracic nerves (Figs. 7.39, 7.40).
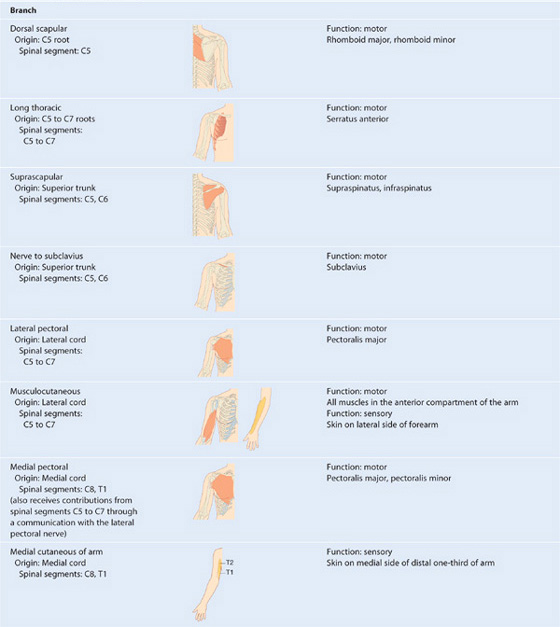
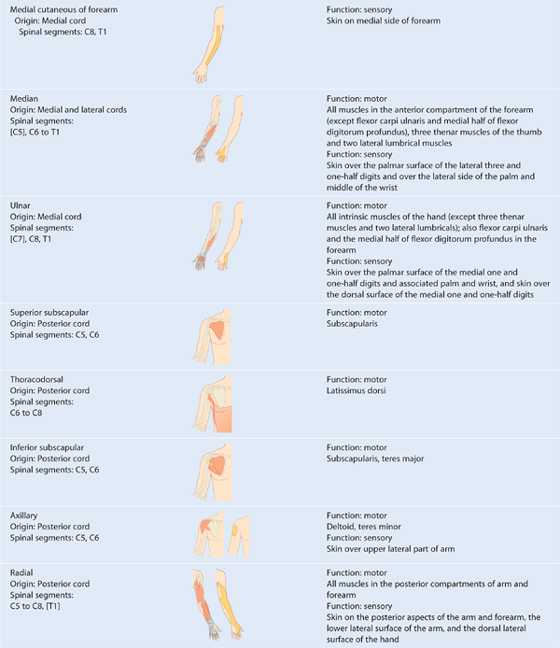
Fig. 7.40 Branches of the roots and trunks of the brachial plexus.
The dorsal scapular nerve:
 originates from the C5 root of the brachial plexus,
originates from the C5 root of the brachial plexus,
 innervates the rhomboid major and minor muscles from their deep surfaces.
innervates the rhomboid major and minor muscles from their deep surfaces.
The long thoracic nerve:
 originates from the anterior rami of C5 to C7,
originates from the anterior rami of C5 to C7,
 lies on the superficial aspect of the serratus anterior muscle.
lies on the superficial aspect of the serratus anterior muscle.
Clinical app
Damage to long thoracic nerve
A mastectomy (surgical removal of the breast) involves excision of the breast tissue to the pectoralis major muscle and fascia. Within the axilla, the breast tissue must be removed from the medial axillary wall. Closely applied to the medial axillary wall is the long thoracic nerve. Damage to this nerve can result in paralysis of the serratus anterior muscle producing a characteristic “winged” scapula. This nerve also can be injured during placement of chest tubes or by trauma to the lateral body wall.
The only branches from the trunks of the brachial plexus are two nerves that originate from the superior trunk (upper trunk): the suprascapular nerve and the nerve to the subclavius muscle (Figs. 7.39, 7.40).
The suprascapular nerve (C5 and C6):
 originates from the superior trunk of the brachial plexus.
originates from the superior trunk of the brachial plexus.
 innervates the supraspinatus and infraspinatus muscles, and
innervates the supraspinatus and infraspinatus muscles, and
The nerve to subclavius muscle (C5 and C6) is a small nerve that:
 originates from the superior trunk of the brachial plexus,
originates from the superior trunk of the brachial plexus,
 passes anteroinferiorly over the subclavian artery and vein, and
passes anteroinferiorly over the subclavian artery and vein, and
 innervates the subclavius muscle.
innervates the subclavius muscle.
Three nerves originate entirely or partly from the lateral cord (Figs. 7.39, 7.41).
Fig. 7.41 Branches of the lateral and medial cords of the brachial plexus.
The musculocutaneous nerve is a large terminal branch of the lateral cord. It passes laterally to penetrate the coracobrachialis muscle and passes between the biceps brachii and brachialis muscles in the arm, and innervates all three flexor muscles in the anterior compartment of the arm, terminating as the lateral cutaneous nerve of forearm.
The lateral root of median nerve is the largest terminal branch of the lateral cord and passes medially to join a similar branch from the medial cord to form the median nerve.
The medial cord has five branches (Figs. 7.39, 7.41).
The medial pectoral nerve is the most proximal branch. It receives a communicating branch from the lateral pectoral nerve and then passes anteriorly between the axillary artery and axillary vein. Branches of the nerve penetrate and supply the pectoralis minor muscle. Some of these branches pass through the muscle to reach and supply the pectoralis major muscle. Other branches occasionally pass around the inferior or lateral margin of the pectoralis minor muscle to reach the pectoralis major muscle.
The medial cutaneous nerve of arm (medial brachial cutaneous nerve) passes through the axilla and into the arm where it penetrates deep fascia and supplies skin over the medial side of the distal third of the arm. In the axilla, the nerve communicates with the intercostobrachial nerve of T2. Fibers of the medial cutaneous nerve of arm innervate the upper part of the medial surface of the arm and floor of the axilla.
The medial cutaneous nerve of forearm (medial antebrachial cutaneous nerve) originates just distal to the origin of the medial cutaneous nerve of arm. It passes out of the axilla and into the arm where it gives off a branch to the skin over the biceps brachii muscle, and then continues down the arm to penetrate the deep fascia with the basilic vein, continuing inferiorly to supply the skin over the anterior surface of the forearm. It innervates skin over the medial surface of the forearm down to the wrist.
The ulnar nerve is a large terminal branch of the medial cord. However, near its origin, it often receives a communicating branch from the lateral root of the median nerve originating from the lateral cord and carrying fibers from C7 (see Fig. 7.39B). The ulnar nerve passes through the arm and forearm into the hand, where it innervates all intrinsic muscles of the hand (except for the three thenar muscles and the two lateral lumbrical muscles). On passing through the forearm, branches of the ulnar nerve innervate the flexor carpi ulnaris muscle and the medial half of the flexor digitorum profundus muscle. The ulnar nerve innervates skin over the palmar surface of the little finger, medial half of the ring finger, and associated palm and wrist, and the skin over the dorsal surface of the medial part of the hand.
Median nerve. The median nerve is formed anterior to the third part of the axillary artery by the union of lateral and medial roots originating from the lateral and medial cords of the brachial plexus (Figs. 7.39, 7.41). It passes into the arm anterior to the brachial artery, through the arm into the forearm where branches innervate most of the muscles in the anterior compartment of the forearm (except for the flexor carpi ulnaris muscle and the medial half of the flexor digitorum profundus muscle, which are innervated by the ulnar nerve).
The median nerve continues into the hand to innervate:
 the three thenar muscles associated with the thumb,
the three thenar muscles associated with the thumb,
 the two lateral lumbrical muscles associated with movement of the index and middle fingers, and
the two lateral lumbrical muscles associated with movement of the index and middle fingers, and
The musculocutaneous nerve, the lateral root of the median nerve, the median nerve, the medial root of the median nerve, and the ulnar nerve form an M over the third part of the axillary artery (Fig. 7.41). This feature, together with penetration of the coracobrachialis muscle by the musculocutaneous nerve, can be used to identify components of the brachial plexus in the axilla.
Branches of the posterior cord
Five nerves originate from the posterior cord of the brachial plexus (Figs. 7.39, 7.42):
 the superior subscapular nerve,
the superior subscapular nerve,
 the inferior subscapular nerve,
the inferior subscapular nerve,
Fig. 7.42 Branches of the posterior cord of the brachial plexus.
The superior subscapular nerve, the thoracodorsal, and the inferior subscapular nerves originate sequentially from the posterior cord and pass directly into muscles associated with the posterior axillary wall (Fig. 7.42). The superior subscapular nerve is short and passes into and supplies the subscapularis muscle. The thoracodorsal nerve is the longest of these three nerves and passes vertically along the posterior axillary wall. It penetrates and innervates the latissimus dorsi muscle. The inferior subscapular nerve also passes inferiorly along the posterior axillary wall and innervates the subscapularis and teres major muscles.
The axillary nerve originates from the posterior cord and passes inferiorly and laterally along the posterior wall to exit the axilla through the quadrangular space (Fig. 7.42). It passes posteriorly around the surgical neck of the humerus and innervates both the deltoid and teres minor muscles. A superior lateral cutaneous nerve of arm originates from the axillary nerve after passing through the quadrangular space and loops around the posterior margin of the deltoid muscle to innervate skin in that region. The axillary nerve is accompanied by the posterior circumflex humeral artery.
The radial nerve is the largest terminal branch of the posterior cord (Fig. 7.42). It passes out of the axilla and into the posterior compartment of the arm by passing through the triangular interval between the inferior border of the teres major muscle, the long head of the triceps brachii muscle, and the shaft of the humerus. It is accompanied through the triangular interval by the profunda brachii artery, which originates from the brachial artery in the anterior compartment of the arm. The radial nerve and its branches innervate:
 all muscles in the posterior compartments of the arm and forearm, and
all muscles in the posterior compartments of the arm and forearm, and
The posterior cutaneous nerve of arm (posterior brachial cutaneous nerve) originates from the radial nerve in the axilla and innervates skin on the posterior surface of the arm.
Lymphatics
All lymphatics from the upper limb drain into lymph nodes in the axilla (Fig. 7.43).
Fig. 7.43 Lymph nodes and vessels in the axilla.
In addition, axillary nodes receive drainage from an extensive area on the adjacent trunk, which includes regions of the upper back and shoulder, the lower neck, the chest, and the upper anterolateral abdominal wall. Axillary nodes also receive drainage from approximately 75% of the mammary gland.
The 20 to 30 axillary nodes are generally divided into five groups on the basis of location (Fig. 7.43).
Pectoral (anterior) nodes occur along the inferior margin of the pectoralis minor muscle and along the course of the lateral thoracic vessels. They receive drainage from the abdominal wall, the chest, and the mammary gland.
Subscapular (posterior) nodes on the posterior axillary wall in association with the subscapular vessels drain the posterior axillary wall and receive lymphatics from the back, the shoulder, and the neck.
Central nodes are embedded in axillary fat and receive tributaries from humeral, subscapular, and pectoral groups of nodes.
Apical nodes are the most superior group of nodes in the axilla and drain all other groups of nodes in the region. In addition, they receive lymphatic vessels that accompany the cephalic vein as well as vessels that drain the superior region of the mammary gland.
Efferent vessels from the apical group converge to form the subclavian trunk, which usually joins the venous system at the junction between the right subclavian vein and the right internal jugular vein in the neck. On the left, the subclavian trunk usually joins the thoracic duct in the base of the neck.
Axillary process of the mammary gland
Although the mammary gland is in superficial fascia overlying the thoracic wall, its superolateral region extends along the inferior margin of the pectoralis major muscle toward the axilla. In some cases, this may pass around the margin of the muscle to penetrate deep fascia and enter the axilla (Fig. 7.44). This axillary process rarely reaches as high as the apex of the axilla.
Fig. 7.44 Axillary process of the breast.
Clinical app
Injuries to the brachial plexus
Brachial plexus injuries are usually the result of blunt trauma producing nerve avulsions and disruption. These injuries are usually devastating for the function of the upper limb and require many months of dedicated rehabilitation for even a small amount of function to return.
Spinal cord injuries in the cervical region and direct pulling injuries tend to affect the roots of the brachial plexus. Severe trauma to the first rib usually affects the trunks. The divisions and cords of the brachial plexus can be injured by dislocation of the glenohumeral joint.
Clinical app
Lymphatic drainage and breast cancer
Lymphatic drainage from the lateral part of the breast passes through nodes in the axilla. Significant disruption to the normal lymphatic drainage of the upper limb may occur if a mastectomy or a surgical axillary nodal clearance has been carried out for breast cancer. Furthermore, some patients have radiotherapy to the axilla to prevent the spread of metastatic disease, but a side effect of this is the destruction of the tiny lymphatics as well as the cancer cells. If the lymphatic drainage of the upper limb is damaged, the arm may swell (lymphedema).
ARM
The arm is the region of the upper limb between the shoulder and the elbow (Fig. 7.45A). The superior aspect of the arm communicates medially with the axilla. Inferiorly, a number of important structures pass between the arm and the forearm through the cubital fossa, which is positioned anterior to the elbow joint.
Fig. 7.45 Arm. A. Proximal and distal relationships. B. Transverse section through the middle of the arm.
The arm is divided into two compartments by medial and lateral intermuscular septa, which pass from each side of the humerus to the outer sleeve of deep fascia that surrounds the limb (Fig. 7.45B).
The anterior compartment of the arm contains muscles that predominantly flex the elbow joint; the posterior compartment contains muscles that extend the joint. Major nerves and vessels supply and pass through each compartment.
Bones
The skeletal support for the arm is the humerus (Fig. 7.46). However, most of the large muscles of the arm insert into the proximal ends of the two bones of the forearm, the radius and the ulna, and flex and extend the forearm at the elbow joint. In addition, the muscles predominantly situated in the forearm that move the hand originate at the distal end of the humerus.
Fig. 7.46 Humerus. Posterior view.
Shaft and distal end of the humerus
In cross-section, the shaft of the humerus is somewhat triangular with (Fig. 7.46):
 anterior, lateral, and medial borders, and
anterior, lateral, and medial borders, and
 anterolateral, anteromedial, and posterior surfaces.
anterolateral, anteromedial, and posterior surfaces.
The posterior surface of the humerus is marked on its superior aspect by a linear roughening for the attachment of the lateral head of the triceps brachii muscle, beginning just inferior to the surgical neck and passing diagonally across the bone to the deltoid tuberosity (Fig. 7.46).
The middle part of the posterior surface and adjacent part of the anterolateral surface are marked by the shallow radial groove, which passes diagonally down the bone and parallel to the sloping posterior margin of the deltoid tuberosity (Fig. 7.46). The radial nerve and the profunda brachii artery lie in this groove.
Approximately in the middle of the shaft, the medial border is marked by thin elongated roughening for the attachment of the coracobrachialis muscle (Fig. 7.46).
Intermuscular septa, which separate the anterior compartment from the posterior compartment, attach to the medial and lateral borders (Fig. 7.47A).
Fig. 7.47 Distal end of the humerus. A. Anterior view. B. Posterior view.
Distally, the humerus becomes flattened, and these borders expand as the lateral supraepicondylar ridge (lateral supracondylar ridge) and the medial supraepicondylar ridge (medial supracondylar ridge) (Fig. 7.47A). The lateral supraepicondylar ridge is more pronounced than the medial and is roughened for the attachment of muscles found in the posterior compartment of the forearm.
The distal end of the humerus, which is flattened in the anteroposterior plane, bears a condyle, two epicondyles, and three fossae, as follows.
The condyle
The two articular parts of the condyle, the capitulum and the trochlea (Fig. 7.47A), articulate with the two bones of the forearm.
The capitulum articulates with the radius of the forearm. Lateral in position and hemispherical in shape, it projects anteriorly and somewhat inferiorly and is not visible when the humerus is viewed from the posterior aspect.
The trochlea articulates with the ulna of the forearm. It is pulley shaped and lies medial to the capitulum. Its medial edge is more pronounced than its lateral edge and, unlike the capitulum, it extends onto the posterior surface of the bone.
The two epicondyles
The two epicondyles lie adjacent, and somewhat superior, to the trochlea and capitulum (Fig. 7.47A).
The medial epicondyle, a large bony protuberance, is the major palpable landmark on the medial side of the elbow, and projects medially from the distal end of the humerus. On its surface, it bears a large oval impression for the attachment of muscles in the anterior compartment of the forearm (common flexor origin). The ulnar nerve passes from the arm into the forearm around the posterior surface of the medial epicondyle and can be palpated against the bone in this location.
The lateral epicondyle is much less pronounced than the medial epicondyle. It is lateral to the capitulum and has a large irregular impression for the attachment of muscles in the posterior compartment of the forearm (common extensor origin).
The three fossae
Three fossae occur superior to the trochlea and capitulum on the distal end of the humerus (Fig. 7.47).
The radial fossa is the least distinct of the fossae and occurs immediately superior to the capitulum on the anterior surface of the humerus.
The coronoid fossa is adjacent to the radial fossa and is superior to the trochlea.
The largest of the fossae, the olecranon fossa, occurs immediately superior to the trochlea on the posterior surface of the distal end of the humerus (Fig. 7.47B).
These three fossae accommodate projections from the bones in the forearm during movements of the elbow joint.
Proximal end of the radius
The proximal end of the radius consists of a head, a neck, and the radial tuberosity (Fig. 7.48).
Fig. 7.48 Anterior view of the proximal end of the radius.
The head of the radius is a thick disc-shaped structure oriented in the horizontal plane. The circular superior surface is concave for articulation with the capitulum of the humerus. The thick margin of the disc is broad medially where it articulates with the radial notch on the proximal end of the ulna.
The neck of the radius is a short and narrow cylinder of bone between the expanded head and the radial tuberosity on the shaft.
The radial tuberosity is a large blunt projection on the medial surface of the radius immediately inferior to the neck. Much of its surface is roughened for the attachment of the biceps brachii tendon. The oblique line of the radius continues diagonally across the shaft of the bone from the inferior margin of the radial tuberosity.
Proximal end of the ulna
The proximal end of the ulna is much larger than the proximal end of the radius and consists of the olecranon, the coronoid process, the trochlear notch, the radial notch, and the tuberosity of ulna (Fig. 7.49).
Fig. 7.49 Lateral, anterior, medial, and posterior views of the proximal end of the ulna.
The olecranon is a large projection of bone that extends proximally from the ulna. Its anterolateral surface is articular and contributes to the formation of the trochlear notch, which articulates with the trochlea of the humerus. The superior surface is marked by a large roughened impression for the attachment of the triceps brachii muscle. The posterior surface is smooth, shaped somewhat triangularly, and can be palpated as the “tip of the elbow.”
The coronoid process projects anteriorly from the proximal end of the ulna (Fig. 7.49). Its superolateral surface is articular and participates with the olecranon in forming the trochlear notch. The lateral surface is marked by the radial notch for articulation with the head of the radius.
Just inferior to the radial notch is a fossa that allows the radial tuberosity to change position during pronation and supination. The posterior margin of this fossa is broadened to form the supinator crest. The anterior surface of the coronoid process is triangular, with the apex directed distally, and has a number of roughenings for muscle attachment. The largest of these roughenings, the tuberosity of ulna, is at the apex of the anterior surface and is the attachment site for the brachialis muscle.
Muscles
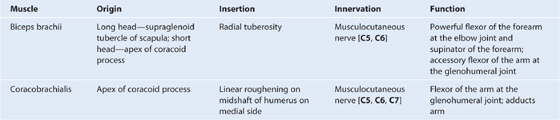
The anterior compartment of the arm contains three muscles—the coracobrachialis, brachialis, and biceps brachii muscles (Table 7.8, Fig. 7.50)—which are innervated predominantly by the musculocutaneous nerve.
Table 7.8 Muscles of the anterior compartment of the arm (spinal segments indicated in bold are the major segments innervating the muscle)
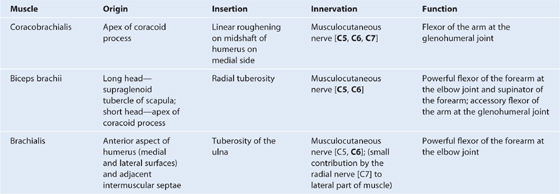
Fig. 7.50 Musculocutaneous, median, and ulnar nerves in the arm.
The posterior compartment contains one muscle—the triceps brachii muscle (Table 7.9, Fig. 7.51)—which is innervated by the radial nerve.
Table 7.9 Muscle of the posterior compartment of the arm (spinal segments indicated in bold are the major segments innervating the muscle)

Fig. 7.51 Radial nerve in the arm.
Clinical app
Rupture of biceps tendon
It is relatively unusual for muscles and their tendons to rupture in the upper limb; however, the tendon that most commonly ruptures is the tendon of the long head of the biceps brachii muscle. In isolation, this has relatively little effect on the upper limb, but it does produce a characteristic deformity—on flexing the elbow, there is an extremely prominent bulge of the muscle belly as its unrestrained fibers contract—the “Popeye” sign.
Nerves
Musculocutaneous nerve
The musculocutaneous nerve leaves the axilla and enters the arm by passing through the coracobrachialis muscle (Fig. 7.50). It passes diagonally down the arm in the plane between the biceps brachii and brachialis muscles. After giving rise to motor branches in the arm, it emerges laterally to the tendon of the biceps brachii muscle at the elbow, penetrates deep fascia, and continues as the lateral cutaneous nerve of forearm.
The musculocutaneous nerve provides:
 motor innervation to all muscles in the anterior compartment of the arm, and
motor innervation to all muscles in the anterior compartment of the arm, and
 sensory innervation to skin on the lateral surface of the forearm.
sensory innervation to skin on the lateral surface of the forearm.
Median nerve
The median nerve enters the arm from the axilla at the inferior margin of the teres major muscle (Fig. 7.50). It passes vertically down the medial side of the arm in the anterior compartment and is related to the brachial artery throughout its course:
 In proximal regions, the median nerve is immediately lateral to the brachial artery.
In proximal regions, the median nerve is immediately lateral to the brachial artery.
The median nerve has no major branches in the arm, but a branch to one of the muscles of the forearm, the pronator teres muscle, may originate from the nerve immediately proximal to the elbow joint.
Ulnar nerve
The ulnar nerve enters the arm with the median nerve and axillary artery (Fig. 7.50). It passes through proximal regions medial to the axillary artery. In the middle of the arm, the ulnar nerve penetrates the medial intermuscular septum and enters the posterior compartment where it lies anterior to the medial head of the triceps brachii muscle. It passes posterior to the medial epicondyle of the humerus and then into the anterior compartment of the forearm.
The ulnar nerve has no major branches in the arm.
Radial nerve
The radial nerve originates from the posterior cord of the brachial plexus and enters the arm by crossing the inferior margin of the teres major muscle (Fig. 7.51). As it enters the arm, it lies posterior to the brachial artery. Accompanied by the profunda brachii artery, the radial nerve enters the posterior compartment of the arm by passing through the triangular interval.
As the radial nerve passes diagonally, from medial to lateral, through the posterior compartment, it lies in the radial groove directly on bone. On the lateral side of the arm, it passes anteriorly through the lateral intermuscular septum and enters the anterior compartment where it lies between the brachialis muscle and a muscle of the posterior compartment of the forearm—the brachioradialis muscle, which attaches to the lateral supraepicondylar ridge of the humerus. The radial nerve enters the forearm anterior to the lateral epicondyle of the humerus, just deep to the brachioradialis muscle.
In the arm, the radial nerve has muscular and cutaneous branches (Fig. 7.51).
Muscular branches include those to the triceps brachii, brachioradialis, and extensor carpi radialis longus muscles. In addition, the radial nerve contributes to the innervation of the lateral part of the brachialis muscle. One of the branches to the medial head of the triceps brachii muscle arises before the radial nerve’s entrance into the posterior compartment and passes vertically down the arm in association with the ulnar nerve.
Cutaneous branches of the radial nerve that originate in the posterior compartment of the arm are the inferior lateral cutaneous nerve of arm and the posterior cutaneous nerve of forearm, both of which penetrate through the lateral head of the triceps brachii muscle and the overlying deep fascia to become subcutaneous.
Clinical App
Radial nerve injury in the arm
The radial nerve is tightly bound with the profunda brachii artery between the medial and lateral heads of the triceps brachii muscle in the radial groove. If the humerus is fractured (Fig. 7.52), the radial nerve may become stretched or transected in this region leading to permanent damage and loss of function. The nerve should always be tested when a fracture of the midshaft of the humerus is suspected. The patient’s symptoms usually include wrist drop (due to denervation of the extensor muscles) and sensory changes over the dorsum of the hand.
Fig. 7.52 Radiograph of the humerus demonstrating a midshaft fracture, which may disrupt the radial nerve.
Arteries and veins
Brachial artery
The major artery of the arm, the brachial artery, is found in the anterior compartment (Fig. 7.53A). Beginning as a continuation of the axillary artery at the lower border of the teres major muscle, it terminates just distal to the elbow joint where it divides into the radial and ulnar arteries.
Fig. 7.53 Brachial artery. A. Brachial artery. B. Branches.
In the proximal arm, the brachial artery lies on the medial side. In the distal arm, it moves laterally to assume a position midway between the lateral epicondyle and the medial epicondyle of the humerus (Fig. 7.53A). It crosses anteriorly to the elbow joint where it lies immediately medial to the tendon of the biceps brachii muscle. The brachial artery is palpable along its length. In proximal regions, the brachial artery can be compressed against the medial side of the humerus.
Branches of the brachial artery in the arm include those adjacent to muscles and two ulnar collateral vessels, which contribute to a network of arteries around the elbow joint (Fig. 7.53B). Additional branches are the profunda brachii artery and nutrient arteries to the humerus, which pass through a foramen in the anteromedial surface of the humeral shaft.
Surface anatomy
Locating the brachial artery in the arm
The brachial artery is on the medial side of the arm in the cleft between the biceps brachii and triceps brachii muscles (Fig. 7.54). The median nerve courses with the brachial artery, whereas the ulnar nerve deviates posteriorly from the vessel in distal regions.
Profunda brachii artery
The profunda brachii artery, the largest branch of the brachial artery, passes into and supplies the posterior compartment of the arm (Fig. 7.53B). It enters the posterior compartment with the radial nerve and together they pass through the triangular interval, which is formed by the shaft of the humerus, the inferior margin of the teres major muscle, and the lateral margin of the long head of the triceps muscle. They then pass along the radial groove on the posterior surface of the humerus deep to the lateral head of the triceps brachii muscle.
Branches of the profunda brachii artery supply adjacent muscles and anastomose with the posterior circumflex humeral artery. The artery terminates as two collateral vessels, which contribute to an anastomotic network of arteries around the elbow joint.
Veins
Paired brachial veins pass along the medial and lateral sides of the brachial artery, receiving tributaries that accompany branches of the artery (Fig. 7.55).
Fig. 7.55 Veins of the arm.
In addition to these deep veins, two large subcutaneous veins, the basilic vein and the cephalic vein, are located in the arm (Fig. 7.55).
The basilic vein passes vertically in the distal half of the arm, penetrates deep fascia to assume a position medial to the brachial artery, and then becomes the axillary vein at the lower border of the teres major muscle. The brachial veins join the basilic, or axillary, vein.
ELBOW JOINT
The elbow joint is a complex joint involving three separate articulations, which share a common synovial cavity (Fig. 7.56; also see Fig. 7.60).
Fig. 7.57 Synovial membrane of elbow joint (anterior view).
Fig. 7.58 Joint capsule and ligaments of the right elbow joint.
Imaging app
Developmental changes in the elbow joint
In an adult it is usually not difficult to interpret a radiograph, but in children developmental patterns have to be considered (Fig. 7.59).

As the elbow develops, numerous secondary ossification centers appear before and around puberty. It is easy to mistakenly interpret these as fractures. In addition, it is also possible for the epiphyses and apophyses to be “pulled off” or disrupted. Therefore, when interpreting a child’s radiograph of the elbow, the physician must know the child’s age. Fusion occurs at around the time of puberty. The approximate ages of appearance of the secondary ossification centers around the elbow joint are:
Imaging app
Visualizing the elbow joint
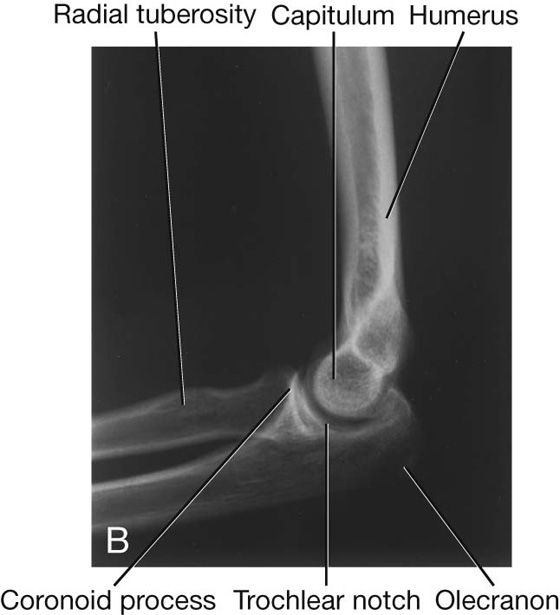
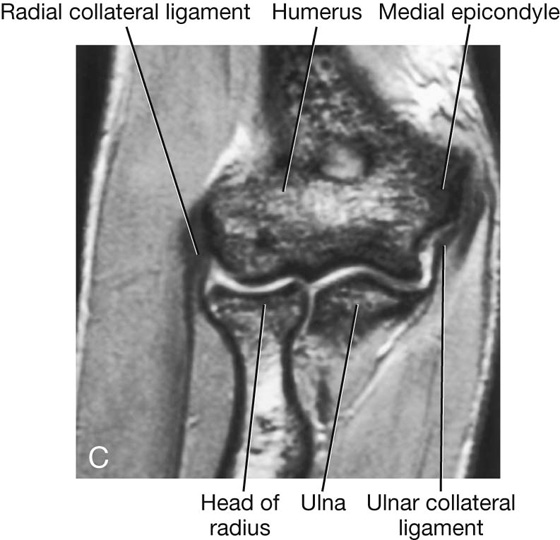
Clinical app
Pulled elbow
Pulled elbow is a disorder that typically occurs in children under 5 years of age. It is commonly caused by a sharp pull of the child’s hand, usually when the child is pulled up onto a curb. The not-yet-developed head of the radius and the laxity of the anular ligament of radius allow the head to sublux from this cuff of tissue.
Clinical app
Fracture of the head of radius
A fracture of the head of radius is a common injury and can cause appreciable morbidity. It is one of the typical injuries that occur with a fall on the outstretched hand. On falling, the force is transmitted to the radial head, which fractures. These fractures result in loss of full extension, and potential surgical reconstruction may require long periods of physiotherapy to obtain a full range of movement at the elbow joint.
Clinical app
“Tennis” and “golfer’s” elbow (epicondylitis)
It is not uncommon for people who are involved in sports such as golf and tennis to develop an overuse strain of the origins of the flexor and extensor muscles of the forearm. The pain is typically around the epicondyles and usually resolves after rest. If pain and inflammation persist, surgical division of the extensor or flexor origin from the bone may be necessary. Typically, in tennis players this pain occurs on the lateral epicondyle and common extensor origin (tennis elbow), whereas in golfers it occurs on the medial epicondyle and common flexor origin (golfer’s elbow).
The joints between the trochlear notch of the ulna and the trochlea of the humerus and between the head of the radius and the capitulum of the humerus are primarily involved with hingelike flexion and extension of the forearm on the arm and, together, are the principal articulations of the elbow joint.
The joint between the head of the radius and the radial notch of the ulna, the proximal radioulnar joint, is involved with pronation and supination of the forearm.
The synovial membrane originates from the edges of the articular cartilage and lines the radial fossa, the coronoid fossa, the olecranon fossa, the deep surface of the joint capsule, and the medial surface of the trochlea (Fig. 7.57).
The synovial membrane is separated from the fibrous membrane of the joint capsule by pads of fat in regions overlying the coronoid fossa, the olecranon fossa, and the radial fossa (Fig. 7.57). These fat pads accommodate the related bony processes during extension and flexion of the elbow. Attachments of the brachialis and triceps brachii muscles to the joint capsule overlying these regions pull the attached fat pads out of the way when the adjacent bony processes are moved into the fossae.
The fibrous membrane of the joint capsule overlies the synovial membrane, encloses the joint, and attaches to the medial epicondyle and the margins of the olecranon, coronoid, and radial fossae of the humerus (Fig. 7.58). It also attaches to the coronoid process and olecranon of the ulna. On the lateral side, the free inferior margin of the joint capsule passes around the neck of the radius from an anterior attachment to the coronoid process of the ulna to a posterior attachment to the base of the olecranon.
The fibrous membrane of the joint capsule is thickened medially and laterally to form collateral ligaments, which support the flexion and extension movements of the elbow joint (Fig. 7.58).
In addition, the external surface of the joint capsule is reinforced laterally where it cuffs the head of the radius with a strong anular ligament of radius (Fig. 7.58). Although this ligament blends with the fibrous membrane of the joint capsule in most regions, they are separate posteriorly. The anular ligament of radius also blends with the radial collateral ligament (Fig. 7.58).
The deep surface of the fibrous membrane of the joint capsule and the related anular ligament of radius that articulate with the sides of the radial head are lined by cartilage. A pocket of synovial membrane (sacciform recess) protrudes from the inferior free margin of the joint capsule and facilitates rotation of the radial head during pronation and supination (Fig. 7.58).
Vascular supply to the elbow joint is through an anastomotic network of vessels derived from collateral and recurrent branches of the brachial, profunda brachii, radial, and ulnar arteries.
The elbow joint is innervated predominantly by branches of the radial and musculocutaneous nerves, but there may be some innervation by branches of the ulnar and median nerves.
CUBITAL FOSSA
The cubital fossa is an important area of transition between the arm and the forearm. It is located anterior to the elbow joint and is a triangular depression formed between two forearm muscles (Fig. 7.61A):
Fig. 7.61 Cubital fossa. A. Margins. B. Contents. C. Position of the radial nerve. D. Superficial structures.
 the brachioradialis muscle originating from the lateral supraepicondylar ridge of the humerus, and
the brachioradialis muscle originating from the lateral supraepicondylar ridge of the humerus, and
 the pronator teres muscle originating from the medial epicondyle of the humerus.
the pronator teres muscle originating from the medial epicondyle of the humerus.
The base of the triangle is an imaginary horizontal line between the medial and lateral epicondyles. The bed or floor of the fossa is formed mainly by the brachialis muscle.
The major contents of the cubital fossa, from lateral to medial, are (Fig. 7.61B):
 the tendon of the biceps brachii muscle,
the tendon of the biceps brachii muscle,
The brachial artery normally bifurcates into the radial and ulnar arteries in the apex of the fossa, although this bifurcation may occur much higher in the arm, even in the axilla (Fig. 7.61B). When taking a blood pressure reading from a patient, the clinician places the stethoscope over the brachial artery in the cubital fossa.
The median nerve lies immediately medial to the brachial artery and leaves the fossa by passing between the ulnar and humeral heads of the pronator teres muscle (Fig. 7.61C).
The brachial artery and the median nerve are covered and protected anteriorly in the distal part of the cubital fossa by the bicipital aponeurosis (Fig. 7.61B). This flat connective tissue membrane passes between the medial side of the tendon of the biceps brachii muscle and deep fascia of the forearm. The sharp medial margin of the bicipital aponeurosis can often be felt.
The radial nerve lies just under the lip of the brachioradialis muscle, which forms the lateral margin of the fossa (Fig. 7.61C). In this position, the radial nerve divides into superficial and deep branches:
 The superficial branch continues into the forearm just deep to the brachioradialis muscle.
The superficial branch continues into the forearm just deep to the brachioradialis muscle.
 The deep branch passes between the two heads of the supinator muscle (Fig. 7.62) to access the posterior compartment of the forearm.
The deep branch passes between the two heads of the supinator muscle (Fig. 7.62) to access the posterior compartment of the forearm.
Fig. 7.62 Radial nerve in posterior compartment of forearm.
The ulnar nerve does not pass through the cubital fossa. Instead, it passes posterior to the medial epicondyle.
The roof of the cubital fossa is formed by superficial fascia and skin. The most important structure within the roof is the median cubital vein (Fig. 7.61D), which passes diagonally across the roof and connects the cephalic vein on the lateral side of the upper limb with the basilic vein on the medial side. The bicipital aponeurosis separates the median cubital vein from the brachial artery and median nerve. Other structures within the roof are cutaneous nerves—the medial cutaneous and lateral cutaneous nerves of the forearm.
Clinical app
Construction of a dialysis fistula
Many patients throughout the world require renal dialysis for kidney failure. The patient’s blood is filtered and cleaned by the dialysis machine. Blood therefore has to be taken from patients into the filtering device and then returned to them. This process of dialysis occurs over many hours and requires flow rates of 250 to 500 mL/min. To enable such large volumes of blood to be removed from and returned to the body, the blood is taken from vessels that have a high flow. As no veins in the peripheral limbs have such high flow, a surgical procedure is necessary to create such a system. In most patients, the brachial artery is anastomosed (joined) to the cephalic vein at the elbow, or the radial artery is anastomosed to the cephalic vein at the wrist. Some surgeons place an arterial graft between these vessels. After 6 weeks, the veins increase in size in response to their arterial blood flow and are amenable to direct cannulation or dialysis.
Clinical app
Blood pressure measurement
Blood pressure measurement is an extremely important physiologic parameter. High blood pressure (hypertension) requires treatment to prevent long-term complications such as stroke. Low blood pressure may be caused by extreme blood loss, widespread infection, or poor cardiac output (e.g., after myocardial infarction). Accurate measurement of blood pressure is essential.
Most clinicians use a sphygmomanometer and a stethoscope. The sphygmomanometer is a device that inflates a cuff around the midportion of the arm to compress the brachial artery against the humerus. The cuff is inflated so it exceeds the systolic blood pressure (greater than 120 mm Hg). The clinician places a stethoscope over the brachial artery in the cubital fossa and listens (auscultates) for the pulse. As the pressure in the arm cuff of the sphygmomanometer is reduced just below the level of the systolic blood pressure, the pulse becomes audible as a regular thumping sound. As the pressure in the sphygmomanometer continues to drop, the regular thumping sound becomes clearer. When the pressure in the sphygmomanometer is less than that of the diastolic blood pressure, the audible thumping sound becomes inaudible. Using the simple scale on the sphygmomanometer, the patient’s blood pressure can be determined. The normal range is 120/80 mm Hg (systolic blood pressure/diastolic blood pressure).
FOREARM
The forearm is the part of the upper limb that extends between the elbow joint and the wrist joint.
Structures pass between the forearm and the hand through, or anterior to, the carpal tunnel (Fig. 7.63A). The major exception is the radial artery, which passes dorsally around the wrist to enter the hand posteriorly.
The bone framework of the forearm consists of two parallel bones, the radius and the ulna (Figs. 7.63A, 7.65). The radius is lateral in position and is small proximally, where it articulates with the humerus, and large distally, where it forms the wrist joint with the carpal bones of the hand.
As in the arm, the forearm is divided into anterior and posterior compartments (Fig. 7.63B). In the forearm, these compartments are separated by:
 the attachment of deep fascia along the posterior border of the ulna.
the attachment of deep fascia along the posterior border of the ulna.
Muscles in the anterior compartment of the forearm flex the wrist and digits and pronate the hand. Muscles in the posterior compartment extend the wrist and digits and supinate the hand. Major nerves and vessels supply or pass through each compartment.
Bones
Shaft and distal end of radius
The shaft of the radius is narrow proximally, where it is continuous with the radial tuberosity and neck, and much broader distally, where it expands to form the distal end (Fig. 7.64).
Fig. 7.64 Shaft and distal end of the right radius.
Throughout most of its length, the shaft of the radius is triangular in cross-section, with (Fig. 7.64):
 three borders (anterior, posterior, and interosseous), and
three borders (anterior, posterior, and interosseous), and
 three surfaces (anterior, posterior, and lateral).
three surfaces (anterior, posterior, and lateral).
The anterior border begins on the medial side of the bone as a continuation of the radial tuberosity. In the superior third of the bone, it crosses the shaft diagonally, from medial to lateral, as the oblique line of the radius. The posterior border is distinct only in the middle third of the bone. The interosseous border is sharp and is the attachment site for the interosseous membrane, which links the radius to the ulna.
The anterior and posterior surfaces of the radius are generally smooth, whereas an oval roughening for the attachment of pronator teres marks approximately the middle of the lateral surface of the radius.
Viewed anteriorly, the distal end of the radius is broad and somewhat flattened anteroposteriorly (Fig. 7.64). Consequently, the radius has expansive anterior and posterior surfaces and narrow medial and lateral surfaces. Its anterior surface is smooth and unremarkable, except for the prominent sharp ridge that forms its lateral margin.
The posterior surface of the radius is characterized by the presence of a large dorsal tubercle (Fig. 7.64), which acts as a pulley for the tendon of one of the extensor muscles of the thumb (extensor pollicis longus). The medial surface is marked by a prominent facet for articulation with the distal end of the ulna (Fig. 7.64). The lateral surface of the radius is diamond shaped and extends distally as a radial styloid process (Fig. 7.64).
The distal end of the bone is marked by two facets for articulation with two carpal bones (the scaphoid and lunate) (Fig. 7.64).
Shaft and distal end of ulna
The shaft of the ulna is broad superiorly where it is continuous with the large proximal end and narrow distally to form a small distal head (Fig. 7.66). Like the radius, the shaft of the ulna is triangular in cross-section and has:
 three borders (anterior, posterior, and interosseous), and
three borders (anterior, posterior, and interosseous), and
 three surfaces (anterior, posterior, and medial).
three surfaces (anterior, posterior, and medial).
Fig. 7.66 Shaft and distal end of right ulna.
The anterior border is smooth and rounded. The posterior border is sharp and palpable along its entire length. The interosseous border is also sharp and is the attachment site for the interosseous membrane, which joins the ulna to the radius.
The anterior surface of the ulna is smooth, except distally, where there is a prominent linear roughening for the attachment of the pronator quadratus muscle. The medial surface is smooth and unremarkable. The posterior surface is marked by lines, which separate different regions of muscle attachments to bone.
The distal end of the ulna is small and characterized by a rounded head and the ulnar styloid process (Fig. 7.66). The anterolateral and distal part of the head is covered by articular cartilage. The ulnar styloid process originates from the posteromedial aspect of the ulna and projects distally.
Clinical app
Fractures of the radius and ulna
When a severe injury occurs to the forearm it usually involves both bones, resulting in either fracture of both bones or more commonly a fracture of one bone and a dislocation of the other. Commonly, the mechanism of injury and the age of the patient determine which of these are likely to occur. Whenever a fracture of the radius or ulna is demonstrated radiographically, further images of the elbow and wrist should be obtained to exclude dislocations.
Joints
Distal radioulnar joint
The distal radioulnar joint occurs between the articular surface of the head of the ulna, with the ulnar notch on the end of the radius, and with a fibrous articular disc, which separates the radioulnar joint from the wrist joint (Fig. 7.67).
Fig. 7.67 Distal radioulnar joint and the interosseous membrane.
Synovial membrane is attached to the margins of the distal radioulnar joint and is covered on its external surface by a fibrous joint capsule.
The distal radioulnar joint allows the distal end of the radius to move anteromedially over the ulna.
Interosseous membrane
The interosseous membrane is a thin fibrous sheet that connects the medial and lateral borders of the radius and ulna, respectively (Fig. 7.67). Collagen fibers within the sheet pass predominantly inferiorly from the radius to the ulna.
The interosseous membrane has a free upper margin, which is situated just inferior to the radial tuberosity, and a small circular aperture in its distal third. Vessels pass between the anterior and posterior compartments superior to the upper margin and through the inferior aperture.
The interosseous membrane connects the radius and ulna without restricting pronation and supination and provides attachment for muscles in the anterior and posterior compartments. The orientation of fibers in the membrane is also consistent with its role in transferring forces from the radius to the ulna and ultimately, therefore, from the hand to the humerus.
Pronation and supination
Pronation and supination of the hand occur entirely in the forearm and involve rotation of the radius at the elbow and movement of the distal end of the radius over the ulna (Fig. 7.68).
Fig. 7.68 Pronation and supination.
At the elbow, the superior articular surface of the radial head spins on the capitulum while, at the same time, the articular surface on the side of the head slides against the radial notch of the ulna and adjacent areas of the joint capsule and anular ligament of radius. At the distal radioulnar joint, the ulnar notch of the radius slides anteriorly over the convex surface of the head of the ulna. During these movements, the bones are held together by:
 the anular ligament of radius at the proximal radioulnar joint,
the anular ligament of radius at the proximal radioulnar joint,
 the interosseous membrane along the lengths of the radius and ulna, and
the interosseous membrane along the lengths of the radius and ulna, and
 the articular disc at the distal radioulnar joint.
the articular disc at the distal radioulnar joint.
Because the hand articulates predominantly with the radius, the translocation of the distal end of the radius medially over the ulna moves the hand from the palm-anterior (supinated) position to the palm-posterior (pronated) position.
Two muscles (biceps brachii and supinator) supinate and two muscles (pronator teres and pronator quadratus) pronate the hand (Fig. 7.68).
Abduction of the ulna during pronation
Abduction of the distal end of the ulna occurs during pronation to maintain the position of the palm of the hand over a central point (Fig. 7.69). The muscle involved in this movement is the anconeus muscle, which is a triangular muscle in the posterior compartment of the forearm that runs from the lateral epicondyle to the lateral surface of the proximal end of the ulna.
Fig. 7.69 Abduction of the distal end of the ulna by the anconeus muscle during pronation.
ANTERIOR COMPARTMENT OF THE FOREARM
Muscles
Muscles in the anterior (flexor) compartment of the forearm occur in three layers: superficial, intermediate, and deep. Generally, these muscles are associated with:
 flexion of the fingers including the thumb, and
flexion of the fingers including the thumb, and
All muscles in the anterior compartment of the forearm are innervated by the median nerve, except for the flexor carpi ulnaris muscle and the medial half of the flexor digitorum profundus muscle, which are innervated by the ulnar nerve.
Superficial layer
All four muscles in the superficial layer—the flexor carpi ulnaris, palmaris longus, flexor carpi radialis, and pronator teres—have a common origin from the medial epicondyle of the humerus, and, except for the pronator teres, extend distally from the forearm into the hand (Table 7.10, Fig. 7.70).
Table 7.10 Superficial layer of muscles in the anterior compartment of the forearm (spinal segments indicated in bold are themajorsegments innervating the muscle)
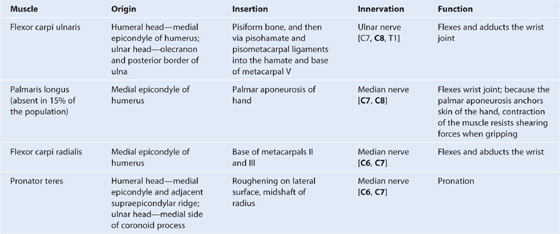
Intermediate layer
The only muscle in the intermediate layer of the anterior compartment of forearm is the flexor digitorum superficialis muscle (Table 7.11, Fig. 7.71).
Table 7.11 Intermediate layer of muscles in the anterior compartment of the forearm (spinal segments indicated in bold are themajor segments innervating the muscle)
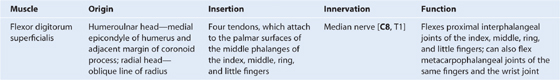
Fig. 7.71 Intermediate layer of forearm muscles.
Deep layer
There are three deep muscles in the anterior compartment of the forearm: the flexor digitorum profundus, flexor pollicis longus, and pronator quadratus (Table 7.12, Fig. 7.72).
Table 7.12 Deep layer of muscles in the anterior compartment of the forearm (spinal segments indicated in bold are the majorsegments innervating the muscle)
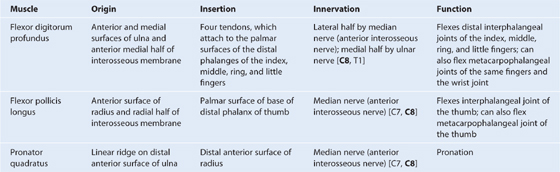
Fig. 7.72 Deep layer of forearm muscles.
Arteries and veins
The largest arteries in the forearm are in the anterior compartment, pass distally to supply the hand, and give rise to vessels that supply the posterior compartment (Fig. 7.73).
Fig. 7.73 Arteries of the anterior compartment of the forearm.
The brachial artery enters the forearm from the arm by passing through the cubital fossa. At the apex of the cubital fossa, it divides into its two major branches, the radial and ulnar arteries.
Radial artery
The radial artery originates from the brachial artery at approximately the neck of the radius and passes along the lateral aspect of the forearm (Fig. 7.73). It is:
 just deep to the brachioradialis muscle in the proximal half of the forearm;
just deep to the brachioradialis muscle in the proximal half of the forearm;
In the distal forearm, the radial artery lies immediately lateral to the large tendon of the flexor carpi radialis muscle and directly anterior to the pronator quadratus muscle and the distal end of the radius (Fig. 7.73).
The radial artery leaves the forearm, passes around the lateral side of the wrist, and penetrates the posterolateral aspect of the hand between the bases of metacarpals I and II (Fig. 7.73). Branches of the radial artery in the hand often provide the major blood supply to the thumb and lateral side of the index finger.
Branches of the radial artery originating in the forearm include:
 a radial recurrent artery, which contributes to an anastomotic network around the elbow joint and to numerous vessels that supply muscles on the lateral side of the forearm (see Fig. 7.53B);
a radial recurrent artery, which contributes to an anastomotic network around the elbow joint and to numerous vessels that supply muscles on the lateral side of the forearm (see Fig. 7.53B);
 a somewhat larger branch, the superficial palmar branch, which enters the hand by passing through, or superficial to, the thenar muscles at the base of the thumb (Fig. 7.73), which anastomoses with the superficial palmar arch formed by the ulnar artery.
a somewhat larger branch, the superficial palmar branch, which enters the hand by passing through, or superficial to, the thenar muscles at the base of the thumb (Fig. 7.73), which anastomoses with the superficial palmar arch formed by the ulnar artery.
Ulnar artery
The ulnar artery is larger than the radial artery and passes down the medial side of the forearm (Fig. 7.73). It leaves the cubital fossa by passing deep to the pronator teres muscle, and then passes through the forearm in the fascial plane between the flexor carpi ulnaris and flexor digitorum profundus muscles.
In the distal forearm, the ulnar artery often remains tucked under the anterolateral lip of the flexor carpi ulnaris tendon.
In distal regions of the forearm, the ulnar nerve is immediately medial to the ulnar artery.
The ulnar artery leaves the forearm, enters the hand by passing lateral to the pisiform bone and superficial to the flexor retinaculum of the wrist, and arches over the palm (Fig. 7.73). It is often the major blood supply to the medial three and one-half digits.
Branches of the ulnar artery that arise in the forearm include:
 numerous muscular arteries, which supply surrounding muscles;
numerous muscular arteries, which supply surrounding muscles;
 the common interosseous artery, which divides into anterior and posterior interosseous arteries (Fig. 7.73); and
the common interosseous artery, which divides into anterior and posterior interosseous arteries (Fig. 7.73); and
 two small carpal arteries (dorsal carpal branch and palmar carpal branch), which supply the wrist.
two small carpal arteries (dorsal carpal branch and palmar carpal branch), which supply the wrist.
The posterior interosseous artery passes dorsally over the proximal margin of the interosseous membrane into the posterior compartment of the forearm.
The anterior interosseous artery passes distally along the anterior aspect of the interosseous membrane and supplies muscles of the deep compartment of the forearm and the radius and ulna (Fig. 7.73). It has numerous branches, which perforate the interosseous membrane to supply deep muscles of the posterior compartment; it also has a small branch, which contributes to the vascular network around the carpal bones and joints. Perforating the interosseous membrane in the distal forearm, the anterior interosseous artery terminates by joining the posterior interosseous artery.
Veins
Deep veins of the anterior compartment generally accompany the arteries and ultimately drain into brachial veins associated with the brachial artery in the cubital fossa.
Nerves
Nerves in the anterior compartment of the forearm are the median and ulnar nerves, and the superficial branch of the radial nerve (Fig. 7.74).
Fig. 7.74 Nerves of anterior forearm.
Median nerve
The median nerve innervates the muscles in the anterior compartment of the forearm except for the flexor carpi ulnaris and the medial part of the flexor digitorum profundus (ring and little fingers). It leaves the cubital fossa by passing between the two heads of the pronator teres muscle and passing between the humeroulnar and radial heads of the flexor digitorum superficialis muscle (Fig. 7.74).
The median nerve continues a straight linear course distally down the forearm in the fascia on the deep surface of the flexor digitorum superficialis muscle. Just proximal to the wrist, it moves around the lateral side of the muscle and becomes more superficial in position, lying between the tendons of the palmaris longus and flexor carpi radialis muscles. It leaves the forearm and enters the palm of the hand by passing through the carpal tunnel deep to the flexor retinaculum (Fig. 7.74).
Most branches to the muscles in the superficial and intermediate layers of the forearm originate medially from the nerve just distal to the elbow joint (Fig. 7.74):
The largest branch of the median nerve in the forearm is the anterior interosseous nerve, which originates between the two heads of the pronator teres. It passes distally down the forearm with the anterior interosseous artery, innervates the muscles in the deep layer (the flexor pollicis longus, the lateral half of flexor digitorum profundus, and pronator quadratus) and terminates as articular branches to joints of the distal forearm and wrist.
A small palmar branch originates from the median nerve in the distal forearm immediately proximal to the flexor retinaculum, passes superficial to the flexor retinaculum of the wrist into the hand, and innervates the skin over the base and central palm.
Ulnar nerve
The ulnar nerve passes through the forearm and into the hand, where most of its major branches occur. In the forearm, the ulnar nerve innervates only the flexor carpi ulnaris muscle and the medial part (ring and little fingers) of the flexor digitorum profundus muscle (Fig. 7.74).
The ulnar nerve enters the anterior compartment of the forearm by passing posteriorly around the medial epicondyle of the humerus and between the humeral and ulnar heads of the flexor carpi ulnaris muscle. After passing down the medial side of the forearm in the plane between the flexor carpi ulnaris and the flexor digitorum profundus muscles, it lies under the lateral lip of the tendon of the flexor carpi ulnaris proximal to the wrist.
The ulnar artery is lateral to the ulnar nerve in the distal two-thirds of the forearm, and both the ulnar artery and nerve enter the hand by passing superficial to the flexor retinaculum and immediately lateral to the pisiform bone (Fig. 7.74).
In the forearm the ulnar nerve gives rise to:
 two small cutaneous branches—the palmar branch originates in the middle of the forearm and passes into the hand to supply skin on the medial side of the palm (Fig. 7.74); the larger dorsal branch originates from the ulnar nerve in the distal forearm and passes posteriorly deep to the tendon of the flexor carpi ulnaris and innervates skin on the posteromedial side of the back of the hand and most skin on the posterior surfaces of the medial one and one-half digits (Fig. 7.74).
two small cutaneous branches—the palmar branch originates in the middle of the forearm and passes into the hand to supply skin on the medial side of the palm (Fig. 7.74); the larger dorsal branch originates from the ulnar nerve in the distal forearm and passes posteriorly deep to the tendon of the flexor carpi ulnaris and innervates skin on the posteromedial side of the back of the hand and most skin on the posterior surfaces of the medial one and one-half digits (Fig. 7.74).
Radial nerve
The radial nerve bifurcates into deep and superficial branches under the margin of the brachioradialis muscle in the lateral border of the cubital fossa (Fig. 7.74).
The deep branch is predominantly motor and passes between the two heads of the supinator muscle to access and supply muscles in the posterior compartment of the forearm.
The superficial branch of the radial nerve is sensory. It passes down the anterolateral aspect of the forearm deep to the brachioradialis muscle and in association with the radial artery. Approximately two-thirds of the way down the forearm, the superficial branch of the radial nerve passes laterally and posteriorly around the radial side of the forearm deep to the tendon of the brachioradialis. The nerve continues into the hand where it innervates skin on the posterolateral surface.
POSTERIOR COMPARTMENT OF FOREARM
Muscles
Muscles in the posterior compartment of the forearm occur in two layers: a superficial and a deep layer. The muscles are associated with:
 extension of the fingers and thumb, and
extension of the fingers and thumb, and
All muscles in the posterior compartment of the forearm are innervated by the radial nerve.
Superficial layer
The seven muscles in the superficial layer are the brachioradialis, extensor carpi radialis longus, extensor carpi radialis brevis, extensor digitorum, extensor digiti minimi, extensor carpi ulnaris, and anconeus (Table 7.13, Fig. 7.75). All have a common origin from the supraepicondylar ridge and lateral epicondyle of the humerus and, except for the brachioradialis and anconeus, extend as tendons into the hand.
Table 7.13 Superficial layer of muscles in the posterior compartment of the forearm (spinal segments indicated in bold are the major segments innervating the muscle)
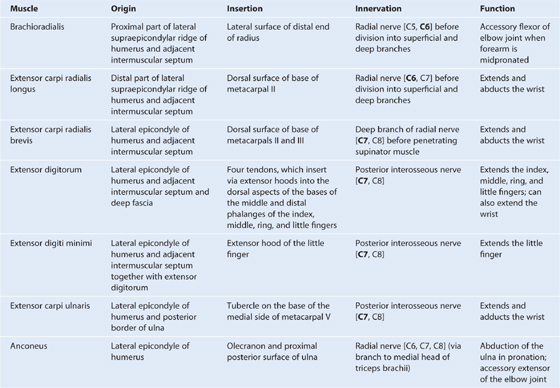
Deep layer
The deep layer of the posterior compartment of the forearm consists of five muscles: supinator, abductor pollicis longus, extensor pollicis brevis, extensor pollicis longus, and extensor indicis (Table 7.14, Fig. 7.76).
Table 7.14 Deep layer of muscles in the posterior compartment of the forearm (spinal segments indicated in bold are the major segments innervating the muscle)
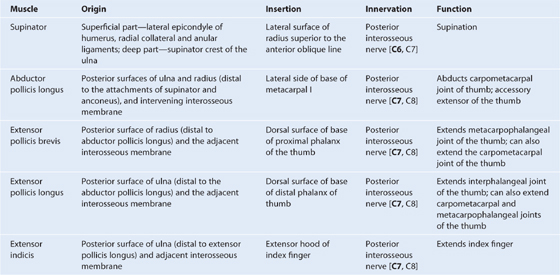
Fig. 7.76 Deep layer of muscles in the posterior compartment of the forearm.
Except for the supinator muscle, all these deep layer muscles originate from the posterior surfaces of the radius, ulna, and interosseous membrane and pass into the thumb and fingers.
Three of these muscles—the abductor pollicis longus, extensor pollicis brevis, and extensor pollicis longus—emerge from between the extensor digitorum and the extensor carpi radialis brevis tendons of the superficial layer and pass into the thumb.
Two of these three “outcropping” muscles (the abductor pollicis longus and extensor pollicis brevis) form a distinct muscular bulge in the distal posterolateral surface of the forearm.
All muscles of the deep layer are innervated by the posterior interosseous nerve, the continuation of the deep branch of the radial nerve.
Arteries and veins
The blood supply to the posterior compartment of the forearm occurs predominantly through branches of the radial, posterior interosseous, and anterior interosseous arteries (Fig. 7.77; also see Fig. 7.73).
Fig 7.77 Arteries and radial nerve in the posterior compartment of the forearm.
Posterior interosseous artery
The posterior interosseous artery originates in the anterior compartment from the common interosseous branch of the ulnar artery and passes posteriorly over the proximal margin of the interosseous membrane and into the posterior compartment of the forearm (see Fig. 7.73). It contributes a branch, the recurrent interosseous artery (see Fig. 7.53B) to the vascular network around the elbow joint and then passes between the supinator and abductor pollicis longus muscles to supply the superficial extensors (Fig. 7.77). After receiving the terminal end of the anterior interosseous artery, the posterior interosseous artery terminates by joining the dorsal carpal arch of the wrist.
Anterior interosseous artery
The anterior interosseous artery, also a branch of the common interosseous branch of the ulnar artery (see Fig. 7.73), is situated in the anterior compartment of the forearm on the interosseous membrane. It has numerous perforating branches, which pass directly through the interosseous membrane to supply deep muscles of the posterior compartment. The terminal end of the anterior interosseous artery passes posteriorly through an aperture in the interosseous membrane in distal regions of the forearm to join the posterior interosseous artery (Fig. 7.77).
Radial artery
The radial artery has muscular branches, which contribute to the supply of the extensor muscles on the radial side of the forearm.
Veins
Deep veins of the posterior compartment generally accompany the arteries. They ultimately drain into brachial veins associated with the brachial artery in the cubital fossa.
Nerves
Radial nerve
The nerve of the posterior compartment of the forearm is the radial nerve (Fig. 7.77). Most of the muscles are innervated by the deep branch, which originates from the radial nerve in the lateral wall of the cubital fossa deep to the brachioradialis muscle and becomes the posterior interosseous nerve (Fig. 7.77), after emerging from between the two heads of the supinator muscle in the posterior compartment of the forearm (Fig. 7.77).
In the lateral wall of the cubital fossa, and before dividing into superficial and deep branches, the radial nerve innervates the brachioradialis and extensor carpi radialis longus muscles.
The deep branch innervates the extensor carpi radialis brevis, then passes between the two heads of the supinator muscle and follows the plane of separation between the two heads dorsally and laterally around the proximal shaft of the radius to the posterior aspect of the forearm. It supplies the supinator muscle and then emerges, as the posterior interosseous nerve, from the muscle to lie between the superficial and deep layers of muscles.
The posterior interosseous nerve supplies the remaining muscles in the posterior compartment and terminates as articular branches, which pass deep to the extensor pollicis longus muscle to reach the wrist.
Surface Anatomy
Identifying tendons and locating major vessels and nerves in the distal forearm
Tendons that pass from the forearm into the hand are readily visible in the distal forearm and can be used as landmarks to locate major vessels and nerves.
In the anterior aspect of the distal forearm, the tendons of the flexor carpi radialis, flexor carpi ulnaris, and palmaris longus muscles can be easily located either by palpating or by asking a patient to flex the wrist against resistance (Fig. 7.78A).
The tendon of flexor carpi radialis is located approximately at the junction between the lateral and middle thirds of an imaginary line drawn transversely across the distal forearm. The radial artery is immediately lateral to this tendon and this site is used for taking a radial pulse (Fig. 7.78A).
The tendon of the flexor carpi ulnaris is easily palpated along the medial margin of the forearm and inserts on the pisiform, which can also be palpated by following the tendon to the base of the hypothenar eminence of the hand (Fig. 7.78A). The ulnar artery and ulnar nerve travel through the distal forearm and into the hand under the lateral lip of the flexor carpi ulnaris tendon and lateral to the pisiform (Fig. 7.78A).
The palmaris longus tendon may be absent, but when present, lies medial to the flexor carpi radialis tendon and is particularly prominent when the wrist is flexed against resistance (Fig. 7.78A). The median nerve is also medial to the flexor carpi radialis tendon and lies under the palmaris longus tendon.
The long tendons of the digits of the hand are deep to the median nerve and between the long flexors of the wrist. Their position can be visualized by rapidly and repeatedly flexing and extending the fingers from medial to lateral.
In the posterior distal forearm and wrist, the tendons of the extensor digitorum (Fig. 7.78B) are in the midline and radiate into the index, middle, ring, and little fingers from the wrist.
The distal ends of the tendons of the extensor carpi radialis longus and brevis muscles are on the lateral side of the wrist (Fig. 7.78C) and can be accentuated by making a tight fist and extending the wrist against resistance.
The tendon of the extensor carpi ulnaris can be felt on the far medial side of the wrist between the distal end of the ulna and the wrist (Fig. 7.78B).
Hyperextension and abduction of the thumb reveals the anatomical snuffbox (Fig. 7.78D). The medial margin of this triangular area is the tendon of the extensor pollicis longus, which swings around the dorsal tubercle of the radius and then travels into the thumb. The lateral margin is formed by the tendons of the extensor pollicis brevis and abductor pollicis longus. The radial artery passes through the anatomical snuffbox when traveling laterally around the wrist to reach the back of the hand and penetrate the base of the first dorsal interosseous muscle to access the deep aspect of the palm of the hand. The pulse of the radial artery can be felt in the floor of the anatomical snuffbox in the relaxed wrist (Fig. 7.78D). The cephalic vein crosses the roof of the anatomical snuffbox, and cutaneous branches of the radial nerve can be felt by moving a finger back and forth along the tendon of the extensor pollicis longus muscle.
HAND
The hand (Fig. 7.79) is the region of the upper limb distal to the wrist joint and is a mechanical and sensory tool. It is subdivided into three parts:
 the digits (five fingers including the thumb).
the digits (five fingers including the thumb).
The five digits consist of the laterally positioned thumb; medial to the thumb are the remaining four fingers—the index, middle, ring, and little fingers.
In the normal resting position, the fingers form a flexed arcade, with the little finger flexed most and the index finger flexed least. In the anatomical position, the fingers are extended.
The hand has an anterior surface (palm) and a dorsal surface (dorsum of hand).
Abduction and adduction of the fingers are defined with respect to the long axis of the middle finger (Fig. 7.79). In the anatomical position, the long axis of the thumb is rotated 90° to the rest of the digits so that the pad of the thumb points medially; consequently, movements of the thumb are defined at right angles to the movements of the other digits of the hand.
Bones
There are three groups of bones in the hand (Figs. 7.80; 7.81):
 The eight carpal bones are the bones of the wrist;
The eight carpal bones are the bones of the wrist;
 The five metacarpals (I to V) are the bones of the metacarpus;
The five metacarpals (I to V) are the bones of the metacarpus;
 The phalanges are the bones of the digits—the thumb has only two, the rest of the digits have three (Fig. 7.80).
The phalanges are the bones of the digits—the thumb has only two, the rest of the digits have three (Fig. 7.80).
Fig 7.80 Bones of the hand and wrist.
The carpal bones and metacarpals of the index, middle, ring, and little fingers (metacarpals II to V) tend to function as a unit and form much of the bony framework of the palm. The metacarpal bone of the thumb functions independently and has increased flexibility at the carpometacarpal joint to provide opposition of the thumb to the fingers.
Carpal bones
The small carpal bones of the wrist are arranged in two rows, a proximal and a distal row, each consisting of four bones (Fig. 7.80).
Proximal row
From lateral to medial and when viewed from anteriorly, the proximal row of bones consists of (Fig. 7.80):
 the lunate, which has a crescent shape,
the lunate, which has a crescent shape,
 the three-sided triquetrum, and
the three-sided triquetrum, and
The pisiform is a sesamoid bone in the tendon of the flexor carpi ulnaris and articulates with the anterior surface of the triquetrum.
The scaphoid has a prominent tubercle on its lateral palmar surface that is directed anteriorly.
Distal row
From lateral to medial and when viewed from anteriorly, the distal row of carpal bones consists of (Fig. 7.80):
 the irregular four-sided trapezium,
the irregular four-sided trapezium,
 the capitate, which has a head, and
the capitate, which has a head, and
The trapezium articulates with the metacarpal bone of the thumb and has a distinct tubercle on its palmar surface that projects anteriorly.
The largest of the carpal bones, the capitate, articulates with the base of metacarpal III.
The hamate, which is positioned just lateral and distal to the pisiform, has a prominent hook (hook of hamate) on its palmar surface that projects anteriorly.
Articular surfaces
The carpal bones have numerous articular surfaces (Fig. 7.80). All of them articulate with each other, and the carpal bones in the distal row articulate with the metacarpals of the digits. With the exception of the metacarpal of the thumb, all movements of the metacarpal bones on the carpal bones are limited.
The expansive proximal surfaces of the scaphoid and lunate articulate with the radius to form the wrist joint (Figs. 7.80, 7.81B).
Carpal arch
The carpal bones do not lie in a flat plane; rather they form an arch whose base is directed anteriorly (Fig. 7.80). The lateral side of this base is formed by the tubercles of the scaphoid and trapezium. The medial side is formed by the pisiform and the hook of hamate.
The flexor retinaculum attaches to, and spans the distance between, the medial and lateral sides of the base to form the anterior wall of the so-called carpal tunnel. The sides and roof of the carpal tunnel are formed by the arch of the carpal bones.
Metacarpals
Each of the five metacarpal bones is related to one digit (Figs. 7.80, 7.81A):
 Metacarpal I is related to the thumb.
Metacarpal I is related to the thumb.
 Metacarpals II to V are related to the index, middle, ring, and little fingers, respectively.
Metacarpals II to V are related to the index, middle, ring, and little fingers, respectively.
Each metacarpal consists of a base, a shaft (body), and distally, a head.
All of the bases of the metacarpals articulate with the carpal bones; in addition, the bases of the metacarpal bones of the fingers articulate with each other.
All of the heads of the metacarpal bones articulate with the proximal phalanges of the digits. The heads form the knuckles on the dorsal surface of the hand when the fingers are flexed.
Phalanges
The phalanges are the bones of the digits (Figs. 7.80, 7.81A):
 The thumb has two—a proximal and a distal phalanx.
The thumb has two—a proximal and a distal phalanx.
 The rest of the digits have three—a proximal, a middle, and a distal phalanx.
The rest of the digits have three—a proximal, a middle, and a distal phalanx.
Each phalanx has a base, a shaft (body), and distally, a head.
The base of each proximal phalanx articulates with the head of the related metacarpal bone.
The head of each distal phalanx is nonarticular and flattened into a crescent-shaped palmar tuberosity, which lies under the palmar pad at the end of the digit.
Imaging app
Visualizing the hand and wrist joint
Fig. 7.81 Hand and wrist joint. A. Radiograph of a normal hand and wrist joint (anteroposterior view). B. Magnetic resonance image of a normal wrist joint in the coronal plane.
Joints
Wrist joint
The wrist joint is a synovial joint between the distal end of the radius and the articular disc overlying the distal end of the ulna, and the scaphoid, lunate, and triquetrum (Fig. 7.81B; also see Fig. 7.80). Together, the articular surfaces of the carpals form an oval shape with a convex contour, which articulates with the corresponding concave surface of the radius and articular disc.
The wrist joint allows movement around two axes. The hand can be abducted, adducted, flexed, and extended at the wrist joint.
The capsule of the wrist joint is reinforced by palmar radiocarpal, palmar ulnocarpal, and dorsal radiocarpal ligaments. In addition, radial and ulnar collateral ligaments of the wrist joint span the distance between the styloid processes of the radius and ulna and the adjacent carpal bones. These ligaments reinforce the medial and lateral sides of the wrist joint and support them during flexion and extension.
Carpal joints
The synovial joints between the carpal bones share a common articular cavity. The joint capsule of the joints is reinforced by numerous ligaments.
Although movement at the carpal joints (intercarpal joints) is limited, they do contribute to the positioning of the hand in abduction, adduction, flexion, and, particularly, extension.
Carpometacarpal joints
There are five carpometacarpal joints between the metacarpals and the related distal row of carpal bones (Fig. 7.81B; also see Fig. 7.80).
The saddle joint, between metacarpal I and the trapezium, imparts a wide range of mobility to the thumb that is not a feature of the rest of the digits. Movements at this carpometacarpal joint are flexion, extension, abduction, adduction, rotation, and circumduction.
The carpometacarpal joints between metacarpals II to V and the carpal bones are much less mobile than the carpometacarpal joint of the thumb, allowing only limited gliding movements. Movement of the joints increases medially, so metacarpal V slides to the greatest degree. This can be best observed on the dorsal surface of the hand as it makes a fist.
Metacarpophalangeal joints
The joints between the distal heads of the metacarpals and the proximal phalanges of the digits are condylar joints, which allow flexion, extension, abduction, adduction, circumduction, and limited rotation. The capsule of each joint is reinforced by the palmar ligament and by medial and lateral collateral ligaments (Fig. 7.82).
Fig. 7.82 Deep transverse metacarpal ligaments.
Deep transverse metacarpal ligaments
The three deep transverse metacarpal ligaments (Fig. 7.82) are thick bands of connective tissue connecting the palmar ligaments of the metacarpophalangeal joints of the fingers to each other. They are important because, by linking the heads of the metacarpal bones together, they restrict the movement of these bones relative to each other. As a result, they help form a unified skeletal framework for the palm of the hand.
Significantly, a deep transverse metacarpal ligament does not occur between the palmar ligament of the metacarpophalangeal joint of the thumb and the palmar ligament of the index finger. The absence of this ligament, and the presence of a saddle joint between metacarpal I and the trapezium, are responsible for the increased mobility of the thumb relative to the rest of the digits of the hand.
Interphalangeal joints of hand
The interphalangeal joints of the hand are hinge joints that allow mainly flexion and extension. They are reinforced by medial and lateral collateral ligaments and palmar ligaments.
Clinical app
Fracture of the scaphoid and avascular necrosis of the proximal scaphoid
The most common carpal injury is a fracture across the waist of the scaphoid bone (Fig. 7.83B). In approximately 10% of individuals, the scaphoid bone has a sole blood supply from the radial artery, which enters through the distal portion of the bone to supply the proximal portion. When a fracture occurs across the waist of the scaphoid, the proximal portion therefore undergoes avascular necrosis.
Carpal tunnel and structures at the wrist
The carpal tunnel is formed anteriorly at the wrist by a deep arch formed by the carpal bones and the flexor retinaculum (Fig. 7.84).
Fig. 7.84 Carpal tunnel. Structure and relations.
The base of the carpal arch is formed medially by the pisiform and the hook of the hamate and laterally by the tubercles of the scaphoid and trapezium.
The flexor retinaculum is a thick connective tissue ligament that bridges the space between the medial and lateral sides of the base of the arch and converts the carpal arch into the carpal tunnel.
The four tendons of the flexor digitorum profundus, the four tendons of the flexor digitorum superficialis, and the tendon of the flexor pollicis longus pass through the carpal tunnel, as does the median nerve (Fig. 7.84).
The flexor retinaculum holds the tendons to the bony plane at the wrist and prevents them from “bowing.”
Free movement of the tendons in the carpal tunnel is facilitated by synovial sheaths, which surround the tendons. All the tendons of the flexor digitorum profundus and flexor digitorum superficialis are surrounded by a single synovial sheath; a separate sheath surrounds the tendon of the flexor pollicis longus. The median nerve is anterior to the tendons in the carpal tunnel.
The tendon of the flexor carpi radialis is surrounded by a synovial sheath and passes through a tubular compartment formed by the attachment of the lateral aspect of the flexor retinaculum to the margins of a groove on the medial side of the tubercle of trapezium.
The ulnar artery, ulnar nerve, and the tendon of the palmaris longus pass into the hand anterior to the flexor retinaculum and therefore do not pass through the carpal tunnel (Fig. 7.84). The tendon of the palmaris longus is not surrounded by a synovial sheath.
The extensor tendons pass into the hand on the medial, lateral, and posterior surfaces of the wrist in six compartments defined by an extensor retinaculum and lined by synovial sheaths (Fig. 7.84):
Clinical app
De Quervain syndrome
De Quervain syndrome is an inflammatory disorder that occurs within the first dorsal extensor compartment and involves the extensor pollicis brevis and abductor pollicis longus tendon and their common tendon sheath. Patients typically present with significant wrist pain preventing appropriate flexion/extension and abduction of the thumb. The cause of this disorder is often overuse. For example, the syndrome is common in young mothers who are constantly lifting young children. Other causes include inflammatory disorders such as rheumatoid arthritis.
Surface Anatomy
Position of the flexor retinaculum and the recurrent branch of the median nerve
The proximal margin of the flexor retinaculum can be determined using two bony landmarks (Fig. 7.85).
The pisiform bone is readily palpable at the distal end of the flexor carpi ulnaris tendon.
The tubercle of the scaphoid can be palpated at the distal end of the flexor carpi radialis tendon as it enters the wrist.
An imaginary line between these two points marks the proximal margin of the flexor retinaculum. The distal margin of the flexor retinaculum is approximately deep to the point where the anterior margin of the thenar eminence meets the hypothenar eminence near the base of the palm.
The recurrent branch of the median nerve lies deep to the skin and deep fascia overlying the anterior margin of the thenar eminence near the midline of the palm (Fig. 7.85).
Clinical app
Carpal tunnel syndrome
Carpal tunnel syndrome is an entrapment syndrome caused by pressure on the median nerve within the carpal tunnel.
Patients typically report pain and pins and needles in the distribution of the median nerve in the hand. Weakness and loss of muscle bulk of the thenar muscles may also occur. Gently tapping over the median nerve (in the region of the flexor retinaculum) readily produces these symptoms (Tinel’s sign).
Palmar aponeurosis
The palmar aponeurosis is a triangular condensation of deep fascia that covers the palm and is anchored to the skin in distal regions (Fig. 7.86).
Fig. 7.86 Palmar aponeurosis.
Transverse fibers interconnect the more longitudinally arranged bundles that continue into the digits.
Vessels, nerves, and long flexor tendons lie deep to the palmar aponeurosis in the palm.
Anatomical snuffbox
The “anatomical snuffbox” is a term given to the triangular depression formed on the posterolateral side of the wrist and metacarpal I by the extensor tendons passing into the thumb (Fig. 7.87). Historically, ground tobacco (snuff) was placed in this depression before being inhaled into the nose. The base of the triangle is at the wrist and the apex is directed into the thumb. The impression is most apparent when the thumb is extended:
 The medial border is formed by the tendon of the extensor pollicis longus.
The medial border is formed by the tendon of the extensor pollicis longus.
Fig. 7.87 Anatomical snuffbox.
The radial artery passes obliquely through the anatomical snuffbox, deep to the extensor tendons of the thumb, and lies adjacent to the scaphoid and trapezium.
Terminal parts of the superficial branch of the radial nerve pass subcutaneously over the snuffbox as does the origin of the cephalic vein from the dorsal venous arch of the hand.
Fibrous digital sheaths
After exiting the carpal tunnel, the tendons of the flexor digitorum superficialis and profundus muscles cross the palm and enter fibrous sheaths on the palmar aspect of the digits (Fig. 7.88). These fibrous sheaths:
 begin proximally, anterior to the metacarpophalangeal joints, and extend to the distal phalanges;
begin proximally, anterior to the metacarpophalangeal joints, and extend to the distal phalanges;
 hold the tendons to the bony plane and prevent the tendons from bowing when the digits are flexed.
hold the tendons to the bony plane and prevent the tendons from bowing when the digits are flexed.
Fig. 7.88 Fibrous digital sheaths and synovial sheaths of the hand.
Within each tunnel, the tendons are surrounded by a synovial sheath. The synovial sheaths of the thumb and little finger are continuous with the sheaths associated with the tendons in the carpal tunnel (Fig. 7.88).
Clinical app
Tenosynovitis
Tenosynovitis is inflammation of a tendon and its sheath. The condition may be due to overuse; however, it can also be associated with other disorders such as rheumatoid arthritis and connective tissue pathologies. If the inflammation becomes severe and ensuing fibrosis occurs, the tendon will not run smoothly within the tendon sheath and typically within the fingers, the tendon may stick or may require excess force to fully extend and flex producing a “triggering” phenomenon.
Extensor hoods
The tendons of the extensor digitorum and extensor pollicis longus muscles pass onto the dorsal aspect of the digits and expand over the proximal phalanges to form complex “extensor hoods” or “dorsal digital expansions” (Fig. 7.89). The tendons of the extensor digiti minimi, extensor indicis, and extensor pollicis brevis muscles join these hoods.
Fig. 7.89 Extensor hood.
Each extensor hood is triangular, with:
 the apex attached to the distal phalanx;
the apex attached to the distal phalanx;
In addition to other attachments, many of the intrinsic muscles of the hand insert into the free margin of the hood on each side. By inserting into the extensor hood, these intrinsic muscles are responsible for complex delicate movements of the digits that could not be accomplished with the long flexor and extensor tendons alone.
In the index, middle, ring, and little fingers, the lumbrical, interossei, and abductor digiti minimi muscles attach to the extensor hoods. In the thumb, the adductor pollicis and abductor pollicis brevis muscles insert into and anchor the extensor hood.
Because force from the small intrinsic muscles of the hand is applied to the extensor hood distal to the fulcrum of the metacarpophalangeal joints, the muscles flex these joints (Fig. 7.89). Simultaneously, the force is transferred dorsally through the hood to extend the interphalangeal joints. This ability to flex the metacarpophalangeal joints, while at the same time extending the interphalangeal joints, is entirely due to the intrinsic muscles of the hand working through the extensor hoods. This type of precision movement is used in the upstroke when writing a t (Fig. 7.89).
Muscles
The intrinsic muscles of the hand are the palmaris brevis, interossei, adductor pollicis, thenar, hypothenar, and lumbrical muscles (Table 7.15, Figs. 7.90 to 7.94). Unlike the extrinsic muscles that originate in the forearm, insert in the hand, and function in forcefully gripping (“power grip”) with the hand, the intrinsic muscles occur entirely in the hand and mainly execute precision movements (“precision grip”) with the fingers and thumb.
Table 7.15 Intrinsic muscles of the hand (spinal segments indicated in bold are the major segments innervating the muscle)
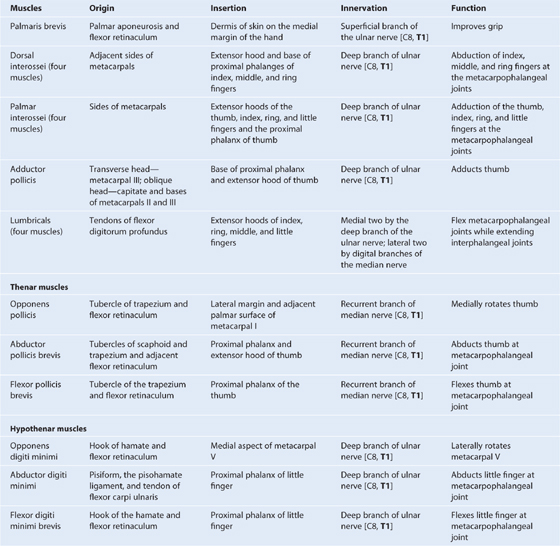
Fig. 7.90 Dorsal interossei (palmar view).
Fig. 7.91 Palmar interossei (palmar view).
Fig. 7.92 Adductor pollicis.
Fig. 7.93 Thenar and hypothenar muscles.
Fig. 7.94 Lumbrical muscles.
All of the intrinsic muscles of the hand are innervated by the deep branch of the ulnar nerve except for the three thenar and two lateral lumbrical muscles, which are innervated by the median nerve. The intrinsic muscles are predominantly innervated by spinal cord segment T1 with a contribution from C8.
Interossei
The four bipennate dorsal interossei are the most posterior of all of the intrinsic muscles and can be palpated through the skin on the posterior aspect of the hand (Fig. 7.90). The muscles lie between, and are attached to, the shafts of adjacent metacarpal bones (Fig. 7.90). Each muscle inserts both into the base of the proximal phalanx and into the extensor hood of its related digit.
The four palmar interossei are anterior to the dorsal interossei, and are unipennate muscles originating from the metacarpals of the digits with which each is associated (Fig. 7.91).
The first palmar interosseous muscle is rudimentary and often considered part of either the adductor pollicis or the flexor pollicis brevis. When present, it originates from the medial side of the palmar surface of metacarpal I and inserts into both the base of the proximal phalanx of the thumb and into the extensor hood. A sesamoid bone often occurs in the tendon attached to the base of the phalanx.
Thenar muscles
The three thenar muscles (the opponens pollicis, flexor pollicis brevis, and abductor pollicis brevis muscles) are associated with opposition of the thumb to the fingers and with delicate movements of the thumb (Table 7.15, Fig. 7.93) and are responsible for the prominent swelling (thenar eminence) on the lateral side of the palm at the base of the thumb.
Hypothenar muscles
The hypothenar muscles (the opponens digiti minimi, abductor digiti minimi, and flexor digiti minimi brevis) contribute to the swelling (hypothenar eminence) on the medial side of the palm at the base of the little finger (Table 7.15, Fig. 7.93). The hypothenar muscles are similar to the thenar muscles in name and in organization.
Lumbrical muscles
There are four lumbrical (worm-like) muscles, each of which is associated with one of the fingers (Fig. 7.94). The muscles originate from the tendons of the flexor digitorum profundus in the palm and insert into the extensor hoods. The lumbricals are unique because they link flexor tendons with extensor tendons. Through their insertion into the extensor hoods, they participate in flexing the metacarpophalangeal joints and extending the interphalangeal joints.
Arteries and veins
The blood supply to the hand is by the radial and ulnar arteries, which form two interconnected vascular arches (superficial and deep) in the palm (Fig. 7.95). Vessels to the digits, muscles, and joints originate from the two arches and the parent arteries:
Fig. 7.95 Arterial supply of the hand.
Ulnar artery and superficial palmar arch
The ulnar artery and ulnar nerve enter the hand on the medial side of the wrist (Figs. 7.95, 7.96). The vessel lies between the palmaris brevis and the flexor retinaculum, and is lateral to the ulnar nerve and the pisiform bone. Distally, the ulnar artery is medial to the hook of the hamate bone and then swings laterally across the palm, forming the superficial palmar arch (Fig. 7.96), which is superficial to the long flexor tendons of the digits and just deep to the palmar aponeurosis. On the lateral side of the palm, the arch communicates with a palmar branch of the radial artery.
Fig. 7.96 Superficial palmar arch.
One branch of the ulnar artery in the hand is the deep palmar branch (Figs. 7.96, 7.97), which arises from the medial aspect of the ulnar artery, just distal to the pisiform, and penetrates the origin of the hypothenar muscles. It curves medially around the hook of the hamate to access the deep plane of the palm and to anastomose with the deep palmar arch derived from the radial artery.
Fig. 7.97 Deep palmar arch.
Branches from the superficial palmar arch include (Fig. 7.96):
 a palmar digital artery to the medial side of the little finger; and
a palmar digital artery to the medial side of the little finger; and
Radial artery and deep palmar arch
The radial artery curves around the lateral side of the wrist, passes over the floor of the anatomical snuffbox and into the deep plane of the palm by penetrating anteriorly through the back of the hand (Fig. 7.95). It passes between the two heads of the first dorsal interosseous muscle and then between the two heads of the adductor pollicis to access the deep plane of the palm and form the deep palmar arch.
The deep palmar arch passes medially through the palm between the metacarpal bones and the long flexor tendons of the digits. On the medial side of the palm, it communicates with the deep palmar branch of the ulnar artery (Fig. 7.97).
Before penetrating the back of the hand, the radial artery gives rise to two vessels (Fig. 7.98):
 the first dorsal metacarpal artery, which supplies adjacent sides of the index finger and thumb.
the first dorsal metacarpal artery, which supplies adjacent sides of the index finger and thumb.
Fig. 7.98 Arteries on the dorsum of hand.
Two vessels, the princeps pollicis artery and the radialis indicis artery, arise from the radial artery in the plane between the first dorsal interosseous and adductor pollicis (Fig. 7.97). The princeps pollicis artery is the major blood supply to the thumb, and the radialis indicis artery supplies the lateral side of the index finger.
The deep palmar arch gives rise to (Fig. 7.97):
Clinical app
Allen’s test
To test for adequate anastomoses between the radial and ulnar arteries, compress both the radial and ulnar arteries at the wrist, then release pressure from one or the other, and determine the filling pattern of the hand. If there is little connection between the deep and superficial palmar arches, only the thumb and lateral side of the index finger will fill with blood (become red) when pressure on the radial artery alone is released.
Veins
As generally found in the upper limb, the hand contains interconnected networks of deep and superficial veins. The deep veins follow the arteries; the superficial veins drain into a dorsal venous network on the back of the hand over the metacarpal bones (Fig. 7.99).
Fig. 7.99 Dorsal venous arch of the hand.
The basilic vein originates from the medial side of the dorsal venous network and passes into the dorsomedial aspect of the forearm.
Nerves
The hand is supplied by the ulnar, median, and radial nerves (Figs. 7.100, 7.102, 7.104). All three nerves contribute to cutaneous or general sensory innervation. The ulnar nerve innervates all intrinsic muscles of the hand except for the three thenar muscles and the two lateral lumbricals, which are innervated by the median nerve. The radial nerve only innervates skin on the dorsolateral side of the hand.
Fig. 7.100 Ulnar nerve in the hand.
Ulnar nerve
The ulnar nerve enters the hand lateral to the pisiform and posteromedially to the ulnar artery (Fig. 7.100). Immediately distal to the pisiform, it divides into a deep branch, which is mainly motor and a superficial branch, which is mainly sensory.
The deep branch of the ulnar nerve passes with the deep branch of the ulnar artery (Fig. 7.100). It penetrates and supplies the hypothenar muscles to reach the deep aspect of the palm, arches laterally across the palm, deep to the long flexors of the digits, and supplies the interossei, adductor pollicis, and the two medial lumbricals. In addition, the deep branch of the ulnar nerve contributes small articular branches to the wrist joint.
As the deep branch of the ulnar nerve passes across the palm, it lies in a fibro-osseous tunnel (Guyon’s canal) between the hook of the hamate and the flexor tendons. Occasionally, small outpouchings of synovial membrane (ganglia) from the joints of the carpus compress the nerve within this canal, producing sensory and motor symptoms.
The superficial branch of the ulnar nerve innervates the palmaris brevis muscle and continues across the palm to supply skin on the palmar surface of the little finger and the medial half of the ring finger (Fig. 7.100).
Clinical app
Ulnar nerve injury
The ulnar nerve is most commonly injured at two sites: the elbow and the wrist.
At the elbow, the nerve lies posterior to the medial epicondyle.
At the wrist, the ulnar nerve passes superficial to the flexor retinaculum and lies lateral to the pisiform bone.
Ulnar nerve lesions are characterized by “clawing” of the hand, in which the metacarpophalangeal joints of the fingers are hyperextended and the interphalangeal joints are flexed because the function of most of the intrinsic muscles of the hand is lost (Fig. 7.101).
Fig. 7.101 Typical appearance of a “clawed hand” due to a lesion of the ulnar nerve.
Clawing is most pronounced in the medial fingers because the function of all intrinsic muscles of these digits is lost while in the lateral two digits, the lumbricals are innervated by the median nerve. Function of the adductor pollicis muscle is also lost.
In lesions of the ulnar nerve at the elbow, function of the flexor carpi ulnaris muscle and flexor digitorum profundus to the medial two digits is lost as well. Clawing of the hand, particularly of the little and ring fingers, is worse with lesions of the ulnar nerve at the wrist than at the elbow because interruption of the nerve at the elbow paralyzes the ulnar half of the flexor digitorum profundus, which leads to lack of flexion at the distal interphalangeal joints in these fingers.
Ulnar nerve lesions at the elbow and wrist result in impaired sensory innervation on the palmar aspect of the medial one and one-half digits.
Damage to the ulnar nerve at the wrist or at a site proximal to the wrist can be distinguished by evaluating the status of function of the dorsal branch (cutaneous) of the ulnar nerve, which originates in distal regions of the forearm. This branch innervates skin over the dorsal surface of the hand on the medial side.
Median nerve
The median nerve is the most important sensory nerve in the hand because it innervates skin on the thumb, index and middle fingers, and lateral side of the ring finger (Fig. 7.102). The nervous system, using touch, gathers information about the environment from this area, particularly from the skin on the thumb and index finger. In addition, sensory information from the lateral three and one-half digits enables the fingers to be positioned with the appropriate amount of force when using precision grip.
Fig. 7.102 Median nerve in the hand.
The median nerve also innervates the thenar muscles that are responsible for opposition of the thumb to the other digits.
The median nerve enters the hand by passing through the carpal tunnel and divides into a recurrent branch and palmar digital branches (Fig. 7.102).
The recurrent branch of the median nerve innervates the three thenar muscles. Originating from the lateral side of the median nerve near the distal margin of the flexor retinaculum, it curves around the margin of the retinaculum and passes proximally over the flexor pollicis brevis muscle. The recurrent branch then passes between the flexor pollicis brevis and abductor pollicis brevis to end in the opponens pollicis.
The palmar digital nerves cross the palm deep to the palmar aponeurosis and the superficial palmar arch and enter the digits. They innervate skin on the palmar surfaces of the lateral three and one-half digits and cutaneous regions over the dorsal aspects of the distal phalanges (nail beds) of the same digits. In addition to skin, the digital nerves supply the lateral two lumbrical muscles.
Surface Anatomy
Motor function of the median and ulnar nerves in the hand
The ability to flex the metacarpophalangeal joints while at the same time extending the interphalangeal joints of the fingers is entirely dependent on the intrinsic muscles of the hand (Fig. 7.103). These muscles are mainly innervated by the deep branch of the ulnar nerve, which carries fibers from spinal cord level (C8)T1.
Adducting the fingers to grasp an object placed between them is caused by the palmar interossei muscles, which are innervated by the deep branch of the ulnar nerve carrying fibers from spinal cord level (C8)T1.
The ability to grasp an object between the pad of the thumb and the pad of one of the fingers depends on normal functioning of the thenar muscles, which are innervated by the recurrent branch of the median nerve carrying fibers from spinal cord level C8(T1).
Superficial branch of the radial nerve
The only part of the radial nerve that enters the hand is the superficial branch (Fig. 7.104). It enters the hand by passing over the anatomical snuffbox on the dorsolateral side of the wrist.
Fig. 7.104 Radial nerve in the hand.
The superficial branch of the radial nerve innervates skin over the dorsolateral aspect of the palm and the dorsal aspects of the lateral three and one-half digits distally to approximately the terminal interphalangeal joints.
Clinical app
Dermatomes and myotomes in the upper limb
Innervation of the upper limb is by the brachial plexus, which is formed by the anterior rami of cervical spinal nerves C5 to C8, and T1. This plexus is initially formed in the neck and then continues into the upper limb. Major nerves that ultimately innervate the arm, forearm, and hand originate from the brachial plexus.
As a consequence of this innervation pattern, clinical testing of lower cervical and T1 nerves is carried out by examining dermatomes, myotomes, and tendon reflexes in the upper limb. Another consequence is that the clinical signs of problems related to lower cervical nerves—pain, pins and needles sensations or paresthesia, and muscle twitching—appear in the upper limb.
Importantly, the major spinal cord level associated with innervation of the diaphragm, C4, is immediately above the spinal cord levels associated with the upper limb. Evaluation of dermatomes and myotomes in the upper limb can provide important information about potential breathing problems that might develop as complications of damage to the spinal cord in regions just below the C4 spinal level.
Dermatomes of the upper limb are shown in Fig. 7.105A Areas where overlap of dermatomes is minimal and can be clinically tested include the:
 upper lateral region of the arm for spinal cord level C5
upper lateral region of the arm for spinal cord level C5
 palmar pad of the thumb for spinal cord level C6
palmar pad of the thumb for spinal cord level C6
 pad of the index finger for spinal cord level C7
pad of the index finger for spinal cord level C7
 pad of the little finger for spinal cord level C8
pad of the little finger for spinal cord level C8
 skin on the medial aspect of the elbow for spinal cord level T1.
skin on the medial aspect of the elbow for spinal cord level T1.
Fig. 7.105 Dermatomes and myotomes in the upper limb. A. Dermatomes. B. Movements produced by myotomes.
Select joint movements are used to test myotomes (Fig. 7.105B):
 Abduction of the arm at the glenohumeral joint is controlled predominantly by C5.
Abduction of the arm at the glenohumeral joint is controlled predominantly by C5.
 Flexion of the forearm at the elbow joint is controlled primarily by C6.
Flexion of the forearm at the elbow joint is controlled primarily by C6.
 Extension of the forearm at the elbow joint is controlled mainly by C7.
Extension of the forearm at the elbow joint is controlled mainly by C7.
 Flexion of the fingers is controlled mainly by C8.
Flexion of the fingers is controlled mainly by C8.
 Abduction and adduction of the index, middle, and ring fingers is controlled predominantly by T1.
Abduction and adduction of the index, middle, and ring fingers is controlled predominantly by T1.
Clinical app
Tendon taps in the upper limb
In an unconscious patient, both somatic sensory and motor functions of spinal cord levels can be tested using tendon reflexes:
 A tap on the tendon of the biceps in the cubital fossa tests mainly for spinal cord level C6.
A tap on the tendon of the biceps in the cubital fossa tests mainly for spinal cord level C6.
 A tap on the tendon of the triceps posterior to the elbow tests mainly for C7.
A tap on the tendon of the triceps posterior to the elbow tests mainly for C7.
Clinical app
Testing sensory innervation carried by major peripheral nerves in the upper limb
In addition to innervating major muscle groups, each of the major peripheral nerves originating from the brachial plexus carries somatic sensory information from patches of skin quite different from dermatomes. Sensation in these areas can be used to test for peripheral nerve lesions:
 The axillary nerve innervates skin on the superior lateral surface on the arm.
The axillary nerve innervates skin on the superior lateral surface on the arm.
 The musculocutaneous nerve innervates skin on the anterolateral side of the forearm.
The musculocutaneous nerve innervates skin on the anterolateral side of the forearm.
 The median nerve innervates the palmar surface of the lateral three and one-half digits.
The median nerve innervates the palmar surface of the lateral three and one-half digits.
 The ulnar nerve innervates the medial one and one-half digits.
The ulnar nerve innervates the medial one and one-half digits.
Fig. 7.106 Anterior and posterior areas of skin innervated by major peripheral nerves in the arm and forearm.
Surface anatomy
Pulse points
Peripheral pulses can be felt at six locations in the upper limb (Fig. 7.107A):
Axillary pulse: axillary artery in the axilla lateral to the apex of the dome of skin covering the floor of the axilla.
Brachial pulse in midarm: brachial artery on the medial side of the arm in the cleft between the biceps brachii and triceps brachii muscles. This is the position where a blood pressure cuff is placed (Fig. 7.107B).
Brachial pulse in the cubital fossa: brachial artery medial to the tendon of the biceps brachii muscle. This is the position where a stethoscope is placed to hear the pulse of the vessel when taking a blood pressure reading (Fig. 7.107B).
Radial pulse in the distal forearm: radial artery immediately lateral to the tendon of the flexor carpi radialis muscle. This is the most common site for “taking a pulse.”
Ulnar pulse in the distal forearm: ulnar artery immediately under the lateral margin of the flexor carpi ulnaris tendon and proximal to the pisiform.
Radial pulse in the anatomical snuffbox: radial artery as it crosses the lateral side of the wrist between the tendon of the extensor pollicis longus muscle and the tendons of the extensor pollicis brevis and abductor pollicis longus muscles.

 PT Case Studies
PT Case Studies Medical Clinical Case Studies
Medical Clinical Case Studies Clinical Cases
Clinical Cases The shoulder is the area of upper limb attachment to the trunk. The bones of the shoulder include the scapula, clavicle, and proximal end of the humerus.
The shoulder is the area of upper limb attachment to the trunk. The bones of the shoulder include the scapula, clavicle, and proximal end of the humerus. The forearm is between the elbow joint and the wrist joint. The bones of the forearm are the ulna and radius.
The forearm is between the elbow joint and the wrist joint. The bones of the forearm are the ulna and radius. The hand is distal to the wrist joint. Bones of the hand are the carpals, metacarpals, and phalanges.
The hand is distal to the wrist joint. Bones of the hand are the carpals, metacarpals, and phalanges.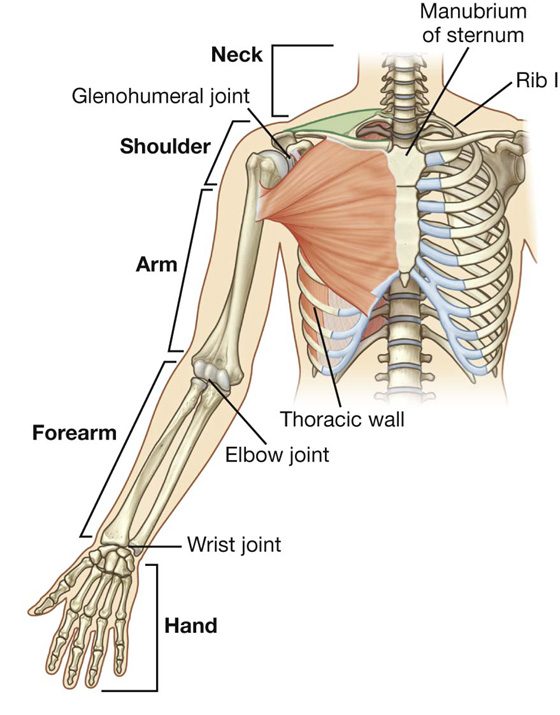
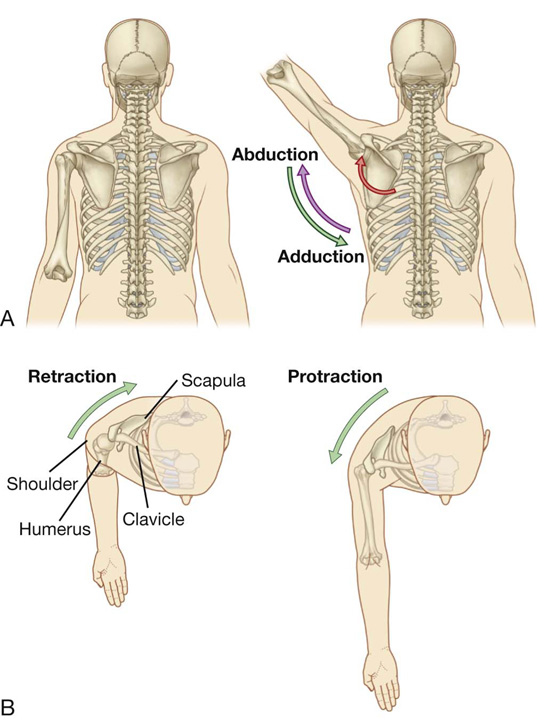
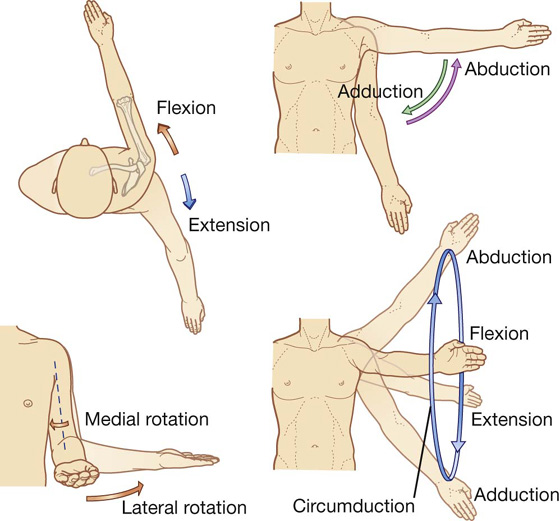
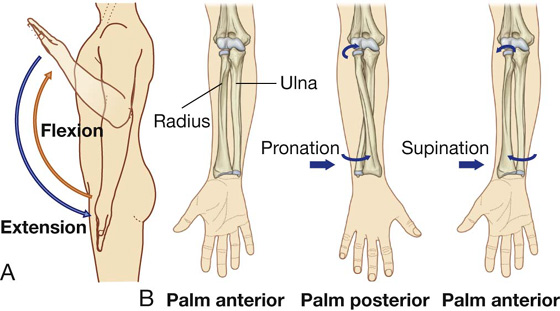
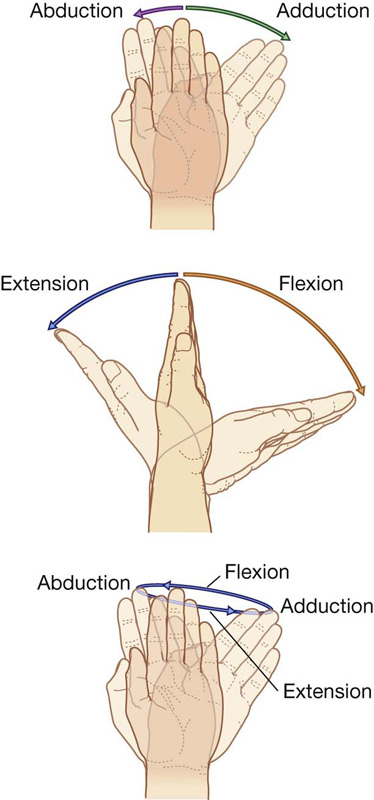
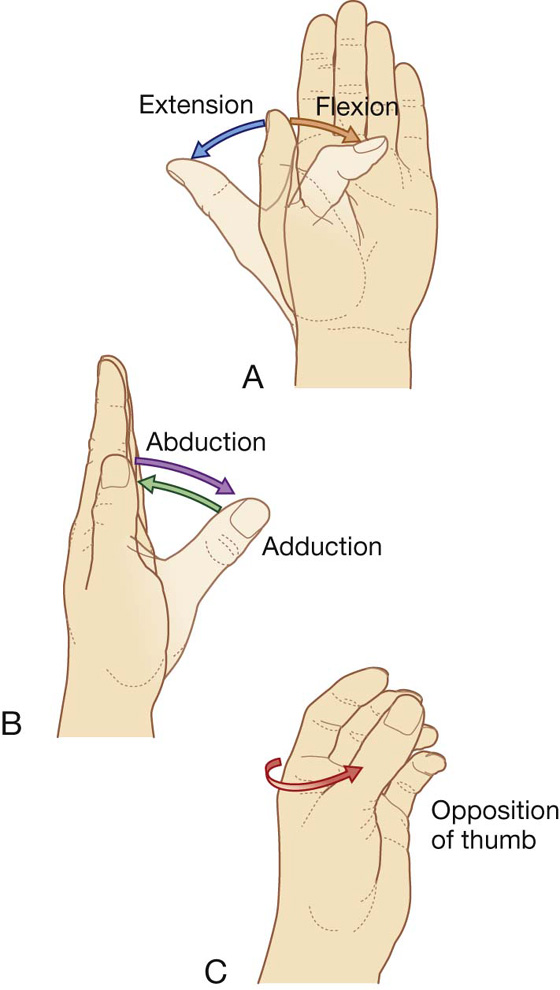
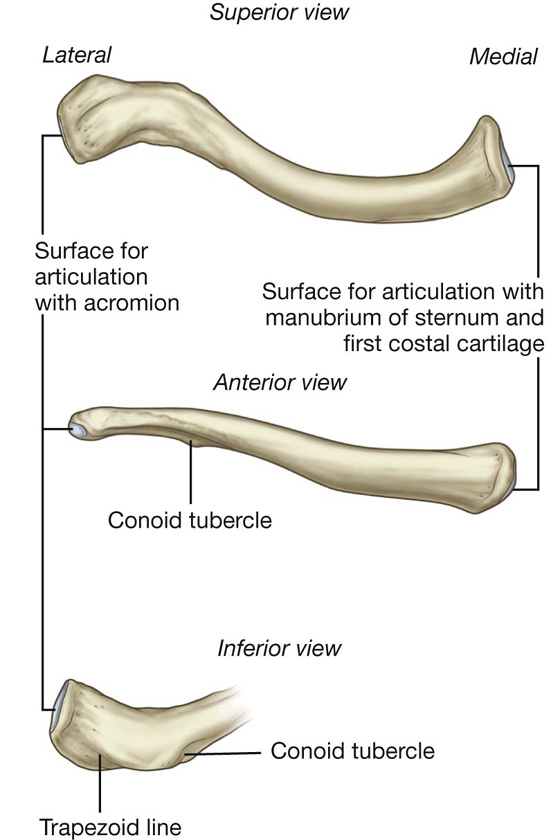
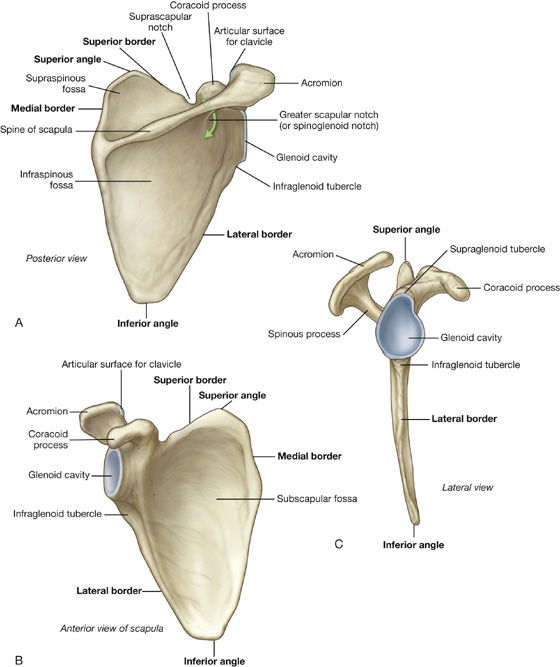
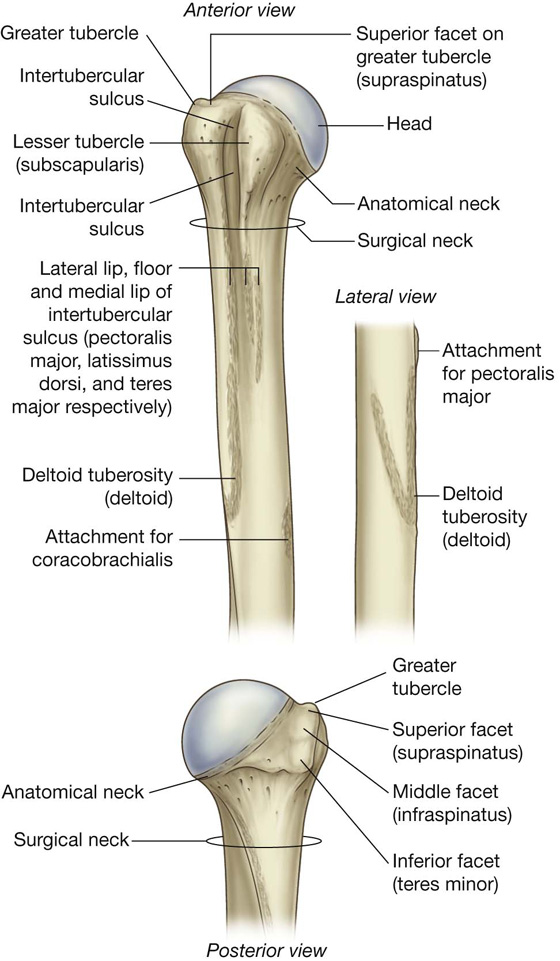
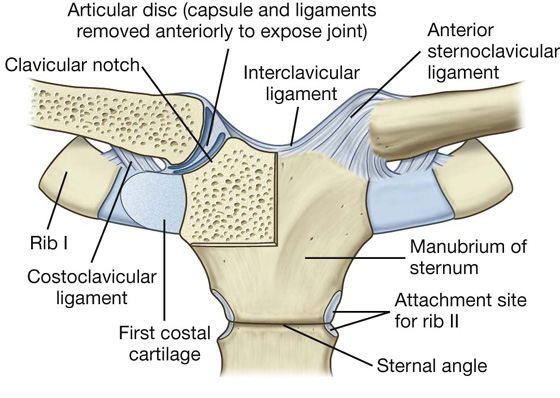
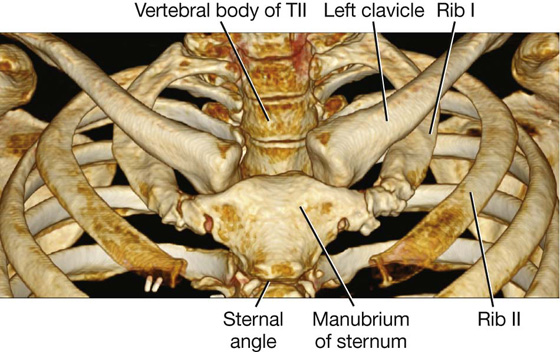
 The anterior and posterior sternoclavicular ligaments are anterior and posterior, respectively, to the joint.
The anterior and posterior sternoclavicular ligaments are anterior and posterior, respectively, to the joint. An interclavicular ligament links the ends of the two clavicles to each other and to the superior surface of the manubrium of sternum.
An interclavicular ligament links the ends of the two clavicles to each other and to the superior surface of the manubrium of sternum. The costoclavicular ligament is positioned laterally to the joint and links the proximal end of the clavicle to the first rib and related costal cartilage.
The costoclavicular ligament is positioned laterally to the joint and links the proximal end of the clavicle to the first rib and related costal cartilage.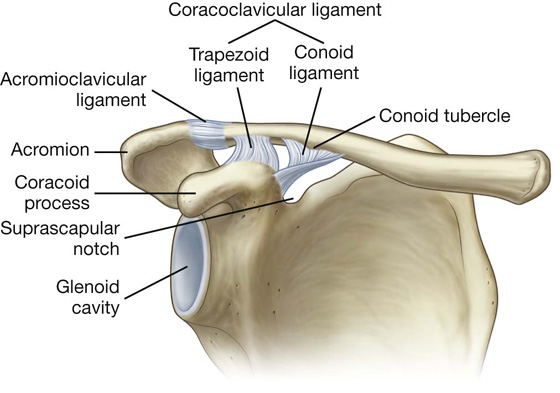
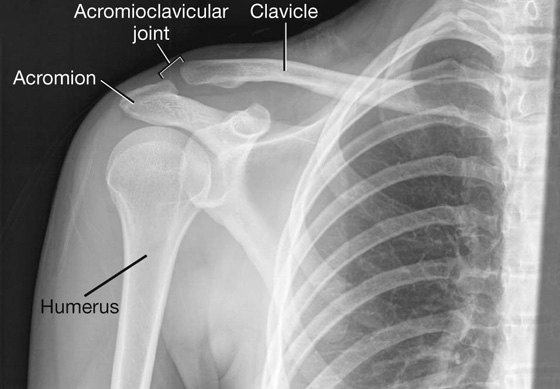
 a small acromioclavicular ligament superior to the joint and passing between adjacent regions of the clavicle and acromion; and
a small acromioclavicular ligament superior to the joint and passing between adjacent regions of the clavicle and acromion; and a much larger coracoclavicular ligament, which is not directly related to the joint, but is an important strong accessory ligament, providing much of the weight-bearing support for the upper limb on the clavicle and maintaining the position of the clavicle on the acromion. It spans the distance between the coracoid process of the scapula and the inferior surface of the acromial end of the clavicle and comprises an anterior trapezoid ligament (which attaches to the trapezoid line on the clavicle) and a posterior conoid ligament (which attaches to the related conoid tubercle).
a much larger coracoclavicular ligament, which is not directly related to the joint, but is an important strong accessory ligament, providing much of the weight-bearing support for the upper limb on the clavicle and maintaining the position of the clavicle on the acromion. It spans the distance between the coracoid process of the scapula and the inferior surface of the acromial end of the clavicle and comprises an anterior trapezoid ligament (which attaches to the trapezoid line on the clavicle) and a posterior conoid ligament (which attaches to the related conoid tubercle).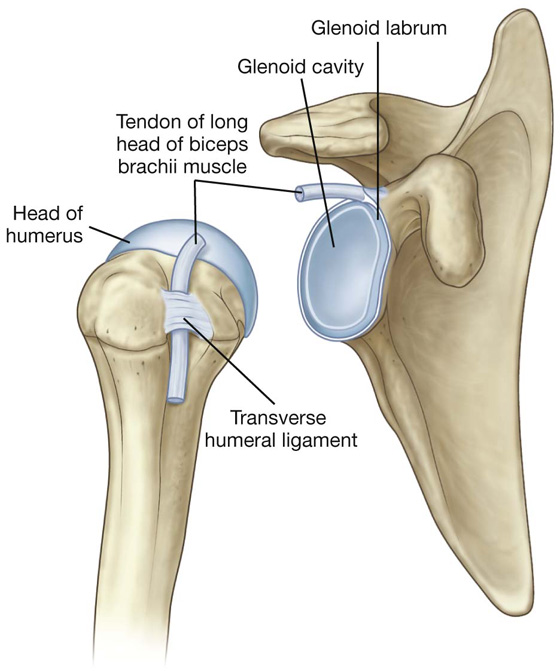
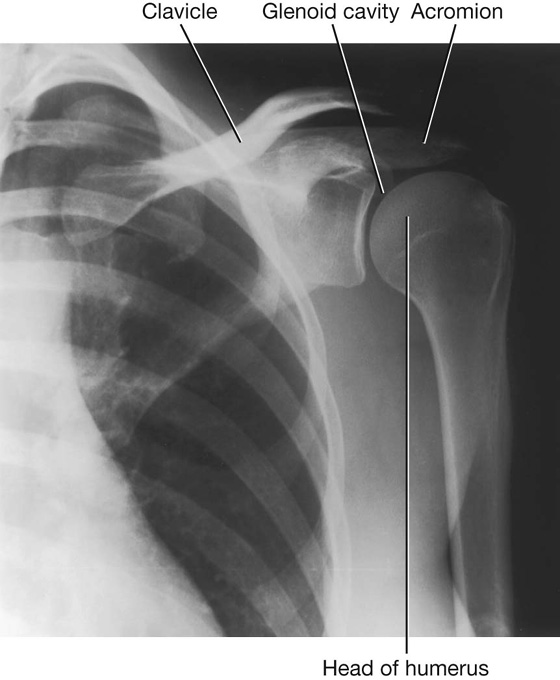
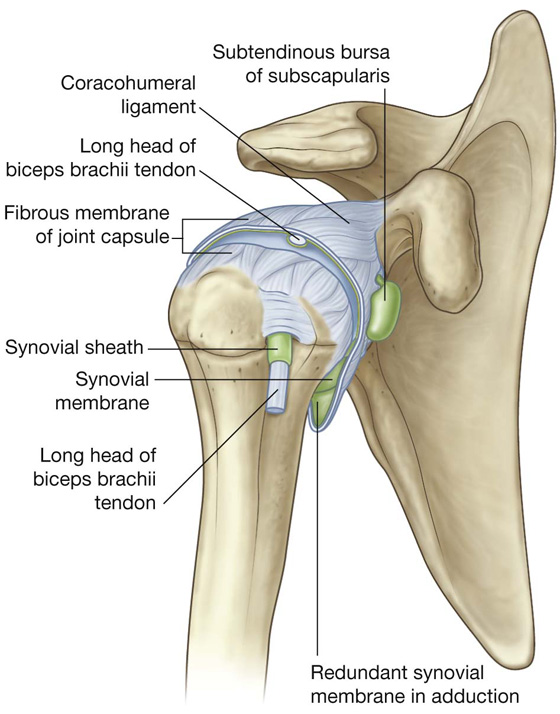
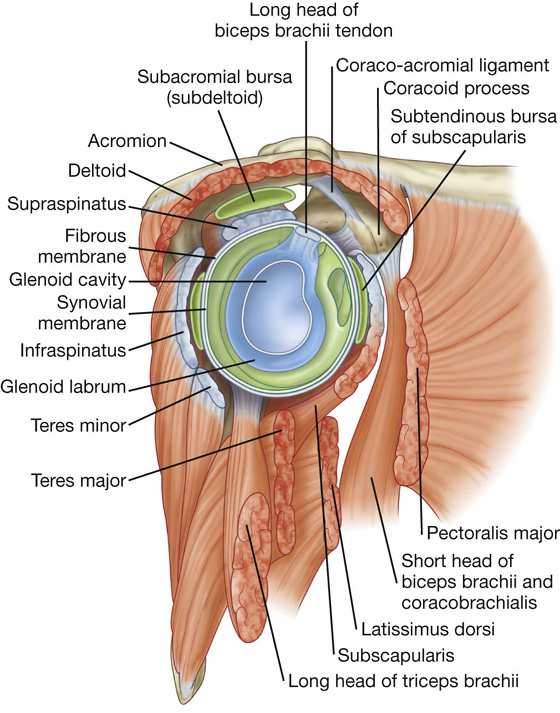
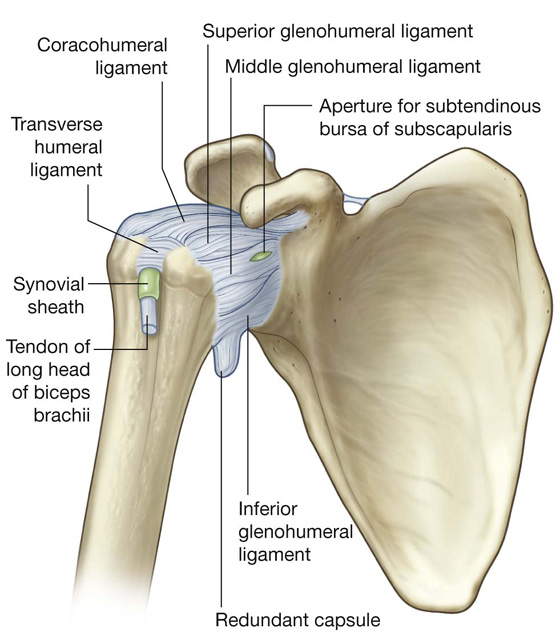
 in relationship to tendons of muscles around the joint (coracobrachialis, teres major, long head of triceps brachii, and latissimus dorsi muscles).
in relationship to tendons of muscles around the joint (coracobrachialis, teres major, long head of triceps brachii, and latissimus dorsi muscles). anterosuperiorly in three locations to form superior, middle, and inferior glenohumeral ligaments, which pass from the superomedial margin of the glenoid cavity to the lesser tubercle and inferiorly related anatomical neck of the humerus;
anterosuperiorly in three locations to form superior, middle, and inferior glenohumeral ligaments, which pass from the superomedial margin of the glenoid cavity to the lesser tubercle and inferiorly related anatomical neck of the humerus; superiorly between the base of the coracoid process and the greater tubercle of the humerus (the coracohumeral ligament;
superiorly between the base of the coracoid process and the greater tubercle of the humerus (the coracohumeral ligament; between the greater and lesser tubercles of the humerus (transverse humeral ligament)—this holds the tendon of the long head of the biceps brachii muscle in the intertubercular sulcus.
between the greater and lesser tubercles of the humerus (transverse humeral ligament)—this holds the tendon of the long head of the biceps brachii muscle in the intertubercular sulcus.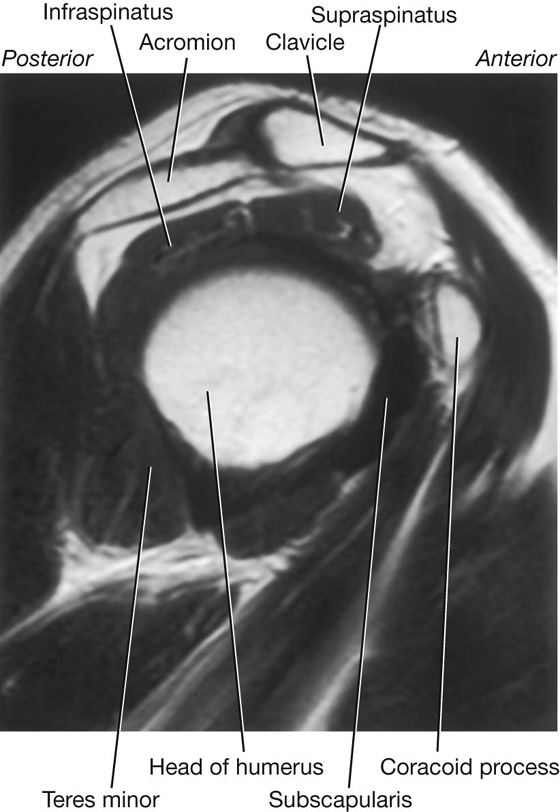
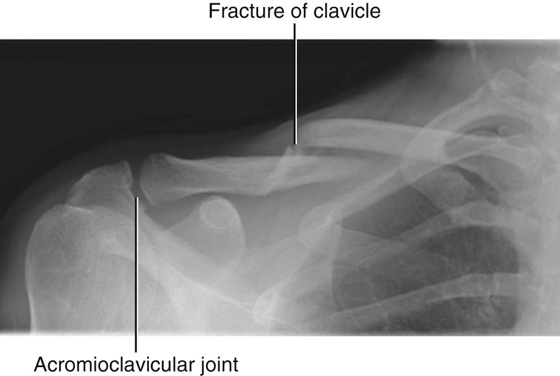
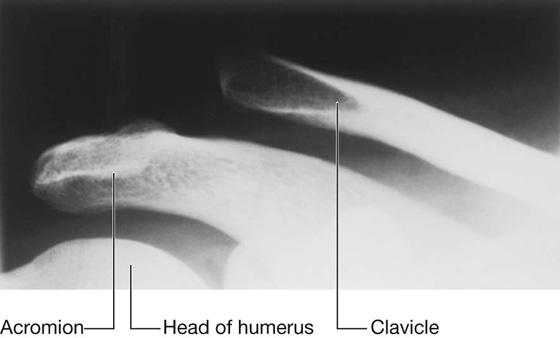
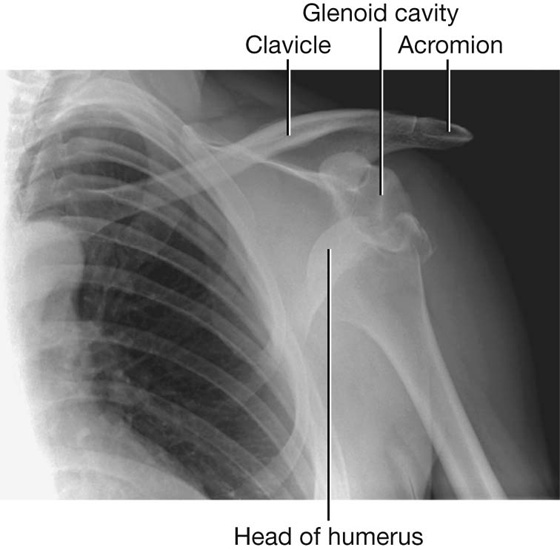
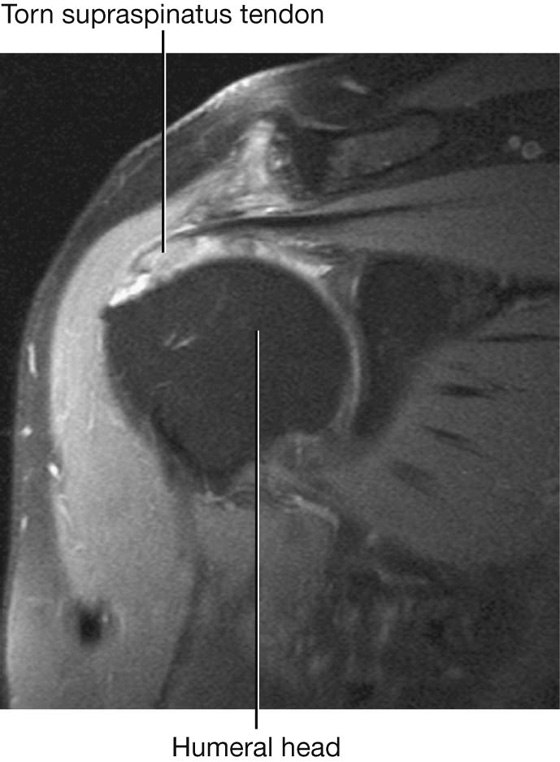
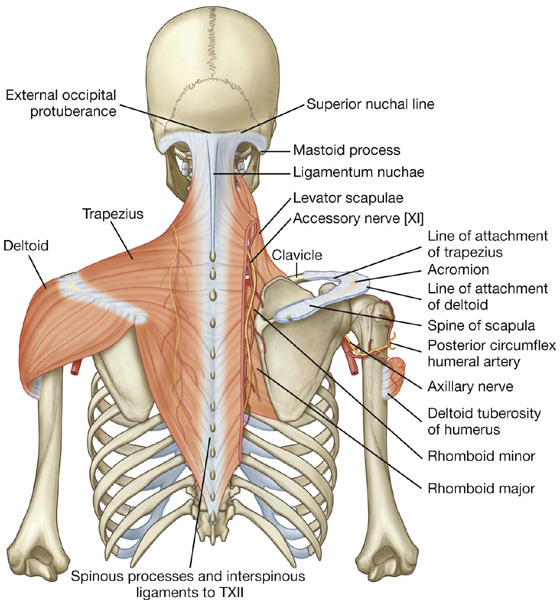
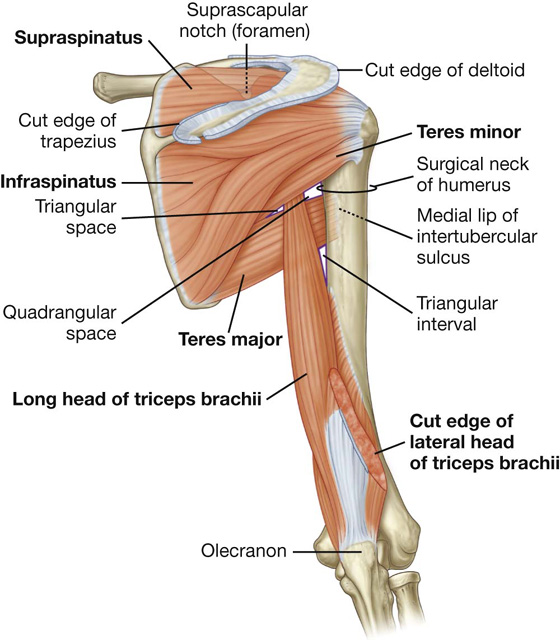
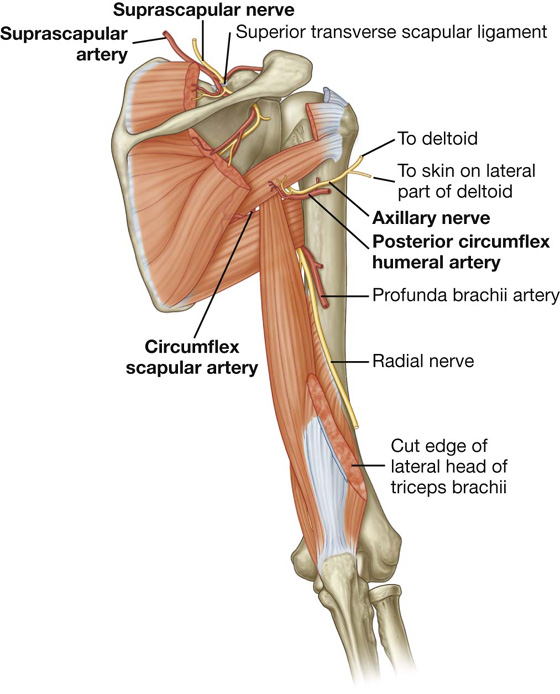
 the shaft of the humerus, and
the shaft of the humerus, and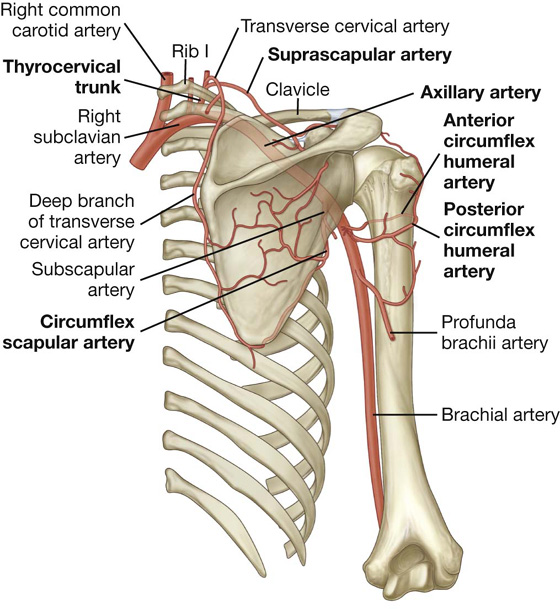
 four sides,
four sides, an inlet, and
an inlet, and a floor (base).
a floor (base).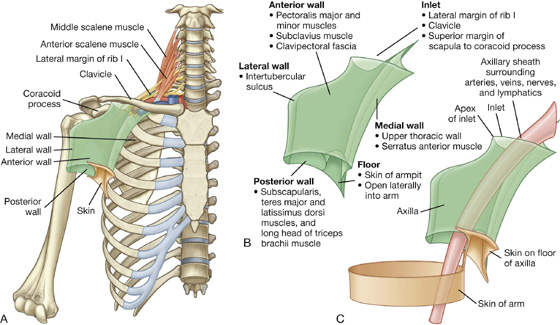
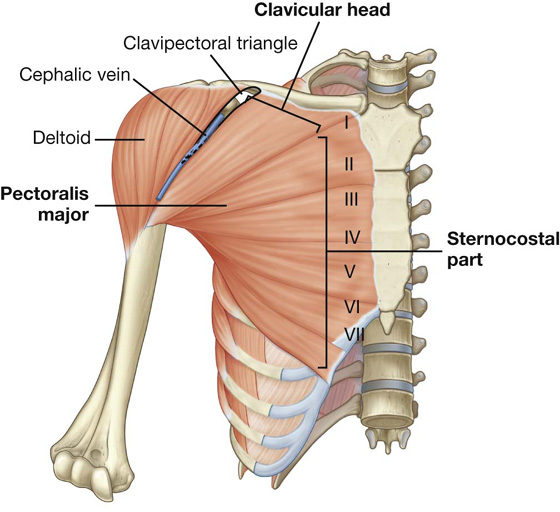
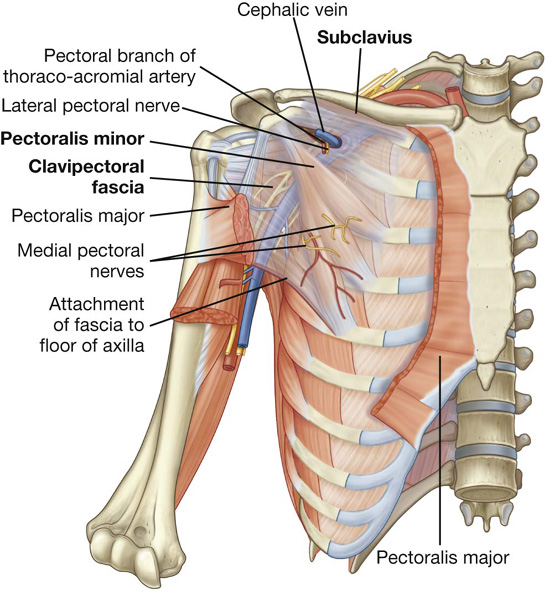
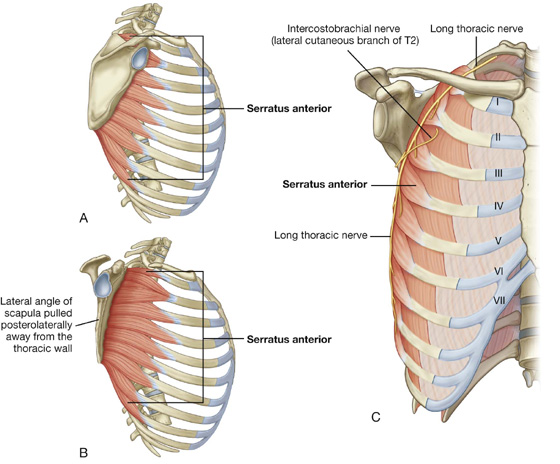
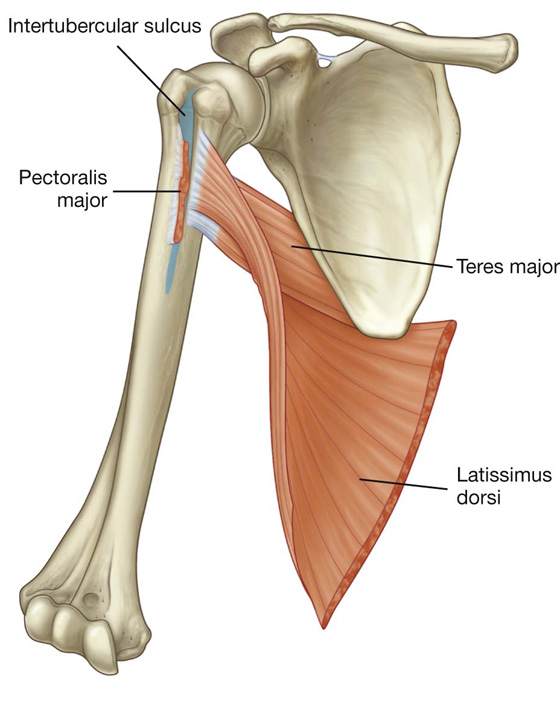
 the distal parts of the latissimus dorsi and teres major muscles (which pass into the wall from the back and posterior scapular region), and
the distal parts of the latissimus dorsi and teres major muscles (which pass into the wall from the back and posterior scapular region), and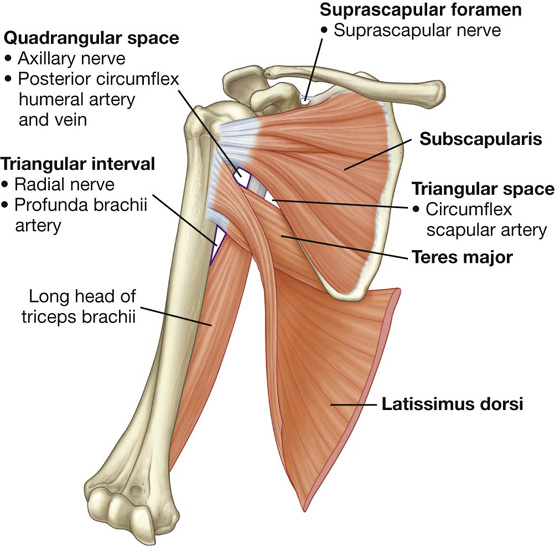
 the quadrangular space,
the quadrangular space, the triangular space, and
the triangular space, and the triangular interval.
the triangular interval. the shaft of the humerus, and
the shaft of the humerus, and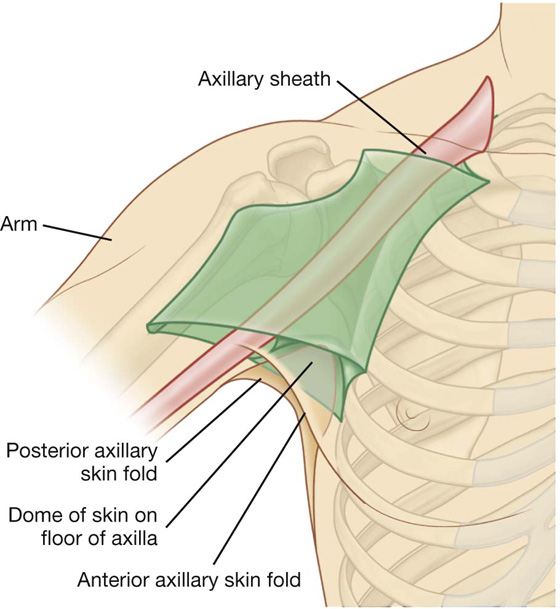
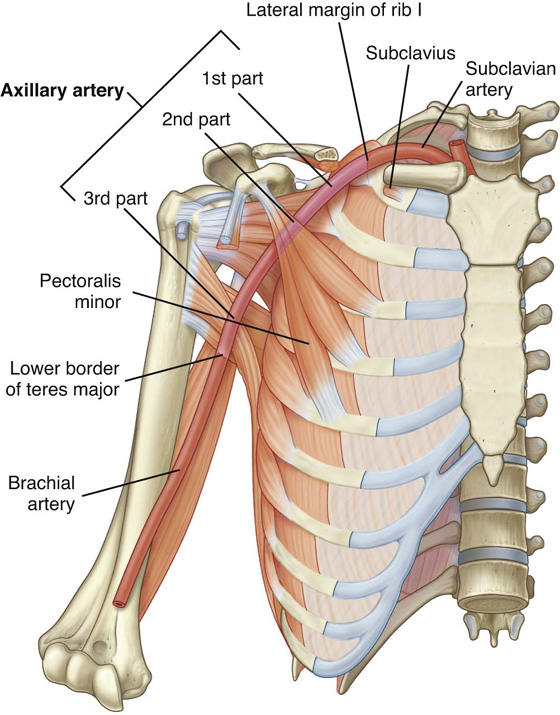
 Two branches, the thoracoacromial artery and the lateral thoracic artery, originate from the second part.
Two branches, the thoracoacromial artery and the lateral thoracic artery, originate from the second part. Three branches, the subscapular artery, the anterior circumflex humeral artery, and the posterior circumflex humeral artery, originate from the third part.
Three branches, the subscapular artery, the anterior circumflex humeral artery, and the posterior circumflex humeral artery, originate from the third part.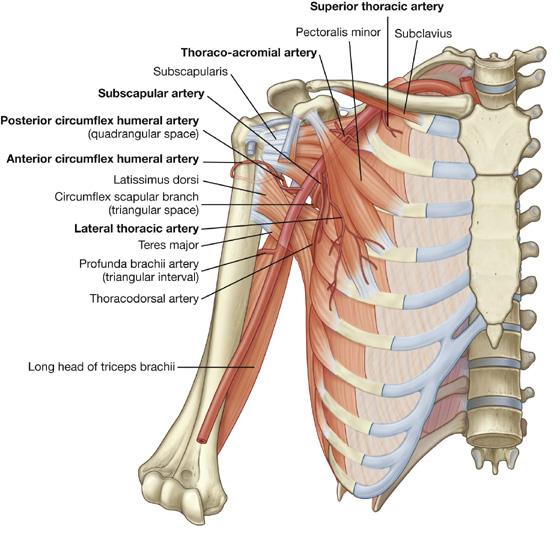
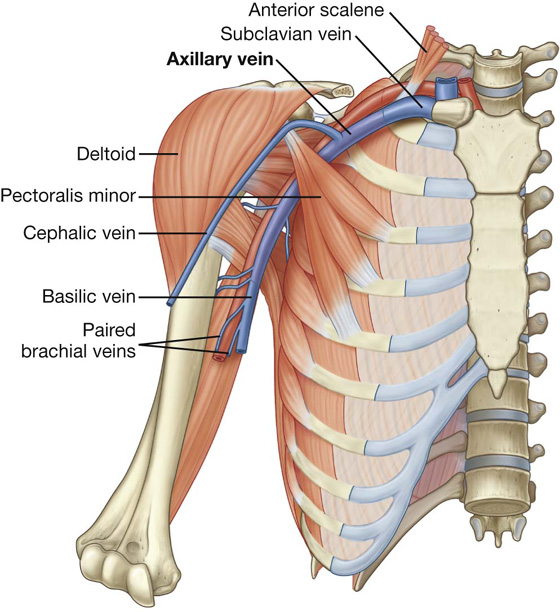
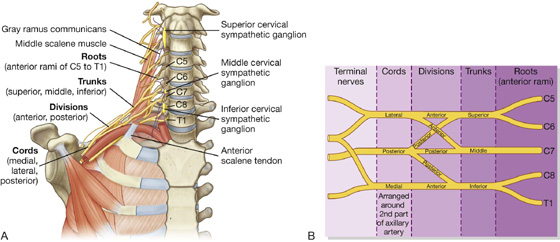
 The three anterior divisions form parts of the brachial plexus that ultimately give rise to peripheral nerves associated with the anterior compartments of the arm and forearm.
The three anterior divisions form parts of the brachial plexus that ultimately give rise to peripheral nerves associated with the anterior compartments of the arm and forearm. The three posterior divisions combine to form parts of the brachial plexus that give rise to nerves associated with the posterior compartments.
The three posterior divisions combine to form parts of the brachial plexus that give rise to nerves associated with the posterior compartments. The lateral cord results from the union of the anterior divisions of the upper and middle trunks and therefore has contributions from C5 to C7; it is positioned lateral to the second part of the axillary artery;
The lateral cord results from the union of the anterior divisions of the upper and middle trunks and therefore has contributions from C5 to C7; it is positioned lateral to the second part of the axillary artery; The medial cord is medial to the second part of the axillary artery and is the continuation of the anterior division of the inferior trunk; it contains contributions from C8 and T1.
The medial cord is medial to the second part of the axillary artery and is the continuation of the anterior division of the inferior trunk; it contains contributions from C8 and T1. The posterior cord occurs posterior to the second part of the axillary artery and originates as the union of all three posterior divisions; it contains contributions from all roots of the brachial plexus (C5 to T1).
The posterior cord occurs posterior to the second part of the axillary artery and originates as the union of all three posterior divisions; it contains contributions from all roots of the brachial plexus (C5 to T1).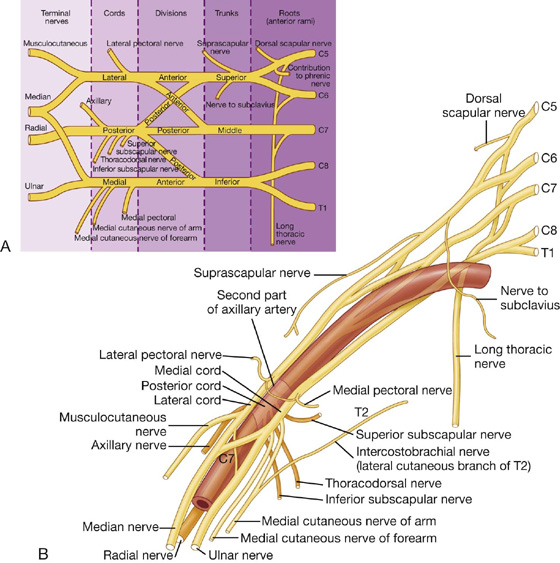
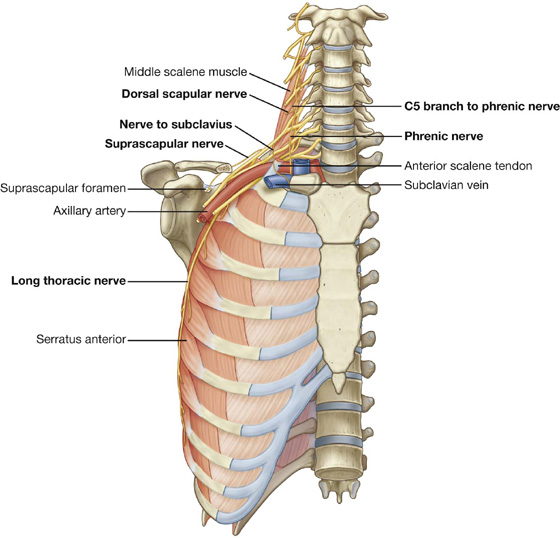
 passes posteriorly, often piercing the middle scalene muscle in the neck, to reach and travel along the medial border of the scapula, and
passes posteriorly, often piercing the middle scalene muscle in the neck, to reach and travel along the medial border of the scapula, and passes vertically down the neck, through the axillary inlet, and down the medial wall of the axilla to supply the serratus anterior muscle, and
passes vertically down the neck, through the axillary inlet, and down the medial wall of the axilla to supply the serratus anterior muscle, and passes laterally through the posterior triangle of the neck and through the suprascapular foramen to enter the posterior scapular region.
passes laterally through the posterior triangle of the neck and through the suprascapular foramen to enter the posterior scapular region. is accompanied in the lateral parts of the neck and in the posterior scapular region by the suprascapular artery.
is accompanied in the lateral parts of the neck and in the posterior scapular region by the suprascapular artery.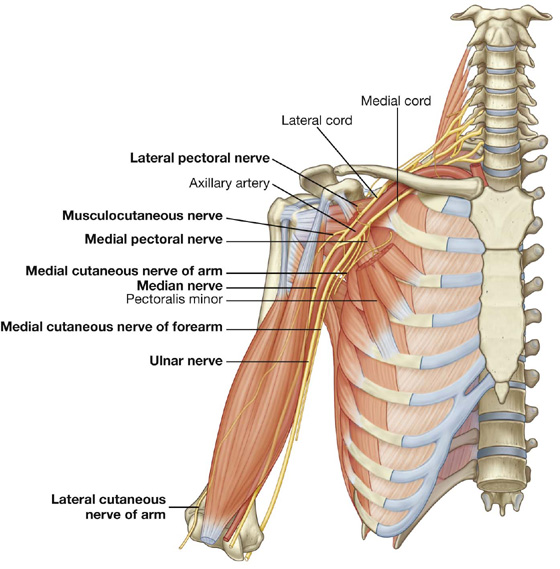
 the skin over the palmar surface of the lateral three and one-half digits and over the lateral side of the palm and middle of the wrist.
the skin over the palmar surface of the lateral three and one-half digits and over the lateral side of the palm and middle of the wrist. the thoracodorsal nerve,
the thoracodorsal nerve, the axillary nerve,
the axillary nerve, the radial nerve.
the radial nerve.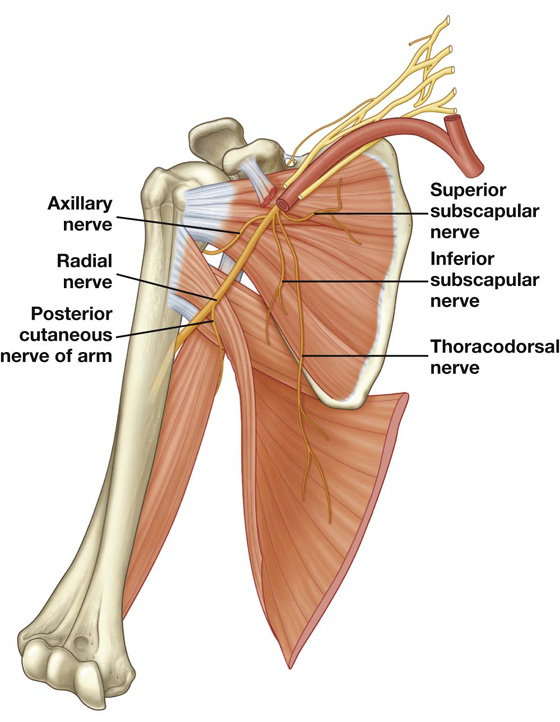
 the skin on the posterior aspect of the arm and forearm, the lower lateral surface of the arm, and the dorsolateral surface of the hand.
the skin on the posterior aspect of the arm and forearm, the lower lateral surface of the arm, and the dorsolateral surface of the hand.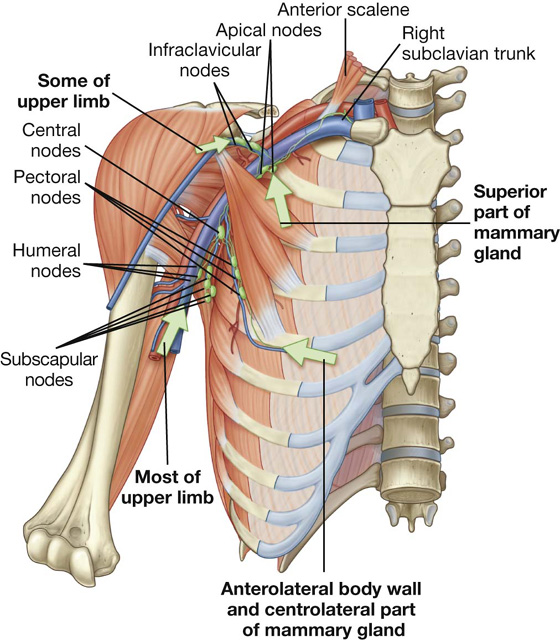
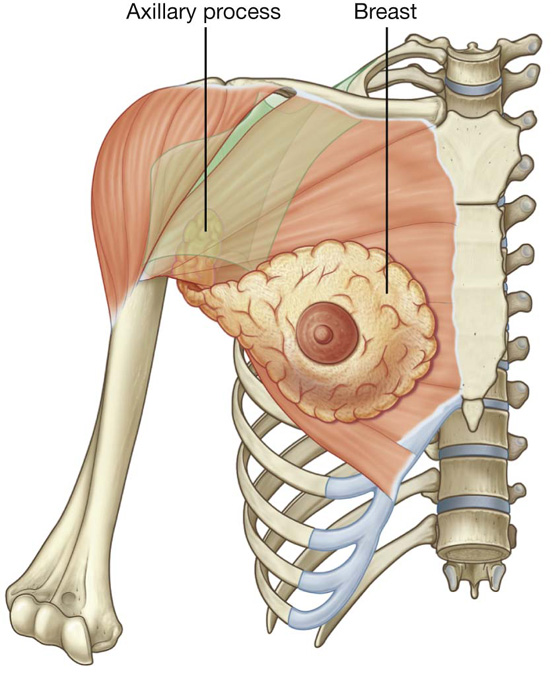
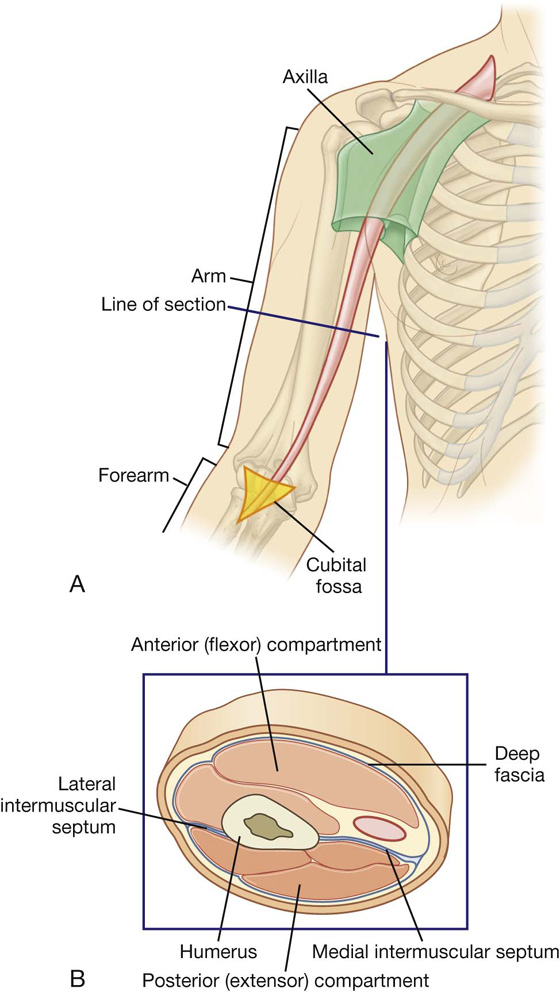
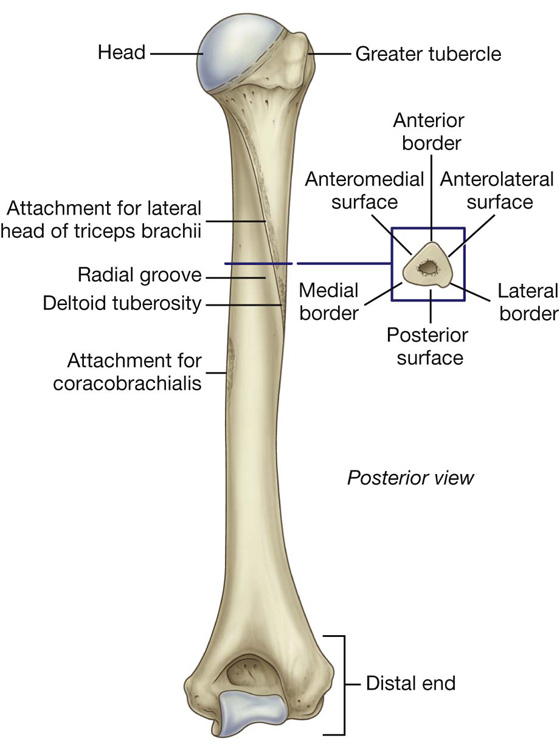
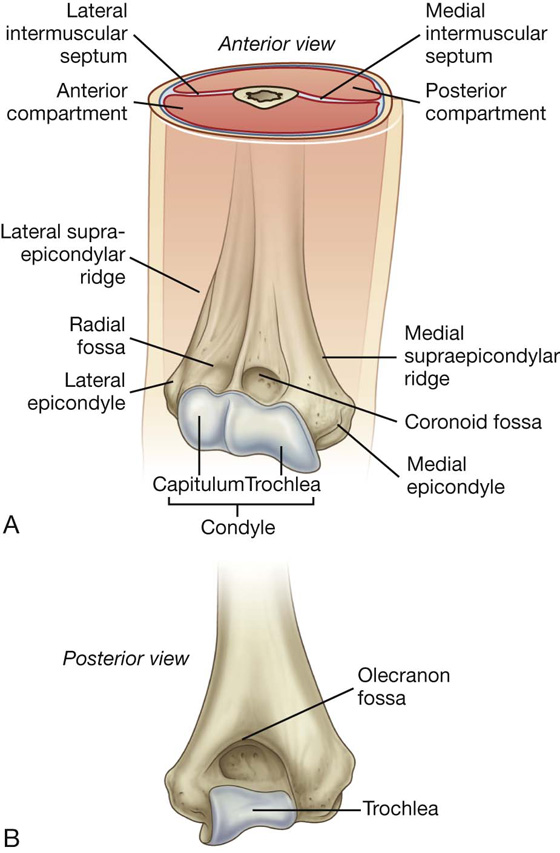
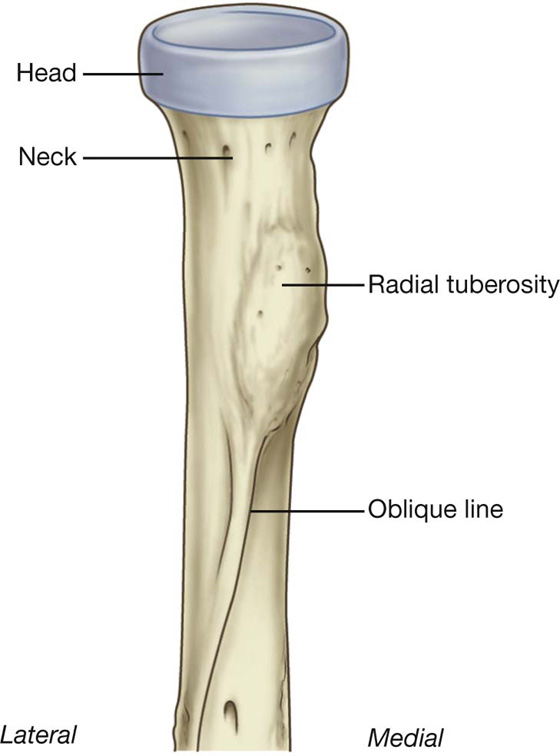
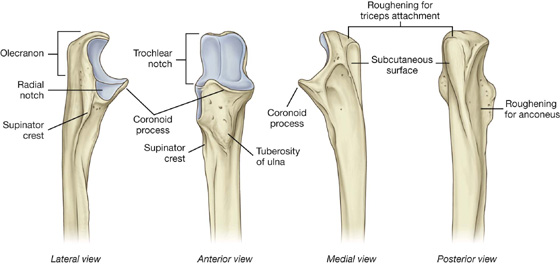
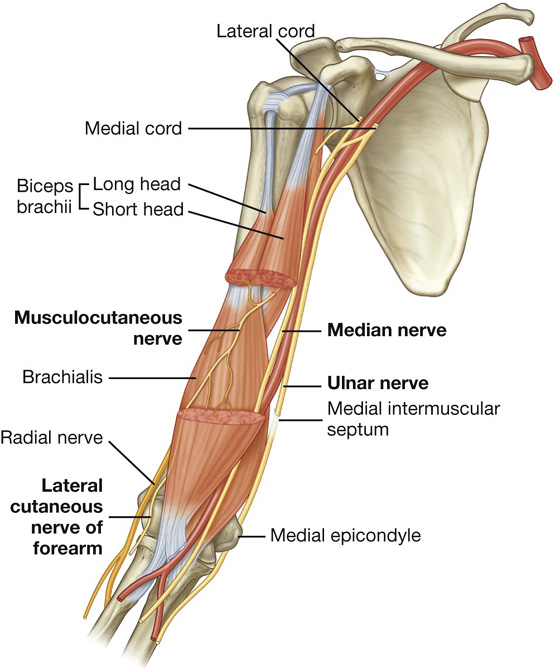
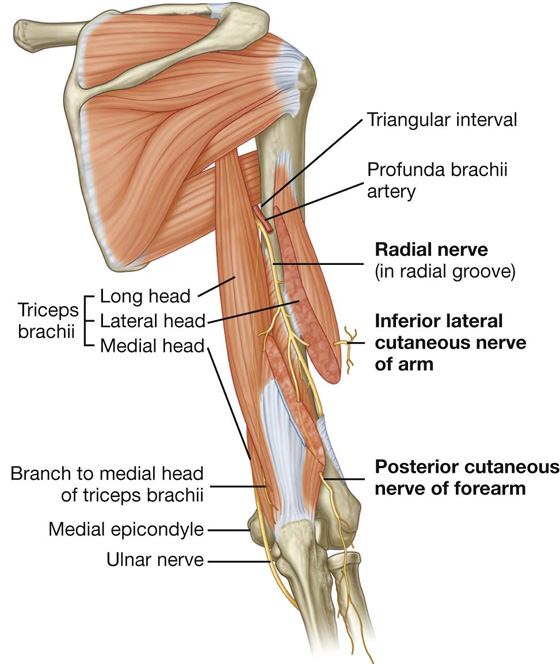
 In more distal regions, the median nerve crosses to the medial side of the brachial artery and lies anterior to the elbow joint.
In more distal regions, the median nerve crosses to the medial side of the brachial artery and lies anterior to the elbow joint.
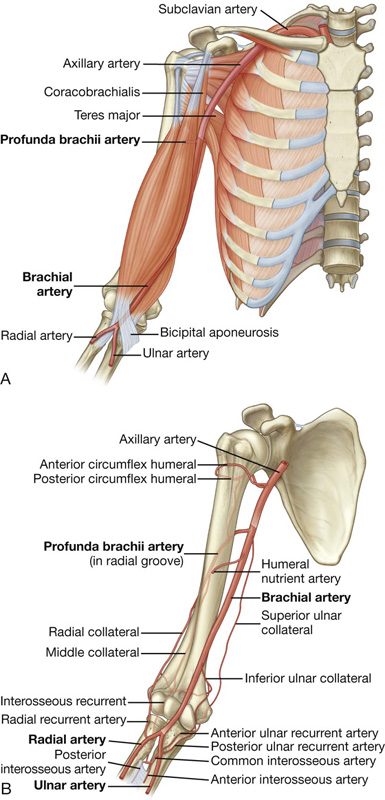
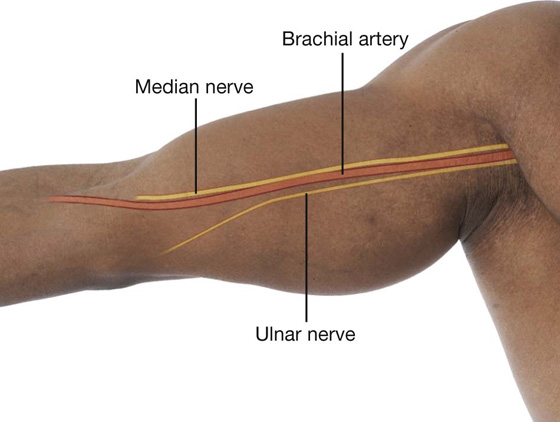
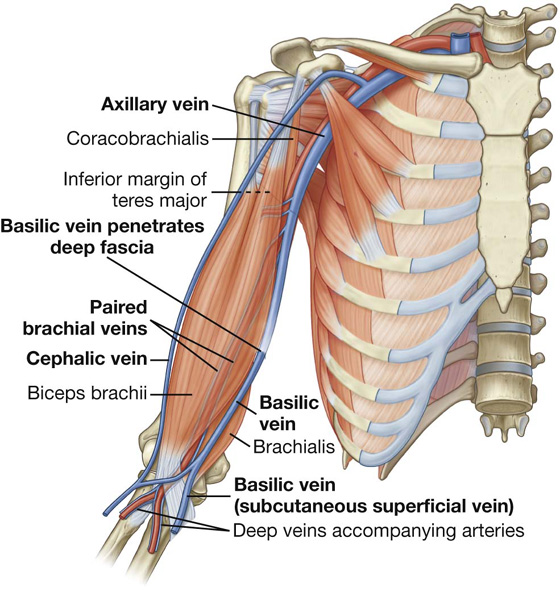
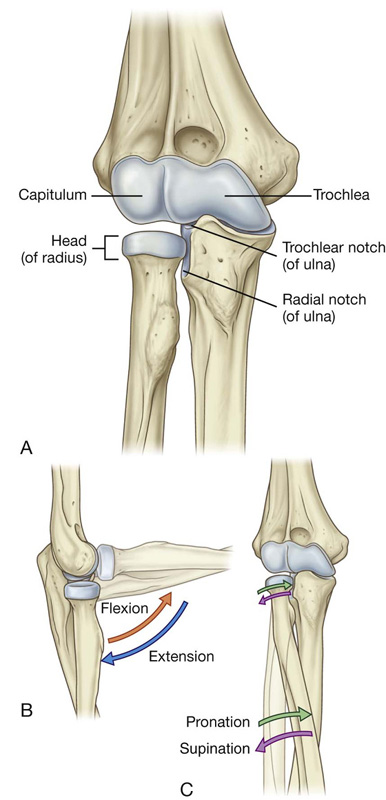
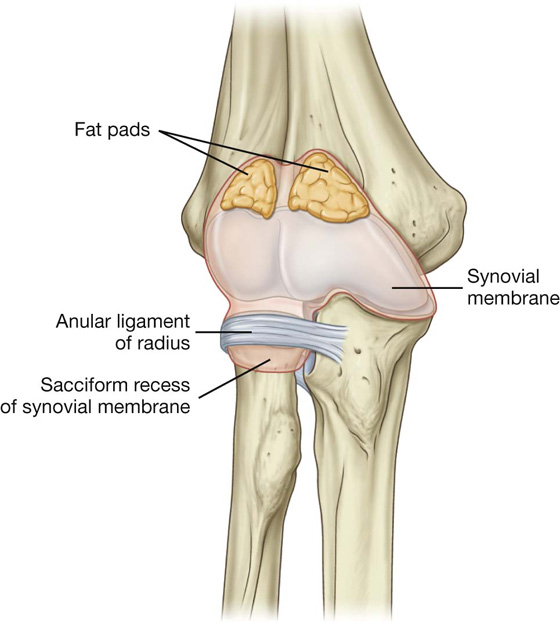
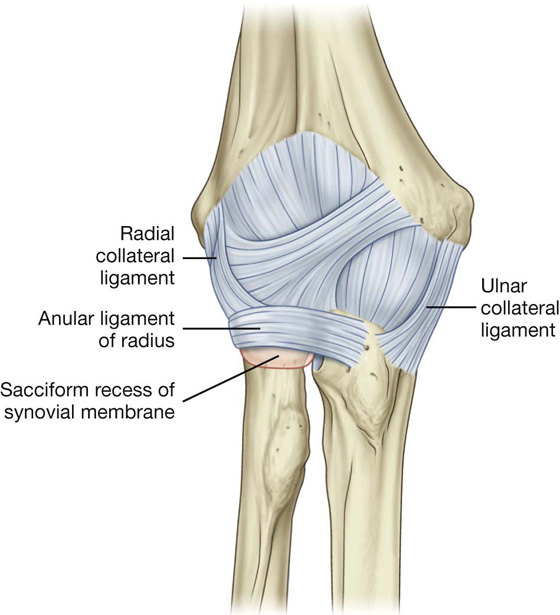
 capitulum—1 year
capitulum—1 year head (of radius)—5 years
head (of radius)—5 years medial epicondyle—5 years
medial epicondyle—5 years trochlea—11 years
trochlea—11 years olecranon—12 years
olecranon—12 years lateral epicondyle—13 years.
lateral epicondyle—13 years.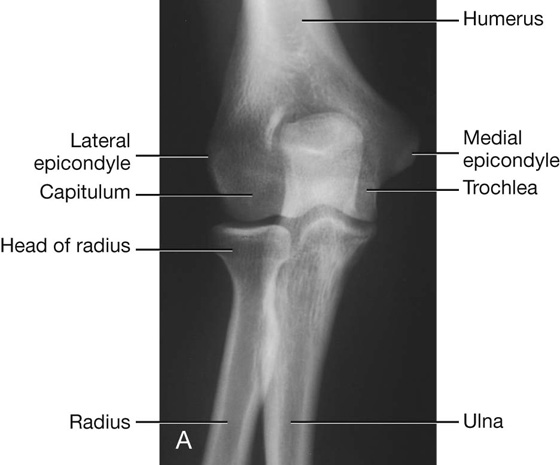
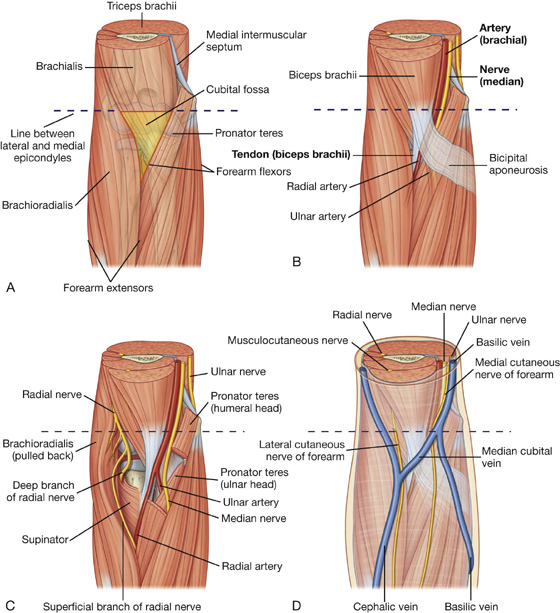
 the brachial artery, and
the brachial artery, and the median nerve
the median nerve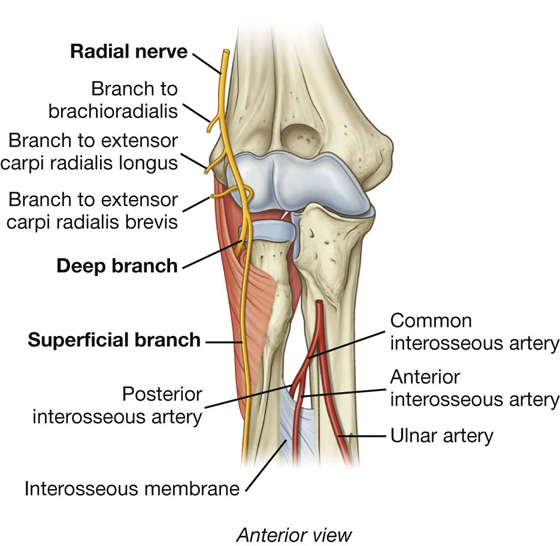
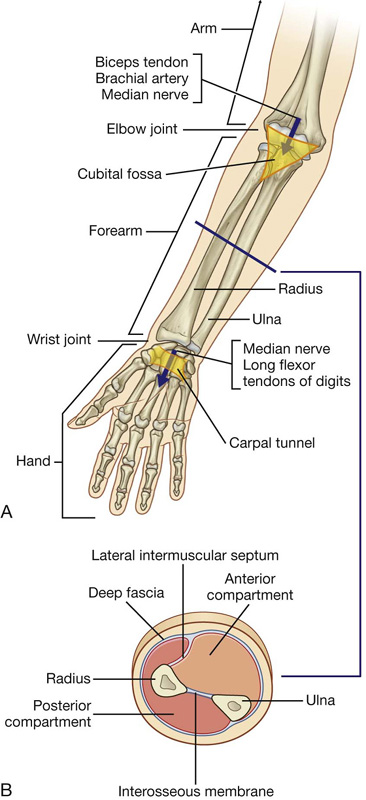
 a lateral intermuscular septum, which passes from the anterior border of the radius to deep fascia surrounding the limb;
a lateral intermuscular septum, which passes from the anterior border of the radius to deep fascia surrounding the limb; an interosseous membrane, which links adjacent borders of the radius and ulna along most of their length; and
an interosseous membrane, which links adjacent borders of the radius and ulna along most of their length; and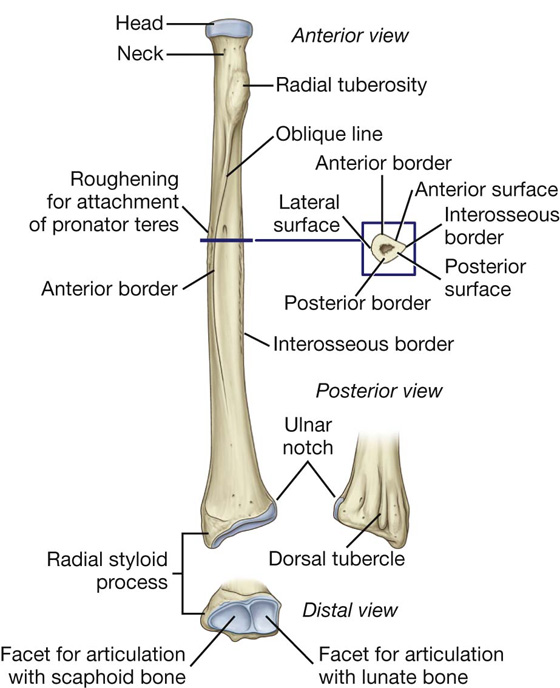

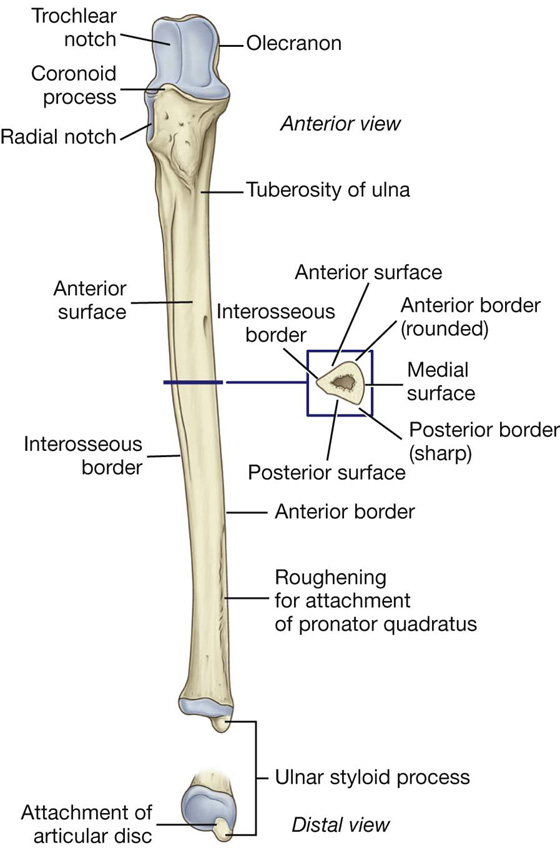
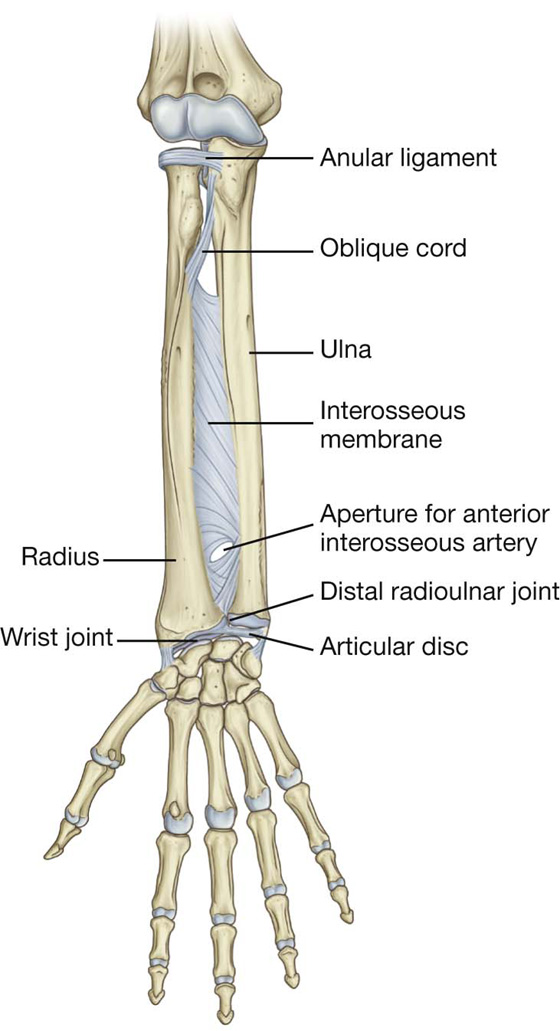
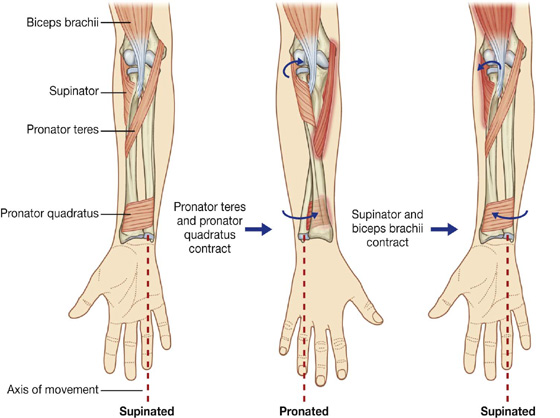
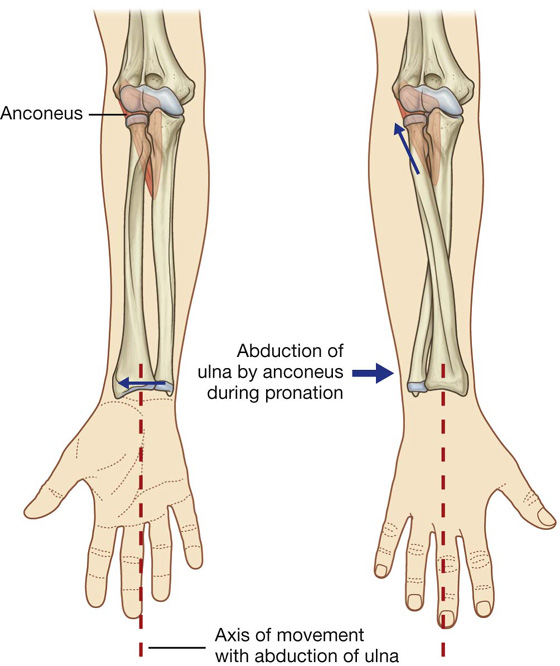
 movements of the wrist joint,
movements of the wrist joint, pronation.
pronation.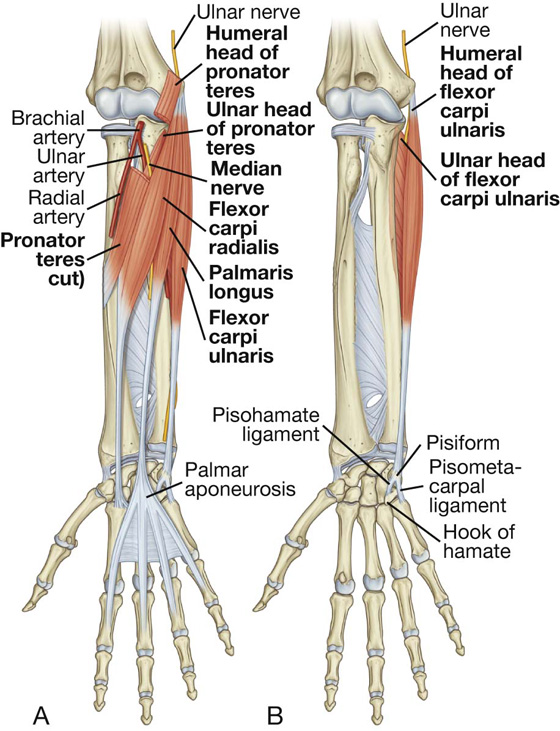
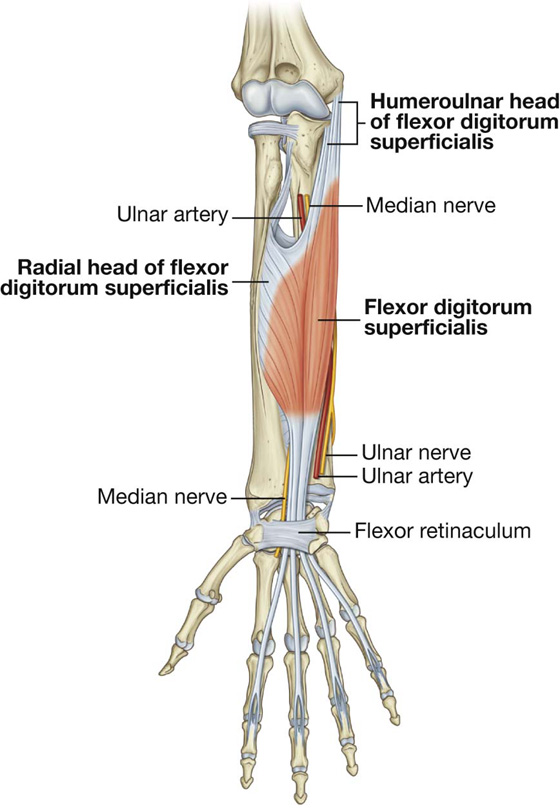
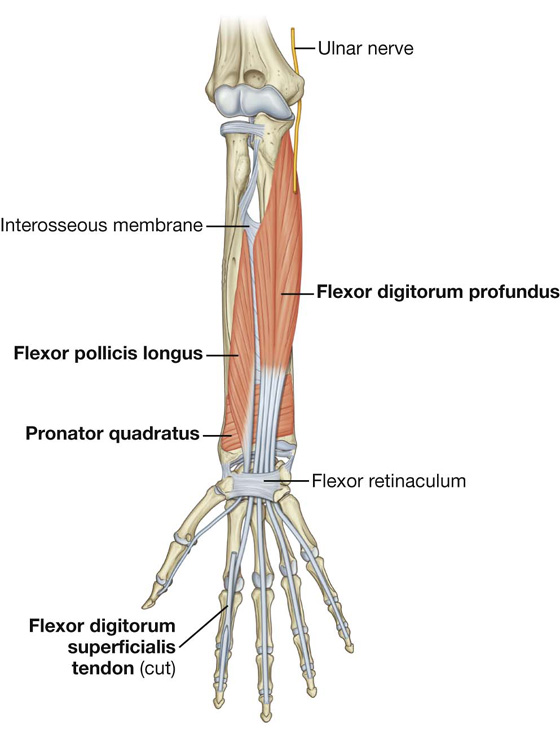
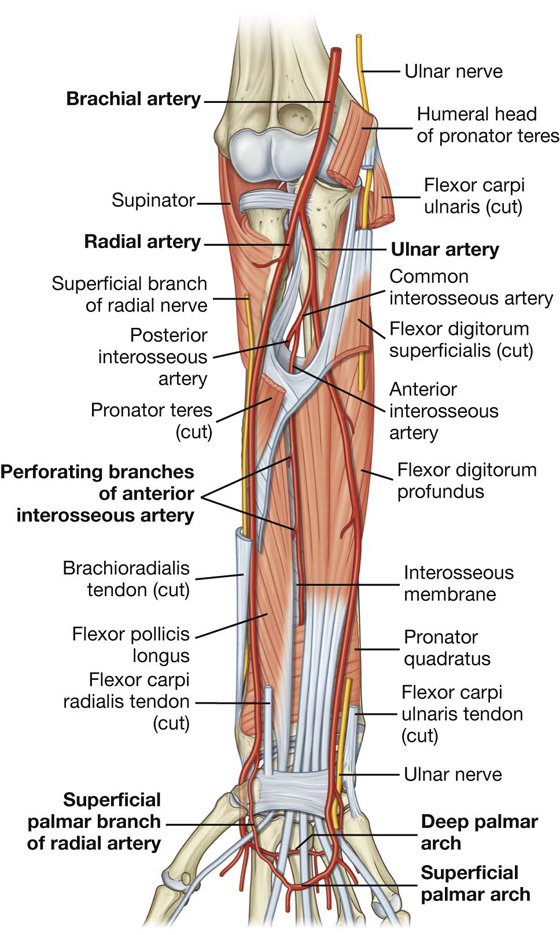
 related on its lateral side to the superficial branch of the radial nerve in the middle third of the forearm;
related on its lateral side to the superficial branch of the radial nerve in the middle third of the forearm; medial to the tendon of the brachioradialis muscle and covered only by deep fascia, superficial fascia, and skin in the distal forearm.
medial to the tendon of the brachioradialis muscle and covered only by deep fascia, superficial fascia, and skin in the distal forearm. a small palmar carpal branch, which contributes to an anastomotic network of vessels that supply the carpal bones and joints;
a small palmar carpal branch, which contributes to an anastomotic network of vessels that supply the carpal bones and joints; the ulnar recurrent artery with anterior and posterior branches, which contribute to an anastomotic network of vessels around the elbow joint;
the ulnar recurrent artery with anterior and posterior branches, which contribute to an anastomotic network of vessels around the elbow joint;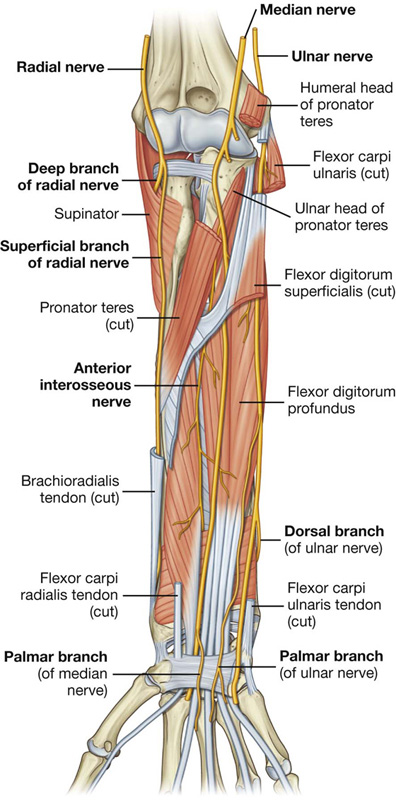
 muscular branches to the flexor carpi ulnaris and to the medial half of the flexor digitorum profundus that arise soon after the ulnar nerve enters the forearm; and
muscular branches to the flexor carpi ulnaris and to the medial half of the flexor digitorum profundus that arise soon after the ulnar nerve enters the forearm; and movement of the wrist joint,
movement of the wrist joint, supination.
supination.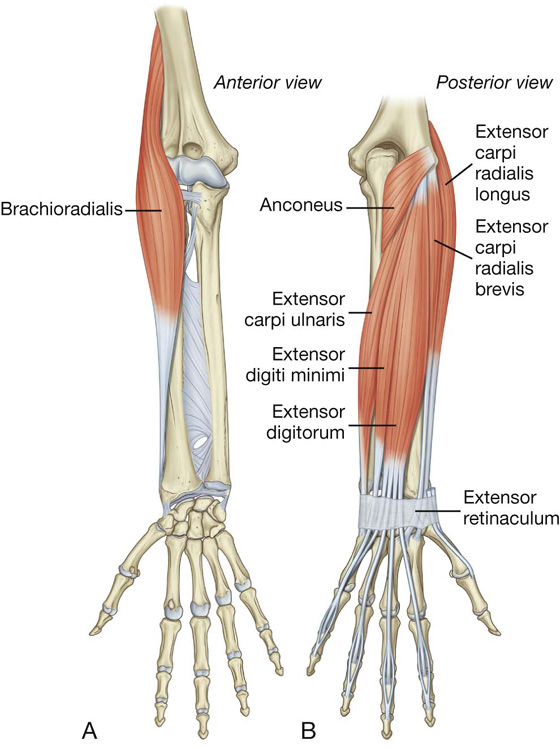
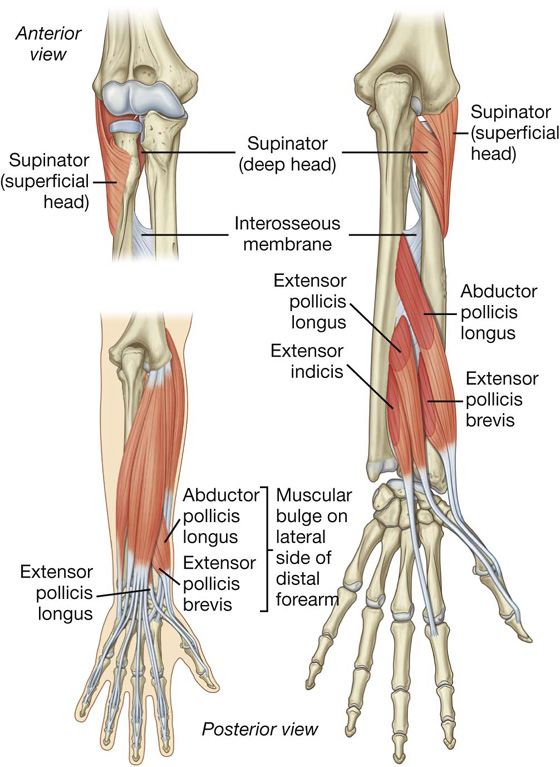
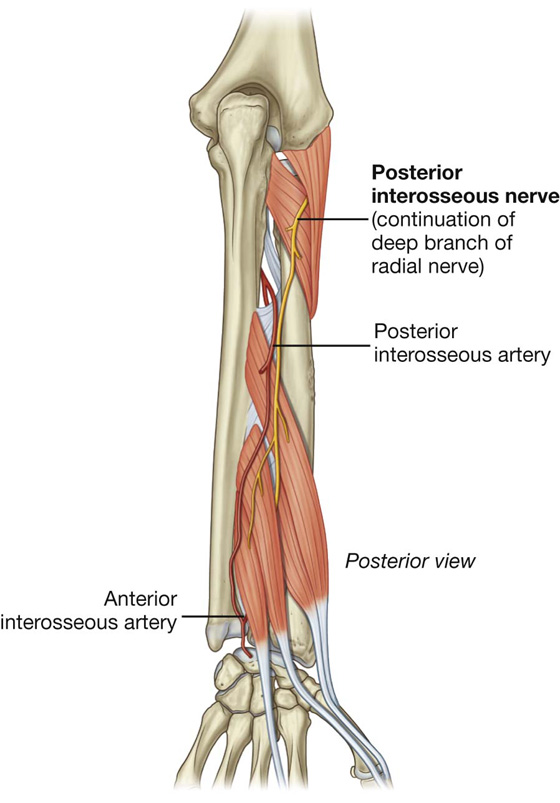
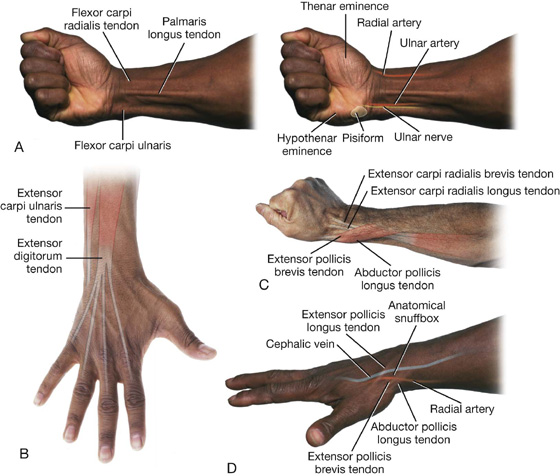
 the wrist (carpus),
the wrist (carpus), the metacarpus, and
the metacarpus, and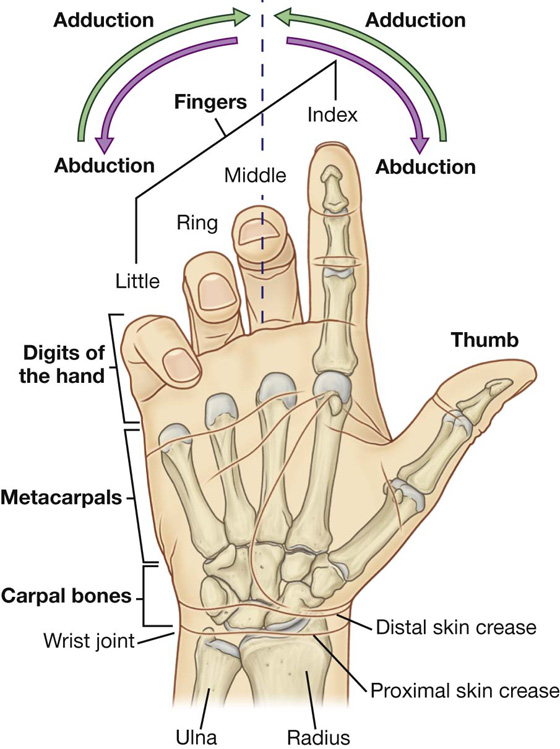
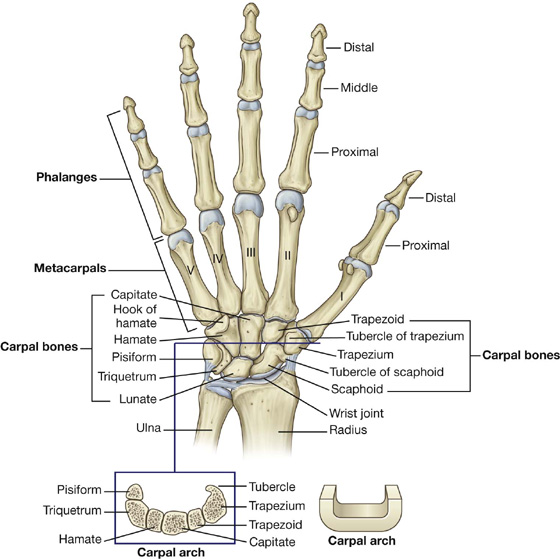
 the boat-shaped scaphoid,
the boat-shaped scaphoid, the pea-shaped pisiform.
the pea-shaped pisiform. the four-sided trapezoid,
the four-sided trapezoid, the hamate, which has a hook.
the hamate, which has a hook.
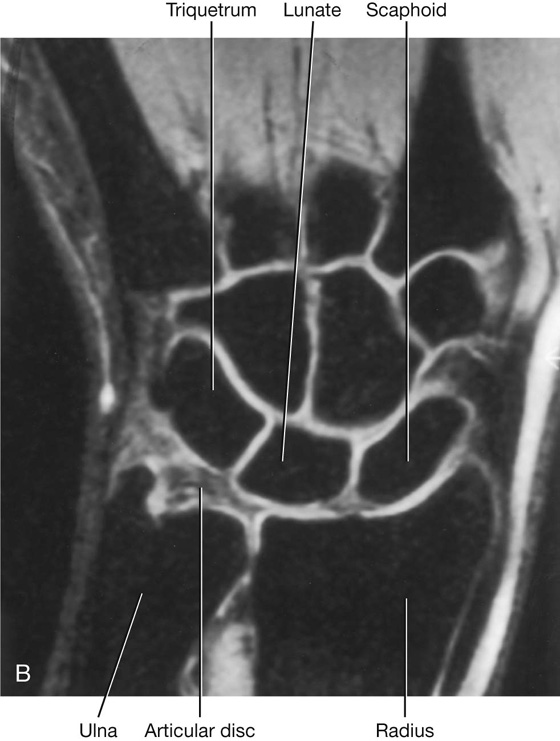
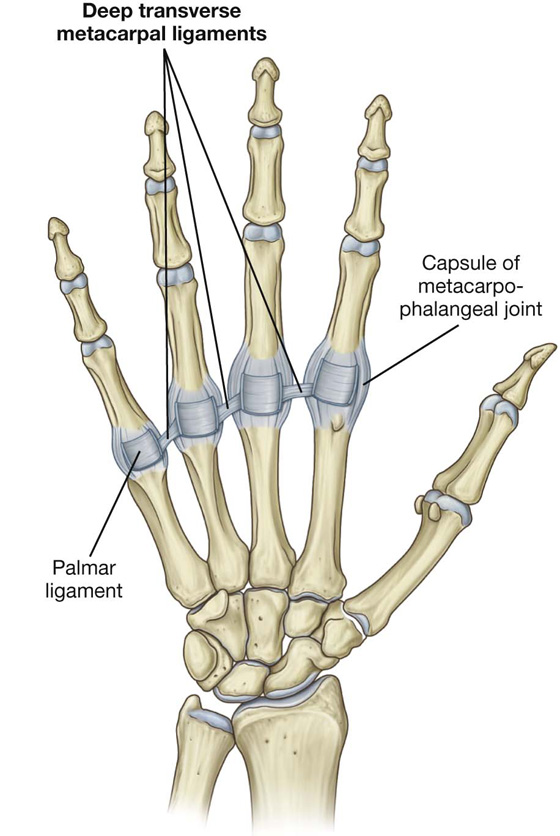
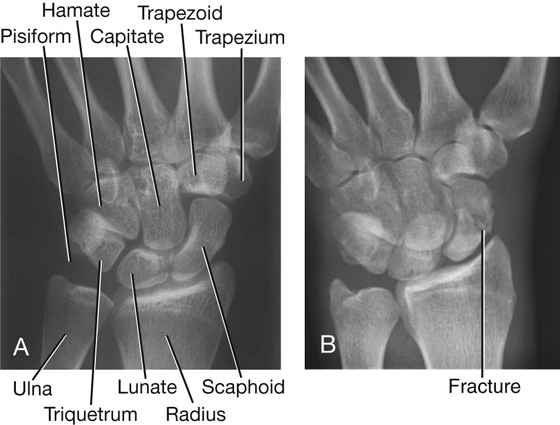
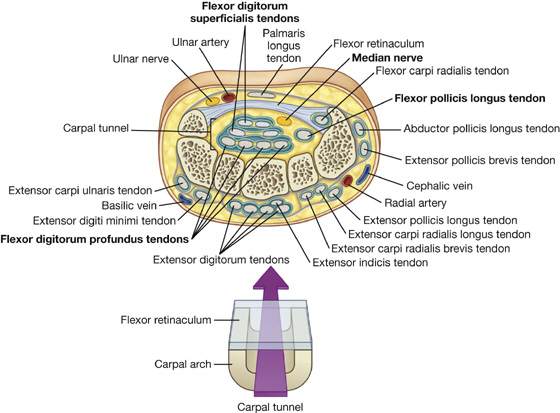
 The tendons of the extensor digitorum and extensor indicis share a compartment and synovial sheath on the posterior surface of the wrist.
The tendons of the extensor digitorum and extensor indicis share a compartment and synovial sheath on the posterior surface of the wrist. The tendons of the extensor carpi ulnaris and extensor digiti minimi have separate compartments and sheaths on the medial side of the wrist.
The tendons of the extensor carpi ulnaris and extensor digiti minimi have separate compartments and sheaths on the medial side of the wrist. The tendons of the abductor pollicis longus and extensor pollicis brevis muscles, the extensor carpi radialis longus and extensor carpi radialis brevis muscles, and the extensor pollicis longus muscle pass through three compartments on the lateral surface of the wrist.
The tendons of the abductor pollicis longus and extensor pollicis brevis muscles, the extensor carpi radialis longus and extensor carpi radialis brevis muscles, and the extensor pollicis longus muscle pass through three compartments on the lateral surface of the wrist.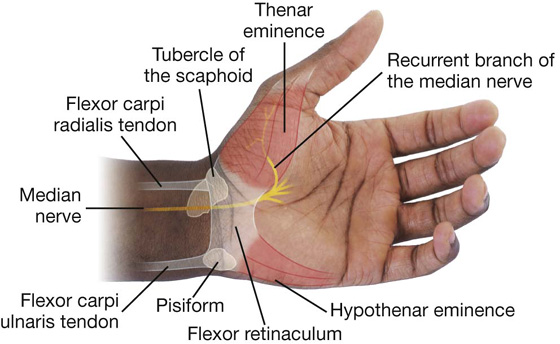
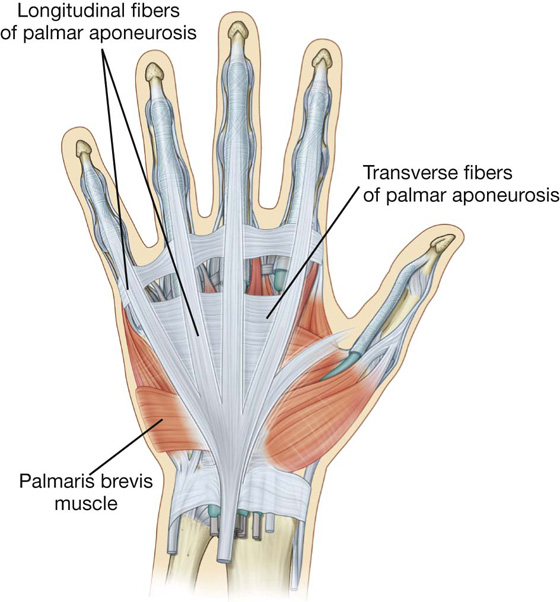
 The lateral border is formed by the tendons of the abductor pollicis longus and extensor pollicis brevis.
The lateral border is formed by the tendons of the abductor pollicis longus and extensor pollicis brevis. The floor of the impression is formed by the scaphoid and trapezium, and the distal ends of the tendons of the extensor carpi radialis longus and extensor carpi radialis brevis.
The floor of the impression is formed by the scaphoid and trapezium, and the distal ends of the tendons of the extensor carpi radialis longus and extensor carpi radialis brevis.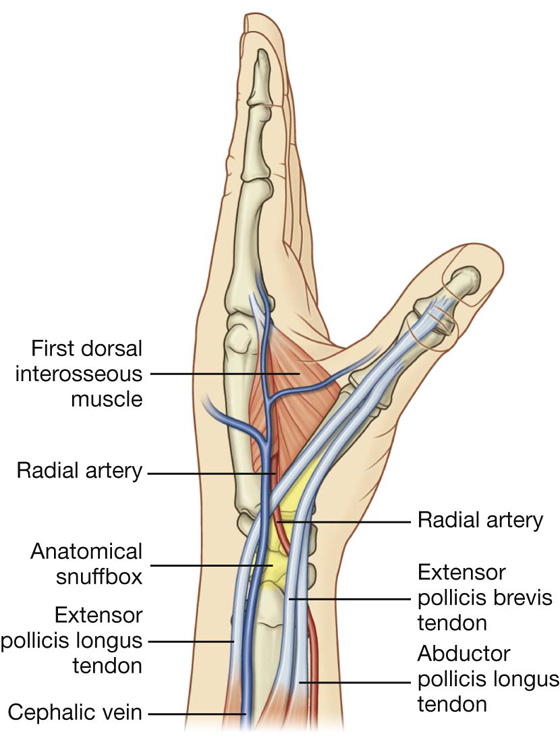
 are formed by fibrous arches and cruciate (cross-shaped) ligaments, which are attached posteriorly to the margins of the phalanges and to the palmar ligaments associated with the metacarpophalangeal and interphalangeal joints; and
are formed by fibrous arches and cruciate (cross-shaped) ligaments, which are attached posteriorly to the margins of the phalanges and to the palmar ligaments associated with the metacarpophalangeal and interphalangeal joints; and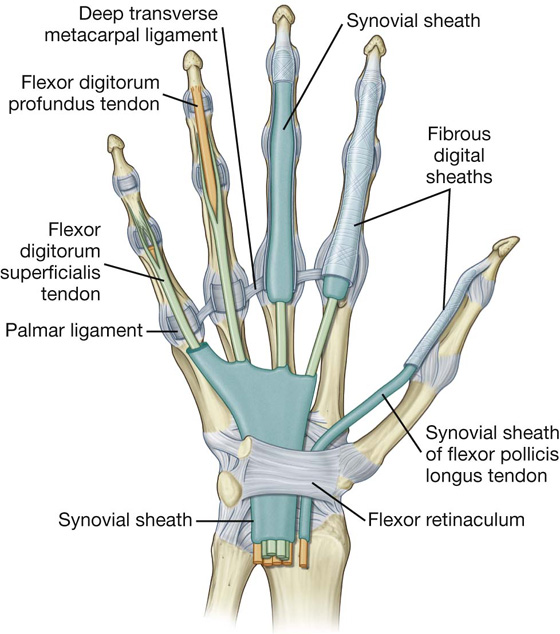
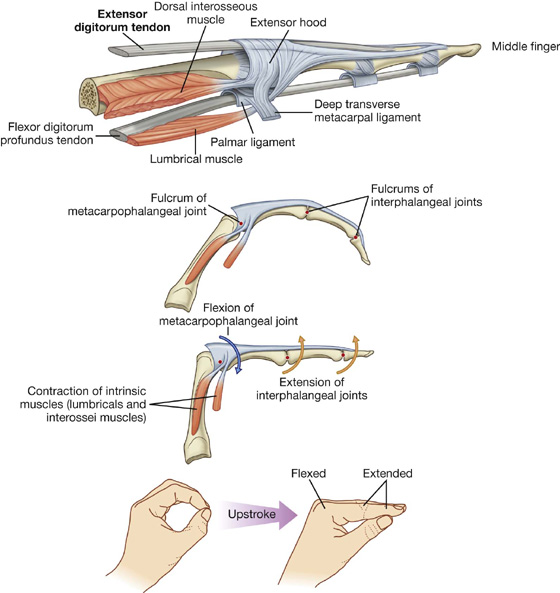
 the central region attached to the middle phalanx (index, middle, ring, and little fingers) or proximal phalanx (thumb); and
the central region attached to the middle phalanx (index, middle, ring, and little fingers) or proximal phalanx (thumb); and each corner of the base wrapped around the sides of the metacarpophalangeal joint—in the index, middle, ring, and little fingers, the corners of the hoods attach mainly to the deep transverse metacarpal ligaments; in the thumb, the hood is attached on each side to muscles.
each corner of the base wrapped around the sides of the metacarpophalangeal joint—in the index, middle, ring, and little fingers, the corners of the hoods attach mainly to the deep transverse metacarpal ligaments; in the thumb, the hood is attached on each side to muscles.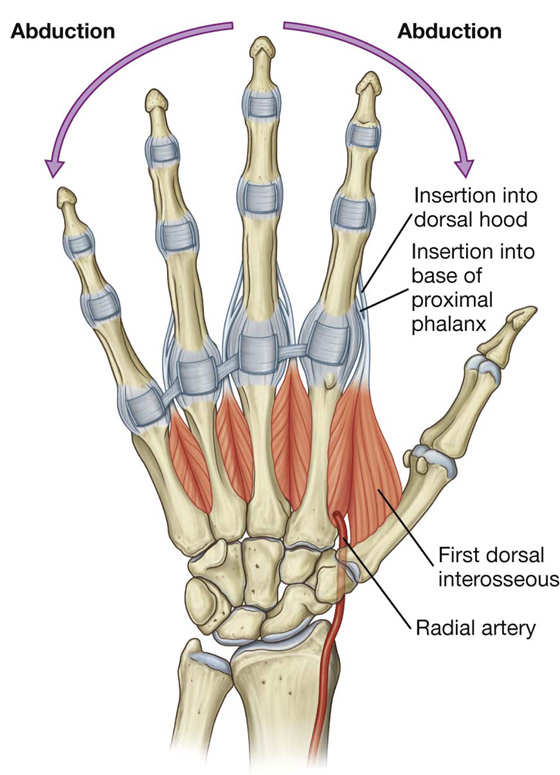
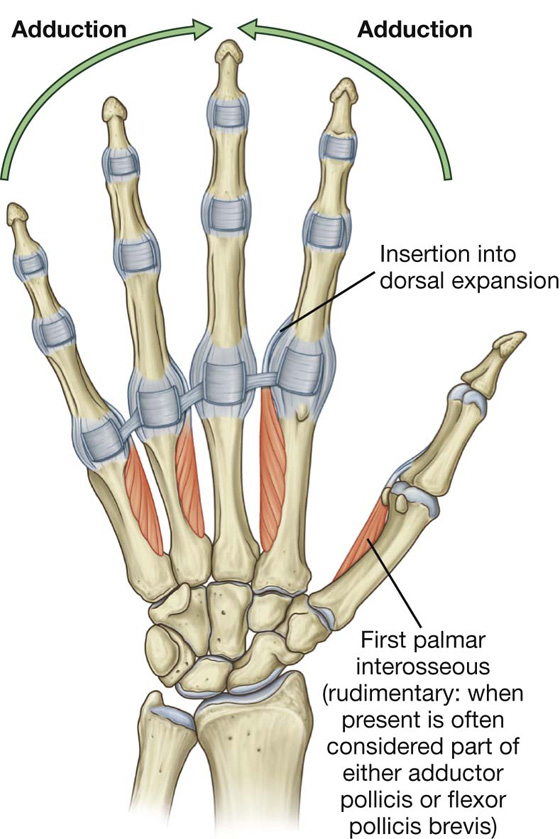
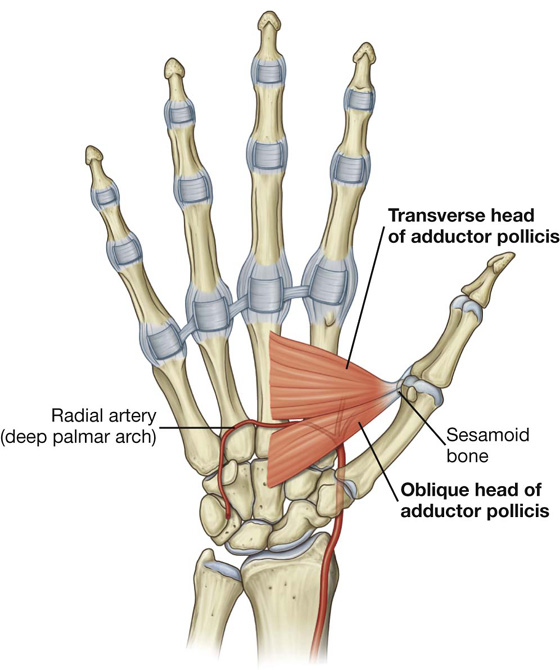
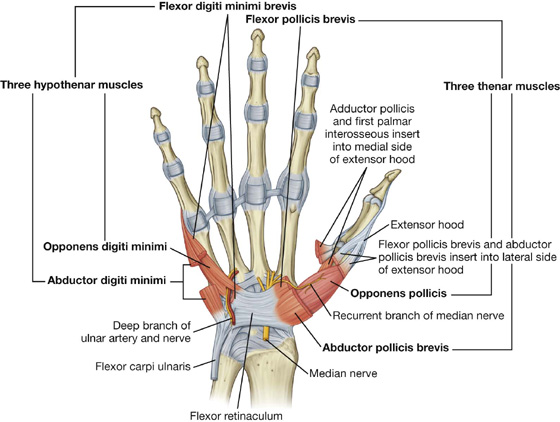
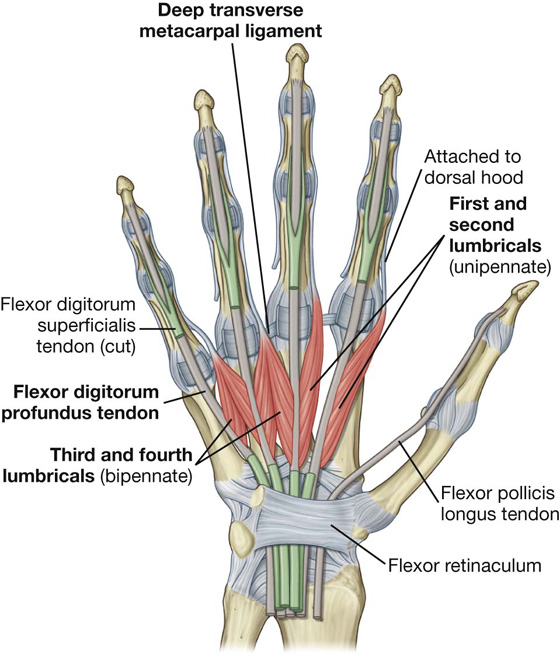
 The radial artery contributes substantially to the supply of the thumb and the lateral side of the index finger.
The radial artery contributes substantially to the supply of the thumb and the lateral side of the index finger. The remaining digits and the medial side of the index finger are supplied mainly by the ulnar artery.
The remaining digits and the medial side of the index finger are supplied mainly by the ulnar artery.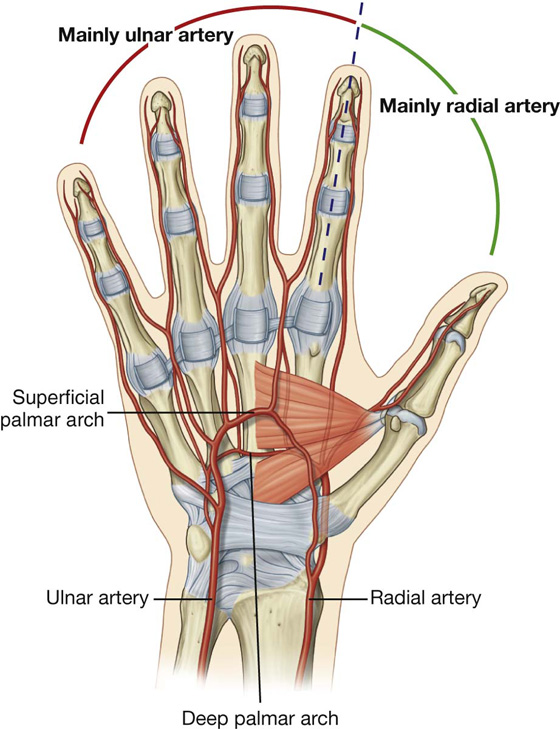
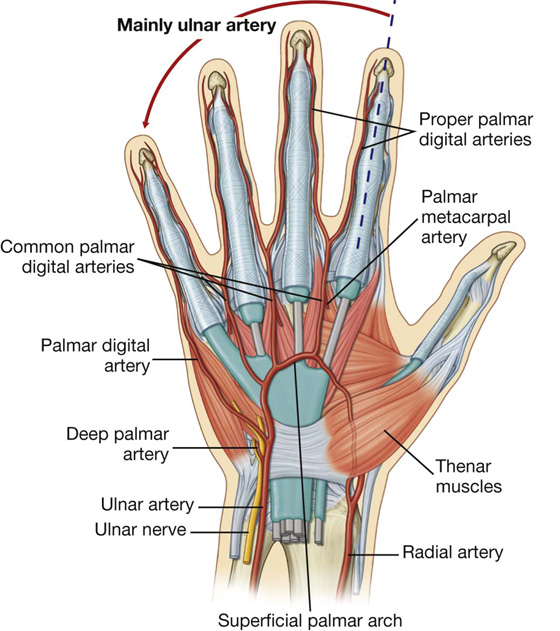
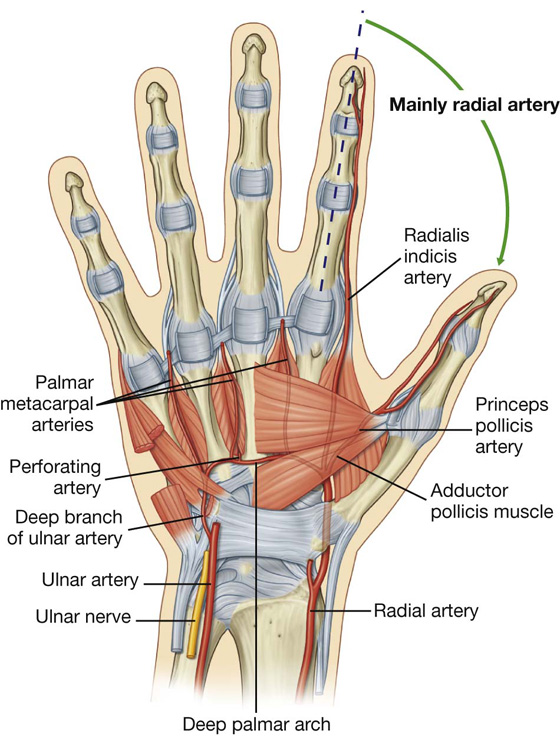
 three large, common palmar digital arteries, which ultimately provide the principal blood supply to the lateral side of the little finger, both sides of the ring and middle fingers, and the medial side of the index finger; they are joined by palmar metacarpal arteries from the deep palmar arch before bifurcating into the proper palmar digital arteries, which enter the fingers.
three large, common palmar digital arteries, which ultimately provide the principal blood supply to the lateral side of the little finger, both sides of the ring and middle fingers, and the medial side of the index finger; they are joined by palmar metacarpal arteries from the deep palmar arch before bifurcating into the proper palmar digital arteries, which enter the fingers. a dorsal carpal branch, which passes medially as the dorsal carpal arch, across the wrist and gives rise to dorsal metacarpal arteries, which subsequently divide to become small dorsal digital arteries, which enter the fingers;
a dorsal carpal branch, which passes medially as the dorsal carpal arch, across the wrist and gives rise to dorsal metacarpal arteries, which subsequently divide to become small dorsal digital arteries, which enter the fingers;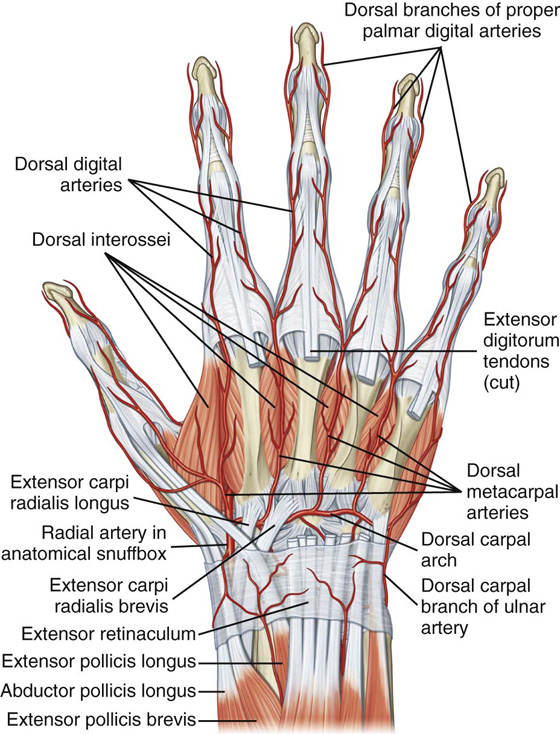
 three palmar metacarpal arteries, which join the common palmar digital arteries from the superficial palmar arch; and
three palmar metacarpal arteries, which join the common palmar digital arteries from the superficial palmar arch; and three perforating branches, which pass posteriorly between the heads of origin of the dorsal interossei to anastomose with the dorsal metacarpal arteries from the dorsal carpal arch.
three perforating branches, which pass posteriorly between the heads of origin of the dorsal interossei to anastomose with the dorsal metacarpal arteries from the dorsal carpal arch.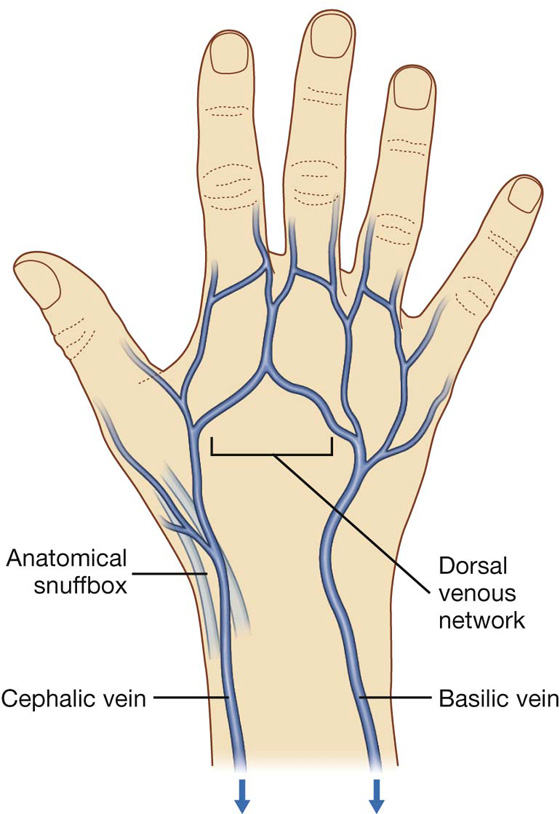
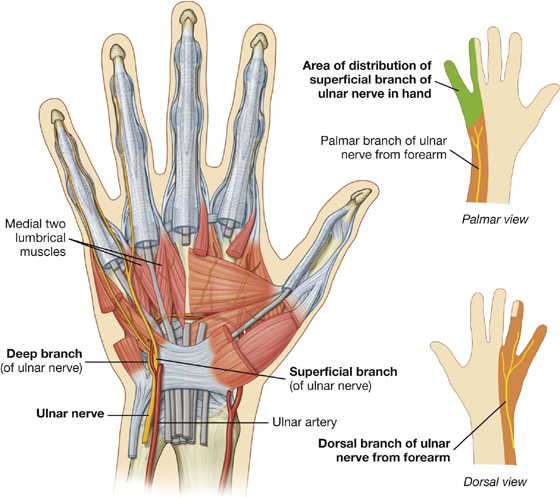
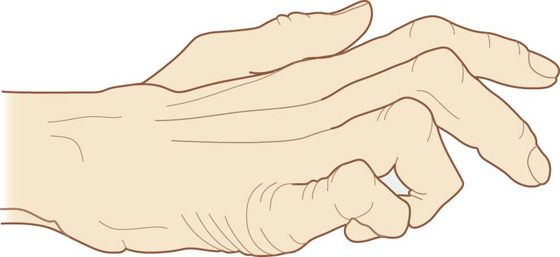
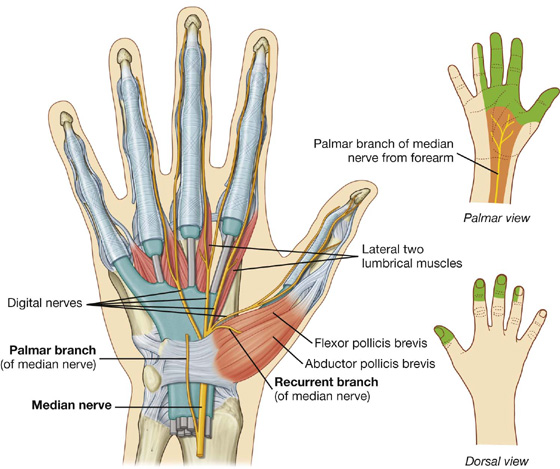

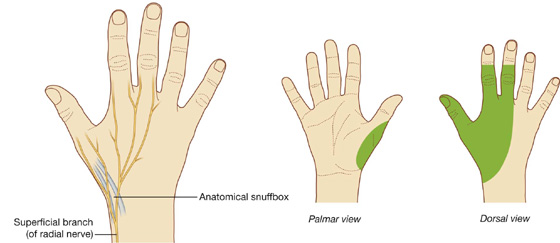
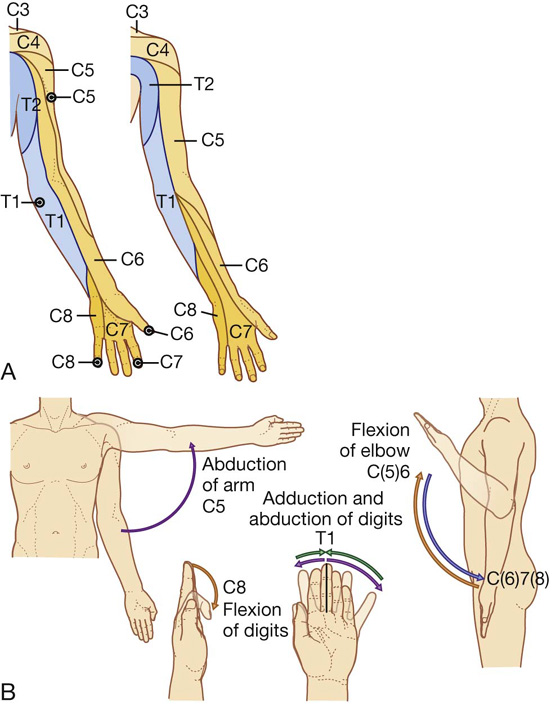
 The radial nerve supplies skin on the posterior surface of the forearm and the dorsolateral surface of the hand.
The radial nerve supplies skin on the posterior surface of the forearm and the dorsolateral surface of the hand.