Posterior spaces between vertebral arches
Curvatures of vertebral column
Joints between vertebrae in the back
Anterior and posterior longitudinal ligaments
Supraspinous ligament and ligamentum nuchae
Superficial group of back muscles
Intermediate group of back muscles
Arrangement of structures in the vertebral canal
 Image Library—illustrations of back anatomy, Chapter 2
Image Library—illustrations of back anatomy, Chapter 2
 Self-Assessment—National Board style multiple-choice questions, Chapter 2
Self-Assessment—National Board style multiple-choice questions, Chapter 2
 Short Questions—these are questions requiring short responses, Chapter 2
Short Questions—these are questions requiring short responses, Chapter 2
 Interactive Surface Anatomy—interactive surface animations, Chapter 2
Interactive Surface Anatomy—interactive surface animations, Chapter 2
Regional anatomy
The back consists of the posterior aspect of the body and provides the musculoskeletal axis of support for the trunk. The back also contains the spinal cord and proximal parts of the spinal nerves, which send and receive information to and from most of the body.
SKELETAL FRAMEWORK
Skeletal components of the back consist mainly of the vertebrae and associated intervertebral discs. The skull, scapulae, pelvic bones (ileum, ischium, pubis), and ribs also contribute to the bony framework of the back and provide sites for muscle attachment.
Vertebrae
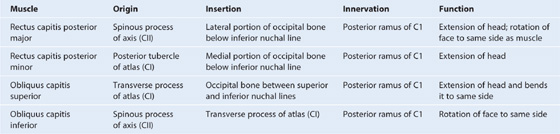
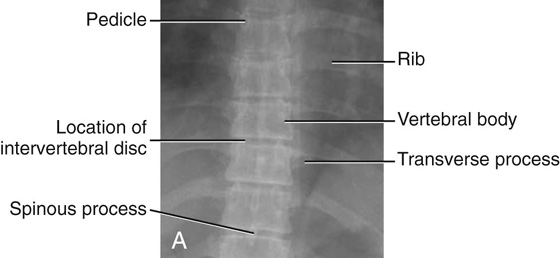
There are approximately 33 vertebrae, which are subdivided into five groups based on morphology and location (Fig. 2.1):
 The seven cervical vertebrae between the thorax and skull are characterized mainly by their small size, bifid spinous processes, and the presence of a foramen in each transverse process (Figs. 2.1, 2.2).
The seven cervical vertebrae between the thorax and skull are characterized mainly by their small size, bifid spinous processes, and the presence of a foramen in each transverse process (Figs. 2.1, 2.2).
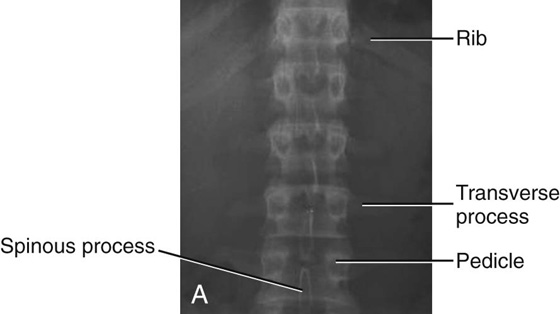
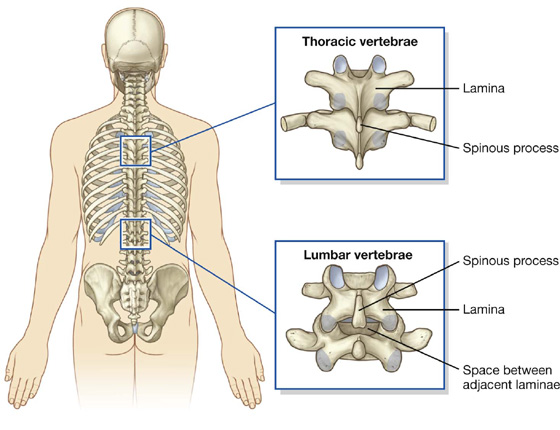
 The 12 thoracic vertebrae are characterized by their articulated ribs (Figs. 2.1, 2.3); ribs are separate bones and articulate via synovial joints with the vertebral bodies and transverse processes of the associated vertebrae; although all vertebrae have rib elements, these elements are small and are incorporated into the transverse processes in regions other than the thorax.
The 12 thoracic vertebrae are characterized by their articulated ribs (Figs. 2.1, 2.3); ribs are separate bones and articulate via synovial joints with the vertebral bodies and transverse processes of the associated vertebrae; although all vertebrae have rib elements, these elements are small and are incorporated into the transverse processes in regions other than the thorax.
 Inferior to the thoracic vertebrae are five lumbar vertebrae, which form the skeletal support for the posterior abdominal wall and are characterized by their large size (Figs. 2.1, 2.4).
Inferior to the thoracic vertebrae are five lumbar vertebrae, which form the skeletal support for the posterior abdominal wall and are characterized by their large size (Figs. 2.1, 2.4).
 Inferior to the sacrum is a variable number, usually four, of coccygeal vertebrae, which fuse into a single small triangular bone called the coccyx.
Inferior to the sacrum is a variable number, usually four, of coccygeal vertebrae, which fuse into a single small triangular bone called the coccyx.
Fig. 2.1 Vertebrae.
Imaging app
Typical cervical vertebrae
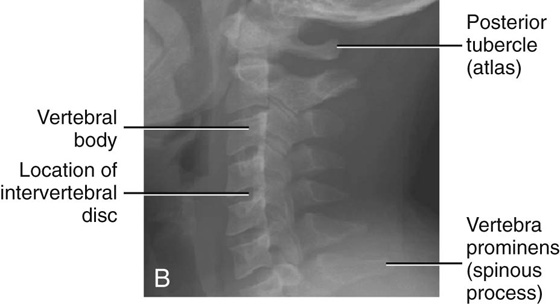
Fig. 2.2 Radiographs of cervical region of vertebral column. A. Anterior-posterior view. B. Lateral view.
Imaging app
Typical thoracic vertebrae
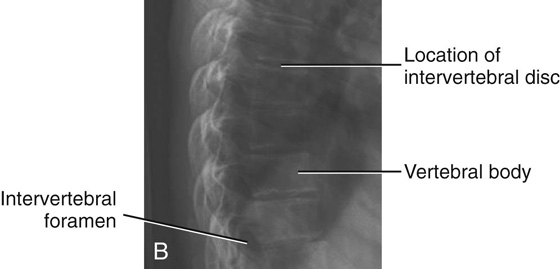
Fig. 2.3 Radiograph of thoracic region of vertebral column. A. Anterior-posterior view. B. Lateral view.
Imaging app
Typical lumbar vertebrae
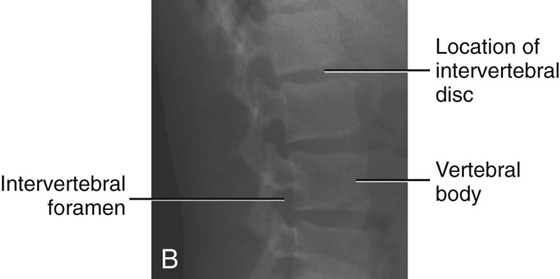
Fig. 2.4 Radiograph of lumbar region of vertebral column. A. Anterior-posterior view. B. Lateral view.
Typical vertebra
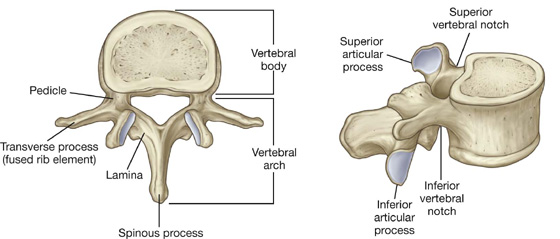
A typical vertebra consists of a vertebral body and a posterior vertebral arch (Fig. 2.5). Extending from the vertebral arch are a number of processes for muscle attachment and articulation with adjacent bone.
Fig. 2.5 Typical vertebra.
The vertebral body is the weightbearing part of the vertebra and is linked to adjacent vertebral bodies by intervertebral discs and ligaments. The size of vertebral bodies increases inferiorly as the amount of weight supported increases.
The vertebral arch forms the lateral and posterior parts of the vertebral foramen.
The vertebral foramina of all the vertebrae together form the vertebral canal, which contains and protects the spinal cord. Superiorly, the vertebral canal is continuous, through the foramen magnum of the skull, with the cranial cavity of the head.
The vertebral arch of each vertebra consists of pedicles and laminae (Fig. 2.5):
 The two pedicles are bony pillars that attach the vertebral arch to the vertebral body.
The two pedicles are bony pillars that attach the vertebral arch to the vertebral body.
 The two laminae are flat sheets of bone that extend from each pedicle to meet in the midline and form the roof of the vertebral arch.
The two laminae are flat sheets of bone that extend from each pedicle to meet in the midline and form the roof of the vertebral arch.
A spinous process projects posteriorly and inferiorly from the junction of the two laminae and is a site for muscle and ligament attachment.
A transverse process extends posterolaterally from the junction of the pedicle and lamina on each side and is a site for articulation with ribs in the thoracic region.
Also projecting from the region where the pedicles join the laminae are superior and inferior articular processes (Fig. 2.5), which articulate with the inferior and superior articular processes, respectively, of adjacent vertebrae.
Between the vertebral body and the origin of the articular processes, each pedicle is notched on its superior and inferior surfaces. These superior and inferior vertebral notches participate in forming intervertebral foramina.
Cervical vertebrae
The seven cervical vertebrae are characterized by their small size and by the presence of a foramen in each transverse process. A typical cervical vertebra has the following features (Fig. 2.6A):
 Each transverse process is trough shaped and perforated by a round foramen transversarium.
Each transverse process is trough shaped and perforated by a round foramen transversarium.
 The spinous process is short and bifid.
The spinous process is short and bifid.
 The vertebral foramen is triangular.
The vertebral foramen is triangular.
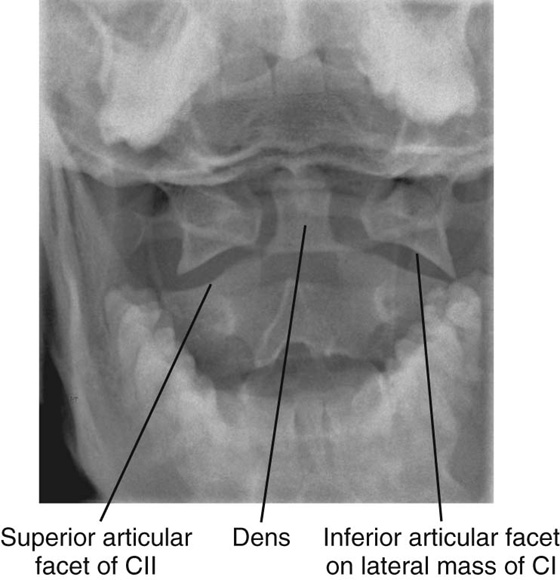
The first and second cervical vertebrae—the atlas and axis—are specialized to accommodate movement of the head.
Atlas and axis
Vertebra CI (the atlas) articulates with the head (Figs. 2.6B, 2.7). Its major distinguishing feature is that it lacks a vertebral body (Fig. 2.6B). In fact, the vertebral body of CI fuses onto the body of CII during development to become the dens of CII. As a result, there is no intervertebral disc between CI and CII. When viewed from above, the atlas is ring shaped and composed of two lateral masses interconnected by an anterior arch and a posterior arch.
Each lateral mass articulates above with an occipital condyle of the skull and below with the superior articular process of vertebra CII (the axis). The superior articular facets are bean shaped and concave, whereas the inferior articular facets are almost circular and flat.
The atlanto-occipital joint allows the head to nod up and down on the vertebral column.
The posterior surface of the anterior arch has an articular facet for the dens, which projects superiorly from the vertebral body of the axis. The dens is held in position by a strong transverse ligament of atlas posterior to it and spanning the distance between the oval attachment facets on the medial surfaces of the lateral masses of the atlas (Fig. 2.6B).
Imaging app
Articulation between atlas and axis
Fig. 2.7 Radiograph showing CI (atlas) and CII (axis) vertebrae. Open mouth, anterior-posterior (odontoid peg) view.
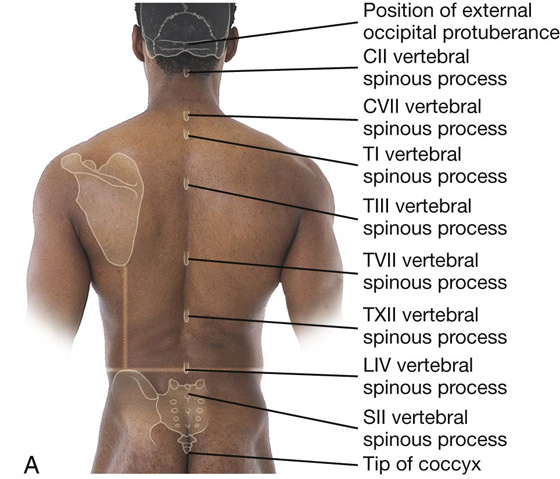
How to identify specific vertebral spinous processes
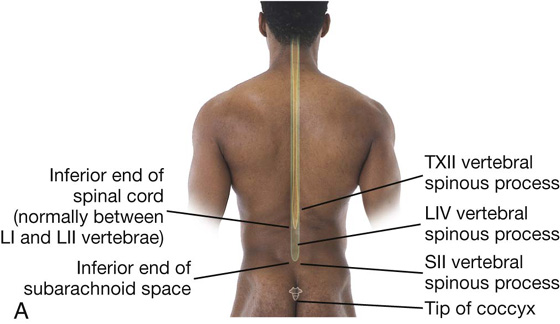
Identification of vertebral spinous processes (Fig. 2.8A) can be used to differentiate between regions of the vertebral column and facilitate visualizing the position of deeper structures, such as the inferior ends of the spinal cord and subarachnoid space.
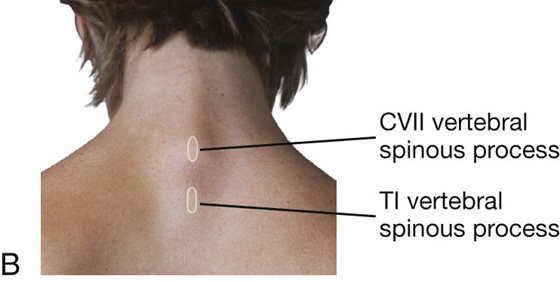
The spinous process of vertebra CII can be identified through deep palpation as the most superior bony protuberance in the midline inferior to the skull.
Most of the other spinous processes, except for that of vertebra CVII, are not readily palpable because they are obscured by soft tissue.
The spinous process of CVII is usually visible as a prominent eminence in the midline at the base of the neck (Fig. 2.8B), particularly when the neck is flexed.
Inferior to the spinous process of CVII is the spinous process of TI, which is also usually visible as a midline protuberance. Often it is more prominent than the spinous process of CVII.
The root of the spine of the scapula is at the same level as the spinous process of vertebra TIII, and the inferior angle of the scapula is level with the spinous process of vertebra TVII.
The spinous process of vertebra TXII is level with the midpoint of a vertical line between the inferior angle of the scapula and the iliac crest.
A horizontal line between the highest point of the iliac crest on each side crosses through the spinous process of vertebra LIV. The LIII and LV vertebral spinous processes can be palpated above and below the LIV spinous process, respectively.
The sacral dimples that mark the position of the posterior superior iliac spine are level with the SII vertebral spinous process.
The tip of the coccyx is palpable at the base of the vertebral column between the gluteal masses.
The tips of the vertebral spinous processes do not always lie in the same horizontal plane as their corresponding vertebral bodies. In thoracic regions, the spinous processes are long and sharply sloped downward so that their tips lie at the level of the vertebral body below. In other words, the tip of the TIII vertebral spinous process lies at vertebral level TIV.
In lumbar and sacral regions, the spinous processes are generally shorter and less sloped than in thoracic regions, and their palpable tips more closely reflect the position of their corresponding vertebral bodies. As a consequence, the palpable end of the spinous process of vertebra LIV lies at approximately the LIV vertebral level.
The dens acts as a pivot that allows the atlas and attached head to rotate on the axis, side to side.
The transverse processes of the atlas are large and protrude farther laterally than those of the other cervical vertebrae. They act as levers for muscle action, particularly for muscles that move the head at the atlanto-axial joints.
The axis is characterized by the large toothlike dens, which extends superiorly from the vertebral body (Figs. 2.6B and 2.7). The anterior surface of the dens has an oval facet for articulation with the anterior arch of the atlas.
The two superolateral surfaces of the dens possess circular impressions that serve as attachment sites for strong alar ligaments, one on each side, which connect the dens to the medial surfaces of the occipital condyles. These alar ligaments check excessive rotation of the head and atlas relative to the axis (Fig. 2.6B).
Thoracic vertebrae
The twelve thoracic vertebrae are all characterized by their articulation with ribs. A typical thoracic vertebra has two partial facets (superior and inferior costal facets) on each side of the vertebral body for articulation with the head of its own rib and the head of the rib below (Fig. 2.6C). The superior costal facet is much larger than the inferior costal facet.
Each transverse process also has a facet (transverse costal facet) for articulation with the tubercle of its own rib. The vertebral body of the vertebra is somewhat heart-shaped when viewed from above, and the vertebral foramen is circular.
Lumbar vertebrae
The five lumbar vertebrae are distinguished from vertebrae in other regions by their large size (Fig. 2.6D). Also, they lack facets for articulation with ribs. The transverse processes are generally thin and long, with the exception of those on vertebra LV, which are massive and somewhat cone-shaped for the attachment of iliolumbar ligaments to connect the transverse processes to the pelvic bones.
The vertebral body of a typical lumbar vertebra is cylindrical and the vertebral foramen is triangular in shape and larger than in the thoracic vertebrae.
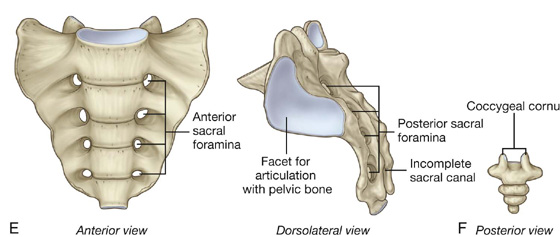
Sacrum
The sacrum is a single bone that represents the five fused sacral vertebrae (Fig. 2.6E). It is triangular in shape with the apex pointed inferiorly, and is curved so that it has a concave anterior surface and a correspondingly convex posterior surface. It articulates above with vertebra LV and below with the coccyx. It has two large L-shaped facets, one on each lateral surface, for articulation with the pelvic bones.
The posterior surface of the sacrum has four pairs of posterior sacral foramina, and the anterior surface has four pairs of anterior sacral foramina for the passage of the posterior and anterior rami, respectively, of S1 to S4 spinal nerves.
The posterior wall of the vertebral canal may be incomplete near the inferior end of the sacrum.
Coccyx
The coccyx is a small triangular bone that articulates with the inferior end of the sacrum and represents three to four fused coccygeal vertebrae (Fig. 2.6F). It is characterized by its small size and by the absence of vertebral arches and therefore a vertebral canal.
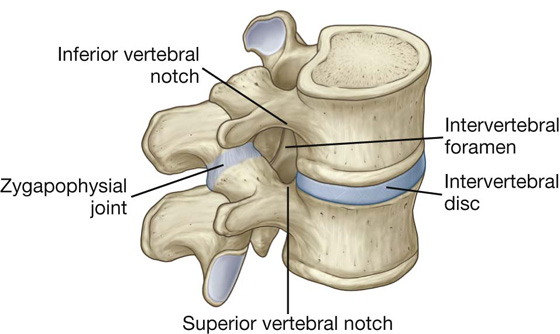
Intervertebral foramina
Intervertebral foramina are formed on each side between adjacent parts of vertebrae and associated intervertebral discs (Fig. 2.9). The foramina allow structures, such as spinal nerves and blood vessels, to pass in and out of the vertebral canal.
Fig. 2.9 Intervertebral foramen.
An intervertebral foramen is formed by the inferior vertebral notch on the pedicle of the vertebra above and the superior vertebral notch on the pedicle of the vertebra below. The foramen is bordered:
 posteriorly by the zygapophysial joint between the articular processes of the two vertebrae, and
posteriorly by the zygapophysial joint between the articular processes of the two vertebrae, and
 anteriorly by the intervertebral disc and adjacent vertebral bodies.
anteriorly by the intervertebral disc and adjacent vertebral bodies.
Each intervertebral foramen is a confined space surrounded by bone, ligaments, and joints. Pathology in any of these structures, and in the surrounding muscles, can affect structures within the foramen.
Posterior spaces between vertebral arches
In most regions of the vertebral column, the laminae and spinous processes of adjacent vertebrae overlap to form a reasonably complete bony posterior (dorsal) wall for the vertebral canal. However, in the lumbar region, large gaps exist between the posterior components of adjacent vertebral arches (Fig. 2.10). These gaps between adjacent laminae and spinous processes become increasingly wide from vertebra LI to vertebra LV. The spaces can be widened further by flexion of the vertebral column. These gaps allow relatively easy access to the vertebral canal for clinical procedures.
Fig. 2.10 Spaces between adjacent vertebral arches in the lumbar region.
Curvatures of vertebral column
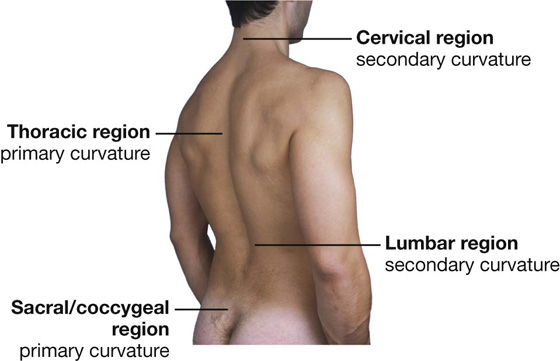
The vertebral column has a number of curvatures (Fig. 2.11):
Fig. 2.11 Curvatures of the vertebral column.
Surface anatomy
Primary and secondary curvatures in the sagittal plane
When viewed from the side, the normal vertebral column has primary curvatures in the thoracic and sacral/coccygeal regions and secondary curvatures in the cervical and lumbar regions (Fig. 2.12). The primary curvatures are concave anteriorly. The secondary curvatures are concave posteriorly.
Clinical app
Spina bifida
Spina bifida is a disorder in which the two sides of vertebral arches, usually in lower vertebrae, fail to fuse during development, resulting in an “open” vertebral canal. There are two types of spina bifida.
 The commonest type is spina bifida occulta, in which there is a defect in the vertebral arch of LV or SI. This defect occurs in as many as 10% of individuals and results in failure of the posterior arch to fuse in the midline. Clinically, the patient is asymptomatic, although there may be a tuft of hair over the spinous processes.
The commonest type is spina bifida occulta, in which there is a defect in the vertebral arch of LV or SI. This defect occurs in as many as 10% of individuals and results in failure of the posterior arch to fuse in the midline. Clinically, the patient is asymptomatic, although there may be a tuft of hair over the spinous processes.
Clinical app
Vertebroplasty
Vertebroplasty is a new technique in which the body of a vertebra can be filled with bone cement (typically methyl methacrylate). The indications for the technique include vertebral body collapse and pain from the vertebral body, which may be secondary to tumor infiltration. The procedure is most commonly performed for osteoporotic wedge fractures, which are a considerable cause of morbidity and pain in older patients. These types of fractures typically occur at the thoracolumbar region.
Clinical app
Scoliosis
Scoliosis is an abnormal lateral curvature of the vertebral column (Fig. 2.13).
Fig. 2.13 Radiograph of thoracic scoliosis.
A true scoliosis involves not only the (right- or left-sided) curvature but also a rotational element of one vertebra on another.
The commonest types of scoliosis are those for which we have little understanding about how or why they occur and are termed idiopathic scoliosis. These are never present at birth and tend to occur in either the infantile, juvenile, or adolescent age groups. The vertebral bodies and posterior elements (pedicles and laminae) are normal in these patients.
Clinical app
Kyphosis
Kyphosis is abnormal curvature (exaggerated anterior concavity) of the vertebral column in the thoracic region, producing a “hunchback” deformity. This condition occurs in certain disease states, the most dramatic of which is usually secondary to tuberculosis infection of a thoracic vertebral body, where the kyphosis becomes angulated at the site of the lesion.
Clinical app
Lordosis
Lordosis is abnormal curvature (exaggerated posterior concavity) of the vertebral column in the lumbar region, producing a swayback deformity.
Clinical app
Variation in vertebral numbers
There are usually seven cervical vertebrae, although in certain diseases these may be fused. Fusion of cervical vertebrae can be associated with other abnormalities in which there is abnormal fusion of vertebrae CI and CII or CV and CVI.
Variations in the number of thoracic vertebrae are well described. One of the commonest abnormalities in the lumbar vertebrae is a partial fusion of vertebra LV with the sacrum (sacralization of the lumbar vertebra). Partial separation of vertebra SI from the sacrum (lumbarization of first sacral vertebra) may also occur.
A hemivertebra occurs when a vertebra develops only on one side.
Clinical app
The vertebrae and cancer
The vertebrae are common sites for metastatic disease (secondary spread of cancer cells). When cancer cells grow within the vertebral bodies and the posterior elements, they destroy the mechanical properties of the bone. Importantly, vertebrae that contain extensive metastatic disease may extrude fragments of tumor into the vertebral canal, compressing the nerves and spinal cord.
Clinical app
Osteoporosis
Osteoporosis is a pathophysiological condition in which bone quality is normal, but the quantity of bone is deficient. It is a metabolic bone disorder that commonly occurs in women in their 50s and 60s and in men in their 70s.
Typical complications of osteoporosis include “crush” vertebral body fractures, distal radial fractures, and hip fractures.
JOINTS
Joints between vertebrae in the back
The two major types of joints between vertebrae are:
 symphyses between vertebral bodies, and
symphyses between vertebral bodies, and
 synovial joints between articular processes.
synovial joints between articular processes.
A typical vertebra has a total of six joints with adjacent vertebrae: four synovial joints (two above and two below) and two symphyses (one above and one below). Each symphysis includes an intervertebral disc.
Although the movement between any two vertebrae is limited, the summation of movement among all vertebrae results in a large range of movement by the vertebral column.
Movements by the vertebral column include flexion, extension, lateral flexion, rotation, and circumduction.
Movements by vertebrae in a specific region (cervical, thoracic, and lumbar) are determined by the shape and orientation of joint surfaces on the articular processes and on the vertebral bodies.
Symphyses between vertebral bodies (intervertebral discs)
The symphysis between adjacent vertebral bodies is formed by a layer of hyaline cartilage on each vertebral body and an intervertebral disc, which lies between the layers.
The intervertebral disc consists of an outer anulus fibrosus, which surrounds a central nucleus pulposus (Fig. 2.14).
Fig. 2.14 Intervertebral joints.
Degenerative changes in the anulus fibrosus can lead to herniation of the nucleus pulposus. Posterolateral herniation can impinge on the roots of a spinal nerve in the intervertebral foramen.
Joints between vertebral arches (zygapophysial joints)
The synovial joints between superior and inferior articular processes on adjacent vertebrae are the zygapophysial joints (Fig. 2.15). A thin articular capsule attached to the margins of the articular facets encloses each joint.
Fig. 2.15 Zygapophysial joints.
In cervical regions, the zygapophysial joints slope inferiorly from anterior to posterior. This orientation facilitates flexion and extension. In thoracic regions, the joints are oriented vertically and limit flexion and extension, but facilitate rotation. In lumbar regions, the joint surfaces are curved and adjacent processes interlock, thereby limiting range of movement, although flexion and extension are still major movements in the lumbar region.
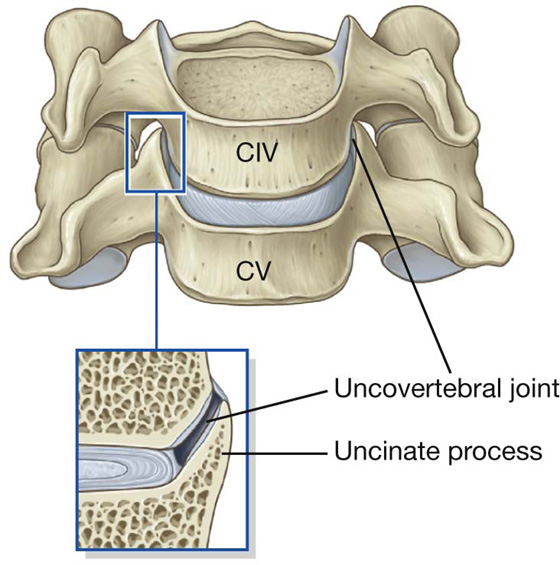
“Uncovertebral” joints
The lateral margins of the upper surfaces of typical cervical vertebrae are elevated into crests or lips termed uncinate processes. These may articulate with the body of the vertebra above to form small “uncovertebral” synovial joints (Fig. 2.16).
Fig. 2.16 Uncovertebral joint.
Clinical app
Back pain
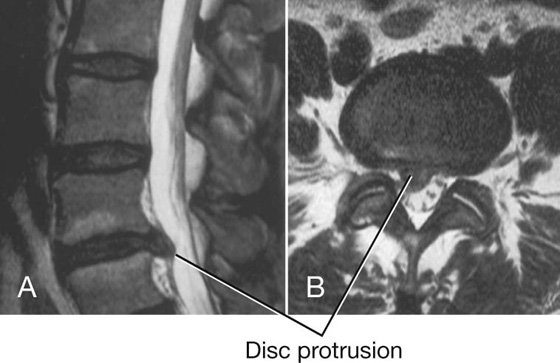
Back pain is an extremely common disorder. It can be related to mechanical problems or to a disc protrusion impinging on a nerve. In cases involving discs, it may be necessary to operate and remove the disc that is pressing on the nerve.
Clinical app
Herniation of intervertebral discs
The discs between the vertebrae are made up of a central portion (the nucleus pulposus) and a complex series of fibrous rings (anulus fibrosus). A tear can occur within the anulus fibrosus through which the material of the nucleus pulposus can track. After a period of time, this material may track into the vertebral canal or into the intervertebral foramen to impinge on neural structures (Fig. 2.17). This is a common cause of back pain. A disc may protrude posteriorly to directly impinge on the cord or the roots of the lumbar nerves, depending on the level, or may protrude posterolaterally adjacent to the pedicle and impinge on the descending root.
In cervical regions of the vertebral column, cervical disc protrusions often become ossified and are termed disc osteophyte bars.
Clinical app
Joint diseases
Some diseases have a predilection for synovial joints rather than symphyses. A typical example is rheumatoid arthritis, which primarily affects synovial joints and synovial bursae, resulting in destruction of the joint and its lining. Symphyses are usually preserved.
LIGAMENTS
Joints between vertebrae are reinforced and supported by numerous ligaments, which pass between vertebral bodies and interconnect components of the vertebral arches.
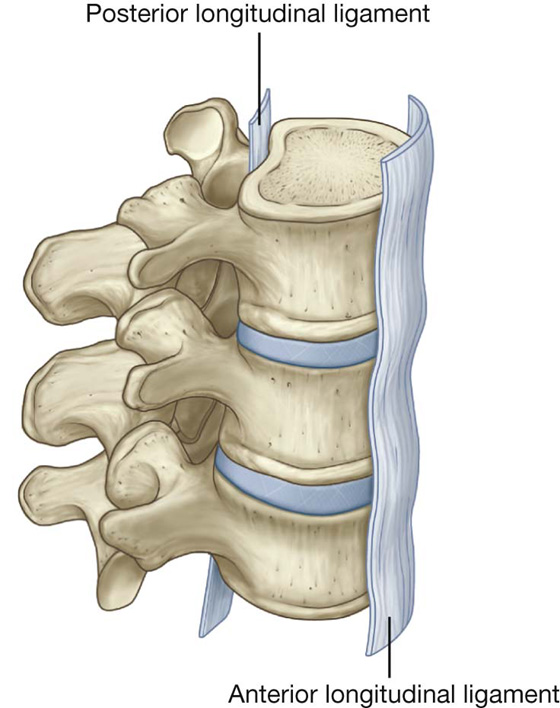
Anterior and posterior longitudinal ligaments
The anterior and posterior longitudinal ligaments are on the anterior and posterior surfaces of the vertebral bodies and extend along most of the vertebral column (Fig. 2.18).
Fig. 2.18 Anterior and posterior longitudinal ligaments of vertebral column.
The anterior longitudinal ligament is attached superiorly to the base of the skull and extends inferiorly to attach to the anterior surface of the sacrum. Along its length, it is attached to the vertebral bodies and intervertebral discs.
The posterior longitudinal ligament is on the posterior surfaces of the vertebral bodies and lines the anterior surface of the vertebral canal. Like the anterior longitudinal ligament, it is attached along its length to the vertebral bodies and intervertebral discs. The upper part of the posterior longitudinal ligament that connects CII to the intracranial aspect of the base of the skull is termed the tectorial membrane.
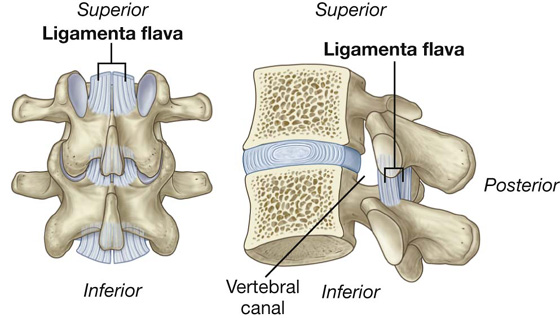
Ligamenta flava
The ligamenta flava, on each side, pass between the laminae of adjacent vertebrae (Fig. 2.19). These thin, broad ligaments consist predominantly of elastic tissue and form part of the posterior surface of the vertebral canal. Each ligamentum flavum runs between the posterior surface of the lamina on the vertebra below to the anterior surface of the lamina of the vertebra above. The ligamenta flava resist separation of the laminae in flexion and assist in extension back to the anatomical position.
Fig. 2.19 Ligamenta flava.
Supraspinous ligament and ligamentum nuchae
The supraspinous ligament connects and passes along the tips of the vertebral spinous processes from vertebra CVII to the sacrum (Fig. 2.20). From vertebra CVII to the skull, the ligament becomes structurally distinct from more caudal parts of the ligament and is called the ligamentum nuchae.
Fig. 2.20 Supraspinous ligament and ligamentum nuchae.
The ligamentum nuchae is a triangular, sheetlike structure in the median sagittal plane:
 The apex is attached to the tip of the spinous process of vertebra CVII.
The apex is attached to the tip of the spinous process of vertebra CVII.
The ligamentum nuchae supports the head. It resists flexion and facilitates returning the head to the anatomical position. The broad lateral surfaces and the posterior edge of the ligament provide attachment for adjacent muscles.
Interspinous ligaments
Interspinous ligaments pass between adjacent vertebral spinous processes (Fig. 2.21). They attach from the base to the apex of each spinous process and blend with the supraspinous ligament posteriorly and the ligamenta flava anteriorly on each side.
Fig. 2.21 Interspinous ligaments.
Clinical app
Ligamenta flava
In degenerative conditions of the vertebral column, the ligamenta flava may hypertrophy. This is often associated with hypertrophy and arthritic change of the zygapophysial joints. In combination, zygapophysial joint hypertrophy, ligamenta flava hypertrophy, and a mild disc protrusion can reduce the dimensions of the vertebral canal.
Vertebral fractures
Vertebral column stability is divided into three arbitrary clinical “columns:” the anterior column consists of the vertebral bodies and the anterior longitudinal ligament; the middle column comprises the vertebral body and the posterior longitudinal ligament; and the posterior column is made up of the ligamenta flava, interspinous ligaments, supraspinous ligaments, and the ligamentum nuchae in the cervical vertebral column.
Destruction of one of the clinical columns is usually a stable injury requiring little more than rest and appropriate analgesia. Disruption of two columns is likely to be unstable and requires fixation and immobilization. A three-column spinal injury usually results in a significant neurological event and requires fixation to prevent further extension of the neurological defect and to create vertebral column stability.
Clinical app
Pars interarticularis fractures
The pars interarticularis is a clinical term used to describe the specific region of a vertebra between the superior and inferior facet (zygapophysial) joints. This region is susceptible to trauma, especially in athletes.
If a fracture occurs around the pars interarticularis, the vertebral body may slip anteriorly and compress the vertebral canal. The most common sites for pars interarticularis fractures are the LIV and LV levels. It is possible for a vertebra to slip anteriorly on its inferior counterpart without a pars interarticularis fracture. Usually this is related to abnormal anatomy of the facet joints: facet joint degenerative change. This disorder is termed spondylolisthesis.
Clinical app
Surgical procedures on the back
Discectomy
A prolapsed intervertebral disc may impinge on the meningeal (thecal) sac, cord, and most commonly the nerve root, producing symptoms attributable to that level. In some instances the disc protrusion will undergo a degree of involution that may allow symptoms to resolve without intervention. In some instances, pain, loss of function, and failure to resolve may require surgery to remove the disc protrusion.
Spinal (vertebral) fusion is performed when it is necessary to fuse one vertebra with the corresponding superior or inferior vertebra, and in some instances multilevel fusion may be necessary. Indications are varied, although they include stabilization after fracture, stabilization related to tumor infiltration, and stabilization when mechanical pain is produced either from the disc or from the posterior elements.
BACK MUSCULATURE
Muscles of the back are organized into superficial, intermediate, and deep groups.
Muscles in the superficial and intermediate groups are extrinsic muscles because they originate embryologically from locations other than the back. They are innervated by anterior rami of spinal nerves:
 The superficial group consists of muscles related to and involved in movements of the upper limb.
The superficial group consists of muscles related to and involved in movements of the upper limb.
Muscles of the deep group are intrinsic muscles because they develop in the back. They are innervated by posterior rami of spinal nerves and are directly related to movements of the vertebral column and head.
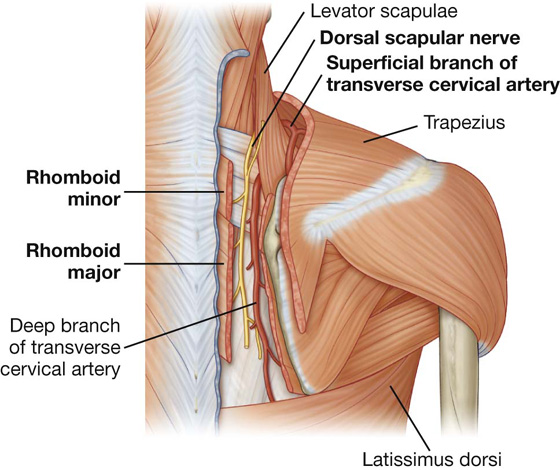
Superficial group of back muscles
The muscles in the superficial group are immediately deep to the skin and superficial fascia. They attach the superior part of the appendicular skeleton (clavicle, scapula, and humerus) to the axial skeleton (skull, ribs, and vertebral column). Because these muscles are primarily involved with movements of this part of the appendicular skeleton, they are sometimes referred to as the appendicular group.
Muscles in the superficial group include the trapezius, latissimus dorsi, rhomboid major, rhomboid minor, and levator scapulae (Fig. 2.22). Rhomboid major, rhomboid minor, and levator scapulae are located deep to the trapezius in the superior part of the back.
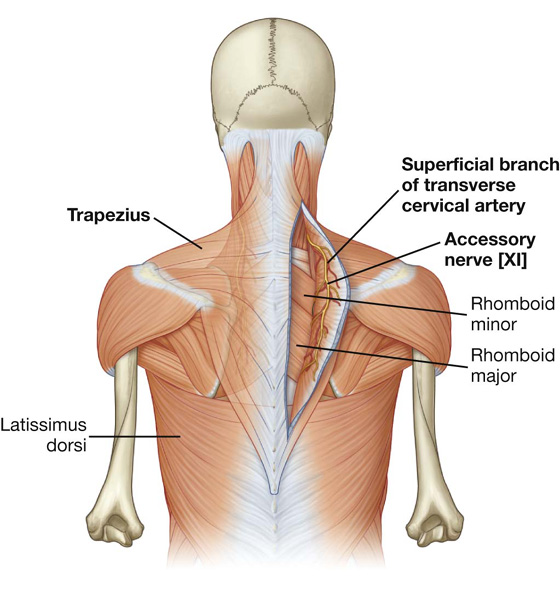
Trapezius
Each trapezius muscle is flat and triangular, with the base of the triangle situated along the vertebral column (the muscle’s origin) and the apex pointing toward the tip of the shoulder (the muscle’s insertion) (Table 2.1, Fig. 2.22). The muscles on both sides together form a trapezoid.
Table 2.1 Superficial (appendicular) group of back muscles
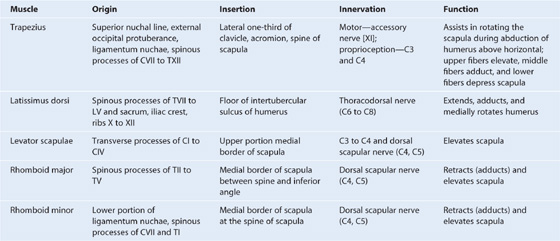
Motor innervation of the trapezius is by the accessory nerve [XI], which descends from the neck onto the deep surface of the muscle (Fig. 2.23). Proprioceptive fibers from trapezius pass in the branches of the cervical plexus and enter the spinal cord at spinal cord levels C3 and C4.
Fig. 2.23 Innervation and blood supply of trapezius.
The blood supply to trapezius is from the superficial branch of the transverse cervical artery (Fig. 2.23), the acromial branch of the suprascapular artery, and dorsal branches of posterior intercostal arteries.
Latissimus dorsi
Latissimus dorsi is a large, flat triangular muscle that begins in the lower portion of the back and tapers as it ascends to a narrow tendon that attaches to the humerus anteriorly (Table 2.1, Figs. 2.22).
Levator scapulae
Levator scapulae is a slender muscle that descends from the transverse processes of the upper cervical vertebrae to the upper portion of the scapula on its medial border at the superior angle (Table 2.1, Fig. 2.22). It is innervated by branches from the anterior rami of spinal nerves C3 and C4 and the dorsal scapular nerve, and its arterial supply consists of branches primarily from the transverse and ascending cervical arteries.
Rhomboid minor and rhomboid major
The two rhomboid muscles are inferior to levator scapulae (Table 2.1, Fig. 2.22).
The two rhomboid muscles work together to retract or pull the scapula toward the vertebral column. The dorsal scapular nerve, a branch of the brachial plexus, innervates both rhomboid muscles (Fig. 2.24).
Fig. 2.24 Innervation and blood supply of the rhomboid muscles.
An injury to the dorsal scapular nerve, which innervates the rhomboids, may result in a lateral shift in the position of the scapula on the affected side (i.e., the normal position of the scapula is lost because of the affected muscle’s inability to prevent antagonistic muscles from pulling the scapula laterally).
Nerve injuries affecting superficial back muscles
Weakness in the trapezius, caused by an interruption of the accessory nerve [XI], may appear as drooping of the shoulder, inability to raise the arm above the head because of impaired rotation of the scapula, or weakness in attempting to raise the shoulder (i.e., shrug the shoulder against resistance).
A weakness in, or an inability to use, the latissimus dorsi, resulting from an injury to the thoracodorsal nerve, diminishes the capacity to pull the body upward while climbing or doing a pull-up.
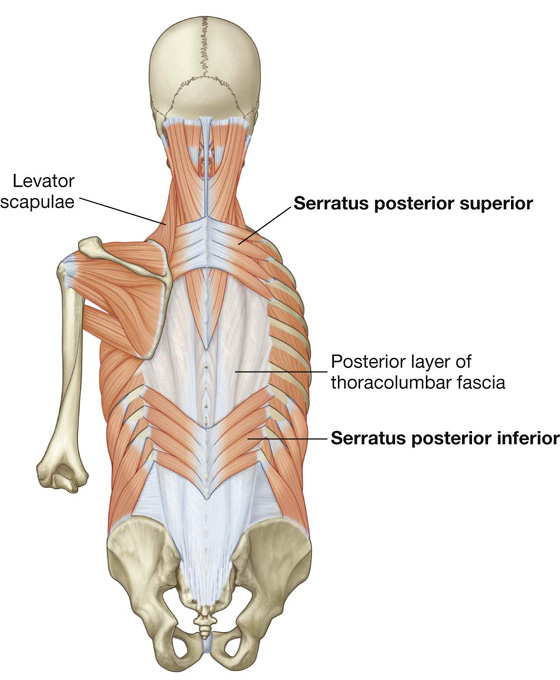
Intermediate group of back muscles
The muscles in the intermediate group of back muscles consist of two thin muscular sheets in the superior and inferior regions of the back, immediately deep to the muscles in the superficial group (Table 2.2, Fig. 2.25). Fibers from these two serratus posterior muscles (serratus posterior superior and serratus posterior inferior) pass obliquely outward from the vertebral column to attach to the ribs. This positioning suggests a respiratory function, and at times, these muscles have been referred to as the respiratory group.
Table 2.2 Intermediate (respiratory) group of back muscles
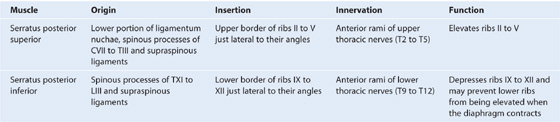
Fig. 2.25 Intermediate group of back muscles—serratus posterior muscles.
Serratus posterior superior is deep to the rhomboid muscles, whereas serratus posterior inferior is deep to the latissimus dorsi. They are innervated by segmental branches of the anterior rami of intercostal nerves. Their vascular supply is provided by a similar segmental pattern through the intercostal arteries.
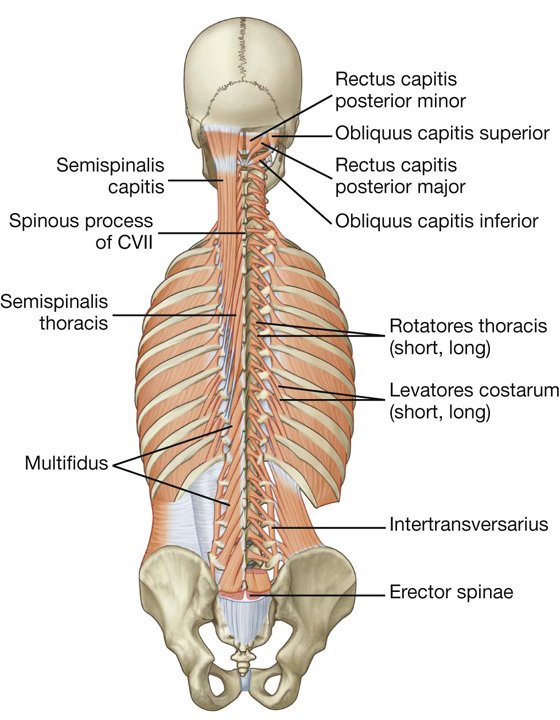
Deep group of back muscles
The deep or intrinsic muscles of the back extend from the pelvis to the skull and are innervated by segmental branches of the posterior rami of spinal nerves. Muscles in this group include the spinotransversales, erector spinae, transversospinales, segmental, and suboccipital muscles.
Spinotransversales muscles
The two spinotransversales muscles run from the spinous processes and ligamentum nuchae upward and laterally (Table 2.3, Fig. 2.26):
Table 2.3 Spinotransversales muscles
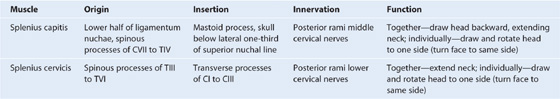
Fig. 2.26 Deep group of back muscles—spinotransversales muscles (splenius capitis and splenius cervicis).
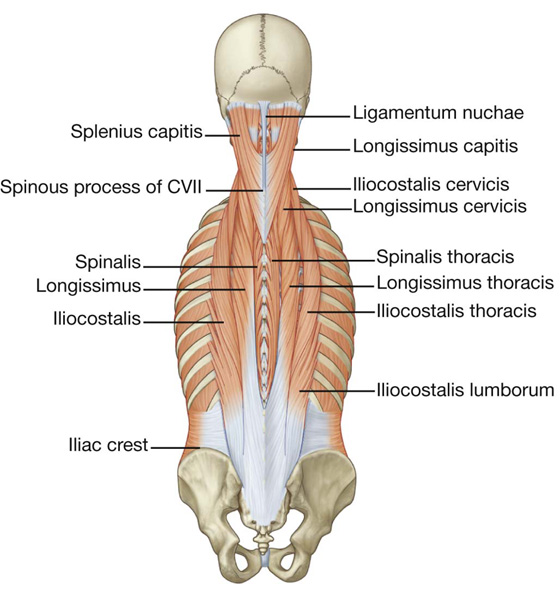
Erector spinae muscles
The erector spinae is the largest group of intrinsic back muscles. The muscles lie posterolaterally to the vertebral column between the spinous processes medially and the angles of the ribs laterally (Table 2.4, Fig. 2.27). In the upper lumbar region, the erector spinae divides into three vertical columns of muscle, each of which is further subdivided regionally (lumborum, thoracis, cervicis, and capitis), depending on where the muscles attach superiorly.
Table 2.4 Erector spinae group of back muscles
|
Muscle |
Origin |
Insertion |
|
Iliocostalis lumborum |
Sacrum, spinous processes of lumbar and lower two thoracic vertebrae and their supraspinous ligaments, and the iliac crest |
Angles of the lower six or seven ribs |
|
Iliocostalis thoracis |
Angles of the lower six ribs |
Angles of the upper six ribs and the transverse process of CVII |
|
Iliocostalis cervicis |
Angles of ribs III to VI |
Transverse processes of CIV to CVI |
|
Longissimus thoracis |
Blends with iliocostalis in lumbar region and is attached to transverse processes of lumbar vertebrae |
Transverse processes of all thoracic vertebrae and just lateral to the tubercles of the lower nine or ten ribs |
|
Longissimus cervicis |
Transverse processes of upper four or five thoracic vertebrae |
Transverse processes of CII to CVI |
|
Longissimus capitis |
Transverse processes of upper four or five thoracic vertebrae and articular processes of lower three or four cervical vertebrae |
Posterior margin of the mastoid process |
|
Spinalis thoracis |
Spinous processes of TX or TXI to LII |
Spinous processes of TI to TVIII (varies) |
|
Spinalis cervicis |
Lower part of ligamentum nuchae and spinous process of CVII (sometimes TI to TII) |
Spinous process of CII (axis) |
|
Spinalis capitis |
Usually blends with semispinalis capitis |
With semispinalis capitis |
Fig. 2.27 Deep group of back muscles—erector spinae muscles.
 The outer or most laterally placed column of the erector spinae muscles is the iliocostalis.
The outer or most laterally placed column of the erector spinae muscles is the iliocostalis.
 The middle or intermediate column is the longissimus.
The middle or intermediate column is the longissimus.
 The most medial muscle column is the spinalis.
The most medial muscle column is the spinalis.
The muscles in the erector spinae group are the primary extensors of the vertebral column and head. Acting bilaterally, they straighten the back, returning it to the upright position from a flexed position, and pull the head posteriorly. They also participate in controlling vertebral column flexion by contracting and relaxing in a coordinated fashion. Acting unilaterally, they bend the vertebral column laterally. In addition, unilateral contractions of muscles attached to the head turn the head to the actively contracting side.
Transversospinales muscles
The transversospinales muscles run obliquely upward and medially from transverse processes to spinous processes, filling the groove between these two vertebral projections (Table 2.5, Fig. 2.28). They are deep to the erector spinae and consist of three major subgroups—the semispinalis, multifidus, and rotatores muscles.
Table 2.5 Transversospinales group of back muscles
|
Muscle |
Origin |
Insertion |
|
Semispinalis thoracis |
Transverse processes of TVI to TX |
Spinous processes of upper four thoracic and lower two cervical vertebrae |
|
Semispinalis cervicis |
Transverse processes of upper five or six thoracic vertebrae |
Spinous processes of CII (axis) to CV |
|
Semispinalis capitis |
Transverse processes of TI to TVI (or TVII) and CVII and articular processes of CIV to CVI |
Medial area between the superior and inferior nuchal lines of occipital bone |
|
Multifidus |
Sacrum, origin of erector spinae, posterior superior iliac spine, mammillary processes of lumbar vertebrae, transverse processes of thoracic vertebrae, and articular processes of lower four cervical vertebrae |
Base of spinous processes of all vertebrae from LV to CII (axis) |
|
Rotatores lumborum |
Mammillary processes of lumbar vertebrae |
Spinous processes of lumbar vertebrae |
|
Rotatores thoracis |
Transverse processes of thoracic vertebrae |
Spinous processes of thoracic vertebrae |
|
Rotatores cervicis |
Articular processes of cervical vertebrae |
Spinous processes of cervical vertebrae |
Fig. 2.28 Deep group of back muscles—transversospinales and segmental muscles.
When muscles in the transversospinales group contract bilaterally, they extend the vertebral column, an action similar to that of the erector spinae group. However, when muscles on only one side contract, they pull the spinous processes toward the transverse processes on that side, causing the trunk to turn or rotate in the opposite direction.
One muscle in the transversospinales group, the semispinalis capitis, has a unique action because it attaches to the skull. Contracting bilaterally, this muscle pulls the head posteriorly, whereas unilateral contraction pulls the head posteriorly and turns it, causing the chin to move superiorly and turn toward the side of the contracting muscle.
Segmental muscles
The two groups of segmental muscles (Table 2.6, Fig. 2.28) are deeply placed in the back and innervated by posterior rami of spinal nerves.
 The first group of segmental muscles are the levatores costarum muscles.
The first group of segmental muscles are the levatores costarum muscles.
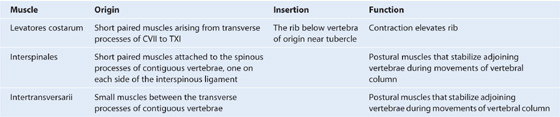
Table 2.6 Segmental back muscles
Suboccipital muscles
A small group of deep muscles in the upper cervical region at the base of the occipital bone move the head. Because of their location they are sometimes referred to as suboccipital muscles (Table 2.7, Figs. 2.28, 2.29). They include, on each side:
 rectus capitis posterior major,
rectus capitis posterior major,
 rectus capitis posterior minor,
rectus capitis posterior minor,
 obliquus capitis inferior, and
obliquus capitis inferior, and
Table 2.7 Suboccipital group of back muscles
Contraction of the suboccipital muscles extends the head at the atlantoaxial joint.
The suboccipital muscles are innervated by the posterior ramus of the first cervical nerve, which enters the area between the vertebral artery and the posterior arch of the atlas (Fig. 2.29). The vascular supply to the muscles in this area is from branches of the vertebral and occipital arteries.
The suboccipital muscles form the boundaries of the suboccipital triangle, an area that contains several important structures (Fig. 2.29):
 Rectus capitis posterior major forms the medial border of the triangle.
Rectus capitis posterior major forms the medial border of the triangle.
 Obliquus capitis superior muscle forms the lateral border.
Obliquus capitis superior muscle forms the lateral border.
 Obliquus capitis inferior muscle forms the inferior border.
Obliquus capitis inferior muscle forms the inferior border.
The contents of the area outlined by these muscles are the posterior ramus of C1, the vertebral artery, and associated veins.
Thoracolumbar fascia
The thoracolumbar fascia covers the deep muscles of the back and trunk (Fig. 2.30). This fascial layer is critical to the overall organization and integrity of the region:
Fig. 2.30 Thoracolumbar fascia and the deep back muscles (transverse section).
In the lumbar region, the thoracolumbar fascia consists of three layers:
 The middle layer is attached medially to the tips of the transverse processes of the lumbar vertebrae and intertransverse ligaments—inferiorly, it is attached to the iliac crest and, superiorly, to the lower border of rib XII.
The middle layer is attached medially to the tips of the transverse processes of the lumbar vertebrae and intertransverse ligaments—inferiorly, it is attached to the iliac crest and, superiorly, to the lower border of rib XII.
The posterior and middle layers of the thoracolumbar fascia come together at the lateral margin of the erector spinae (Fig. 2.30). At the lateral border of the quadratus lumborum, the anterior layer joins them and forms the aponeurotic origin for the transversus abdominis muscle of the abdominal wall.
SPINAL CORD
The spinal cord extends from the foramen magnum to approximately the level of the disc between vertebrae LI and LII in adults, although it can end as high as vertebra TXII or as low as the disc between vertebrae LII and LIII (Fig. 2.31). In neonates, the spinal cord extends approximately to vertebra LIII, but can reach as low as vertebra LIV. The distal end of the cord (the conus medullaris) is cone shaped. A fine filament of connective tissue (the pial part of the filum terminale) continues inferiorly from the apex of the conus medullaris.
Fig. 2.31 Spinal cord.
The spinal cord is not uniform in diameter along its length. It has two major swellings or enlargements in regions associated with the origin of spinal nerves that innervate the upper and lower limbs. A cervical enlargement occurs in the region associated with the origins of spinal nerves C5 to T1, which innervate the upper limbs. A lumbosacral enlargement occurs in the region associated with the origins of spinal nerves L1 to S3, which innervate the lower limbs (Fig. 2.31).
The external surface of the spinal cord is marked by a number of fissures and sulci (Fig. 2.32):
 The anterior median fissure extends the length of the anterior surface.
The anterior median fissure extends the length of the anterior surface.
 The posterior median sulcus extends along the posterior surface.
The posterior median sulcus extends along the posterior surface.
Fig. 2.32 Features of the spinal cord.
Internally, the cord has a small central canal surrounded by gray and white matter (Fig. 2.32):
Vasculature
Arteries
The arterial supply to the spinal cord comes from two sources (Fig. 2.33A). It consists of:
After entering an intervertebral foramen, the segmental spinal arteries give rise to anterior and posterior radicular arteries (Fig. 2.33). This occurs at every vertebral level. The radicular arteries follow, and supply, the anterior and posterior roots. At various vertebral levels, the segmental spinal arteries also give off segmental medullary arteries (Fig. 2.33B). These vessels pass directly to the longitudinally oriented vessels, reinforcing these.
The longitudinal vessels consist of:
The anterior and posterior spinal arteries are reinforced along their length by 8 to 10 segmental medullary arteries (Fig. 2.33). The largest of these is the arteria radicularis magna or the artery of Adamkiewicz (Fig. 2.33A). This vessel arises in the lower thoracic or upper lumbar region, usually on the left side, and reinforces the arterial supply to the lower portion of the spinal cord, including the lumbar enlargement.
Veins
Veins that drain the spinal cord form a number of longitudinal channels (Fig. 2.34):
 one midline channel parallels the anterior median fissure;
one midline channel parallels the anterior median fissure;
 one midline channel passes along the posterior median sulcus.
one midline channel passes along the posterior median sulcus.
Fig. 2.34 Veins that drain the spinal cord.
These longitudinal channels drain into an extensive internal vertebral plexus in the extradural (epidural) space of the vertebral canal, which then drains into segmentally arranged vessels that connect with major systemic veins, such as the azygos system in the thorax. The internal vertebral venous plexus also communicates with intracranial veins.
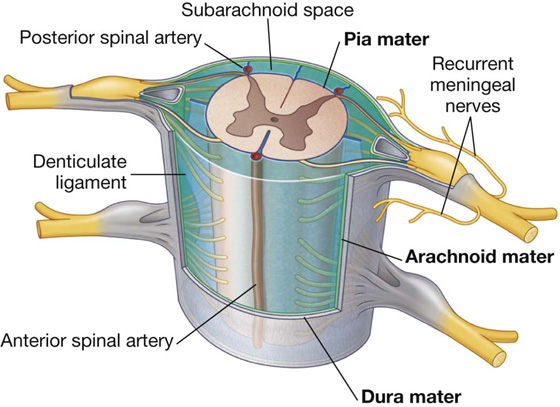
Meninges
Spinal dura mater
The spinal dura mater (Fig. 2.35) is the outermost meningeal membrane and is separated from the bones forming the vertebral canal by an extradural (epidural) space. Superiorly, it is continuous with the inner meningeal layer of cranial dura mater at the foramen magnum of the skull. Inferiorly, the dural sac dramatically narrows at the level of the lower border of vertebra SII and forms an investing sheath for the pial part of the filum terminale of the spinal cord. This terminal cordlike extension of dura mater (the dural part of the filum terminale) attaches to the posterior surface of the vertebral bodies of the coccyx.
Fig. 2.35 Meninges.
As spinal nerves and their roots pass laterally, they are surrounded by tubular sleeves of dura mater, which merge with and become part of the outer covering (epineurium) of the nerves.
Arachnoid mater
The arachnoid mater is a thin delicate membrane against, but not adherent to, the deep surface of the dura mater (Fig. 2.35). It is separated from the pia mater by the subarachnoid space. The arachnoid mater ends at the level of vertebra SII (see Fig. 2.31).
Subarachnoid space
The subarachnoid space between the arachnoid and pia mater contains cerebrospinal fluid (CSF) (Fig. 2.35). The subarachnoid space around the spinal cord is continuous at the foramen magnum with the subarachnoid space surrounding the brain. Inferiorly, the subarachnoid space terminates at approximately the level of the lower border of vertebra SII (see Fig. 2.31).
Delicate strands of tissue (arachnoid trabeculae) are continuous with the arachnoid mater on one side and the pia mater on the other, span the subarachnoid space, and interconnect the two adjacent membranes. Large blood vessels are suspended in the subarachnoid space by similar strands of material, which expand over the vessels to form a continuous external coat.
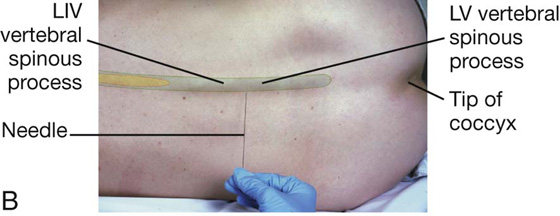
The subarachnoid space extends further inferiorly than the spinal cord. The spinal cord ends at approximately the disc between vertebrae LI and LII, whereas the subarachnoid space extends to approximately the lower border of vertebra SII (see Fig. 2.31). The subarachnoid space is largest in the region inferior to the terminal end of the spinal cord where it surrounds the cauda equina. As a consequence, CSF can be withdrawn from the subarachnoid space in the lower lumbar region without endangering the spinal cord (Fig. 2.36).
Surface anatomy
Visualizing the inferior ends of the spinal cord and subarachnoid space
The spinal cord does not occupy the entire length of the vertebral canal. Normally in adults, it terminates at the level of the disc between vertebrae LI and LII; however, it may end as high as TXII or as low as the disc between vertebrae LII and LIII. The subarachnoid space ends at approximately the level of vertebra SII (Fig. 2.36A).
Because the subarachnoid space can be accessed in the lower lumbar region without endangering the spinal cord, it is important to be able to identify the position of the lumbar vertebral spinous processes. The LIV vertebral spinous process is level with a horizontal line between the highest points on the iliac crests. In the lumbar region, the palpable ends of the vertebral spinous processes lie opposite their corresponding vertebral bodies. The subarachnoid space can be accessed between vertebral levels LIII and LIV and between LIV and LV without endangering the spinal cord (Fig. 2.36B). The subarachnoid space ends at vertebral level SII, which is level with the sacral dimples marking the posterior superior iliac spines.
Pia mater
The spinal pia mater is a vascular membrane that firmly adheres to the surface of the spinal cord (Fig. 2.35). It extends into the anterior median fissure and reflects as sleevelike coatings onto posterior and anterior rootlets and roots as they cross the subarachnoid space. As the roots exit the space, the sleevelike coatings reflect onto the arachnoid mater.
On each side of the spinal cord, a longitudinally oriented sheet of pia mater (the denticulate ligament) extends laterally from the cord toward the arachnoid and dura mater (Fig. 2.35).
The denticulate ligaments generally occur between the exit points of adjacent posterior and anterior rootlets and position the spinal cord in the center of the subarachnoid space.
Arrangement of structures in the vertebral canal
The vertebral canal is bordered:
 anteriorly by the bodies of the vertebrae, intervertebral discs, and the posterior longitudinal ligament (Fig. 2.37);
anteriorly by the bodies of the vertebrae, intervertebral discs, and the posterior longitudinal ligament (Fig. 2.37);
Fig. 2.37 Arrangement of structures in the vertebral canal and the back.
 laterally, on each side by the pedicles and intervertebral foramina; and
laterally, on each side by the pedicles and intervertebral foramina; and
Between the walls of the vertebral canal and the dural sac is an extradural space containing a vertebral plexus of veins embedded in fatty connective tissue.
Spinal nerves
Each spinal nerve is connected to the spinal cord by posterior and anterior roots (Fig. 2.38):
Fig. 2.38 Basic organization of a spinal nerve.
Medially, the posterior and anterior roots divide into rootlets, which attach to the spinal cord.
A spinal segment is the area of the spinal cord that gives rise to the posterior and anterior rootlets, which will form a single pair of spinal nerves. Laterally, the posterior and anterior roots on each side join to form a spinal nerve.
Each spinal nerve divides, as it emerges from an intervertebral foramen, into two major branches: a small posterior ramus and a much larger anterior ramus (Fig. 2.38):
 The posterior rami innervate only intrinsic back muscles (the epaxial muscles) and an associated narrow strip of skin on the back.
The posterior rami innervate only intrinsic back muscles (the epaxial muscles) and an associated narrow strip of skin on the back.
Near the point of division into anterior and posterior rami, each spinal nerve gives rise to two to four small recurrent meningeal (sinuvertebral) nerves (see Fig. 2.35). These nerves reenter the intervertebral foramen to supply dura, ligaments, intervertebral discs, and blood vessels.
All major somatic plexuses (cervical, brachial, lumbar, and sacral) are formed by anterior rami.
Because the spinal cord is much shorter than the vertebral column, the roots of spinal nerves become longer and pass more obliquely from the cervical to coccygeal regions of the vertebral canal (Fig. 2.39).
Fig. 2.39 Course of spinal nerves in the vertebral canal.
In adults, the spinal cord terminates at a level approximately between vertebrae LI and LII, but this can range between vertebra TXII and the disc between vertebrae LII and LIII. Consequently, posterior and anterior roots forming spinal nerves emerging between vertebrae in the lower regions of the vertebral column are connected to the spinal cord at higher vertebral levels.
Below the end of the spinal cord, the posterior and anterior roots of lumbar, sacral, and coccygeal nerves pass inferiorly to reach their exit points from the vertebral canal. This terminal cluster of roots is the cauda equine (Fig. 2.39).
Clinical app
Lumbar cerebrospinal fluid tap
A lumbar tap (puncture) is carried out to obtain a sample of CSF for examination. In addition, passage of a needle or conduit into the subarachnoid space (CSF space) is used to inject antibiotics, chemotherapeutic agents, and anesthetics. The lumbar region is an ideal site to access the subarachnoid space because the spinal cord terminates around the level of the disc between vertebrae LI and LII in the adult. The subarachnoid space extends to the region of the lower border of the SII vertebra. There is therefore a large CSF-filled space containing lumbar and sacral nerve roots, but no spinal cord.
Depending on the clinician’s preference, the patient is placed in the lateral or prone position. A needle is passed in the midline in between the spinous processes into the extradural space. Further advancement punctures the dura and arachnoid mater to enter the subarachnoid space. Most needles push the roots away from the tip without causing the patient any symptoms. Once the needle is in the subarachnoid space, fluid can be aspirated. In some situations, it is important to measure CSF pressure.
Clinical app
Anesthesia within the vertebral canal
Local anesthetics can be injected into the extradural space (extradural or epidural anesthesia) or the subarachnoid space (spinal anesthesia) in the lower lumbar region to anesthetize the sacral and lumbar nerve roots. Such anesthesia is useful for operations on the pelvis and the legs, which can then be carried out without the need for general anesthesia.
When doing epidural anesthesia, a needle is placed through the skin, supraspinous ligament, interspinous ligament, and ligamenta flava into the areolar tissue and fat around the dura mater. Anesthetic agent is introduced and diffuses around the vertebral canal to anesthetize the exiting nerve roots.
In spinal anesthesia, the needle continues through the dura and associated arachnoid into the subarachnoid space to directly anesthetize the nerve roots.
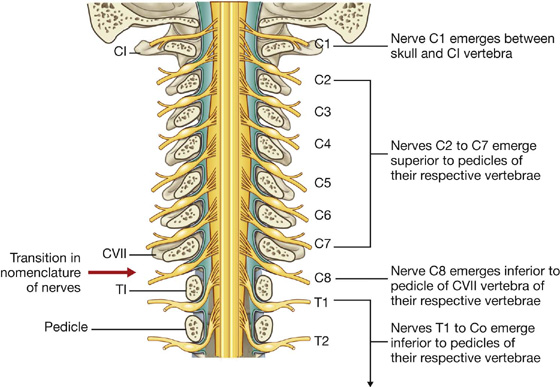
Nomenclature of spinal nerves
There are approximately 31 pairs of spinal nerves (Fig. 2.39), named according to their position with respect to associated vertebrae:
 eight cervical nerves—C1 to C8,
eight cervical nerves—C1 to C8,
 twelve thoracic nerves—T1 to T12,
twelve thoracic nerves—T1 to T12,
 five sacral nerves—S1 to S5, and
five sacral nerves—S1 to S5, and
The first cervical nerve (C1) emerges from the vertebral canal between the skull and vertebra CI (Fig. 2.40). Therefore cervical nerves C2 to C7 also emerge from the vertebral canal above their respective vertebrae. Because there are only seven cervical vertebrae, C8 emerges between vertebrae CVII and TI. As a consequence, all remaining spinal nerves, beginning with T1, emerge from the vertebral canal below their respective vertebrae.
Fig. 2.40 Nomenclature of the spinal nerves.
Clinical app
Herpes zoster
Herpes zoster is the virus that produces chickenpox in children. In some patients the virus remains dormant in the cells of the spinal ganglia. Under certain circumstances, the virus becomes activated and travels along the neuronal bundles to the areas supplied by that nerve (the dermatome). A rash ensues, which is characteristically exquisitely painful.

 PT Case Studies
PT Case Studies Medical Clinical Case Studies
Medical Clinical Case Studies Clinical Cases
Clinical Cases Next are five sacral vertebrae fused into one single bone called the sacrum, which articulates on each side with a pelvic bone and is a component of the pelvic wall.
Next are five sacral vertebrae fused into one single bone called the sacrum, which articulates on each side with a pelvic bone and is a component of the pelvic wall.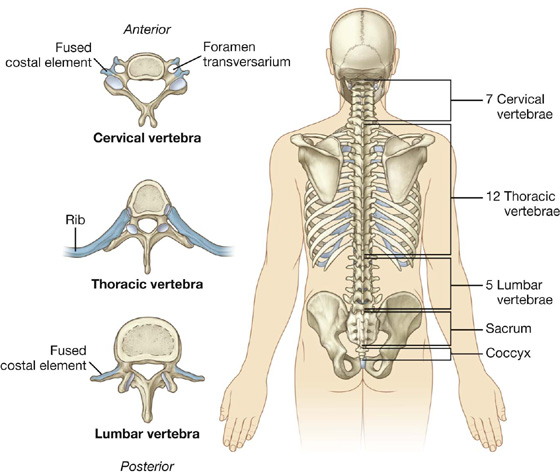

 The vertebral body is short in height and square shaped when viewed from above and has a concave superior surface and a convex inferior surface.
The vertebral body is short in height and square shaped when viewed from above and has a concave superior surface and a convex inferior surface.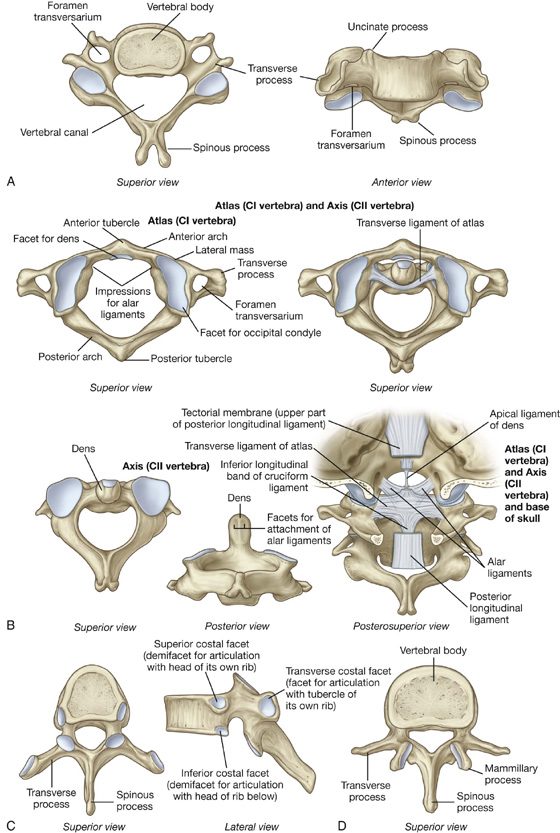
 The primary curvature of the vertebral column is concave anteriorly, reflecting the original shape of the embryo, and is retained in the thoracic and sacral regions in adults.
The primary curvature of the vertebral column is concave anteriorly, reflecting the original shape of the embryo, and is retained in the thoracic and sacral regions in adults. Secondary curvatures, which are concave posteriorly, form in the cervical and lumbar regions and bring the center of gravity into a vertical line, which allows the body’s weight to be balanced on the vertebral column in a way that expends the least amount of muscular energy to maintain an upright bipedal stance.
Secondary curvatures, which are concave posteriorly, form in the cervical and lumbar regions and bring the center of gravity into a vertical line, which allows the body’s weight to be balanced on the vertebral column in a way that expends the least amount of muscular energy to maintain an upright bipedal stance.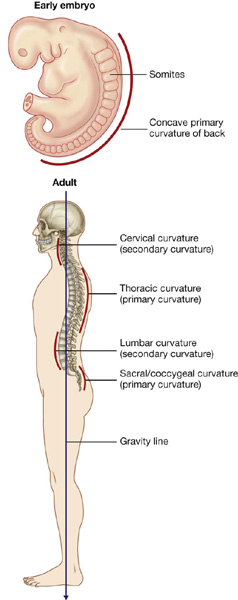
 The more severe form of spina bifida involves complete failure of fusion of the posterior arch at the lumbosacral junction with a large outpouching of the meninges. This may contain cerebrospinal fluid (a meningocele) or a portion of the spinal cord (a myelomeningocele). These abnormalities may result in a variety of neurological deficits, including problems with walking and bladder function.
The more severe form of spina bifida involves complete failure of fusion of the posterior arch at the lumbosacral junction with a large outpouching of the meninges. This may contain cerebrospinal fluid (a meningocele) or a portion of the spinal cord (a myelomeningocele). These abnormalities may result in a variety of neurological deficits, including problems with walking and bladder function.
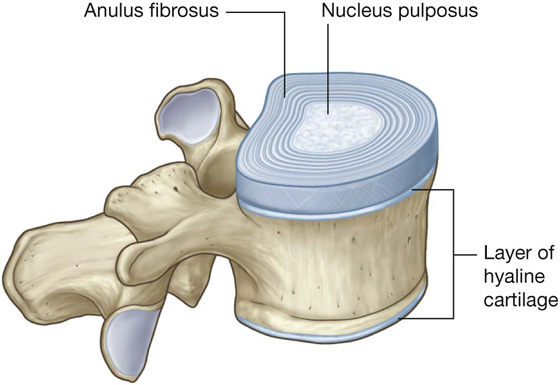
 The anulus fibrosus consists of an outer ring of collagen surrounding a wider zone of fibrocartilage arranged in a lamellar configuration. This arrangement of fibers limits rotation between vertebrae.
The anulus fibrosus consists of an outer ring of collagen surrounding a wider zone of fibrocartilage arranged in a lamellar configuration. This arrangement of fibers limits rotation between vertebrae. The nucleus pulposus fills the center of the intervertebral disc, is gelatinous, and absorbs compression forces between vertebrae.
The nucleus pulposus fills the center of the intervertebral disc, is gelatinous, and absorbs compression forces between vertebrae.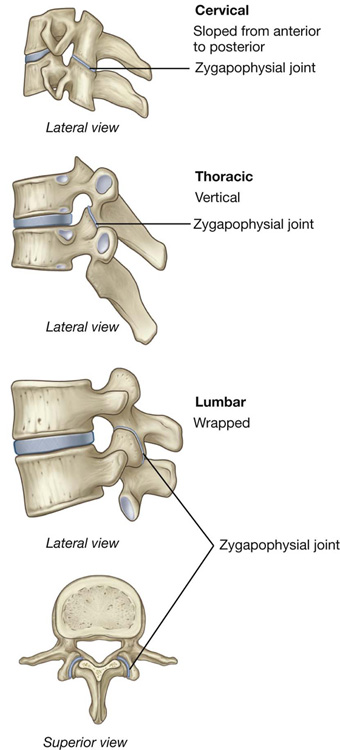
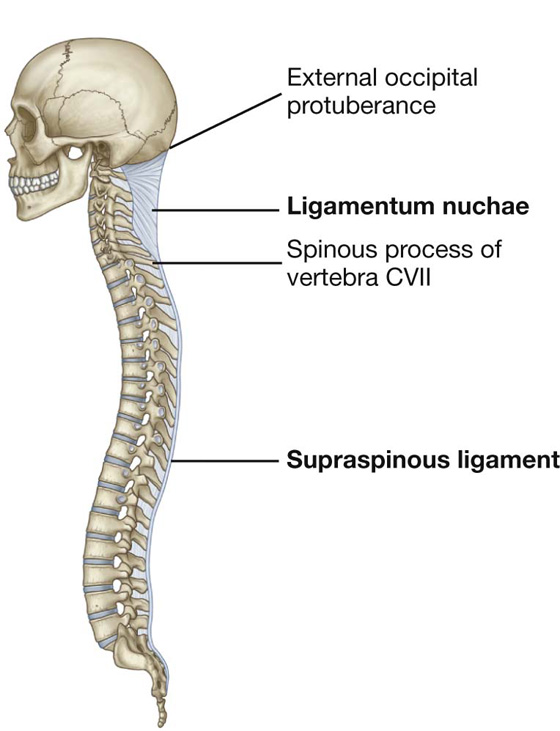
 The base of the triangle is attached to the skull, from the external occipital protuberance to the foramen magnum.
The base of the triangle is attached to the skull, from the external occipital protuberance to the foramen magnum. The deep side of the triangle is attached to the posterior tubercle of vertebra CI and the spinous processes of the other cervical vertebrae.
The deep side of the triangle is attached to the posterior tubercle of vertebra CI and the spinous processes of the other cervical vertebrae.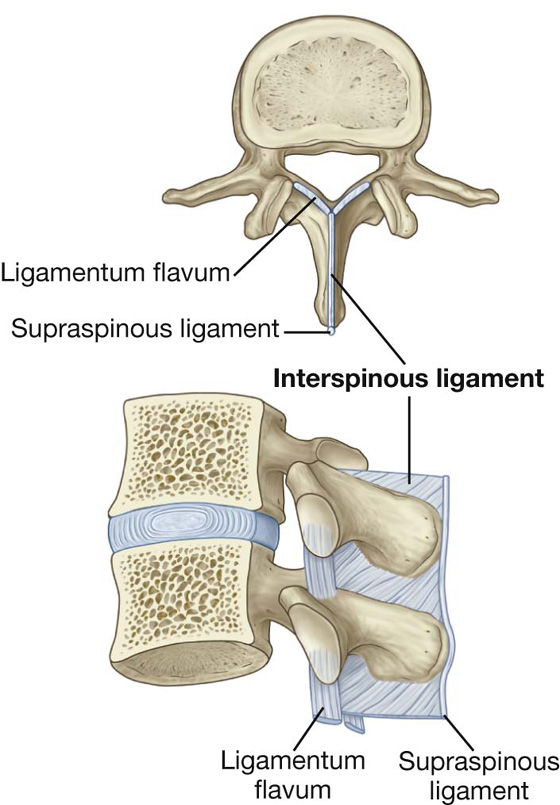
 The intermediate group consists of muscles attached to the ribs and may serve a respiratory function.
The intermediate group consists of muscles attached to the ribs and may serve a respiratory function.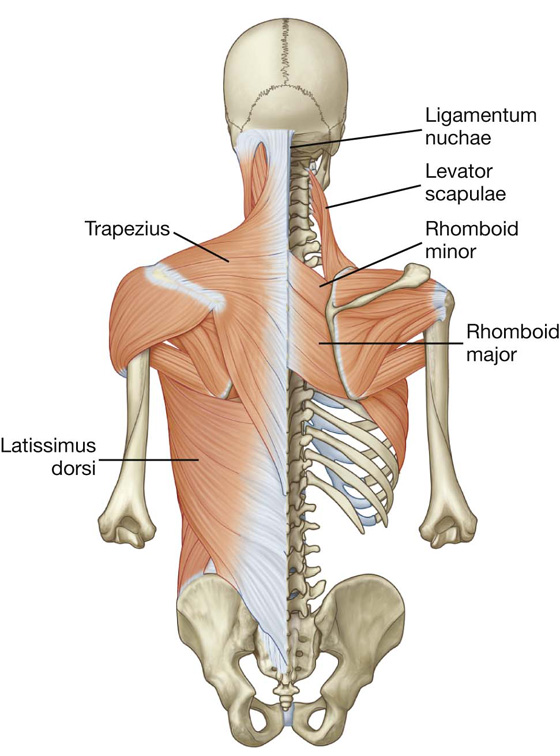
 Splenius capitis is a broad muscle attached to the occipital bone and mastoid process of the temporal bone.
Splenius capitis is a broad muscle attached to the occipital bone and mastoid process of the temporal bone. Splenius cervicis is a narrow muscle attached to the transverse processes of the upper cervical vertebrae.
Splenius cervicis is a narrow muscle attached to the transverse processes of the upper cervical vertebrae.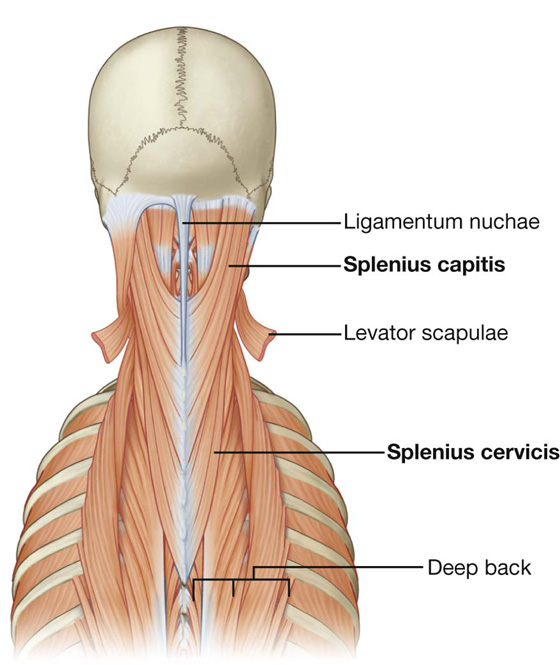
 The semispinalis muscles are the most superficial collection of muscle fibers in the transversospinales group. They begin in the lower thoracic region and end by attaching to the skull, crossing between four and six vertebrae.
The semispinalis muscles are the most superficial collection of muscle fibers in the transversospinales group. They begin in the lower thoracic region and end by attaching to the skull, crossing between four and six vertebrae. Deep to the semispinalis is the second group of muscles, the multifidus. Muscles in this group span the length of the vertebral column spanning between two and four vertebrae.
Deep to the semispinalis is the second group of muscles, the multifidus. Muscles in this group span the length of the vertebral column spanning between two and four vertebrae. The small rotatores muscles are the deepest of the transversospinales group and span the length of the vertebral column, crossing two vertebrae (long rotators) or attaching to adjacent vertebra (short rotators).
The small rotatores muscles are the deepest of the transversospinales group and span the length of the vertebral column, crossing two vertebrae (long rotators) or attaching to adjacent vertebra (short rotators). The second group of segmental muscles are the true segmental muscles of the back—the interspinales and the intertransversarii.
The second group of segmental muscles are the true segmental muscles of the back—the interspinales and the intertransversarii. obliquus capitis superior.
obliquus capitis superior.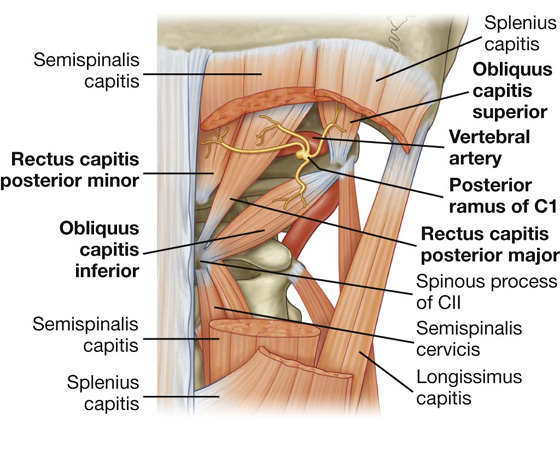
 Superiorly, it passes anteriorly to the serratus posterior superior muscle and is continuous with deep fascia in the neck.
Superiorly, it passes anteriorly to the serratus posterior superior muscle and is continuous with deep fascia in the neck. In the thoracic region, it covers the deep muscles and separates them from the muscles in the superficial and intermediate groups.
In the thoracic region, it covers the deep muscles and separates them from the muscles in the superficial and intermediate groups. Medially, it attaches to the spinous processes of the thoracic vertebrae and, laterally, to the angles of the ribs.
Medially, it attaches to the spinous processes of the thoracic vertebrae and, laterally, to the angles of the ribs.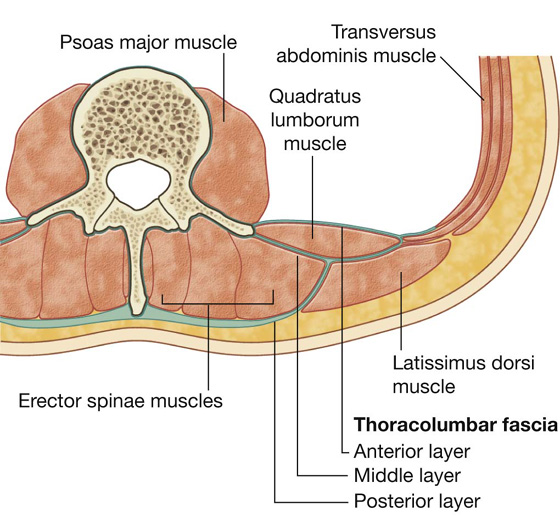
 The posterior layer is thick and is attached to the spinous processes of the lumbar vertebrae, sacral vertebrae, and the supraspinous ligament—from these attachments, it extends laterally to cover the erector spinae.
The posterior layer is thick and is attached to the spinous processes of the lumbar vertebrae, sacral vertebrae, and the supraspinous ligament—from these attachments, it extends laterally to cover the erector spinae. The anterior layer covers the anterior surface of the quadratus lumborum muscle (a muscle of the posterior abdominal wall) and is attached medially to the transverse processes of the lumbar vertebrae—inferiorly, it is attached to the iliac crest and, superiorly, it forms the lateral arcuate ligament for attachment of the diaphragm.
The anterior layer covers the anterior surface of the quadratus lumborum muscle (a muscle of the posterior abdominal wall) and is attached medially to the transverse processes of the lumbar vertebrae—inferiorly, it is attached to the iliac crest and, superiorly, it forms the lateral arcuate ligament for attachment of the diaphragm.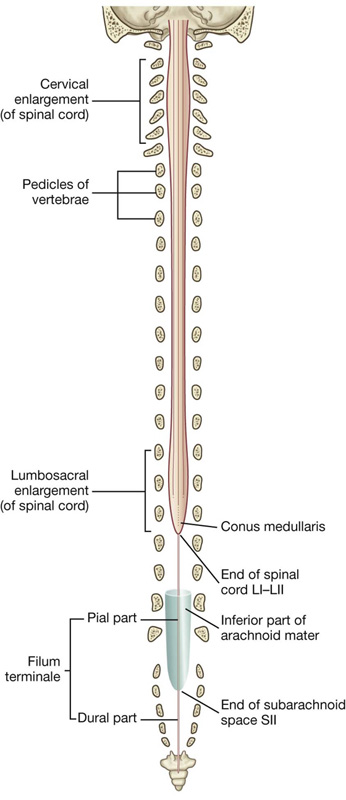
 The posterolateral sulcus on each side of the posterior surface marks where the posterior rootlets of spinal nerves enter the cord.
The posterolateral sulcus on each side of the posterior surface marks where the posterior rootlets of spinal nerves enter the cord.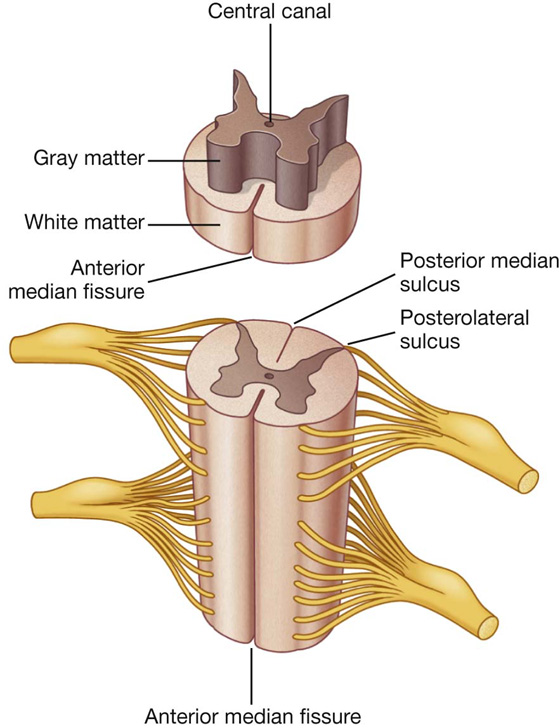
 The gray matter is rich in nerve cell bodies, which form longitudinal columns along the cord, and in cross-section these columns form a characteristic H-shaped appearance in the central regions of the cord.
The gray matter is rich in nerve cell bodies, which form longitudinal columns along the cord, and in cross-section these columns form a characteristic H-shaped appearance in the central regions of the cord. The white matter surrounds the gray matter and is rich in nerve cell processes, which form large bundles or tracts that ascend and descend in the cord to other spinal cord levels or carry information to and from the brain.
The white matter surrounds the gray matter and is rich in nerve cell processes, which form large bundles or tracts that ascend and descend in the cord to other spinal cord levels or carry information to and from the brain. longitudinally oriented vessels, arising superior to the cervical portion of the cord, which descend on the surface of the cord; and
longitudinally oriented vessels, arising superior to the cervical portion of the cord, which descend on the surface of the cord; and feeder arteries that enter the vertebral canal through the intervertebral foramina at every level; these feeder vessels, or segmental spinal arteries, arise predominantly from the vertebral and deep cervical arteries in the neck, the posterior intercostal arteries in the thorax, and the lumbar arteries in the abdomen.
feeder arteries that enter the vertebral canal through the intervertebral foramina at every level; these feeder vessels, or segmental spinal arteries, arise predominantly from the vertebral and deep cervical arteries in the neck, the posterior intercostal arteries in the thorax, and the lumbar arteries in the abdomen.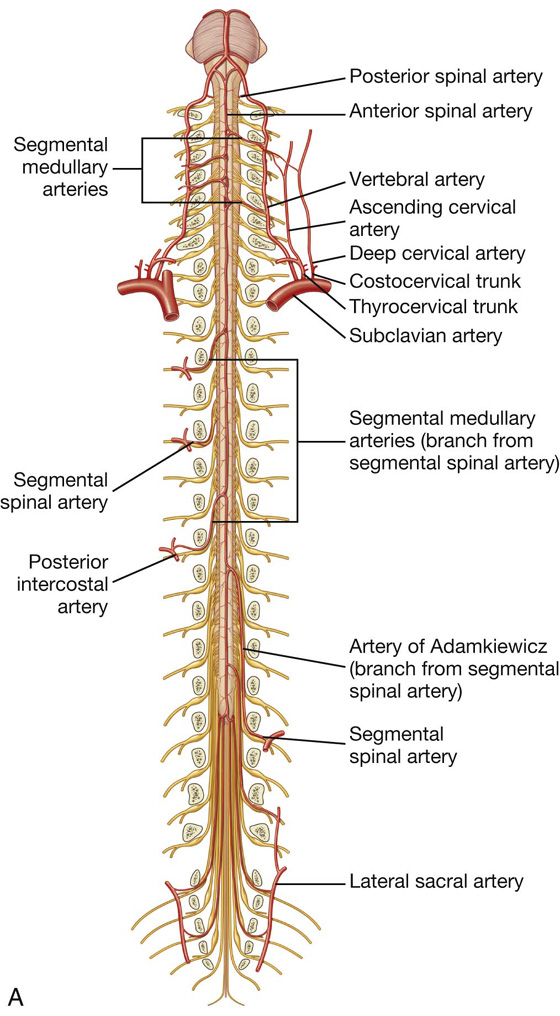
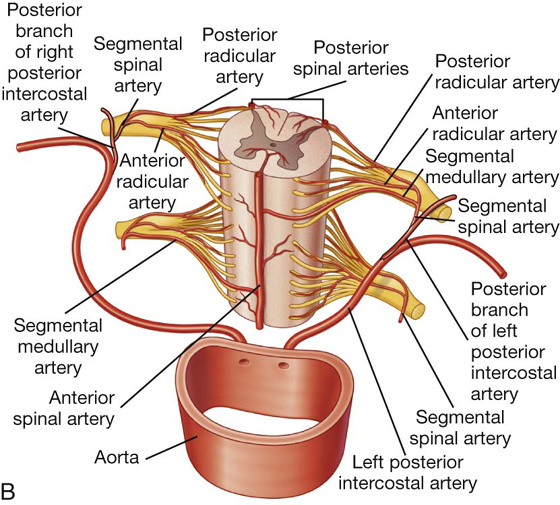
 a single anterior spinal artery, which originates within the cranial cavity as the union of two vessels that arise from the vertebral arteries—the resulting single anterior spinal artery passes inferiorly, approximately parallel to the anterior median fissure, along the surface of the spinal cord; and
a single anterior spinal artery, which originates within the cranial cavity as the union of two vessels that arise from the vertebral arteries—the resulting single anterior spinal artery passes inferiorly, approximately parallel to the anterior median fissure, along the surface of the spinal cord; and two posterior spinal arteries, which also originate in the cranial cavity, usually arising directly from a terminal branch of each vertebral artery (the posterior inferior cerebellar artery)—the right and left posterior spinal arteries descend along the spinal cord, each as two branches that bracket the posterolateral sulcus and the connection of posterior roots with the spinal cord.
two posterior spinal arteries, which also originate in the cranial cavity, usually arising directly from a terminal branch of each vertebral artery (the posterior inferior cerebellar artery)—the right and left posterior spinal arteries descend along the spinal cord, each as two branches that bracket the posterolateral sulcus and the connection of posterior roots with the spinal cord. two pairs of veins on each side bracket the connections of the posterior and anterior roots to the cord;
two pairs of veins on each side bracket the connections of the posterior and anterior roots to the cord;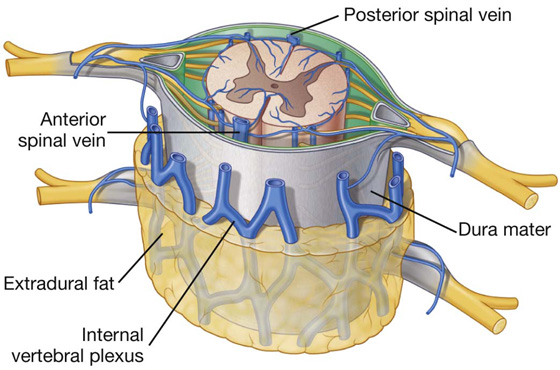
 Medially, each denticulate ligament is attached to the spinal cord in a plane that lies between the origins of the posterior and anterior rootlets.
Medially, each denticulate ligament is attached to the spinal cord in a plane that lies between the origins of the posterior and anterior rootlets. Laterally, each denticulate ligament forms a series of triangular extensions along its free border, with the apex of each extension being anchored through the arachnoid mater to the dura mater.
Laterally, each denticulate ligament forms a series of triangular extensions along its free border, with the apex of each extension being anchored through the arachnoid mater to the dura mater.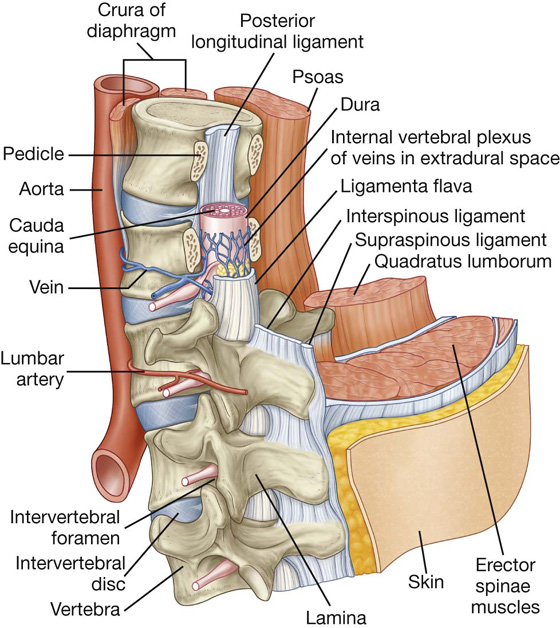
 posteriorly by the laminae and ligamenta flava, and in the median plane the roots of the interspinous ligaments and vertebral spinous processes.
posteriorly by the laminae and ligamenta flava, and in the median plane the roots of the interspinous ligaments and vertebral spinous processes. The posterior root contains the processes of sensory neurons carrying information to the CNS. The cell bodies of the sensory neurons, which are derived embryologically from neural crest cells, are clustered in a spinal ganglion at the distal end of the posterior root, usually in the intervertebral foramen.
The posterior root contains the processes of sensory neurons carrying information to the CNS. The cell bodies of the sensory neurons, which are derived embryologically from neural crest cells, are clustered in a spinal ganglion at the distal end of the posterior root, usually in the intervertebral foramen. The anterior root contains motor nerve fibers, which carry signals away from the CNS. The cell bodies of the primary motor neurons are in anterior regions of the spinal cord.
The anterior root contains motor nerve fibers, which carry signals away from the CNS. The cell bodies of the primary motor neurons are in anterior regions of the spinal cord.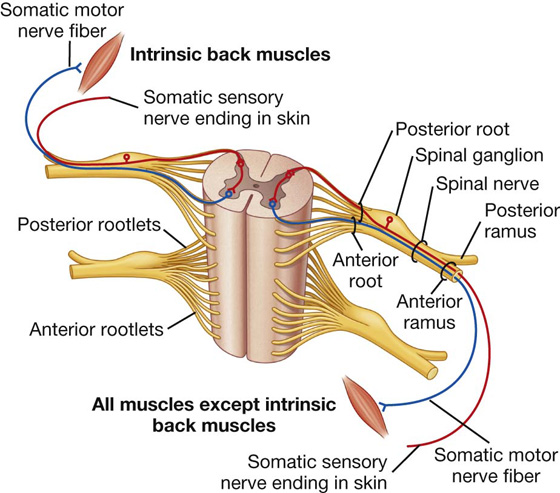
 The anterior rami innervate most other skeletal muscles (the hypaxial muscles) of the body, including those of the limbs and trunk, and most remaining areas of the skin, except for certain regions of the head.
The anterior rami innervate most other skeletal muscles (the hypaxial muscles) of the body, including those of the limbs and trunk, and most remaining areas of the skin, except for certain regions of the head.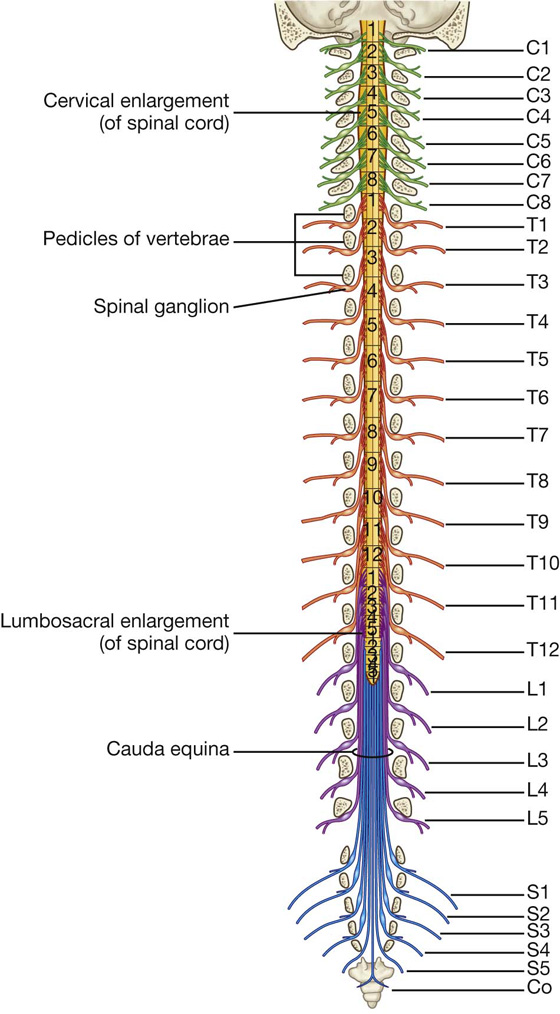
 five lumbar nerves—L1 to L5,
five lumbar nerves—L1 to L5, one coccygeal nerve—Co.
one coccygeal nerve—Co.