Chapter 6 Upper Extremity Peripheral Nerve Blockade
 Upper extremity blockade may be performed for therapeutic, diagnostic, prophylactic, and prognostic indications.
Upper extremity blockade may be performed for therapeutic, diagnostic, prophylactic, and prognostic indications. Ultrasound-based techniques result in faster onset, shorter procedure time, higher success rates, longer block duration, and fewer vascular punctures than alternative techniques.
Ultrasound-based techniques result in faster onset, shorter procedure time, higher success rates, longer block duration, and fewer vascular punctures than alternative techniques. Foreknowledge of brachial plexus anatomy and desired site of action is critical to selection of appropriate location of brachial plexus blockade.
Foreknowledge of brachial plexus anatomy and desired site of action is critical to selection of appropriate location of brachial plexus blockade. In ultrasound-guided techniques, the deepest and most distal structures from the needle insertion site should be blocked first.
In ultrasound-guided techniques, the deepest and most distal structures from the needle insertion site should be blocked first.Introduction
Upper extremity peripheral nerve blockade, in one form or another, has been performed since ancient Egypt as evidenced by 5000-year-old pictographs illustrating nerve compression anesthesia for hand surgery.1 Today, the development of image-guidance technology and efficacious injectable drugs have made upper extremity peripheral nerve blockade an increasingly useful tool in pain physicians’ and regional anesthesiologists’ diagnostic and therapeutic arsenal. Peripheral nerve blockade is a growing and dynamic field with diverse approaches, technological equipment, and a variety of local anesthetics and adjuvant therapies.
Brachial Plexus Anatomy
Familiarity with brachial plexus anatomy is critical to optimal and safe performance of peripheral nerve techniques. The most proximal portion of the brachial plexus is located in the posterior triangle of the neck, bordered by the clavicle inferiorly, the trapezius muscle posteriorly, and the sternocleidomastoid muscle anteriorly. There, the plexus is deep to the skin, subcutaneous tissue, deep fascia, and platysma muscle and is formed by the union of the anterior (ventral) primary rami of cervical nerves five through eight (C5-C8) and the greater part of the first thoracic nerve (T1). In some patients, the fourth cervical (C4) and second thoracic (T2) nerves also contribute to the brachial plexus. At its most proximal, the C5-T1 nerve roots conjoin to form the superior (C5-C6), middle (C7), and inferior trunks (C8-T1) (Fig. 6-1).
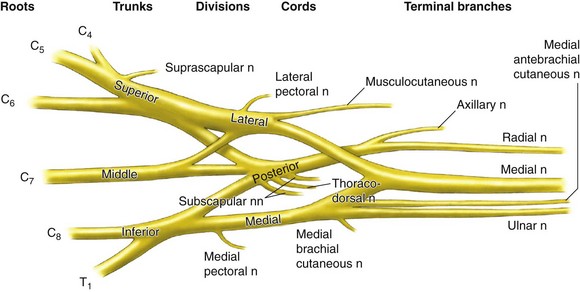
Fig. 6-1 Brachial plexus anatomy.
(Reprinted with permission from Torsher L, Smith H, Jacob A: Interscalene blockade. In Hebl JR, Lennon RL, editors: Mayo Clinic atlas of regional anesthesia and ultrasound-guided nerve blockade, New York, 2010, Oxford University Press, p 192.)
A superficial landmark, the interscalene groove, overlies the trunks and is palpable as an indentation between the anterior and middle scalene muscles. This groove, at the level of the cricoid cartilage, is the needle entry site used most frequently for interscalene brachial plexus blockade. The phrenic nerve, derived from the C3-C5 nerve roots, runs parallel to the vertebral artery at this location as it passes through the neck on the ventral surface of the anterior scalene muscle. Sonographic study has revealed that the phrenic nerve is visible as a hypoechoic structure in 93% of subjects.2 The phrenic nerve is immediately adjacent to the superior trunk at the C6 level, thus explaining the uniform deactivation of this nerve during interscalene blockade.3
As the three trunks descend toward the first rib, the brachial plexus differentiates into anterior and posterior divisions, corresponding to the ventral and dorsal aspects of the upper extremity. Located posterolateral to the subclavian artery, the divisions pass below the middle third of the clavicle and above the first rib before fusing into medial, lateral, and posterior cords. Approaches to the brachial plexus immediately above and below the clavicle are the so-named supraclavicular and infraclavicular blocks. At the lateral border of the pectoralis minor muscle, the axillary artery is surrounded by the lateral, posterior, and medial cords of the brachial plexus. As the cords enter the axilla, they give rise to the sensorimotor branches of the plexus, the radial, median, ulnar, and musculocutaneous nerves. These peripheral nerves consist of individual myelinated nerve fibers embedded within an endoneurial connective tissue layer and grouped into discrete bundles or fascicles. Nerve fascicles are interlaced by connective tissue and surrounded by an outer epineurial membrane.4
Indications and Contraindications
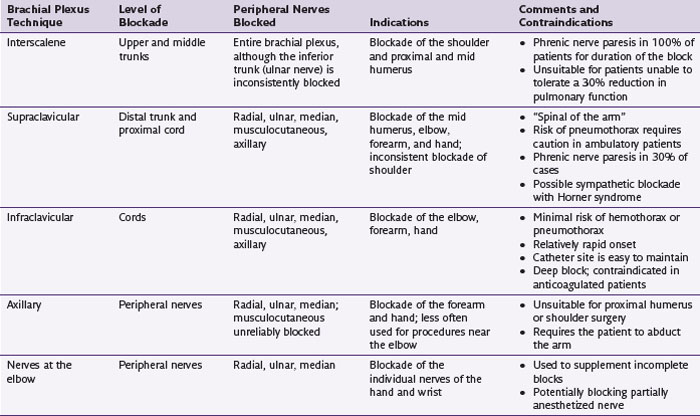
Because several nerves join or diverge from the brachial plexus between its central origins and its most distal peripheral branches, no single location suffices to produce complete blockade of the upper extremity. Thus, proximal block locations are selected based on foreknowledge of the current or future pain distribution. Table 6-1 lists the more common indications and techniques for blockade of various elements of the brachial plexus.
Equipment
Blockade of the brachial plexus can be accomplished through a variety of methods based on block location, equipment availability, and the experience of the practitioner. Traditional methods of nerve localization include paresthesia-seeking, nerve stimulation, or transarterial approaches.5–7 Ultrasonography is increasingly the most common tool for visualizing the neuroanatomy and surrounding structures.8
Paresthesia
Nerve Stimulator
Nerve stimulation uses small electrical currents to induce nerve depolarization and subsequent motor responses. Nerve stimulators generate a square wave, typically one or two times per second and 0.1 seconds in duration. The amplitude is initially set around 1.0 to 1.5 mA and decreased after a motor response is identified. High degrees of block success are obtained when a motor response is maintained below 0.7 mA. Motor response with amplitude less then 0.3 may be associated with an intraneural needle position. Of note, two recent studies9,10 have demonstrated that needle-to-nerve contact fails to provide a motor response at amplitudes of 0.7 mA up to 15% of the time, a phenomenon that has yet to be adequately explained.
Techniques
Interscalene
Traditional interscalene blockade of the trunks of the brachial plexus is achieved by inserting a needle between the anterior and middle scalene muscles at the level of the cricoid cartilage in the posterior cervical triangle of the neck (Fig. 6-2).
With the needle directed toward the sternal notch, the trunks are encountered at a depth of 1 to 2 cm. This modified technique, described by Winnie in 1970,11 uses either nerve stimulation or paresthesia to identify the trunks of the brachial plexus. A response in the deltoid or distal arm is acceptable. When sonographic identification of the supraclavicular brachial plexus is performed, the divisions of the brachial plexus are traced cephalad from the clavicle to the interscalene location. In-plane or out-of-plane needle approaches for interscalene blockade have been described. In-plane needle insertion is performed from posterior to anterior to avoid needle trauma to the phrenic nerve. The out-of-plane insertion is performed from the caudal side of the probe.
Supraclavicular
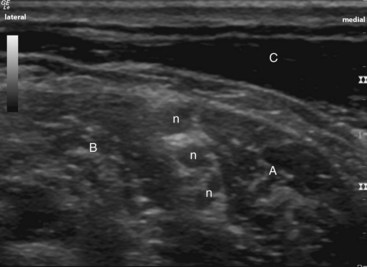
Before the development of ultrasonography, supraclavicular blockade was performed using paresthesia or nerve stimulation. These techniques were associated with a 0.5% to 6.1% risk of pneumothorax.4 The use of ultrasonography has renewed interest in the supraclavicular approach to brachial plexus blockade because most providers believe that direct observation allows them to avoid this complication.8,12,13 It should be noted, however, that case reports of pneumothorax during ultrasound-guided supraclavicular and infraclavicular blockade have been reported. To perform this technique, the ultrasound probe is placed in the supraclavicular fossa angled toward the first rib. An image should be acquired that includes a longitudinal view of the first rib along with a cross-sectional view of the subclavian artery and brachial plexus (Fig. 6-3).
Infraclavicular
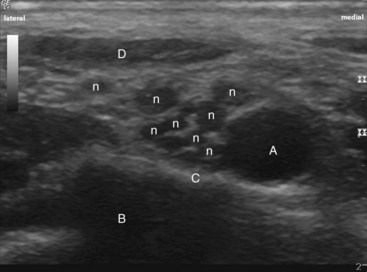
A touted benefit of the infraclavicular approach to the brachial plexus is that it can be performed with the patient’s arm in an adducted position. Two of the most frequently used traditional approaches were initially reported by Wilson et al14 and Raj et al,15 which are performed using nerve stimulation or paresthesia nerve localization techniques. In the Raj approach, a needle is inserted at the midpoint of the inferior border of the clavicle. The needle is directed lateral toward the axilla. In the Wilson (“coracoid”) approach, the needle is inserted perpendicular to the skin 2 cm medial and 2 cm inferior to the tip of the coracoid process. A motor or sensory response in the hand is ideal, and biceps or deltoid responses may signify inadequate distal blockade. The deep location of the nerve cords makes this location the most challenging ultrasound-guided block compared with other approaches to the brachial plexus. In-plane or out-of-plane ultrasound-guided approaches can be used.16–18 The probe is placed perpendicular to the inferior border of the middle of the clavicle, where the subclavian artery and the cords of the brachial plexus can be seen in cross section (Fig. 6-4).
Axillary
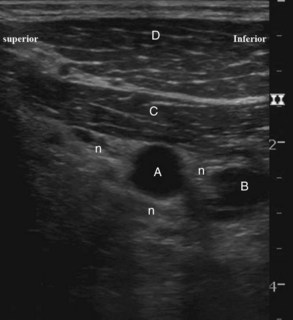
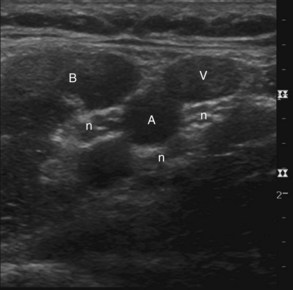
Multiple techniques have been described for brachial plexus blockade in the axilla. All techniques require a 90-degree abduction of the arm at the shoulder. Common techniques include transarterial, nerve stimulation, paresthesia, and ultrasound guidance. All techniques take advantage of the close proximity of the terminal nerves to the axillary artery. Transarterial techniques rely on blood aspiration to identify the anterior and posterior walls of the artery to achieve perivascular local anesthetic spread. Nerve stimulation and paresthesia techniques try to avoid vascular puncture and instead rely on individual nerve localization. Injection of local anesthetic around two separate terminal nerve branches is recommended for successful blockade. For ultrasound techniques, the axillary artery remains the most prominent landmark for identifying the neuroanatomical structures (Fig. 6-5).
The probe is placed near the axilla perpendicular to the long axis of the arm so the axillary artery can be seen in cross section. The nerves viewed in short axis may be seen in a variety of positions around the artery because anatomical variation in the axilla is significant.19 In-plane needle guidance is recommended, with deeper and more distal nerves blocked first. In each approach, the musculocutaneous nerve must be blocked separately. The musculocutaneous nerve is highly visible under ultrasonography, typically occupying the fascial interface between the biceps and coracobrachialis muscles. Alternatively, the musculocutaneous nerve may be blocked by subcutaneous injection at the elbow.
Blockade of isolated upper extremity peripheral nerves, either for supplementation of inadequate surgical block or producing selective nerve distribution blockade, is easily performed at a supracondylar location. From medial to lateral, the ulnar, median, and radial nerves are visualized by cross-sectional ultrasonography by scanning with the probe just above the elbow.20
Outcomes Evidence
Upper extremity blockade, whether it is for primary anesthesia, postoperative analgesia, or acute pain intervention, is generally highly successful. Block success rates, depending on the anatomical location and end points measured, range from 85% to 100%. Recent evidence has shown that block outcomes using ultrasonography exceed other nerve localization techniques. Specific advantages of ultrasonography in upper extremity blockade include fewer needle passes, faster onset, shorter procedure time, higher success rates, longer block duration, and fewer vascular punctures.21 Improvements in patient safety related to ultrasonography use, however, are yet to be proven. In fact, pneumothorax, local anesthetic toxicity (seizures and cardiac arrest), and peripheral nerve injury have all been reported during ultrasound-guided upper extremity blockade.22
Risk and Complication Avoidance
Peripheral nerve blockade may be associated with a unique set of complications, and care must be taken to minimize relevant risks. Complications may be classified as neurological, vascular, infectious, or related to local anesthetic toxicity. Although rare, peripheral nerve injuries are potentially catastrophic complications that may lead to long-term neuropathic pain or limb disability. Patient, procedure, and technical risk factors have all been identified as potential etiologies. Expert opinion suggests that multiple factors commonly play a role and that patients with several concomitant risks may have a higher incidence of neurological complications. Avoidance, or risk management, is complex but hinges primarily on appropriate preventive decision-making strategies and use of safe techniques. Neurological history and examination may reveal underlying patient neuropathic or degenerative processes that may preclude nerve blockade. Maintenance of sterile technique, use of minimal effective drug doses and concentrations, use of incremental aspiration and injection practices, and avoidance of intraneural or intrafascicular injection are all prudent measures to facilitate patient safety. Thus, use of imaging technology and other methods of nerve localization that allow needle and nerve distinction may help clinicians minimize risk of neurological complication. Recent evidence suggests that disruption of the perineurial membrane, which surrounds and regulates the microenvironment of nerve fascicles, with saline or local anesthetic injection produces histologic changes consistent with nerve injury.23
1 Barash PG, Cullen BF, Stoelting RK, et al. Clinical anesthesia, ed 6. Philadelphia: Lippincott Williams & Wilkins; 2009.
2 Kessler J, Schafhalter-Zoppoth I, Gray AT. An ultrasound study of the phrenic nerve in the posterior cervical triangle: implications for the interscalene brachial plexus block. Reg Anesth Pain Med. 2008;33(6):545-550.
3 Urmey WF, Talts KH, Sharrock NE. One hundred percent incidence of hemidiaphragmatic paresis associated with interscalene brachial plexus anesthesia as diagnosed by ultrasonography. Anesth Analg. 1991;72(4):498-503.
4 Neal JM, Gerancher JC, Hebl JR, et al. Upper extremity regional anesthesia: essentials of our current understanding, 2008. Reg Anesth Pain Med. 2009;34(2):134-170.
5 Aantaa R, Kirvela O, Lahdenpera A, et al. Transarterial brachial plexus anesthesia for hand surgery: a retrospective analysis of 346 cases. J Clin Anesth. 1994;6(3):189-192.
6 Selander D, Edshage S, Wolff T. Paresthesiae or no paresthesiae? Nerve lesions after axillary blocks. Acta Anaesthesiol Scand. 1979;23(1):27-33.
7 Sia S, Bartoli M, Lepri A, et al. Multiple-injection axillary brachial plexus block: a comparison of two methods of nerve localization-nerve stimulation versus paresthesia. Anesth Analg. 2000;91(3):647-651.
8 Kapral S, Krafft P, Eibenberger K, et al. Ultrasound-guided supraclavicular approach for regional anesthesia of the brachial plexus. Anesth Analg. 1994;78(3):507-513.
9 Beach ML, Sites BD, Gallagher JD. Use of a nerve stimulator does not improve the efficacy of ultrasound-guided supraclavicular nerve blocks. J Clin Anesth. 2006;18(8):580-584.
10 Perlas A, Chan VW, Simons M. Brachial plexus examination and localization using ultrasound and electrical stimulation: a volunteer study. Anesthesiology. 2003;99(2):429-435.
11 Winnie AP. Interscalene brachial plexus block. Anesth Analg. 1970;49(3):455-466.
12 Franco CD, Gloss FJ, Voronov G, et al. Supraclavicular block in the obese population: an analysis of 2020 blocks. Anesth Analg. 2006;102(4):1252-1254.
13 Chan VW, Perlas A, Rawson R, et al. Ultrasound-guided supraclavicular brachial plexus block. Anesth Analg. 2003;97(5):1514-1517.
14 Wilson JL, Brown DL, Wong GY, et al. Infraclavicular brachial plexus block: parasagittal anatomy important to the coracoid technique. Anesth Analg. 1998;87(4):870-873.
15 Raj PP, Montgomery SJ, Nettles D, et al. Infraclavicular brachial plexus block—a new approach. Anesth Analg. 1973;52(6):897-904.
16 Bigeleisen P, Wilson M. A comparison of two techniques for ultrasound guided infraclavicular block. Br J Anaesth. 2006;96(4):502-507.
17 Sandhu NS, Capan LM. Ultrasound-guided infraclavicular brachial plexus block. Br J Anaesth. 2002;89(2):254-259.
18 Ootaki C, Hayashi H, Amano M. Ultrasound-guided infraclavicular brachial plexus block: an alternative technique to anatomical landmark-guided approaches. Reg Anesth Pain Med. 2000;25(6):600-604.
19 Retzl G, Kapral S, Greher M, et al. Ultrasonographic findings of the axillary part of the brachial plexus. Anesth Analg. 2001;92(5):1271-1275.
20 Rettke SR, Smith HM. Elbow blockade. In: Hebl JR, Lennon RL, editors. Mayo Clinic atlas of regional anesthesia and ultrasound-guided nerve blockade. New York: Oxford University Press; 2010:467.
21 McCartney CJ, Lin L, Shastri U. Evidence basis for the use of ultrasound for upper-extremity blocks. Reg Anesth Pain Med. 2010;35(2 suppl):S10-S15.
22 Neal JM, Brull R, Chan VW, et al. The ASRA evidence-based medicine assessment of ultrasound-guided regional anesthesia and pain medicine: executive summary. Reg Anesth Pain Med. 2010;35(2 suppl):S1-S9.
23 Sala-Blanch X, Ribalta T, Rivas E, et al. Structural injury to the human sciatic nerve after intraneural needle insertion. Reg Anesth Pain Med. 2009;34(3):201-205.