Chapter 24 Upper Airway Retraction
New and Old Laryngoscope Blades
II History
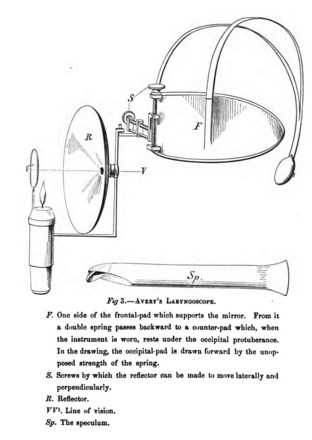
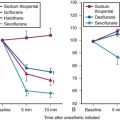
Benjamin Babington first described mirror-based indirect laryngoscopy in 1829,1 although it is often erroneously attributed to Manuel Garcia, a singer who described visualization of his own vocal cords in 1855.2–8 Babington also hinged a tongue depressor to his initial mirror design, but he subsequently abandoned the depressor and focused on the mirror alone (Fig. 24-1). In 1844, John Avery combined a reflective speculum with an external light source to view the larynx (Fig. 24-2).4 Mirror laryngoscopy for the investigation of laryngeal pathology was pioneered by Johann Czermak, who used instruments designed by Ludwig Turck in the late 1850s.5–8 Czermak subsequently applied an external light source and a head-mounted mirror to improve visualization.7

Figure 24-1 British physician Benjamin Babington combined a mirror and spatula.
(From Mackenzie M: Use of the laryngoscope in diseases of the throat, ed 2, Philadelphia, 1869, Lindsay & Blakiston.)
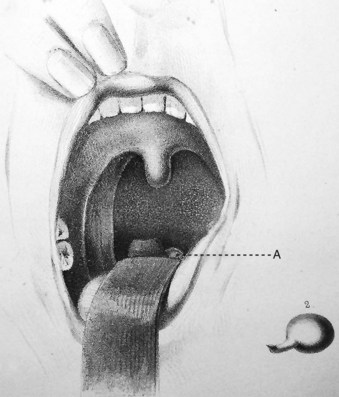
Horace Green, widely considered to be America’s first laryngologist, used tongue spatulas and probangs to examine and treat diseases of the larynx and trachea in the mid-1800s. In 1845, Green performed transoral removal of a laryngeal polyp in an 11-year-old girl using a bent tongue spatula to expose the larynx and polyp to direct vision (Fig. 24-3).7,9 Green’s technique9 is remarkably similar to the indirect elevation of the epiglottis described almost 90 years later by Macintosh:
Green goes on to describe the use of a hook and knife passed “nearly an inch into the glottis” to extract the polyp. Despite Green’s accomplishments in direct laryngeal exposure, laryngeal surgery, and intubation, the first publication on direct laryngoscopy is credited to Alfred Kirstein in 1895, who called the new procedure autoscopy and devised techniques for use with the patient in sitting and supine positions.10,11 Kirtsein’s 1896 treatise on the procedure presages the development of laryngoscopy blades used in the modern era.11 He observes that the tongue must be drawn forward and downward (with the patient sitting in front of the operator): “To get this position of the tongue, a tongue depressor is necessary (i.e., spatula)—which, however, unlike the ordinary spatula, must not be placed in front of the circumvallate papillae but must be applied behind the same to the root of the tongue” (Fig. 24-4). The epiglottis can be elevated directly by an instrument that projects over the epiglottis (e.g., the tip of the spatula introduced behind the epiglottis) or indirectly by a method described by Reichert in 1879 and promulgated by Kirstein11:
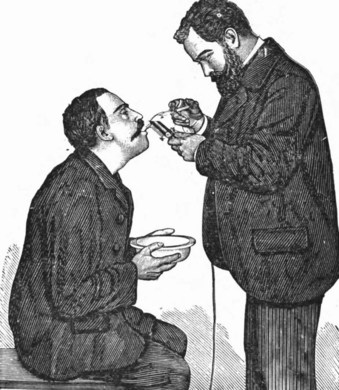
Figure 24-4 Alfred Kirstein performed autoscopy in the 1890s.
(From Kirstein A, Thorner M: Autoscopy of the larynx and the trachea (direct examination without mirror), Philadelphia, 1896, FA Davis.)
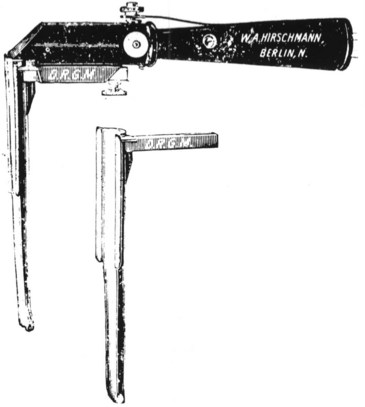
Kirstein developed two spatulas (Fig. 24-5). One had a distal, bent, bifid tip, which he called the standard spatula, that was designed for placement in the valleculae and pressed on the median glossoepiglottic ligament. Kirstein’s intralaryngeal, perfectly straight spatula was designed to be introduced behind the epiglottis and press it against the root of the tongue. His descriptions of these instruments and intended uses portray exactly the functioning of modern curved- and straight-blade laryngoscopes.11
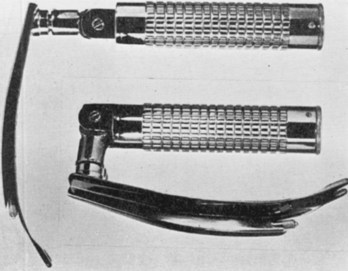
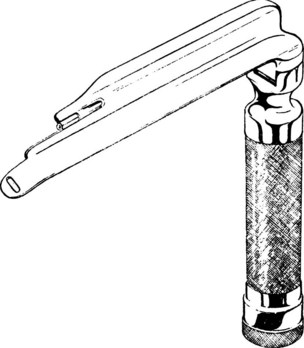
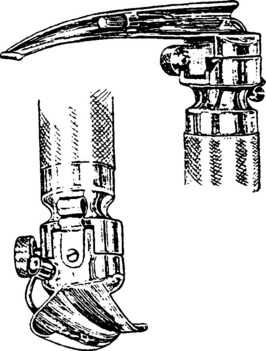
Chevalier Jackson, a professor of laryngology at Jefferson Medical College in Philadelphia (after Jacob de Silva Solis-Cohen, another Jefferson pioneer), refined laryngoscopy techniques in supine patients and established the principles of modern laryngoscopic exposure. Jackson created a tubed glottiscope in 1903 and was the first to apply enclosed distal lighting using a tungsten bulb that was connected to a large battery.5–912 Subsequent versions of Jackson’s tubular laryngoscope incorporated a removable, sliding floor that facilitated tube insertion, and he reported on the routine insertion of tracheal tubes using direct laryngoscopy in 1913 (Fig. 24-6).12,13 In the same year, Henry Janeway, an anesthesiologist at Bellevue Hospital in New York City, described a smaller and more portable laryngoscope powered by batteries located in the handle (Fig. 24-7).14 It featured a straight blade with a slight distal curve.14 Janeway’s blade did not achieve commercial success, but similar large, C-shaped, straight-blade designs created by Flagg, McGill, and Guedel became widely adopted.15,16
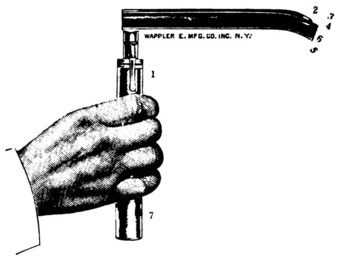
Figure 24-7 Henry Janeway produced a portable laryngoscope powered by batteries located in the handle.
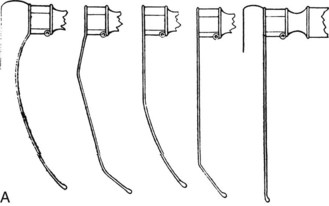
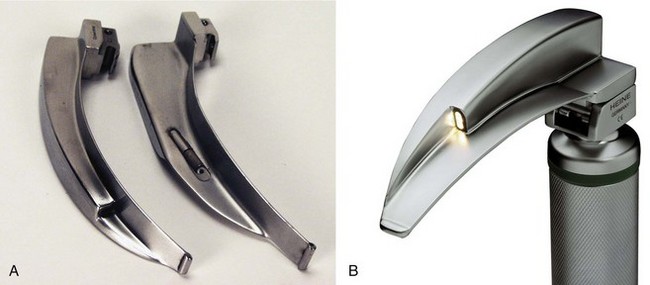
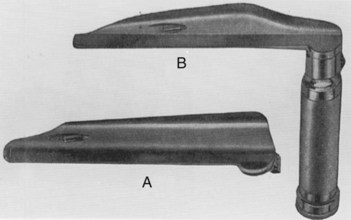
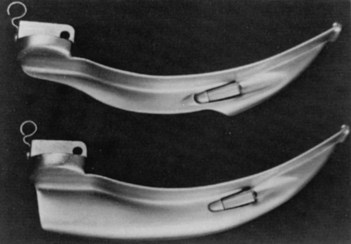
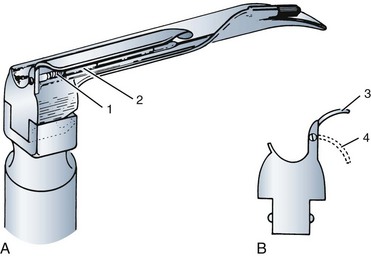
Laryngoscope blade design and laryngoscopy technique underwent little apparent evolution until Robert Miller’s 1941 narrow-lumen, D-shaped, straight-blade design and Robert Macintosh’s 1943 publication about a new curved-blade laryngoscope (Fig. 24-8, A).17,18 The Macintosh and Miller blades have become universally adopted and the benchmarks against which all direct laryngoscope blades are compared. Although innumerable modifications of these standard designs have been described in the past 70 years, only a few alternative designs have achieved widespread use. In the 1970s, the flexible fiberoptic bronchoscope offered another option for use in difficult situations, and rigid fiberoptic devices such as the Bullard laryngoscope were first introduced in the late 1980s. The 1990s saw the introduction of additional rigid fiberoptic laryngoscopes and commercially available fiberoptic stylets. In the 21st century, video-assisted devices have been added to clinical practice.
III Direct Laryngoscope Design
A Components of a Direct Laryngoscope
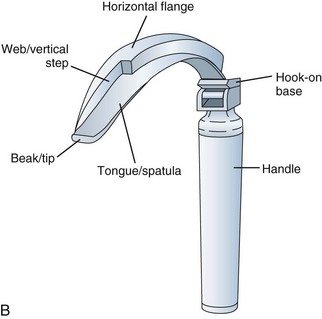
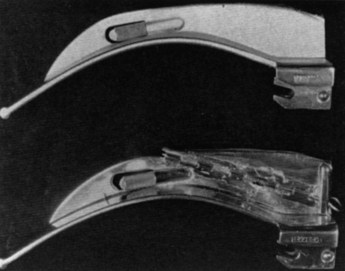
A laryngoscope consists of a handle, a blade, and a light source. There are marked variations in blade shape, tip design, and the mechanism and location of illumination systems (i.e., bulbs, or light-conducting fibers). The section of the blade that contacts the tongue is the spatula, and the left edge of the blade (from the operator’s perspective) is the flange. (see Fig. 24-8, B). The proximal vertical flange is sometimes called the vertical step. At the base (or heel) of the blade is the block, which interacts with the top of the handle. The connection between the blade and handle causes the light to come on when the blade is opened. Blades are designed to attach and detach from the handle with a standardized fitting (engaged at 45 degrees) that connects a hook on the blade to a small rod at the top of the handle.
B Direct Laryngoscope Lighting
Visualization of the laryngeal inlet during direct laryngoscopy depends on adequate illumination of airway structures by the laryngoscope. Illumination is a function of the intensity and color of the supplied light and the area over which it falls. These factors depend on the nature of the laryngoscope blade’s light source and the potential of the power source applied to it. Light can be measured in several ways: at its source (i.e., luminous flux, measured in lumens), at its receiving surface (i.e., illuminance, measured in lux), or by the amount of light re-emitted from a surface in a given direction (i.e., luminance, measured in candela per square meter [cd/m2]).19,20 During direct laryngoscopy, perception of the surface brightness of the larynx depends on light transmitted back to the laryngoscopist’s eyes from the surface of the larynx; this is luminance.
A significant variable in the perception of adequate lighting during laryngoscopy is the operator. As clinicians age, they develop presbyopia (beginning in the fourth decade, regardless of visual acuity), and the amount of light needed for a given visual task increases. This is especially significant in performing direct laryngoscopy because the larynx is sighted with only one eye due to the severe visual restrictions of the procedure.21 The procedure is visually analogous to looking down a 1-inch pipe at a target 12 to 18 inches away; visual restrictions include the mouth, teeth, tongue, blade, and epiglottis. Because the right and left eye are separated in the skull by 4 to 5 inches, the two views are disparate and cannot be merged into a stereoscopic view of the larynx. Subconsciously, we suppress the nondominant image through a phenomenon known as binocular suppression. It is not known what component of difficult laryngoscopy is related to inadequate lighting, but adequate illuminance is especially important when landmarks are obscured by secretions, blood, and vomitus and when the epiglottis causes shadowing of the larynx.
Historically, there was no standard for laryngoscope light, but the International Organization for Standardization recently agreed on a standard of 500 lux after 10 minutes of operation.22 The illuminance of a laryngoscope light at the distal tip of the blade is a function of the distance from the light source to the tip of the blade, the type of bulb or fiberoptic-conducting system, and the battery type and charge status.23 The light-to-tip distance is important because the amount of illuminance at a target is governed by the inverse square law (i.e., if the distance from the light source is doubled, one fourth of the amount of light lands on the target). Across different clinical settings, there may be dramatic differences in the illuminance of blade and handle pairs. Marked variation and poor light performance of laryngoscopes is widespread in anesthesia and emergency departments.23,24 In a study of many emergency departments in Philadelphia, there was a 500-fold difference in the illuminance produced by different blade and handle pairs, ranging from 11 to more than 6000 lux.24
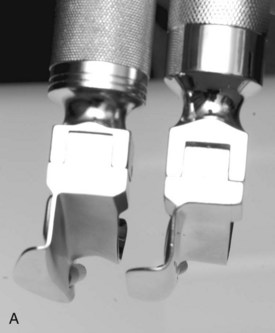
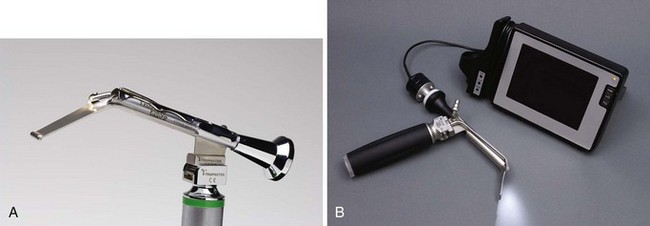
Bulb-on-blade laryngoscopes (called conventional blades) and fiber-lit laryngoscopes (in the United States, called green-line scopes) use different, non-interchangeable fittings (Fig. 24-9). Bulb-on-blade laryngoscopes have a simple electrical connection between the handle and blade. The electrical circuit is completed by opening the blade, providing power to the bulb, which is mounted on the distal aspect of the blade. Halogen and xenon bulbs are used by many manufacturers, but within the past 5 years, super-bright LED bulbs have become available. LED bulbs have tremendous advantages compared with other bulbs. They use a fraction of the energy of xenon or halogen bulbs, and they operate at much lower temperatures. The light they produce is much whiter, which may improve the discrimination of landmarks. The more yellow color of standard bulbs can be especially poor for distinguishing reddish yellow mucosal structures (e.g., epiglottis from the posterior pharyngeal wall). The primary reason LED lights will become standard on all instruments in the future is cost; as LEDs become much more commonly used on laryngoscopes and other portable medical instruments, the cost of the bulbs will continue to decrease. Some manufacturers already offer inexpensive, single-use, all-steel, LED-bulb blades (Fig. 24-10). Another advantage of LED bulb-on-blade designs is that they do not require expensive handle-battery systems because of their low energy requirements. This extends the operational and shelf life of the handle-battery pair dramatically, an important feature when stocking laryngoscopes in code carts and other settings.

Figure 24-10 Examples of all-steel laryngoscope blades with LED bulbs on them.
(Courtesy of SunMed, Largo, FL.)
An alternative illumination system uses light-conducting fibers in the blade with a bulb mounted in the top of the laryngoscope handle. In the United States, these blades have a green dot on the base, and the handles have a green ring on the top. Different types of fiber-lit blades and handles are not interchangeable. Fiber-lit systems depend on a good fit between the base of the blade and the top of the handle. A spring-loaded mechanism depresses the light at the top of the handle, making an electrical connection with the batteries. Problems with the spring may cause erratic performance, and a poor fit can allow light to escape between the bulb source in the handle and the fiberoptic bundle in the blade. The best light-conducting material is glass fiber, and the best designed of the glass fiber–lit blades use large arrays of fiber bundles (Fig. 24-11). There is significant variation in the size and quality of these glass fibers among manufacturers. Glass fiber is relatively expensive, and its light conduction deteriorates over time, depending on sterilization techniques.25 Fast deterioration in light conduction, erosion of the bond between the glass and blade, and rusting of the blade occurs with lower-quality glass fiber blades.
Acrylic can be used for light conduction, and although it is not as effective a light conductor as glass, it is inexpensive and easy to integrate onto a laryngoscope blade (Fig. 24-12). Glass fibers must be wrapped in a steel rod and then attached to the blade or threaded through a channel that runs the length of the blade, but an acrylic rod can be easily attached as a separate component. Better acrylic fiber–lit blades enclose part or all of the acrylic rod to minimize light loss (Fig. 24-13). Acrylic fiber–lit blades usually are designed as single-use blades; they are inexpensive to produce, and their light conduction deteriorates significantly with sterilization. The inferior light-conducting performance of acrylic can be compensated by super-bright bulbs (LED is best) and powerful handles, but these features necessitate relatively expensive lamps, reflectors, and battery systems (Fig. 24-14).

Figure 24-12 Disposable, fiber-lit blades are available in stainless steel with acrylic stems (SunMed Healthcare, Largo, FL).
A major variable in laryngoscope lighting involves the battery source. Standard handles use two C-sized batteries, and most pediatric handles or stubby handles use AA batteries. Several companies offer small handles that use a single, 3-volt, CR123 lithium battery (i.e., camera type). Compared with alkaline batteries, lithium batteries (regardless of size) have a flatter discharge curve, and they slowly diminish in power output over a long time. When lithium batteries start to fade, they die quickly; but during operation, they maintain a much more steady power output. Alkaline battery–powered handles continue to turn on even though light output has diminished dramatically. This phenomenon contributes to delayed battery replacement, because few clinical settings monitor blade and handle pairs using light meters. Many manufacturers offer rechargeable fiber-lit handles using nickel–metal hydride or nickel-cadmium batteries; combined with LED bulbs and special reflectors, these handles create brilliant white light that is far superior to older illumination technology (Fig. 24-15).
C Direct Laryngoscope Blade Design
Laryngoscope blade design has evolved through trial and error and by sophisticated technical analysis. Macintosh published a series of blade design drawings with which he had experimented; models varied from the curved blade so widely accepted subsequently to entirely straight blades18,26 (Fig. 24-16). Some investigators have made use of lateral head and neck fluoroscopy and radiography during laryngoscopy to help elucidate relationships of the tongue, hyoid bone, epiglottis, and laryngoscope blade during laryngoscopy.27,28
The scientific evaluation of laryngoscope blades has been impeded by the visual restrictions inherent to laryngoscopy; for example, the target is seen monocularly and therefore cannot be simultaneously viewed by two operators.21 Although a head-mounted direct laryngoscopy video system was invented in 1998 that allowed routine recording of the procedure from the operator’s perspective, few studies of laryngoscope blade design have used this objective tool.29 Most studies have relied on subjectively reported laryngeal view (i.e., visualization of the larynx by the laryngoscopist for a few seconds). The standard reporting system of laryngeal view (i.e., Cormack-Lehane classification) has poor interobserver reliability and is not very sensitive because up to 99% of direct laryngoscopies involve Cormack-Lehane grade 1 or 2 views.30 This grading system does not allow detection of differences between blade designs without a very large number of patients because of the relative scarcity of grade 3 and 4 views. The combination of restricted visualization, subjective reporting of the view, and lack of a sensitive means of reporting has historically retarded rigorous research on laryngoscopy blade design. As observed by McIntyre in a 1989 review article on blade design, “detailed evaluations of the performance of any particular laryngoscope blade are extremely rare and critical analysis virtually nonexistent.” 31
IV Direct Laryngoscopy Blades
A Macintosh and Related Curved Blades
1 Macintosh Laryngoscope Blade
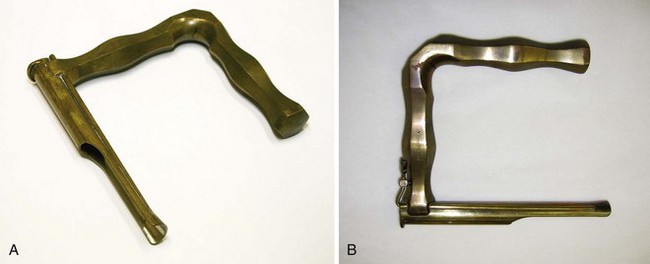
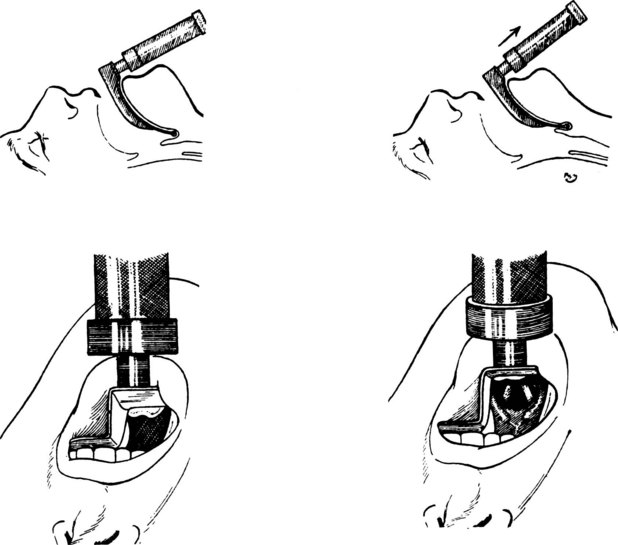
Macintosh’s 1943 publication of his curved-blade laryngoscope design defined a new blade and emphasized a novel technique of laryngeal exposure for anesthesiologists (i.e., indirect elevation of the epiglottis) (see Figs. 24-8A and 24-16).18 Although the pioneers of laryngology, including Green and Kirstein, were familiar with indirect elevation of the epiglottis, this technique was not widely appreciated in the new clinical discipline of anesthesiology. Macintosh stumbled into the design by accidentally exposing the larynx indirectly after inserting a Boyle-Davis mouth gag to keep the mouth open and depress the tongue during a tonsillectomy case: “Opening the mouth with the [Boyle-Davis] gag, I found the cords perfectly displayed.… Before the morning had finished, I had Richard Salt [senior technical assistant of his anesthesia department] … [solder] the Davis blade onto a laryngoscope handle, and this functioned quite adequately as a laryngoscope.”32 The Crowe-Davis gag had been in use for several decades (Fig. 24-17); Boyle popularized the use of this mouth gag in England during World War II.33

Figure 24-17 Davis blade.
(Courtesy of the University of Melbourne Museum Image Archives, Melbourne, Australia.)
Macintosh’s classic article in The Lancet described using his shorter, curved blade by placing its tip in the vallecula between the epiglottis and the base of the tongue, with subsequent indirect elevation of the epiglottis.18 Macintosh contended that he could use the blade at a lighter plane of anesthesia because of the predominant glossopharyngeal nerve innervation of the base of tongue area rather than the superior laryngeal nerve innervation of the dorsal surface of the epiglottis. This was important before the widespread use of neuromuscular blockers. He also mentioned the need to insert the blade to the right of the tongue, with a sweep to the left to displace and control the tongue.18 In this original communication, Macintosh stated and later reiterated that “the precise shape or curve of the blade does not seem to matter much provided that the tip does not go beyond the epiglottis.”18 However, numerous modifications of the Macintosh blade have been reported.
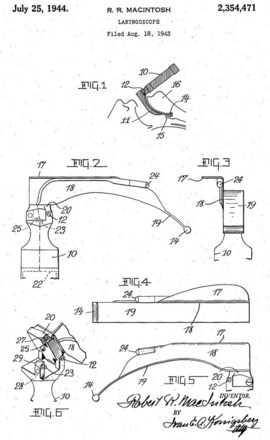
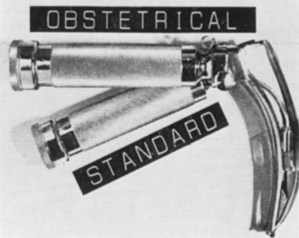
The specific design of the Macintosh blade has a circuitous history. Macintosh, a New Zealander, invented the blade while working in England. Richard Foregger, the son of Richard von Foregger, a manufacturer of early anesthesia devices, was stationed briefly in England during the Second World War. Macintosh gave his new blade to Foregger’s son to bring to America, and he also gave blades to two English manufacturers (Medical Industrial Equipment and Longworth Scientific Instruments).34 Macintosh did not pursue patents or royalties on his design. The U.S. patent application by the Foregger company shows Macintosh’s name spelled incorrectly (with a capital I in the middle), and this incorrect spelling persists on many labels34 (Fig. 24-18). The American and English Macintosh blade designs are descendants of the blades initially produced by the Foregger and Longworth companies, respectively.34 Macintosh thought that one size would fit all adults, but the blade was initially used in obstetrics cases (i.e., only in women). Eventually, a larger size was devised, which evolved into the modern Macintosh 4, whereas the original design approximates what became the Macintosh 3. Although manufacturers have produced a Macintosh 2 and Macintosh 1, these sizes were not endorsed by Macintosh, and direct laryngoscopy in small children and infants usually is done with straight blades.
2 English Macintosh Blade
The English Macintosh laryngoscope, initially produced by Longworth in the United Kingdom, is continuously curved along the entire spatula, the flange runs to the tip of the blade, and the proximal flange is smaller34–36 (Fig. 24-19). In contrast, many versions of the American Macintosh are straight in the distal portion, have a distal tip without a flange, and have a very large proximal flange. The bulb on an English Macintosh is closer to the distal tip, increasing illuminance measured at the tip. Although not standardized across all English-labeled Macintosh blades, most English designs use a clear bulb, whereas American Macintosh designs usually come with a frosted bulb. English blades and American Macintosh blades are also offered with fiber-lit illumination systems, which typically use smaller (2- to 3-mm), round bundles.
Asai and colleagues conducted a randomized crossover study of the English blade, comparing it with the standard Macintosh in 300 patients.35 They found that the view with the English blade was better than the view with the standard blade in 34%, no different in 54%, and worse in 11% of patients. For the 42 patients with a Cormack-Lehane grade of 3 or worse with one blade, the view was rated better with the English blade than the standard blade in 60%, worse in 7%, and no different in 33% of patients.35 Yardeni and colleagues, in performing an in vitro technical analysis of various blades, concluded that the English Macintosh 4 provided the best results, surpassing those delivered by the American size 4 and English Macintosh 3 blades, even at shallow insertion depths.36 The flange heights on English Macintosh 4 and 3 blades are similar, but on the American Macintosh, the proximal flange on the 4 is much larger than the 3, and the larger size confers a significant risk of dental injury in some patients.
Levitan advocates the use of a narrow-flange-height Macintosh 4 German or English design on all adult emergency cases; if the full depth of the blade is not required, the flange height with these blades does not cause a problem (its height is the same as a Macintosh 3), but if more blade is needed, the depth can be increased without the need to switch the blade.37 As stressed originally by Chevalier Jackson, epiglottoscopy must always be performed to find the epiglottis before making any effort to expose the larynx; otherwise, a large blade can be inserted too deeply and fail to identify landmarks.38
3 German Macintosh Blade
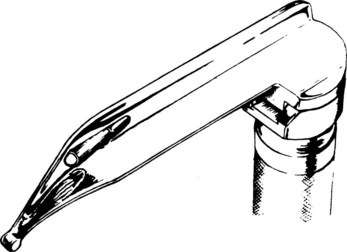
Heine, the German medical instrument company, pioneered incorporation of a rectangular, large (4.3-mm), glass-fiber bundle combined with a small flange height and full-length flange similar to that of an English Macintosh (Fig. 24-20). Like the English Macintosh, it has a small light-to-tip distance. When paired with rechargeable batteries and especially with an LED bulb, this large fiber bundle provides an extremely intense, white light. This design is easy to clean because it has no irregular surfaces. Other manufacturers have copied this design, with some labeling it a German Macintosh.
4 Improved-Vision Macintosh Blade
In Macintosh’s original 1943 report of his curved-blade laryngoscope, the accompanying photograph of the blade showed a subtle flattening of the curve midblade. This disappeared early in the blade’s history, probably because of manufacturing considerations.32 In 1984, Gabor Racz described a modification in which the midportion of the Macintosh blade spatula was made concave (dorsally) in cross section, and the slight flattening of the midblade was reintroduced while the vertical step and flange were left intact (Fig. 24-21).39 The combined modifications should help to reduce the crest-of-hill effect whereby the midblade convexity can encroach on the direct line of sight from eye to laryngeal inlet. Racz reported that the blade had been used successfully in several cases in which conventional laryngoscopy had failed.39 The improved-view Macintosh is commercially available in multiple sizes from several manufacturers.
5 Bowen-Jackson Blade
Recognizing that curved and straight blades had advantages and disadvantages, Ronald Bowen and Ian Jackson attempted to create a blade that could be used in all difficult situations. The resulting blade is almost straight, but it has a fairly marked distal curve (Fig. 24-22). The distal beak of the blade is bifid to allow straddling of the glossoepiglottic fold. The maximum depth of the vertical step is substantially less than that of the Macintosh blade, and it occurs midblade and tapers proximally to allow its use in patients with limited mouth opening or prominent teeth. When attached to the handle, the blade forms an angle of 100 degrees to help avoid contact with the chest.40
6 Left-Handed Laryngoscope
A mirror-image version of the Macintosh blade exists for use with the right hand. Inappropriately referred to as the left-handed laryngoscope, it is identical to the regular Macintosh blade except for the reversed configuration of the flange. Potential uses include laryngoscopy of patients in the right lateral decubitus position, procedures in those with right-sided facial or oropharyngeal abnormalities, and procedures in which the endotracheal tube (ETT) should be located on the left side of the mouth.41,42
7 Curved Blades with Exaggerated Distal Curvature
Several blades have been described with a more acute curvature of the distal spatula than that of the Macintosh. Of historical interest, the Gubuya-Orkin blade, described in 1959, was unique in having an S-shaped blade with a malleable distal 3 cm. The investigators described bending it through a range of 15 to 45 degrees, with an optimal position thought to be 35 degrees from the horizontal for indirect lifting of the epiglottis (Fig. 24-23).43 Found to be effective in some cases in which Macintosh laryngoscopy had failed, the Gubuya-Orkin blade can be considered a forerunner of other blades with marked fixed or variable distal curvature.
Unlike the Macintosh blade, the Blechman blade has an accentuated curve at its distal tip. Its reverse-Z vertical step and flange begin distal to the block of the blade and extend only to within 5 cm of the blade tip. The curved Fink laryngoscope blade similarly has a sharper curve at the distal spatula and reduced vertical step proximally compared with the Macintosh. The ULX Macintosh (Upsher Laryngoscopy Systems, Mercury Medical, Clearwater, FL) blade has a more pronounced curve throughout the entire blade length than the standard Macintosh. The Wiemers or Freiburg blade, marketed in Europe, has less initial curvature than a Macintosh and has an acutely curved tip (Fig. 24-24).44 As a group, these blades may have utility in patients with limitations of mouth opening, impaired head and neck mobility, or prominent upper incisors, in whom the tip of a Macintosh blade may fail to engage the glossoepiglottic fold at the appropriate angle. More specific indications for these blades await scientific evaluation.
B Miller and Related Straight Blades
1 Miller Laryngoscope Blade
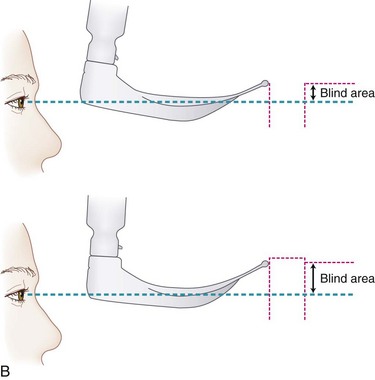
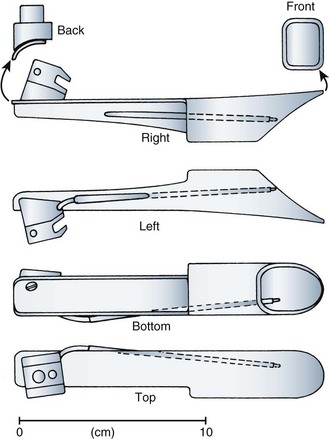
The use of straight blades, with entrapment and direct lifting of the epiglottis, was the common laryngoscopic technique when Miller introduced his modification of the straight laryngoscope blade in 1941. The blade he described was longer than the medium-sized blades available at the time, had a comparatively smaller flange height, was narrower at the tip, and featured a gradual curve starting 2 inches (5 cm) from the distal end (Fig. 24-25).17 Miller contended that the smaller flange height would allow less mouth opening (permitting freer anterior movement of the mandible) and less potential for damage to the teeth. Although Miller’s original design could accept a 38-F tube down the barrel, the flange height of modern Miller blades has become substantially smaller, and an adult-sized tracheal tube cannot fit down a Miller size 3 blade. Miller warned that the lumen should not be used for this purpose in his original description of the design.17 With a smaller degree of mouth opening, Miller conceded that available room for tube manipulation would be less and that a stylet would be desirable.17 In 1942, Cassels echoed Miller’s contention that a greater distal curvature of the straight blade would facilitate exposure of the laryngeal inlet, accompanying his report with an elegant diagram to help illustrate his theory.45 For a given position of the base of a straight blade between the teeth, especially when the mouth opening is limited, a curved distal tip can enable the laryngoscopist to visualize a more anterior aspect of the laryngeal inlet (Fig. 24-26). The Miller laryngoscope blade continues to be a commonly used straight blade.
2 Magill, Flagg, and Guedel Blades
The Magill blade, first marketed in 1921, is mainly straight, with a U-shaped step and flange concave to the right. The step and flange continue to within an inch of the end of the blade. The Flagg blade is straight with a very slight curve at the distal tip and was originally designed for use with Flagg catheters and tubes. With a light source placed quite distally, the C-shaped cross section tapers gradually from its proximal to distal end (Fig. 24-27).46 The Guedel has an extremely large spatula and U-shape flange that is concave to the right. Its distal tip has slightly more curve than the Flagg, and the blade is angled on its base to result in a 72-degree angle with the handle to help promote a lifting action instead of using the teeth as a fulcrum.
3 Soper Blade
The straight Soper blade originally was described in 1947. When he was Wing Commander in the Royal Air Force Medical Division, Robert Soper developed the blade in response to the Macintosh’s occasional failure to elevate a long, “flabby” epiglottis.47 Although described as a modification of the Macintosh blade, it is largely straight except for a slight distal curvature. It retains the reverse-Z-shaped vertical step and flange of the Macintosh blade. A small, transverse slot cut into the blade a few millimeters from the tip is designed to help prevent the epiglottis from slipping off the blade (Fig. 24-28). The Soper blade is still commercially available in adult and pediatric lengths.
4 Gould Blade
Gould, in 1954, modified a Soper blade by (1) lining the flange with rubber and reducing the proximal vertical step and (2) lengthening and blunting the distal end of the blade (Fig. 24-29). He made a similar modification to a Macintosh blade, although neither version attained widespread use.48
5 Wisconsin Blades
The Wisconsin blade is a large, straight blade with a circular flange. The original design had a slightly flared distal flange. The Whitehead modifications—the Wis-Foregger and Wis-Hipple blades—are variations of the original Wisconsin design with slightly modified flanges, bulb locations, and spatulas (Fig. 24-30).46
6 Snow Blade
In 1962, Snow recognized the advantages of a straight blade in certain difficult situations, but finding difficulty with epiglottic entrapment with the Wis-Foregger and problematic ETT passage with the Miller, he modified a straight blade by slightly curving the distal tip beginning 1 inch (2.5 cm) from its semirounded beak. He also increased the vertical step and flange combination to create a C-shaped groove that was concave to the right, which allowed a better view and easier tube passage (Fig. 24-31).49
7 Phillips Blade
Otto Phillips developed a blade similar to the Snow blade. In 1973, Phillips described it as a combination of the shaft of the Jackson blade and curved tip of the Miller blade. He thought that the Jackson shaft offered a good conduit for ETT passage and reasoned that the curved tip of the Miller would help to lift the hyoid bone and attached structures, affording good visualization of the glottis.50 The light bulb is located on the left side of the blade, and in some versions of the blade, it may be unprotected from the tongue, although other versions use a fiberoptic carrier shielded by the vertical step (Fig. 24-32). The C-shaped vertical step and flange are less complete than a Wisconsin arc, are concave to the right, and extend to within 5 cm of the end of the blade. Phillips conducted an observational study of the use of the blade in the hands of experienced and inexperienced users in more than 1000 patients and found that successful intubation was achieved on the first attempt with the Phillips blade in 84% of cases.50 The Phillips blade is produced in size 1 for pediatric patients and size 2 for adult patients. It is available commercially and has relatively widespread use.
8 Schapira Blade
Max Schapira described a blade that is straight with a slight distal anterior curvature but with a minimal vertical component and no horizontal flange (see Fig. 24-30).51 The blade remains available commercially.
9 Henderson Laryngoscope
The Henderson laryngoscope blade (Karl Storz, Tuttlingen, Germany) is a modification of the straight blade. It was introduced by John Henderson of Glasgow, an enthusiastic proponent of straight-blade laryngoscopy in anesthesia practice.52,53 The Henderson blade is straight over its entire length and has a semicircular vertical step and flange, resulting in a wide slot that permits easy ETT entry, passage, and exit. The step, flange, and light carrier continue to within 2.5 cm of the blade tip, which with the straight blade is designed to maximize light delivery. The fiberoptic light carrier is shielded from the tongue within the lumen of the blade (Fig. 24-33). The distal tip of the blade has a rounded, knurled edge, which can be seen when viewing down the barrel. Having a visible distal tip makes it easy to determine whether the blade has been advanced far enough to lift the epiglottis; when using a Miller blade or others with a distal upturned tip, repeated rounds of advancing and lifting are often required until the epiglottis is controlled.
The Henderson blade is available in small and large sizes. The 148- and 192-cm-long blades have lumens sufficiently large to accommodate passage of ETTs with 7- and 8-mm inner diameters (IDs), respectively. Henderson evaluated the blade in 300 patients and reported easy positioning of the blade in 91%, a grade 1 view in 93%, and successful direct ETT passage on the first attempt in 97% of patients.53 He published a case series documenting successful glottic exposure and intubation using paraglossal straight blade laryngoscopy in situations in which the Macintosh blade had failed.52
10 Dörges Universal Blade
The Dörges universal laryngoscope blade has been described as an effort to create a single blade with utility in many situations.54 The blade is mainly straight with a slightly curved distal end, enabling its use by direct or indirect elevation of the epiglottis. It tapers gradually from the heel to 11 mm at its tip, corresponding to the width of a Macintosh 2 blade tip. The working length of 125 mm, however, is between those of Macintosh 3 and 4 blades. The angle of the blade tip with the handle is 76 degrees, as opposed to the usual 58 degrees of the Macintosh blade, potentially facilitating blade insertion into patients with a prominent sternal area. Similarly, the lower profile, 15-mm, reverse-Z-shaped vertical step and flange may facilitate the blade’s insertion in patients with limited mouth opening. Two marks corresponding to a patient weight of 10 or 20 kg on the front and rear of the blade serve as a rough guide for insertion depth when using the blade in a pediatric patient (Fig. 24-34).
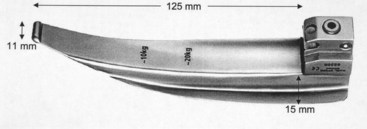
Figure 24-34 The Dörges universal laryngoscope blade has markings that indicate appropriate insertion depths for pediatric use.
(From Gerlach K, Wenzel V, von Knobelsdorff G, et al: A new universal laryngoscope blade: A preliminary comparison with Macintosh laryngoscope blades. Resuscitation 57:63–67, 2003.)
11 Grandview Blade
The Grandview laryngoscope blade (Hartwell Medical, Carlsbad, CA) was designed by a paramedic in the United States, and it has achieved widespread use in U.S. Emergency Medical Systems.55 It has a curvature somewhat similar to that of a Dörges blade, in that it is mostly straight but has a slightly bent distal tip. Its primary unique feature is its massive proximal spatula, and it is advertised as “the tongue tamer” (Fig. 24-35). Another feature of the Grandview is its use of a super-bright LED bulb. It comes in two sizes and in a reusable or single-use version. Its reusable version has a gold-colored tip to make tip visualization easier. There are no published clinical case series validating the Grandview blade as superior to a conventional Macintosh, although anecdotally, the manufacturer has received very positive feedback, and it has been successful commercially. Inadequate tongue control is a frequent error among novice intubators, and the larger spatula blade may be valued by those who intubate less frequently. Conversely, a larger blade volume may make it harder to reach the larynx in patients with a small displacement space (i.e., thyromental distance) and a large tongue-to-pharynx ratio.
C Blades with Fixed and Various Degrees of Acute Angulation
1 Belscope
a Description
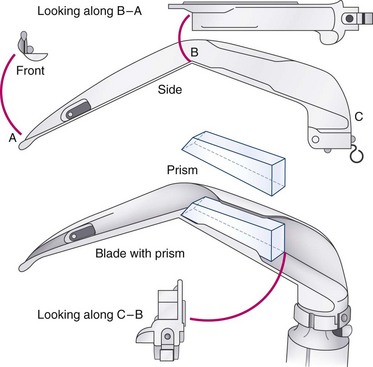
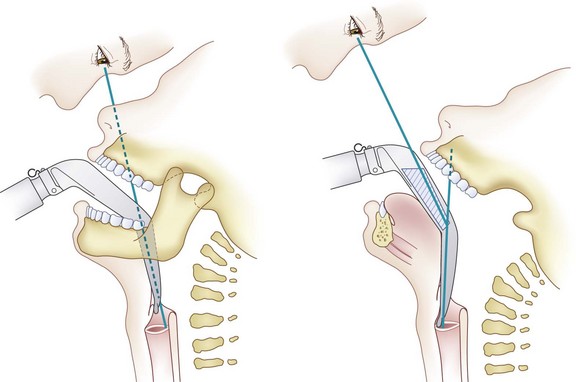
The Bellhouse laryngoscope, or Belscope, is a straight blade bent 45 degrees at its midpoint.56 The blade comes off the handle at a slightly offset angle and has a vertical step less than that of a Macintosh blade and no horizontal flange (Fig. 24-36). The Belscope is available in three lengths from tip to angle: 6.7, 8, and 9.3 cm. Because the blade typically is used to elevate the epiglottis directly, less compression and anterior displacement of the tongue may be needed to obtain a view of the larynx. The Belscope may be useful when poor atlanto-occipital extension, a large tongue, or a short mandible hinder optimal positioning of a Macintosh laryngoscope blade. If visualization remains suboptimal with the Belscope, a prism can be attached proximal to the angulation to provide an indirect view of the glottic opening.
b Blade Use
Without the prism, the Belscope can be used in a fashion similar to a straight blade. Displacing the tongue to the left, the blade may be inserted into the proximal esophagus and then withdrawn to expose the laryngeal inlet. Retraction of the upper lip may be advantageous. Because of the blade’s 45-degree angulation, there may be less chance of the proximal blade applying pressure to the upper teeth. In the event that the larynx is not primarily visualized with the blade, use of the prism (suitably defogged) rotates the image of the larynx by 34 degrees (Fig. 24-37). Often, a styleted tracheal tube curved anteriorly is necessary for advancement through the glottis.56
c Clinical Experience
Bellhouse reported his experience of 3500 intubations in which he used the Belscope without failure.56 The report included a subseries of 12 patients in whom the Belscope successfully exposed the glottis after the Macintosh had failed. Bellhouse emphasized the need for practice in the use of the blade because its feel was different from that of other blades.56 Separately, Mayall reported a second series of 12 patients with Cormack-Lehane grade 3 laryngoscopies with the Macintosh blade, all of whom were converted to a “good view of the cords” with the Belscope without use of the prism.57 In a crossover study by Sultana and colleagues comparing Macintosh and Belscope laryngoscopy, of 22 grade 3 views obtained, 19 were with the Macintosh blade. Tube passage using the Belscope required lip retraction by an assistant more frequently than with the Macintosh.58
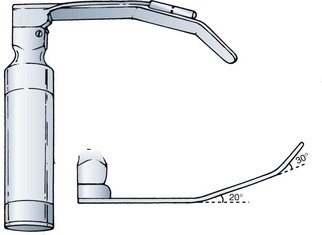
2 Choi Double-Angle Laryngoscope
In 1990, Choi described a double-angled blade with the spatula incorporating two incremental angles—the proximal (20 degrees) and the distal (30 degrees) (Fig. 24-38).59 The spatula and beak are wide and flat for tongue or epiglottis control, and there is no vertical step or flange. The light source lies along the left edge of the blade between the two angles, with the bulb pointing toward the center of the glottis. The blade can be used with direct or indirect lifting of the epiglottis. It is commercially available in one adult and one pediatric size.59
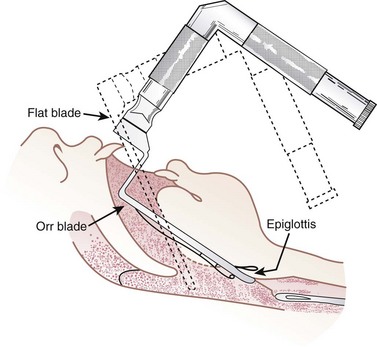
3 Orr Laryngoscope
The Orr blade was developed to help eliminate contact with the upper teeth. Two right-angle bends (Fig. 24-39) are designed to enable the blade to sit down inside the mouth, shifting the fulcrum into the pharynx and away from the teeth. It typically is used to elevate the epiglottis directly, and the ETT is advanced from the right side of the mouth. Rarely used now, the Orr blade was available in two lengths.60
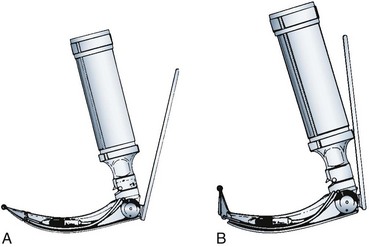
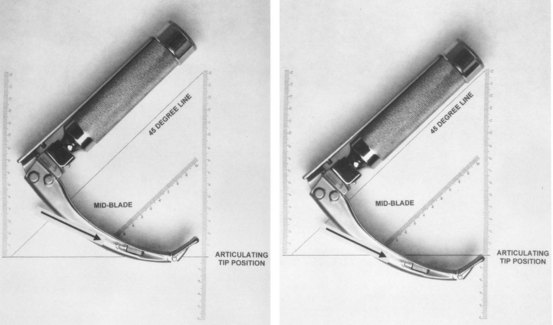
4 Levering Tip Laryngoscope
a Description
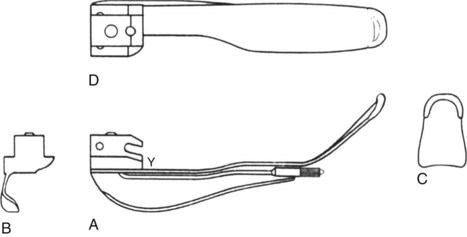
The levering tip or articulating laryngoscope (Corazzelli-London-McCoy [CLM] blade, Mercury Medical, Clearwater, FL) is a modification of standard curved (and straight) laryngoscope blades. A curved blade first described in 1993 is marketed by several manufacturers (e.g., the Flipper, Rüsch, Duluth, GA; Heine Flex Tip, Heine Optotechnik, Herrsching, Germany). These laryngoscope blades have a hinged distal tip activated by a lever that lies adjacent to the handle of the laryngoscope. Depressing the lever toward the handle elevates the tip, located 25 mm from the end of the blade, by approximately 70 degrees (Fig. 24-40).61 The lever acts on the tip through a spring-loaded drum on the proximal end of the blade, which pushes a shaft linking with the distal hinge. In the resting position, the blade looks and acts like a standard blade, with the vertical step of the distal adjustable tip locking with that of the rest of the blade. The blade-lever assembly can be used with any compatible standard handle. When activated, the levering tip laryngoscope may have the advantage of having a fulcrum at a point lower in the pharynx, helping to provide an optimal tip angle and contact with the hyoepiglottic ligament in situations such as limited mouth opening, a large tongue, or prominent or overriding upper teeth.
c Clinical Experience
Since the introduction of the CLM, several case reports have attested to its value in difficult situations.62–69 Subsequent prospective series have confirmed the CLM’s utility in some difficult situations and confirmed clinical suspicions that its use in otherwise easy situations may worsen the view. Studies have been consistent in their findings that without cervical spine precautions, improvement with the use of blade tip activation from Cormack-Lehane grade 3 views to grade 2 or better is significant, occurring in 44% to 91% of cases.44,62–69 In most studies, the CLM blade has failed to meaningfully improve Cormack-Lehane grade 4 views.
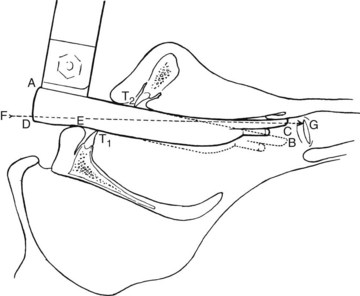
The levering tip blade is less useful in otherwise easy laryngoscopies. Although one report documented a 66% improvement in 38 patients (arytenoids only) with Cormack-Lehane grade 2 laryngoscopic views, the same report revealed a 22% overall incidence of a worsening view obtained with tip activation, all in patients with Cormack-Lehane grades 1 and 2.69 In easy laryngoscopic situations, the blade tip easily engages and can lift the hyoepiglottic ligament and hyoid bone at the appropriate angle. With no potential for further upward travel, blade tip activation instead forces the midportion of the blade downward and into the direct line of sight, potentially obscuring the view (Fig. 24-41).70 The better the view before tip activation, the more likely this phenomenon appears to be.
Several studies have documented that the improvement in laryngoscopic view obtained with tip activation of the CLM is less than that obtained by external laryngeal pressure,67,68,70 although application of external laryngeal pressure and tip activation has an additive effect.67 McCoy and colleagues found that the force incurred when using the levering tip blade was significantly less than that needed to visualize the larynx with the Macintosh blade.62 There was no increase in heart rate, mean arterial pressure, or plasma norepinephrine levels with use of the levering tip blade,62 possibly because there was less need to provide forward displacement of attached structures while elevating the epiglottis.
The CLM blade may be useful in patients requiring cervical spine precautions. In three studies simulating cervical spine precautions with use of manual in-line stabilization or application of a cervical collar, activation of the levering tip improved the Cormack-Lehane laryngeal view by at least one grade in 45% to 74% of patients, and in the patients with a grade 3 view, conversion to a grade 2 or better view occurred in 83% to 92% of cases.71–73 In the 319 patients enrolled in these three studies, the view was worsened by use of the activated CLM blade in only one case. A separate study looking at head extension using external anatomic markers during CLM laryngoscopy demonstrated that 6 to 8 degrees less head extension was necessary for arytenoid-only and full-glottic exposure compared with Macintosh blade use.74 MacIntyre and colleagues, using lateral radiographs to look at cervical spine movement with Macintosh and CLM blade use, could not demonstrate a significant difference in the degree of extension occurring between C0 and C3.75 In a cadaver series with surgically induced lesions at C5-C6, Miller, Macintosh, and McCoy blade laryngoscopy use was assessed fluoroscopically. The Miller was superior to the Macintosh or the CLM blade at minimizing axial distraction, but no significant difference in anteroposterior displacement or angular rotation at the level of the lesion was demonstrated between blades.76
5 Flexiblade
a Description
The Flexiblade (Arco Medic, Omer, Israel) incorporates a flexible component into a rigid blade. This direct laryngoscope is flexible in the intermediate portion of the blade. Activation of the trigger, which, unlike that in the CLM, lies along the front of the handle, results in variable flexion of six intermediate segments located 3.5 to 10 cm from the blade’s tip. This adjusts the blade’s curvature through a 20-degree arc, going from a shape similar to that of a Miller blade to that of a Macintosh blade (Fig. 24-42).77 The Flexiblade can be attached to a standard laryngoscope handle or a remote light source by a fiberoptic cable. It is available in three sizes that correspond roughly to Macintosh 2, 3, and 4 blades.
c Adapters
Perera and coworkers evaluated the Flexiblade in 200 patients.78 In patients with an initial Cormack-Lehane grade 3 view with the Flexiblade in the neutral position, blade activation converted the view to grade 2 or 1 in 84% of cases. In this series, blade activation worsened the view in only four patients, and as with the CLM blade, all of those patients had grade 1 or 2 views before blade flexion. Yardeni and colleagues77 performed an in vitro technical analysis of the blade after the technique described by Marks and associates28 and confirmed that the Flexiblade behaves in fashion similar to that of a Miller or Macintosh blade in the neutral and fully elevated positions, respectively.78
D Blades Designed for Other Anatomic Variants
1 Blades with Reduced Vertical Step
Several blades have been designed with a reduced vertical step. In theory, this should help with blade insertion in patients with limited mouth opening and pose a lower risk to the upper teeth. The risk is increased if the laryngoscopist levers on the teeth, but studies have demonstrated that the horizontal flanges of well-used Macintosh blades show significant signs of wear at the level of the upper teeth, suggesting frequent contact with the blade, and other studies have demonstrated that even experienced clinicians generate significant axial force on the upper incisors.79,80 Although these findings may suggest that one of the functions of the vertical step is to maintain mouth opening through contact with the upper teeth, most clinicians prefer to minimize contact with the upper teeth. To address the issue of step or flange contact with the upper teeth, several modifications to blades have been made.
a Bizzarri-Giuffrida Blade
The Bizzarri-Giuffrida blade was developed in response to the problem of the Macintosh blade’s vertical step and flange proximally touching the upper teeth, causing difficulty in rotation of the blade into the hypopharynx and full insertion into the valleculae, particularly in patients with limited mandibular mobility. The blade is curved in fashion similar to that of the Macintosh blade and omits the vertical step, with the exception of a minimal amount at midblade, where it is needed to protect the light carrier (Fig. 24-43). The experience of several hundred patients was “complete satisfaction,” particularly by those with buckteeth, a receding jaw, bull neck, or an anterior larynx. The investigators reported successful use of the blade during awake direct laryngoscopy.81
b Callander-Thomas Blade
In 1987, Callander and Thomas described a blade incorporating a reduction in the proximal portion of the vertical step and flange of the Macintosh blade (Fig. 24-44).82 The reduction in the step height was postulated to improve the blade’s utility in patients with limited mouth opening and to decrease the risk of dental damage.82
c Bucx Blade
A modification similar to the Callander-Thomas blade was made by Bucx and colleagues after technical analysis suggested it to be a good model.83 This blade had a Macintosh-style curve and had the vertical step and flange reduced to a minimum from blade base to 8 cm from the blade tip. Bucx and coworkers clinically evaluated the blade, randomly assigning 46 patients to two groups for laryngoscopy and intubation with a regular Macintosh or the modified blade.84 Although the mean force exerted on the maxillary incisors was significantly reduced in the modified-blade group, there was a decided tendency toward anteflexion of the head during laryngoscopy with the modified blade and an increased need for the assistant to retract the upper lip to aid with intubation. Although the accepted purpose of the vertical step of laryngoscope blades is control of soft tissue, especially the tongue, this study suggests the possibility that the vertical step and flange at the level of the upper teeth may help to maintain mouth opening and counteract the tendency of the head to anteflex during laryngoscopy.
d Onkst Blade
In 1961, Onkst modified a Macintosh 3 blade to help avoid undue pressure on the upper incisors. The proximal portions of the blade’s vertical step and flange are hinged and, although normally kept in the upright position by a weak spring, allow the vertical step and flange to fold down in response to pressure on the teeth, theoretically avoiding dental damage (Fig. 24-45).85
e Racz-Allen Hinged-Step Blade
The Racz-Allen blade has a hinged step and flange.86 The vertical step of this modified straight blade is maintained in position by a spring. During laryngoscopy, any pressure on the vertical step from the upper teeth causes an upward and lateral deflection of the hinged portion. The main blade is convex in cross section to a greater extent than the Miller blade to help maintain vision when the concave, hinged portion is displaced. A threaded shaft is removable, allowing disassembly of the two portions of the blade for cleaning (Fig. 24-46).86 The blade length is intermediate between a Miller 2 and 3. Racz and Allen reported more than 2000 successful intubations at their institution with the blade.86
2 Blades and Devices That Avoid Chest Impingement
a Modified Blades
The Polio blade was introduced by Foregger in 1954 and designed for use during intubation of patients in iron lung respirators. It features a Macintosh-style blade that attaches to a battery handle at an obtuse angle of 170 degrees (Fig. 24-47).87 It may still be used when a regular handle attachment setup encounters forward impingement (e.g., obesity, kyphosis with barrel chest deformity, mammary gland hypertrophy, a short neck),87 although the extremely obtuse angle of the blade to the handle may make it difficult to generate an adequate lifting force. For obstetric cases, Kessell modified a Macintosh blade’s block so that the blade comes off the handle at an angle of 110 degrees instead of the usual 90 degrees (Fig. 24-48).88 Beaver described a straight blade with a handle set at 25 degrees to facilitate intubation of patients in “box” respirators.89
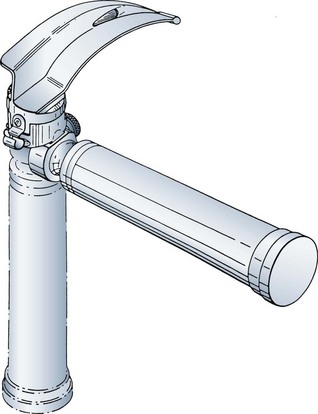
b Modified Handles
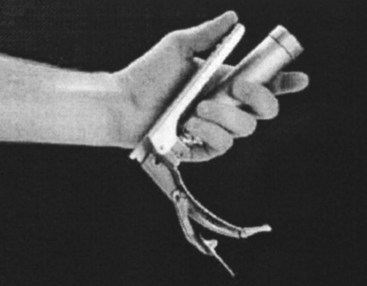
Handles with one half of the length of regular laryngoscope handles have been used to help avoid chest or breast impingement (Fig. 24-49). Patil and colleagues described a shortened, adjustable-angle laryngoscope handle incorporating a blade-lock device that allows blade positioning at 180, 135, 90, or 45 degrees to the handle (Fig. 24-50). When there is potential impingement of a laryngoscope handle on a patient’s chest, the instrument can be inserted at 180 degrees; the angle of the blade to handle then can be reduced to 135 or 90 degrees, allowing laryngoscopy to be performed.90
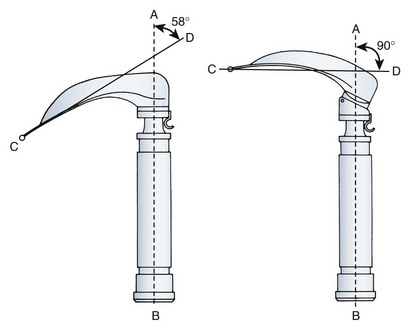
c Adapters
The Jellicoe adapter was described to overcome the true angle between the Macintosh blade tip and handle of 58 degrees. The adapter increases this angle to 90 degrees (Fig. 24-51), facilitating blade entry into patients’ oral cavities in some situations.91 In 1991, Dhara and Cheong described a multiple-angle laryngoscope adapter that fits between the handle and blade and that provides working angles of 65, 90, 110, 130, 150, and 180 degrees between blade and handle.92 The Yentis adapter is a 2.5-cm cube block that fits between a standard handle and laryngoscope blade (Fig. 24-52). It allows insertion of the blade into the patient’s mouth with the handle swung 90 degrees to the right. After the blade is inserted, the handle can be swung back to the normal position for laryngoscopy.93
3 Blades for a Small Infraoral Cavity
a Bainton Blade
The Bainton blade is unique in this collection of blades because it is designed specifically for pathologic conditions that obliterate the hypopharynx. The very large and long straight blade is compatible with regular laryngoscope handles. The distal 7 cm of the blade has a squared, tubular design to help create a hypopharyngeal space where there may be none (Fig. 24-53). The lumen accepts an ETT up to size 8.0, and an intraluminal light source ensures that lighting is not compromised by tissues crowding the bulb. Bainton successfully tested his prototype in dogs with artificially induced hypopharyngeal swelling and in a small series of 12 patients with edematous conditions of the pharynx (one with a friable, bleeding tumor).94
b Diaz Pediatric Tubular Laryngoscope
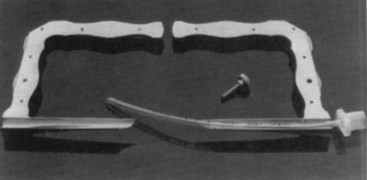
The Diaz pediatric tubular laryngoscope features a U-shaped handle and blade assembly. With a gradual distal curve, the blade is composed of two halves that are held together with a removable screw. A tubular scope with a straight blade design results when the two halves are attached (Fig. 24-54). The enclosed channel houses two light sources (one on each side) that are powered from an external fiberoptic light source. Endotracheal intubation is accomplished through the lumen of the scope, which must be disassembled by removal of the screw before the scope’s removal from the patient.95
E Pediatric Laryngoscopes
1 Oxford (Bryce-Smith) Blade
The Oxford, or Bryce-Smith, blade, was intended for neonates but is applicable for infants up to age 3 months. Primarily a straight blade, it tapers gradually from its proximal width of 1.8 cm to 1 cm distally. The step and flange are U-shaped, and although the distal 2.5 cm is open, a slight distal step remains for tongue control. The horizontal flange is quite broad proximally, helping to prevent the upper lip from obscuring the view and potentially helping in difficult cleft-palate situations (Fig. 24-55).96
2 Seward Blade
The Seward blade was created for use in the neonate, but additional sizes allow it to be used in children up to age 5 years. The primarily straight blade is 10.5 cm long, has a mild distal angulation and sharply tapering width, and ends in a thickened beak. The adult bulb is protected from the tongue on the inside of the reverse-Z-shaped step and flange (Fig. 24-56).97
3 Robertshaw Blade
Robertshaw originally modified a baby Soper straight blade by slightly curving the distal end while modifying the step and flange from the Soper’s reverse-Z to a slight C shape. The light source was well protected from the tongue inside the vertical step. A subsequent modification exhibited additional leftward bending of the vertical step, creating a wider channel for visualization (Fig. 24-57).98
4 Other Blades
The Propper, or Heine, blade is straight with a slightly curved tip. The horizontal flange is in the reverse-Z configuration, curving away from the blade.46 Other modifications have been made for pediatric use. Matsuki described a widened, thin blade attached to the handle at a slightly obtuse angle to aid in control of the infant’s tongue.99 Rokowski and Gurmarnik described a modification of the standard Miller 0 blade in which the distal portion of the blade was widened to a triangular configuration for neonates or to a circular configuration for infants.100 The width of the flange was reduced by 2 mm without modifying the height of the step to improve the area available for ETT manipulation and laryngeal visualization. Diaz combined several of the improvements in pediatric blades into one unit by modifying a Miller 1 blade to include an attached oxygen insufflation port, a corrugated lingual surface, and outward bending of the C-shaped flange to widen the cross-sectional area.101 No formal evaluation has been published.
F Laryngoscope Blades with Accessory Devices
1 Blades with Integrated Oxygen Delivery Channels
Some blades, mainly in pediatric sizes, are available with integrated channels designed for the insufflation of oxygen during direct laryngoscopy. The concept has evolved from earlier reports of oxygen insufflation through feeding tubes taped to blades during laryngoscopy in neonates and infants.102,103 Hencz described permanently affixing a wide-bore aspirating needle for the same purpose.104 Todres and Crone formally described the Oxyscope laryngoscope, which incorporates a built-in oxygen insufflation channel.105 It was originally made available in Miller 0 and 1 blades and subsequently in Macintosh blades. Studies during laryngoscopy in spontaneously breathing, anesthetized infants have demonstrated higher oxygen tensions with oxygen administration through these blades.105,106 They continue to be marketed under various brand names, mainly in the Miller configuration.
2 Blades with Integrated Suction Channels
Some adult and pediatric blades have an integrated suction channel or blades that allow suction through an oxygen administration port.107–109 The modified blades allow suctioning during ongoing laryngoscopy and may be useful in patients with copious secretions or emesis or in situations such as bleeding after tonsillectomy. The Khan blade has a 1.75-mm-ID tube welded to a straight blade with a proximal hub angled so that the laryngoscopist’s thumb can occlude a port to control the amount of suction applied.108 Tull suction blades, available in Miller and Macintosh versions, have a finger-controlled valve lying next to the laryngoscope handle to enable the laryngoscopist to apply suction at will.46
3 Blade with a Secondary Ultraviolet Light Source
In 2009, Intubrite introduced a new concept in laryngoscope blade illumination that combined a white LED light with a second ultraviolet (UV) or black light.110 The UV light is a higher frequency (wavelength) than white light that lies in the invisible part of the electromagnetic spectrum. It overpowers the lower end of the white light spectrum, where reds and yellows cause a whitewash effect. According to Intubrite, the UV light reduces the scatter from standard white light and improves visualization of the airway. The ligamentous vocal cords contain high levels of phosphorus that, when struck by the black light (UV), phosphoresce (Fig. 24-58). The company claims that by varying the wavelength of UV light and adding a spectrally specific white LED light, this illumination system better outlines the texture and structure of the airway and diminishes the reflectivity from fluids within the passage.
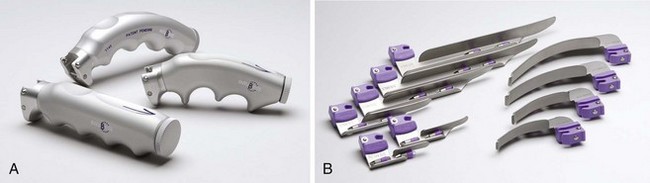
4 Ultra-lightweight Tactical Laryngoscope
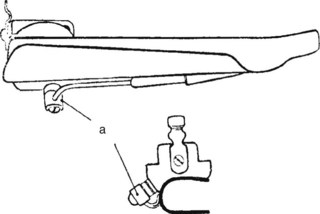
The TruLite (Truphatek International Ltd., Netanya, Israel) is a single patient–use laryngoscope, which combines a low-profile Macintosh or Miller metal blade hinged to a small plastic handle (Fig. 24-59).111 With two AA batteries, the laryngoscope blade and handle weighs only 120 g. The LED light provides a bright white light. The preconfigured and attached metal blade, extreme light weight, and small overall size and packaging make it ideal for tactical settings and use in aircraft medical operations. It is offered in three Miller sizes (1 to 3) and four Macintosh sizes (1 to 4), all of which have small, narrow flange heights.
V Rigid Indirect Laryngoscopes with Optically Assisted Views
Rigid indirect laryngoscopes enable a view of the laryngeal inlet indirectly through a fiberoptic bundle, video camera, or other optical aid. Examples of optically aided laryngoscopes include the Siker blade with its built-in mirror, blades using attachable prisms (e.g., Huffman, Belscope), and the Viewmax and EVO2 blades, which have integrated optical rods. Other indirect rigid laryngoscopes deliver an image endoscopically through a fiberoptic bundle or using video technology. The ensuing discussion is limited to mirrored blades and those that use prisms or optical rods. Fiberoptic instruments and video laryngoscopes are covered in Chapters 19 and 25, respectively.
A Siker Laryngoscope
In 1956, Siker described an angled laryngoscope with an incorporated reflecting surface. The portion of the blade distal to the mirror is angulated at 135 degrees from the proximal section (Fig. 24-60). The stainless steel mirror is attached to the blade by means of a copper jacket to facilitate conduction of heat from the patient, thereby minimizing fogging of the mirror.112 After blade insertion, if the laryngeal inlet cannot be directly visualized, the mirror can be used to indirectly identify the epiglottis and then the cords. Facility with the use of this blade takes some experience because the mirror inverts the reflected image. A styleted tube is essential; as the tube enters the larynx, it appears to move in a posteroinferior direction. In his original publication, Siker described the blade’s use in 100 unselected patients. Laryngoscopy failed in just one patient because of excessive blade length. In three other patients with failed laryngoscopy and intubation with standard blades, the Siker succeeded. He emphasized the need for practice in the use of the blade.112
B McMorrow-Mirakhur Mirrored Laryngoscope
McMorrow and Mirakhur described a modification of the levering tip laryngoscope that incorporates an adjustable mirror.113 Looking like a regular CLM (McCoy) laryngoscope in the resting position (Fig. 24-61), the McMorrow-Mirakhur laryngoscope can be operated as both a regular Macintosh blade or levering tip blade, as previously described. The difference is that it has a mirror lying posteriorly on the blade. As the levering tip is activated by moving the control lever toward the laryngoscope handle (Fig. 24-62), the mirror is deployed posteriorly and inferiorly with respect to the blade. If necessary, further depression of the control lever toward the handle changes the mirror pitch to a usable angle (Fig. 24-63), ultimately providing an additional 60-degree field of view compared with the Macintosh alone. If intubation is performed between the blade and the mirror, the scope has to be removed in its activated state. The blade should be heated or the mirror defogged before each use.
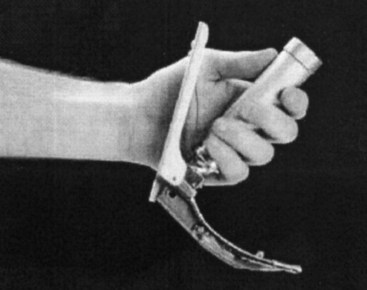
Figure 24-61 The McMorrow-Mirakhur laryngoscope in the resting position.
(From McMorrow RCN, Mirakhur RK: A new mirrored laryngoscope. Anaesthesia 58:998–1002, 2003.)
McMorrow and Mirakhur tested the laryngoscope in 15 patients presenting for elective surgery and compared it with the Macintosh and McCoy blades. Manual in-line neck stabilization was used to create difficult conditions for laryngoscopy, and all patients had Cormack-Lehane grade 3 views with the Macintosh blade. Using the McMorrow-Mirakhur blade with mirror deployment, the view was improved from grade 3 to grade 1 in 50% of patients and to grade 2 in 21%. The view was considered worse in 7%, and no change was seen in 21% of patients.113
C Huffman Prism
Although a prism had been described by Janeway in 1913, Huffman revisited the concept in 1968. He attached a Plexiglas prism to a Macintosh 3 blade by means of a steel clip. Because the image of the cords is deflected by approximately 30 degrees, Huffman theorized that less force on the tongue and hypopharynx would be needed to achieve laryngeal inlet visualization (Fig. 24-64).114 Subsequently, he affixed a second prism distal to the first to achieve a total refraction of 80 degrees. He used the resulting instrument to inspect the larynx at light planes of anesthesia, but he speculated that it would be a useful tool for difficult laryngoscopy.115 Huffman prisms continue to be available in various sizes for Macintosh blades.
D Rüsch Viewmax Laryngoscope
1 Description
The Viewmax (Rüsch, Duluth, GA) laryngoscope blade is similar in shape to a Macintosh, but it incorporates a removable lens system (i.e., Viewscope) ending in a proximal eyepiece, which can refract the distal image 20 degrees from the horizontal (Fig. 24-65). This has the potential to improve laryngeal inlet visualization compared with that obtained by direct vision. The blade of the Viewmax is wider than that of a standard Macintosh, and although the lens system provides some vertical component, the blade otherwise has little formal vertical step. With the resultant lessened ability to sweep the tongue to the left, the blade can be used midline in the patient’s mouth. The Viewmax is available in an adult and a pediatric size, corresponding to Macintosh size  and 2 blades, respectively. (The name Viewmax is also applied to another company’s [Timesco, London, England] version of the improved-view Macintosh blade.) The Viewmax has received limited investigation in manikins and cadavers with mixed results compared to a standard Macintosh blade.116–118
and 2 blades, respectively. (The name Viewmax is also applied to another company’s [Timesco, London, England] version of the improved-view Macintosh blade.) The Viewmax has received limited investigation in manikins and cadavers with mixed results compared to a standard Macintosh blade.116–118
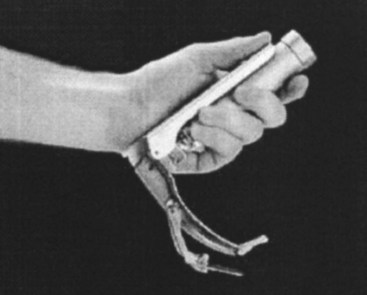
2 Truview EVO2
The Truview EVO2 uses an optical rod similar to the Viewmax, but it has an angulated shape (Fig. 24-66). The EVO2 is made by Truphatek International, which also manufactures the Viewmax, a product distributed by Rüsch. The EVO2 has a 42-degree refraction angle to its optical system. Instead of a gently curved shape like the Viewmax, the EVO2 is an angulated blade; the proximal two thirds of the blade are straight, although it has a wide spatula, and the last third of the blade has a steep upward angle and a flat tip like a standard Macintosh blade. The optical lens system runs straight along the proximal two thirds of the blade.
3 Clinical Experience
In pediatric and adult patients, the EVO2 has provided much improved laryngeal views compared with the standard Macintosh and Miller blades, although some studies have found slightly longer intubation times.119–125 In adult patients with anticipated difficult laryngoscopy, the EVO2 has significantly improved the laryngeal view. In a small case series of cervical spine patients intubated while in a cervical collar, the EVO2 provided full glottic visualization, whereas the standard Macintosh blade provided very poor or nonexistent views.120
VII Clinical Pearls
• Laryngoscope blades are not identical, and even within same designs (e.g., Macintosh and Miller), there is considerable variation among manufacturers. Depending on blade design, light source, battery type, and battery charge status, there can be a 500-fold difference in illuminance among blades in different clinical settings.
• With curved-blade laryngoscopes, design variables that are important to consider include the height of the proximal flange and the distance from the light source to the tip of the blade. Typically, a small flange is advantageous, and a shorter light-to-tip distance creates more light at the target.
• Low-profile Macintosh 4 blades (German or English designs) can be used in all adults, by varying the depth of insertion. When using a blade with more length than may be needed, the practitioner should identify the epiglottis on insertion and avoid passing by this critical landmark. Starting with a longer blade eliminates the need for switching out to a larger blade in emergency situations. A smaller flange permits insertion even in small-mouthed persons.
• Whiter, brighter light is provided by LED and fiber-illuminated systems than with traditional bulb-on-blade devices. Battery status and battery type are important to ensure good light output. Lithium, nickel-hydride, and other battery types have better discharge profiles (i.e., more uniform output) for high-drain devices such as laryngoscopes than alkaline batteries, which have long run times but very diminished output over time.
• Fiber-lit laryngoscopes have light sources in the handle and use glass or acrylic rods to transmit light from the base to the tip of the blade. Conventional blades have an electrical connection at the top of the handle and base of the blade. There is wide variation in bulb types, and LED, xenon, and halogen bulbs are available in both systems.
• LED bulbs have several major advantages over other bulb types. They produce a very white light that may improve discrimination of the epiglottis edge against the mucosa of the hypopharynx, and they use markedly less energy than filament bulbs. They have become so inexpensive that many companies offer disposable conventional blades with an LED bulb on the blade.
• Considerations in straight-blade design include the flange height, spatula shape, and location of the light source. A light source on the left flange may embed in tissue and provide poor illumination. Large-flange and large-spatula designs provide easier tube delivery but have to displace more tissue to get to the larynx. The shape of the distal tip (e.g., slightly upturned distal tip of the Miller design) affects how the blade is advanced to lift the epiglottis directly.
All references can be found online at expertconsult.com.
5 Burkle CM, Zepeda FA, Bacon DR, Rose SH. A historical perspective on use of the laryngoscope as a tool in anesthesiology. Anesthesiology. 2004;100:1003–1006.
6 Cooper RM. Laryngoscopy—Its past and future. Can J Anaesth. 2004;51:R1–R5.
7 Zeitels SM. Universal modular glottiscope system: The evolution of a century of design and technique for direct laryngoscopy. Ann Otol Rhinol Laryngol Suppl. 1999;179:2–24.
18 Macintosh RR. A new laryngoscope. Lancet. 1943;1:205.
37 Levitan RM. The airway cam guide to intubation and practical emergency airway management. Wayne, PA: Airway Cam Technologies; 2004.
38 Jackson C. Bronchoscopy and esophagoscopy: A manual of peroral endoscopy and laryngeal surgery. Philadelphia: WB Saunders; 1922.
1 Babington BG. Lecture to the Hunterian Society. London Medical Gazette. 1829;3:555.
2 Garcia M. Observations on the human voice. Proc R Soc Lond. 1855;7:399–410. Available at http://books.google.com/?id=o6PYNM7RNwkC&pg=PA399&lpg=PA399&dq=%22Observations+on+the+Human+Voice%22+%22Proceedings+of+the+Royal+Society%22&q (accessed April 2012)
3 Harrison D. Benjamin Guy Babington and his mirror. J Laryngol Otol. 1998;112:235–242.
4 Mackenzie M. Use of the laryngoscope in diseases of the throat, ed 2. Philadelphia: Lindsay & Blakiston; 1869.
5 Burkle CM, Zepeda FA, Bacon DR, Rose SH. A historical perspective on use of the laryngoscope as a tool in anesthesiology. Anesthesiology. 2004;100:1003–1006.
6 Cooper RM. Laryngoscopy—Its past and future. Can J Anaesth. 2004;51:R1–R5.
7 Zeitels SM. Universal modular glottiscope system: The evolution of a century of design and technique for direct laryngoscopy. Ann Otol Rhinol Laryngol Suppl. 1999;179:2–24.
8 Koltai PJ, Nixon RE. The story of the laryngoscope. Ear Nose Throat J. 1989;68:494–502.
9 Green H. Morbid growths within the larynx. In: Green H, ed. On the surgical treatment of polypi of the larynx and oedema of the glottis. New York: GP Putnam, 1852.
10 Kirstein A. Autoskopie des Larynx und der Trachea (Laryngoscopia directa, Euthyskopie, Besichtigung ohne Spiegel). Arch Laryngol Rhinol. 1895;3:156–164.
11 Kirstein A, Thorner M. Autoscopy of the larynx and the trachea (direct examination without mirror). Philadelphia: FA Davis; 1896.
12 Zeitels SM. Chevalier Jackson’s contributions to direct laryngoscopy. J Voice. 1998;12:1–6.
13 Jackson C. The technique of insertion of intratracheal insufflation tubes. Surg Gynecol Obstet. 1913;17:507–509.
14 Janeway HH. Intra-tracheal anesthesia from the standpoint of the nose, throat and oral surgeon with a description of a new instrument for catheterizing the trachea. Laryngoscope. 1913;23:1082–1090.
15 Flagg P. Exposure and illumination of the pharynx and larynx by the general practitioner. A new laryngoscope designed to simplify the technique. Arch Otolaryngol. 1928;8:716–717.
16 Magill IW. Technique in endotracheal anaesthesia. Br Med J. 1930;2:817–819.
17 Miller RA. A new laryngoscope. Anesthesiology. 1941;2:317–320.
18 Macintosh RR. A new laryngoscope. Lancet. 1943;1:205.
19 Crosby E, Cleland M. An assessment of the luminance and light field characteristics of used direct laryngoscopes. Can J Anaesth. 1999;46:792–796.
20 Skilton RW, Parry D, Arthurs GJ, et al. A study of the brightness of laryngoscope light. Anaesthesia. 1996;51:667–672.
21 Levitan RM, Ochroch AE, Higgins MS. Contrary to popular belief and traditional instruction, the larynx is sighted one eye at a time during direct laryngoscopy [letter]. Acad Emerg Med. 1998;5:844–846.
22 International Organisation for Standardisation. Anaesthetic and respiratory equipment—Laryngoscopes for tracheal intubation, ed 2. ISO 7376:2009 (E). Available at http://www.iso.org/iso/search. htm?qt=7376&searchSubmit=Search&sort=rel&type=simple&published=true (accessed April 2012)
23 Baker PA, McQuoid S, Thompson J, Jacobs RJ. An audit of laryngoscopes and application of a new ISO standard. Paediatr Anaesth. 2011;21:428–434.
24 Levitan RM, Kelly JJ, Kinkle WC, Fasano C. Light intensity of curved laryngoscope blades in Philadelphia emergency departments. Ann Emerg Med. 2007;50:253–257.
25 Bucx MJ, De Gast HM, Veldhuis J, et al. The effect of mechanical cleaning and thermal disinfection on light intensity provided by fibrelight Macintosh laryngoscopes. Anaesthesia. 2003;58:461–465.
26 Macintosh RR. Laryngoscope blades [letter]. Lancet. 1944;1:485.
27 Horton WA, Fahy L, Charters P. Disposition of cervical vertebrae, atlanto-axial joint, hyoid and mandible during x-ray laryngoscopy. Br J Anaesth. 1989;63:435–438.
28 Marks RD, Hancock R, Charters P. An analysis of laryngoscope blade shape and design: New criteria for laryngoscope evaluation. Can J Anaesth. 1993;40:262–270.
29 Levitan RM. A new tool for teaching and supervising direct laryngoscopy. Acad Emerg Med. 1996;3:79–81.
30 Ochroch AE, Kush S, Stuart S, et al. Assessment of laryngeal view in direct laryngoscopy: The percentage of glottic opening (POGO) score compared to Cormack and Lehane grading. Can J Anaesth. 1999;46:987–990.
31 McIntyre JWR. Laryngoscope design and the difficult adult tracheal intubation. Can J Anaesth. 1989;36:94–98.
32 Scott J, Baker PA. How did the Macintosh laryngoscope become so popular? Paediatr Anaesth. 2009;19(Suppl 1):24–29.
33 Jephcott A. The Macintosh laryngoscope—A historical note on its clinical and commercial development. Anaesthesia. 1984;39:474–479.
34 Younis RT, Lazar RH. History and current practice of tonsillectomy. Laryngoscope. 2002;112:3–5.
35 Asai T, Matsumoto S, Fujise K, et al. Comparison of two Macintosh laryngoscope blades in 300 patients. Br J Anaesth. 2003;90:457–460.
36 Yardeni IZ, Gefen A, Smolyarenko V, et al. Design evaluation of commonly used rigid and levering laryngoscope blades. Acta Anaesthesiol Scand. 2002;46:1003–1009.
37 Levitan RM. The Airway Cam guide to intubation and practical emergency airway management. Wayne, PA: Airway Cam Technologies; 2004.
38 Jackson C. Bronchoscopy and esophagoscopy: A manual of peroral endoscopy and laryngeal surgery. Philadelphia: WB Saunders; 1922.
39 Racz GB. Improved vision modification of the Macintosh laryngoscope [letter]. Anaesthesia. 1984;39:1249–1250.
40 Bowen RA, Jackson I. A new laryngoscope. Anaesthesia. 1952;7:254–256.
41 McComish PB. Left sided laryngoscopes [letter]. Anaesthesia. 1960;15:326.
42 Pope ES. Left handed laryngoscope. Anaesthesia. 1960;15:326–328.
43 Gabuya R, Orkin LR. Design and utility of a new curved laryngoscope blade. Anesth Analg. 1959;38:364–369.
44 Maleck WH, Koetter KP, Lentz M, et al. A randomized comparison of three laryngoscopes with the Macintosh. Resuscitation. 1999;42:241–245.
45 Cassels WH. Advantages of a curved laryngoscope. Anesthesiology. 1942;3:580–581.
46 Dorsch JA, Dorsch SE. Understanding anesthesia equipment, ed 4. Baltimore: Williams & Wilkins; 1999.
47 Soper RL. A new laryngoscope for anaesthetists. Br Med J. 1947;1:265.
48 Gould RB. Modified laryngoscope blade. Anaesthesia. 1954;9:125.
49 Snow J. Modification of laryngoscope blade. Anesthesiology. 1962;23:394.
50 Phillips OC, Duerksen RL. Endotracheal intubation: A new blade for direct laryngoscopy. Anesth Analg. 1973;52:691–697.
51 Schapira M. A modified straight laryngoscope blade designed to facilitate endotracheal intubation. Anesth Analg. 1973;52:553–554.
52 Henderson JJ. The use of paraglossal straight blade laryngoscopy in difficult tracheal intubation. Anaesthesia. 1997;52:552–560.
53 Henderson JJ. Laryngeal view and ease of endotracheal intubation achieved with a new straight laryngoscope (Henderson laryngoscope). Anesthesiology. 1999;91:A563.
54 Gerlach K, Wenzel V, von Knobelsdorff G, et al. A new universal laryngoscope blade: A preliminary comparison with Macintosh laryngoscope blades. Resuscitation. 2003;57:63–67.
55 Heartwell Medical. Grandview laryngoscope blade. Available at http://www.hartwellmedical.com/grandview.php (accessed April 2012)
56 Bellhouse CP. An angulated laryngoscope for routine and difficult tracheal intubation. Anesthesiology. 1988;69:126–129.
57 Mayall RM. The Belscope for management of the difficult airway [letter]. Anesthesiology. 1992;76:1059–1060.
58 Sultana A, Simmons M, Gatt S. The Belscope—A new angulated laryngoscope: Randomised, prospective, controlled comparison with the Macintosh laryngoscope. Anaesth Intensive Care. 1994;22:98.
59 Choi JJ. A new double-angle blade for direct laryngoscopy [letter]. Anesthesiology. 1990;72:576.
60 Orr RB. A new laryngoscope blade designed to facilitate difficult endotracheal intubation. Anesthesiology. 1969;31:377–378.
61 McCoy EP, Mirakhur RK. The levering laryngoscope. Anaesthesia. 1993;48:516–519.
62 McCoy EP, Mirakhur RK, McCloskey BV. A comparison of the stress response to laryngoscopy. Anaesthesia. 1995;50:943–946.
63 Chadwick IS, McCluskey A. Another trachea intubated with the McCoy laryngoscope [letter]. Anaesthesia. 1995;50:571.
64 Chisholm DG, Calder I. Experience with the McCoy laryngoscope in difficult laryngoscopy. Anaesthesia. 1997;52:896–913.
65 Johnston HM, Rao U. The McCoy levering laryngoscope blade [letter]. Anaesthesia. 1994;49:358.
66 Ward M. The McCoy levering laryngoscope blade [letter]. Anaesthesia. 1994;49:357–358.
67 Harioka T, Nomura K, Mukaida K, et al. The McCoy laryngoscope, external laryngeal pressure, and their combined use. Anaesth Intensive Care. 2000;28:537–539.
68 Randell T, Maattanen M, Kytta J. The best view at laryngoscopy using the McCoy laryngoscope with and without cricoid pressure. Anaesthesia. 1998;53:536–539.
69 Tuckey JP, Cook TM, Render CA. An evaluation of the levering laryngoscope. Anaesthesia. 1996;51:71–73.
70 Levitan RM, Ochroch EA. Explaining the variable effect on laryngeal view obtained with the McCoy laryngoscope [letter]. Anaesthesia. 1999;54:599–601.
71 Laurent SC, de Melo AE, Alexander-Williams JM. The use of the McCoy laryngoscope in patients with simulated cervical spine injuries. Anaesthesia. 1996;51:74–75.
72 Gabbott DA. Laryngoscopy using the McCoy laryngoscope after application of a cervical collar. Anaesthesia. 1996;51:812–814.
73 Uchida T, Yoshio H, Saito Y, et al. The McCoy levering laryngoscope in patients with limited neck extension. Can J Anaesth. 1997;44:674–676.
74 Sugiyama K, Yokoyama K. Head extension angle required for direct larynygoscopy with the McCoy laryngoscope blade [letter]. Anesthesiology. 2001;94:939–940.
75 MacIntyre PA, McLeod ADM, Hurley R, et al. Cervical spine movements during laryngoscopy. Anaesthesia. 1999;54:413–418.
76 Gerling MC, Davis DP, Hamilton RS, et al. Effects of cervical spine immobilization technique and laryngoscope blade selection on an unstable cervical spine in a cadaver model of intubation. Ann Emerg Med. 2000;36:293–300.
77 Yardeni IZ, Abramowitz A, Zelman V. A new laryngoscope with flexible adjustable rigid blade. Br J Anaesth. 1999;83:537–539.
78 Perera CN, Wiener PC, Harmer M, et al. Evaluation of the use of the Flexiblade. Anaesthesia. 2000;55:890–893.
79 Bucx MJ, Snijders CJ, van Geel RT, et al. Forces acting on the maxillary incisor teeth during laryngoscopy using the Macintosh laryngoscope. Anaesthesia. 1994;49:1064–1070.
80 Bucx MJ, van Geel RT, Wegener JT, et al. Does experience influence the forces exerted on maxillary incisors during laryngoscopy? A manikin study using the Macintosh laryngoscope. Can J Anaesth. 1995;42:144–149.
81 Bizzarri DV, Giuffrida JG. Improved laryngoscope blade designed for ease of manipulation and reduction of trauma. Anesth Analg. 1958;37:231–232.
82 Callander CC, Thomas J. Modification of Macintosh laryngoscope for difficult intubation [letter]. Anaesthesia. 1987;42:671–672.
83 Bucx MJL, Snijders CJ, van der Vegt MH, et al. An evaluation of a modified Macintosh laryngoscope in a manikin. Can J Anaesth. 1998;45:483–487.
84 Bucx MJ, Snijders CJ, van der Vegt MH, et al. Reshaping the Macintosh blade using biomechanical modelling. Anaesthesia. 1997;52:662–667.
85 Onkst HR. Modified laryngoscope blade. Anesthesiology. 1961;22:846–848.
86 Racz GB, Allen FB. A new pressure-sensitive laryngoscope [letter]. Anesthesiology. 1985;62:356–358.
87 Lagade MRG, Poppers PJ. Revival of the Polio laryngoscope blade [letter]. Anesthesiology. 1982;57:545.
88 Kessell J. A laryngoscope for obstetrical use—An obstetrical laryngoscope. Anaesth Intensive Care. 1977;5:265–266.
89 Beaver RA. Special laryngoscopes. Anaesthesia. 1955;10:83–84.
90 Patil VU, Stehling LC, Zauder HL. An adjustable laryngoscope handle for difficult intubations [letter]. Anesthesiology. 1984;60:609.
91 Jellicoe JA, Harris NR. A modification of a standard laryngoscope for difficult tracheal intubation in obstetric cases. Anaesthesia. 1984;39:800–802.
92 Dhara SS, Cheong TW. An adjustable multiple angle laryngoscope adaptor. Anaesth Intensive Care. 1991;19:243–245.
93 Yentis SM. A laryngoscope adaptor for difficult intubation. Anaesthesia. 1987;42:764–766.
94 Bainton CR. A new laryngoscope blade to overcome pharyngeal obstruction. Anesthesiology. 1987;67:767–770.
95 Diaz JH, Guarisco JL, LeJeune FE. A modified tubular pharyngolaryngoscope for difficult pediatric laryngoscopy [letter]. Anesthesiology. 1990;73:357–358.
96 Bryce-Smith R. A laryngoscope blade for infants [letter]. Br Med J. 1952;1:217.
97 Seward EH. Laryngoscope for resuscitation of the newborn. Lancet. 1957;2:1041.
98 Robertshaw FL. A new laryngoscope for infants and children. Lancet. 1962;2:1034.
99 Matsuki A. New pediatric laryngoscope [letter]. Anesthesiology. 1982;57:556.
100 Rokowski WJ, Gurmarnik S. Laryngoscope blades modified for neonates and infants [letter]. Anesth Analg. 1983;62:241–242.
101 Diaz JH. Further modifications of the Miller blade for difficult pediatric laryngoscope [letter]. Anesthesiology. 1984;60:612–613.
102 Cork RC, Woods W, Vaughan RW, et al. Oxygen supplementation during endotracheal intubation of infants [letter]. Anesthesiology. 1979;51:186.
103 Wung J, Stark R, Indyk L. Oxygen supplement during endotracheal intubation of the infant. Pediatrics. 1977;59:1046–1048.
104 Hencz P. Modified laryngoscope for endotracheal intubation of neonates [letter]. Anesthesiology. 1980;53:84.
105 Todres ID, Crone RK. Experience with a modified laryngoscope in sick infants. Crit Care Med. 1981;9:544–545.
106 Ledbetter JL, Rasch DK, Pollard TG, et al. Reducing the risks of laryngoscopy in anaesthetised infants. Anaesthesia. 1988;43:151–153.
107 Gabrielczyk MR. A new integrated suction laryngoscope [letter]. Anaesthesia. 1986;41:970–971.
108 Khan AK. A controllable suctioning laryngoscope [letter]. Anesth Analg. 1990;71:200.
109 Fishelev W, Vatashsky E, Aronson HB. Suction catheter attached to laryngoscope [letter]. Anaesthesia. 1984;39:188–189.
110 Intubrite: Information about the Intubrite HyperVisualization System. Available at http://www.intubrite.com (accessed April 2012)
111 Truphatek: Information about the TruLite laryngoscope. Available at http://www.truphatek.com/p-27 (accessed April 2012.)
112 Siker ES. A mirror laryngoscope. Anesthesiology. 1956;17:38–42.
113 McMorrow RC, Mirakhur RK. A new mirrored laryngoscope. Anaesthesia. 2003;58:998–1002.
114 Huffman JP. The application of prisms to curved laryngoscopes: A preliminary study. J Am Assoc Nurse Anesth. 1968;36:138–139.
115 Huffman JP, Elam JO. Prisms and fiber optics for laryngoscopy. Anesth Analg. 1971;50:64–67.
116 Brillhart A, Dasti A, Matz W, Schrading WA. The Rusch ViewMax vs Macintosh laryngoscopy in human cadavers: improved vocal cord visualization? Am J Emerg Med. 2009;27:864–867.
117 Leung YY, Hung CT, Tan ST. Evaluation of the new Viewmax laryngoscope in a simulated difficult airway. Acta Anaesthesiol Scand. 2006;50:562–567.
118 Zamora JE, Nolan RL, Sharan S, Day AG. Evaluation of the Bullard, GlideScope, Viewmax, and Macintosh laryngoscopes using a cadaver model to simulate the difficult airway. J Clin Anesth. 2011;23:27–34.
119 Singh I, Khaund A, Gupta A. Evaluation of Truview evo2 laryngoscope in anticipated difficult intubation—A comparison to Macintosh laryngoscope. Indian J Anaesth. 2009;53:164–168.
120 Gotou M, Inoue T. Application of the Truview EV02 optical laryngoscope to patients with cervical spinal disease. J Anesth. 2007;21:295–296.
121 Inal MT, Memis D, Kargi M, et al. Comparison of TruView EVO2 with Miller laryngoscope in paediatric patients. Eur J Anaesthesiol. 2010;27:950–954.
122 Singh R, Singh P, Vajifdar H. A comparison of Truview infant EVO2 laryngoscope with the Miller blade in neonates and infants. Paediatr Anaesth. 2009;19:338–342.
123 Li JB, Xiong YC, Wang XL, et al. An evaluation of the TruView EVO2 laryngoscope. Anaesthesia. 2007;62:940–943.
124 Matsumoto S, Asai T, Shingu K. Truview video laryngoscope in patients with difficult airways. Anesth Analg. 2006;103:492–493.
125 Barak M, Philipchuck P, Abecassis P, Katz Y. A comparison of the Truview blade with the Macintosh blade in adult patients. Anaesthesia. 2007;62:827–831.