CHAPTER 63 Triceps Insufficiency Following Total Elbow Arthroplasty
INTRODUCTION
Triceps insufficiency can occur as a result of traumatic rupture of the tendon or, most commonly, following a failed surgical reattachment, particularly when there is poor tendon quality.5,12,15,17,18 As a complication following elbow replacement, this is becoming much more appreciated.4
According to the limited literature available on this topic, the incidence of triceps insufficiency following total elbow arthroplasty ranges from 1% to 29%.7,9,10,14,16,17 A recent report using the Gschwend approach documents four of 28 elbows with triceps insufficiency after a triceps-splitting approach to insert the GSB implant (Center Pulse, Zurich).11 In a recent comprehensive review of the literature, Voloshin et al22 documented an incidence of approximately 1% to 5% of triceps insufficiency associated with total elbow arthroplasty. Typically, literature reviews understate the true incidence of this problem.
The key factor in avoiding the development of this problem is the nature and execution of the surgical exposure. In this regard, a number of recent studies23 have examined modifications to existing exposures (see Chapter 7).6,19 Olecranon osteotomy is contraindicated in joint replacement surgery. Hence, some means of dealing with the triceps attachment is necessary. There are several options:
PRESENTATION AND SYMPTOMS
All patients will report loss of active extension and about 15% to 20% will also report pain.4 The most common problem is the inability to reach above the head and to push through doors. The mean time from initial procedure to revision for triceps insufficiency is about 3 years. In our experience the clinical findings at the time of surgical revision were (1) a change in the posterior contour of the elbow with visual and palpable prominence of the implant and atrophy of the subcutaneous tissue; (2) the presence of an olecranon bursitis; (3) atrophy of the triceps muscle; and (4) discernable lateral subluxation or dislocation of the extensor mechanism.
MANAGEMENT
Our recommendations are based on the Mayo Clinic experience with triceps insufficiency for any cause21 and particularly after joint replacement.4 From 887 total elbow arthroplasty operations, we identified 16 elbows that underwent subsequent surgical treatment for triceps insufficiency at our institution. The underyling diagnoses for which the primary total elbow arthroplasty was performed were rheumatoid arthritis in nine cases and post-traumatic conditions in seven cases. Initially, the triceps-sparing approach as described by Bryan and Morrey2 was used in 15; in one patient, the triceps-splitting approach as described by Campbell3 was used.
REPAIR OR RECONSTRUCTION
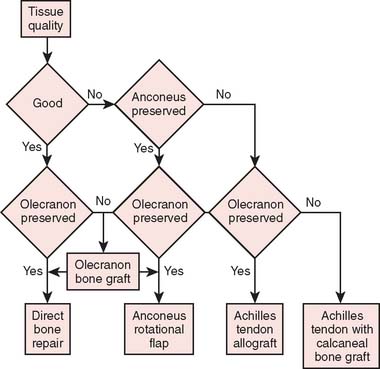
The logic we currently employ to determine how these problems should be managed is similar to the algorithm developed for management of triceps insufficiency for any cause13,21 (Fig. 63-1). If the tissue quality is good and the olecranon is preserved, we repeat the direct attachment to bone if the tissue is of adequate quality for this. If the tissue is not of good quality but the anconeus and the olecranon are preserved, then we perform an anconeus rotational flap. Finally, if the tissue is not of good quality and the anconeus is not perserved, then an Achilles tendon allograft is carried out. The calcaneus is used to supplement the olecranon if it is resorbed; otherwise, the tendinous tissue is sewn to the intact olecranon and the calcaneus is removed from the allograft.
REATTACHMENT
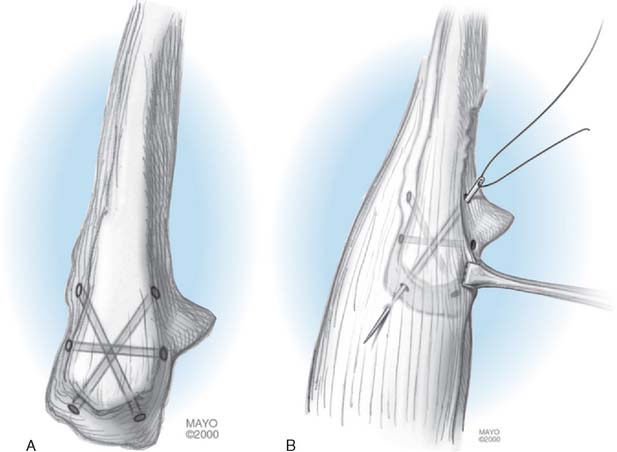
This is not commonly indicated if the tendon was properly reattached initially. The key is to avoid the intervention of synovium between the attachment of the triceps tissue and the olecranon. The way to ensure this is to add a circumferential “cinch” suture to apply or compress the triceps tendon closely to its attachment site (Fig. 63-2).
ANCONEUS ROTATIONAL FLAP
Technique
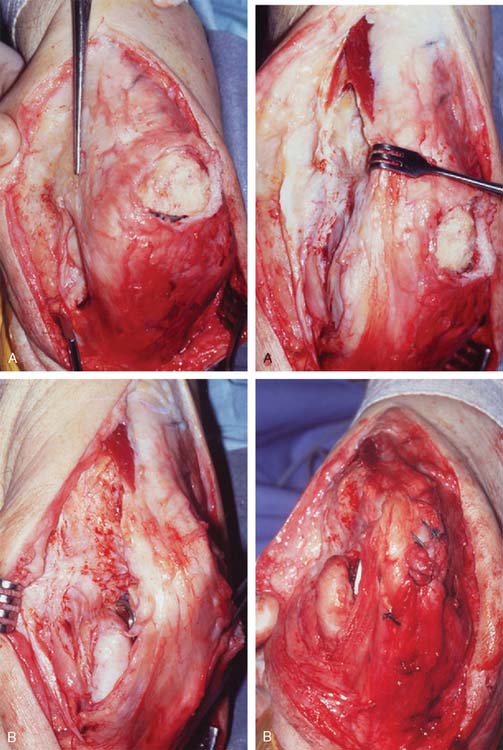
With the patient supine and the arm brought across the chest, the previous skin incision is entered. The triceps mechanism is carefully explored, and the ulnar nerve is protected. The Kocher interval between the anconeus and extensor carpi ulnaris is identified. The anconeus is elevated from the olecranon insertion, leaving intact the distal 20% (Fig. 63-3A). The humeral attachment is detached, allowing the entire extensor mechanism to be rotated from lateral to medial. The fascial attachment of the anconeus is oriented over the posterior aspect of the olecranon and secured with a criss-cross and transverse suture, as described previously (see Fig. 63-3B). The original triceps attachment is now medially displaced. It is incorporated back into the extensor mechanism in order to enhance extension strength.
ACHILLES TENDON RECONSTRUCTION
Technique
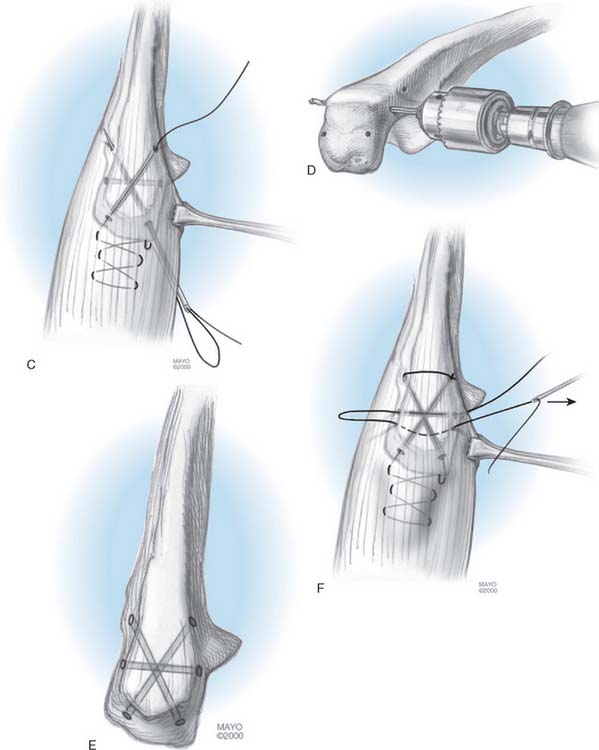
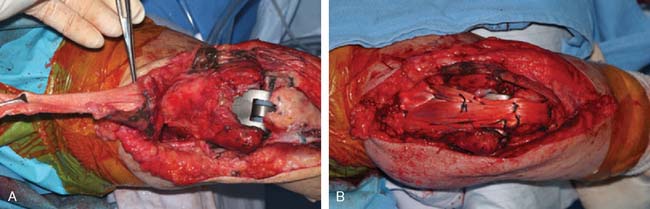
The patient is supine on the table, and the arm is brought across the chest. The olecranon and triceps are widely exposed. The ulnar nerve is identified and protected or translocated, if appropriate. If the olecranon is intact, the triceps muscle is mobilized and the radial nerve is identified and protected as necessary. The fascial expansion of the allograft tendon is brought around the triceps, and the aponeurosis of the allograft securely fastened to the triceps muscle (Fig. 63-4A). The tendinous portion of the achilles allograft is then attached to the olecranon by creating a groove in the posterior aspect of the olecranon with a high-speed burr (Fig. 63-4A, arrow). The graft is placed in the groove and folds over the tip of the olecranon. It is secured with a No. 5 nonabsorbable suture through drill holes in the proximal ulna.
The arm is placed in 45 degrees of extension, and a No. 5 nonabsorbable suture is used to securely attach the distal aspect of the triceps and its tendinous attachment to the allograft. A No. 1 Ethibond running locked suture is then employed circumferentially to attach the fascia of the allograft to the muscle and fascia of the triceps mechanism (see Fig. 63-4B).
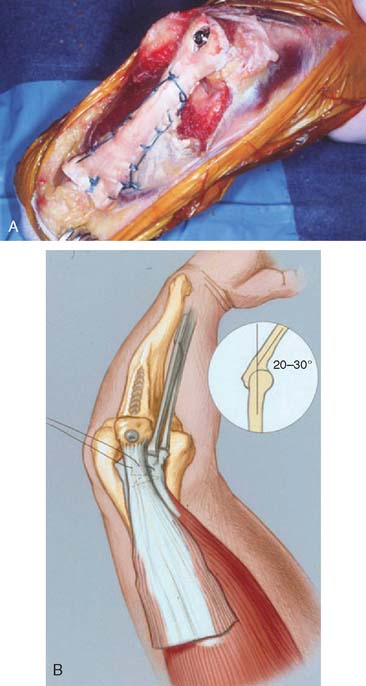
Note: If the olecranon is deficient, the calcaneus is left on the Achilles tendon and is fashioned in such a way as to be applied to the proximal ulna (Fig. 63-5). The allograft is secured with two Kirschner wires and a circumferential wire according to the AO method. Once the allograft has been secured, once again the elbow is brought into 40 to 45 degrees of extension and the fascial expansion of the tendon is secured to the triceps mechanism as described above.
OUTCOME
By employing the above-mentioned logic, we were successful in obtaining extension against gravity in 15 of 16 elbows. There were no significant complications. The major determinant of the success of the operation is the adequacy of the olecranon process. If the olecranon process is absent, it may be reconstructed with the calcaneus along with the Achilles graft. If the olecranon is resorbed and is deficient, simply attaching or reconstructing the triceps is inadequate to restore function.
PROGNOSTIC FACTORS
The most important prognostic factor is the presence or absence of an olecranon process. This detrimental prognostic feature can be obviated by the use of a bone graft. Otherwise the overall quality of the tissues and the number of previous surgical procedures20 are the most important factors that influence outcome.
1 Boorman R.S., Page W.T., Weldon E.J., Lippitt S., Matsen F.A.III. A triceps-on approach to semiconstrained total elbow arthroplasty. Tech. Shoulder Elbow Surg. 2003;4:139.
2 Bryan R.S., Morrey B.F. Extensive posterior exposure of the elbow. A triceps-sparing approach. Clin. Orthop. Rel. Res. 1982;166:188.
3 Campbell W.C.. Crenshaw A.H., editor. Campbell’s Operative Orthopaedics. Surgical Approaches, ed. 5, Vol. 1. St. Louis: C. V. Mosby Co., 1971;119.
4 Celli A., Arash A., Adams R.A., Morrey B.F. Triceps insufficiency following total elbow arthroplasty. J. Bone Joint Surg. 2005;87A:1957.
5 Clayton M.L., Thirupathi R.G. Rupture of the triceps tendon with olecranon bursitis. Clin. Orthop. Rel. Res. 1984;184:183.
6 Ebraheim N.A., Andreshak T.G., Yeasting R.A., Saunders R.C., Jackson W.T. Posterior extensile approach to the elbow joint and distal humerus. Orthop. Rev. 1993;22:578-582.
7 Gill D.R.J., Morrey B.F. The Coonrad-Morrey total elbow arthroplasty in patients who have rheumatoid arthritis. J. Bone Joint Surg. 1998;80A:1327.
8 Gschwend N., Simmen B.R., Matejovsky Z. Late complications in elbow arthroplasty. J. Shoulder Elbow Surg. 1996;5(2 Pt 1):86.
9 Hildebrand K.A., Patterson S.D., Regan W.D., MacDermid J.C., King G.J. Functional outcome of semiconstrained total elbow arthroplasty. J. Bone Joint Surg. 2000;82A:1379.
10 Inglis A.E., Pellicci P.M. Total elbow replacement. J. Bone Joint Surg. 1980;62A:1252.
11 Kelly E.W., Coghlan J., Bell S. Five to thirteen year follow-up of the GSB III total elbow arthroplasty. J. Shoulder Elbow Surg. 2004;13:434.
12 Morrey B.F. Complications of Elbow Replacement Surgery. The Elbow and its Disorders, 3rd ed., Philadelphia: WB Saunders; 2000:667.
13 Morrey B.F. Rupture of the triceps tendon. In: Morrey B.F., editor. The Elbow and Its Disorders. 3rd ed. Philadelphia: WB Saunders; 2000:479.
14 Morrey B.F., Adams R.S. Semiconstrained arthroplasty for the treatment of rheumatoid arthritis of the elbow. J. Bone Joint Surg. 1992;74A:479.
15 Morrey B.F., Bryan R.S. Complication of total elbow arthroplasty. Clin. Orthop. Relat. Res. 1982;170:204.
16 Morrey B.F., Bryan R.S., Dobyns J.H., Linscheid R.L. Total elbow arthroplasty—A five-year experience at the Mayo Clinic. J. Bone Joint Surg. 1981;63A:1050.
17 Pierce T.D., Herndon F.H. The triceps preserving approach to total elbow arthroplasty. Clin. Orthop. Relat. Res. 1998;354:144.
18 Sanchez-Sotero J., Morrey B.F. Surgical techniques for reconstruction of chronic insufficiency of the triceps. J. Bone Joint Surg. 2002;84B:1116.
19 Schildhauer T.A., Nork S.E., Mills W.J., Henley M.B. Extensor mechanism-sparing paratricipital posterior approach to the distal humerus. J. Orthop. Trauma. 2003;17:374.
20 Schneeberger A.G., Adams R., Morrey B.F. Semiconstrained total elbow replacement for the treatment of post-traumatic osteoarthrosis. J. Bone Joint Surg. Am. 1997;79:1211.
21 van Riet R.P., Morrey B.F., Ho E., O’Driscoll S.W. Surgical treatment of distal triceps ruptures. J. Bone Joint Surg. 2003;85A:1961.
22 Voloshin, I., Kakar, S., Kaye, E. K., and Morrey, B. F.: Complications of total elbow replacement: Systematic review of literature in the last decade. J. Am. Assoc. Orthop. Surg. 2007 (in press).
23 Wilkinson J.M., Stanley D. Posterior surgical approaches to the elbow: A comparative anatomic study. J. Shoulder Elbow Surg. 2001;10:380.
24 Wolfe S.W., Figgie M.P., Inglis A.E., Bohn W.W., Ranawat C.S. Management of infection about total elbow prostheses. J. Bone Joint Surg. 1990;72A:198.