CHAPTER 46 Surgical Failure of Tennis Elbow
INTRODUCTION
Lateral epicondylitis is the most common elbow affliction in adults. Surgical intervention appears to be increasing, in part due to the introduction of orthopedic releases. Failures after surgery are recognized, but the cause and the means of re-evaluation are seldom addressed. Initially, the most frequent explanation for residual symptoms is too brief a period after surgery or inadequate rehabilitation. The latter may be due to noncompliance or an inadequate program of strengthening and stretching exercises.22 This type of problem is readily determined with a careful interview. The reliability of surgical procedures for lateral epicondylitis makes the need for reoperation uncommon. For this reason, few surgeons have extensive experience with the management of patients after failed intervention for epicondylitis, and reports of such experience in the literature are lacking. The intent of this chapter is to share our experience with this problem and to provide a basis for determining the cause of failure and a basis for further management. Specific focus is on determining which patients might benefit from a second surgical procedure. To be perfectly candid, a review of the literature on this subject over the last 10 years has, I feel, obscured rather than clarified this particular problem.
ETIOLOGY AND PATHOLOGY
Because the treatment of surgical failure in large measure relates to the etiology and pathology of the condition, analysis of treatment failure logically begins with a brief consideration of the pathoanatomy of lateral epicondylitis. This is discussed in detail in Chapter 44. It is well accepted that the pathology involves the extensor carpi radialis brevis tendon.4,6,8,13,15,22,25
Although generally considered an inflammatory lesion, as many as 14 pathologic features are reported in the literature (Box 46-1).26 A careful blinded study of pathologic and control material reported that the material removed at surgery reveals hyaline degeneration with neovasculature. This represents an aborted effort of healing but is not inflammation. Inappropriate or inaccurate initial diagnoses may occur,32 such as interosseous nerve entrapment,1,6,19,31,33 or even intra-articular plica.29
Regardless of the etiology or underlying pathology, nonoperative management is usually successful in 90% of patients.22 Similarly, when surgery is performed, a 90% success rate is typically reported. The interesting feature of these data is that the success of surgery seems independent of the surgical technique.2,3,6,14,21,22,26,28,34 On the other hand, when surgical intervention is not successful, there are few reports of subsequent management.9,12,18,19,23
PATIENT EVALUATION
CLASSIFICATION
Type I—Inaccurate Initial Diagnosis
Several other possible causes of lateral elbow pain include degenerative arthrosis,20 anconeus or extensor muscle compartment syndrome,1,25 lateral ligament instability especially with a history of trauma,23 and entrapment of the posterior interosseous nerve (PIN) in the region of the arcade of Frohse17,30,33 (Fig. 46-1), cutaneous nerve entrapment,10 and intra-articular plica.29
The distinction between lateral epicondylitis and PIN entrapment has been well discussed in the literature.5,11,20,27,28,33 The distinction is made even more difficult because PIN entrapment may coexist with lateral epicondylitis in about 5% percent of individuals.33 In one series, a concurrent and unrecognized PIN entrapment also was suspected as the cause of failure in 2 of 15 patients.33 I have found a reliable triad to help make this diagnosis, consisting of: localization of pain at the arcade of Frohse reproduced by direct palpation; pain aggravated by resisted supination; and pain relief by injection of 2 mL of lidocaine (Xylocaine). Electromyographic changes, on the other hand, are not usually present, nor are they necessary to diagnose nerve entrapment.
Improper Patient Selection
It should also be noted that patient selection is a consideration with a type I failure. Issues include adequate motivation, compliance, and consideration of secondary gain.31 The same factors that resulted in a failure of nonoperative treatment are present in the patient undergoing surgery. The best solution for this difficult problem is obvious: avoid the initial surgical procedure in patients known to be at risk for secondary gain. Avoid additional surgery at all costs.
Type II—Inadequate or Incomplete Procedure
In some patients, an incomplete release or excision of the pathologic tissue is the cause of persistent symptoms. This was the most common finding in our19 and Nirschl’s experience. In fact, of 35 secondary procedures by Nirschl, the extensor carpi radialis brevis (ECRB) was felt not to have been addressed at all in 27, and inadequately excised in 7.23 By excising this area, 83% experienced a good or excellent result.
Type III—Introduction of New Pathology
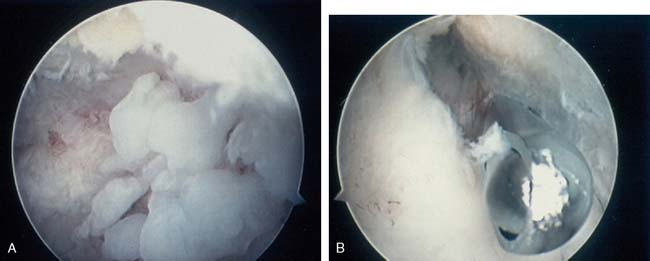
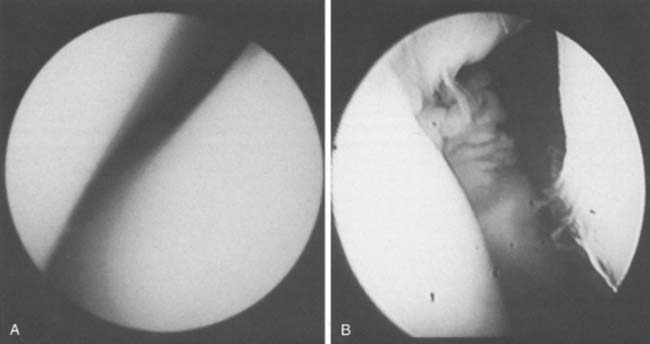
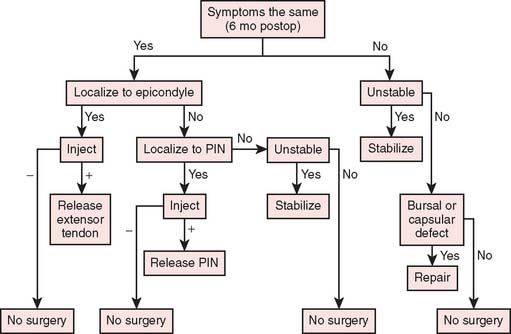
The cause of type III failure is surgically introduced pathology. Synovial fistula or herniation, adventitial bursa, and ligament insufficiency are the most likely causes. Synovial fistulas have been identified as occurring as a complication after 4 of 149 percutaneous procedures33 (Fig. 46-2). Instability may be subtle and we often employ a fluoro-scan to assist in making the diagnosis (Fig. 46-3). An algorithm may also be useful here (Fig. 46-4).
PHYSICAL EXAMINATION
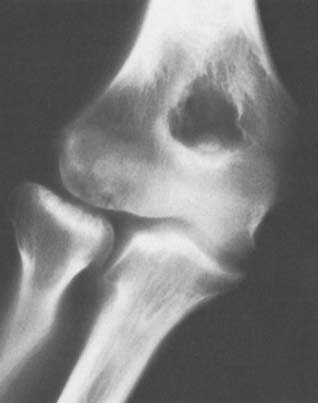
The examination focuses on the three categories of failure. All patients should be evaluated by measurement of flexion-extension and pronation-supination motion. Pain from resisted supination suggests PIN symptoms, and pain elicited by resisted wrist extension suggests persistent lateral epicondylitis. In type I failure, palpation is directed specifically at both the lateral epicondyle and the arcade of Frohse. If the original cause was a traumatic event for a type I failure, and in all patients in whom symptoms had changed (type III/failure), examination for varus instability24 or posterolateral rotatory instability (PLRI) is performed. Patients with night pain or motion loss are further evaluated for arthrosis, sepsis, or osteochondritis dissecans of the capitellum. In this latter group, arthroscopy is a useful means of further assessment.
Types I and II
If the injection at the epicondyle is unsuccessful and if the physical examination suggests PIN entrapment, a second injection with lidocaine is performed in the region of the PIN as it enters the supinator muscle at the arcade of Frohse. If most symptoms (70% to 80%) are relieved, PIN entrapment is diagnosed. Some surgeons believe that the nerve may also be compressed as it exits the supinator, so this also must be considered.
The joint is evaluated by intra-articular injection of 4 to 5 mL of lidocaine in patients whose symptoms are suggestive of intra-articular pathology, but the routine radiographs are inconclusive. A technetium-99m bone scan may be used to localize an articular process (Fig. 46-5). Increasingly, arthroscopy is helpful in diagnosing synovial or articular pathology. As Baker has correctly observed, a certain percentage of patients will exhibit capsular involvement diagnosed at arthroscopy (personal communication-Champ Baker, Columbus GA) (Fig. 46-6). Symptoms consistent with an unstable elbow are evaluated by stress radiography under fluoroscopy. This diagnosis also may be confirmed by arthroscopy.
Type III
Patients in whom the symptom complex was different after the initial surgical procedure uncommonly represent an incorrect initial diagnosis. The diagnosis is more commonly related to the surgical procedure itself. In type III failure, diagnostic possibilities include adventitial bursa, capsular fistula, and instability. Diagnostic studies are directed by the physical examination and again may include injection in the area of maximal local tenderness. Radiographs may reveal ectopic bone causing residual but different symptoms (Fig. 46-7).7 In the past, an arthrogram was helpful in demonstrating capsular herniation or ligamentous insufficiency (see Fig. 46-2). If motion causes pain or if catching is present, instability is assessed by fluoroscopic stress radiography (see Fig. 46-3). In a patient in whom intra-articular pathology is suspected, intra-articular injection with lidocaine, tomography, bone scan, and arthroscopy are performed, in that order, until the diagnosis is made (see Figs. 46-2 and 46-3). Arthroscopy is particularly helpful in demonstrating subtle instability by revealing laxity of the radiohumeral joint (Fig. 46-8).
TREATMENT
The time before subsequent intervention is an important issue. A review of the literature suggests that a successful surgical procedure is evident within the first 3 or 4 months. One year of follow-up assessment is certainly more than adequate to reveal whether surgical intervention has been successful. Posch and colleagues25 demonstrated that only 1 of 43 patients improved more than 1 year after surgery.
All patients with type I failure are treated nonoperatively if the local injection in the region of the lateral epicondyle or in the region of the arcade of Frohse does not relieve the symptoms. Type II, inadequate treatment problems can be reoperated after 6 to 9 months. In the group of patients in whom the symptoms have changed (type III), however, particularly if an instability pattern is diagnosed, surgery may be offered as soon as this diagnosis is made.
SURGICAL TREATMENT
If the examination dictates, exploration of the PIN is carried out through the same incision. If a traumatic event preceded the symptoms and if instability has been diagnosed, the lateral collateral ligament is stabilized (see Chapter 47).
In type II problems in patients who met the criteria for surgical intervention, the entire extensor mass and specifically the ECRB are carefully explored.19,23
RESULTS
Type I Failure
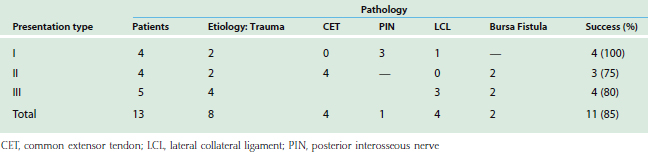
Four patients were reviewed who met the criteria for additional surgical intervention with type I failure due to inaccurate diagnoses. Data referable to the presentation and results are shown in Table 46-1. All were successfully managed.
Type II Failure
Of the four with inadequate initial resection, subsequent localized débridement was successful in three (75%). This is similar to the outcome reported by Nirschl.23
Type III Results
Those patients with type III pathology represented a different patient population (see Table 46-1). One had successful removal of an adventitial bursa (Fig. 46-9). Four of the five patients in this group now have satisfactory outcomes. The only patient with an unsatisfactory result was improving 6 months after ligament reconstruction, but because of continued pain at the radiohumeral articulation, the radial head was removed by another orthopedic surgeon. Symptoms worsened.
OTHER REPORTS
As noted earlier, the only other study of reoperation is that of Nirschl, who reported a similar rate of success as we had documented.23 For reasons that are obscure to me, several reports document successful relief of pain by an anconeus muscle rotation transfer to the lateral epicondyle.9,18 Even an adipofascial radial forearm flap coverage of the epicondyle has been reported as a successful revision procedure.12
CONCLUSION
Our treatment logic is shown in Figure 46-10. Type I failure represents either improper patient selection, or an incorrect initial diagnosis. The type II failure is persistence of the original pathologic condition that has not been corrected by surgery. Type III failure, identified by altered symptoms, may represent a condition associated with the surgical procedure. A careful history leading to studies directed at a specific cause generally isolates the basis of persistent symptoms. In patients with type I failure, pain typically does not localize well to the lateral epicondyle. Overlooking PIN entrapment should also be considered. In type II failure, if the assessment suggests residual pain at the epicondyle, further release of the extensor tendon at the lateral epicondyle is generally successful. In a patient with a type III failure, either instability or bursal or capsular pathology must be considered. The pivot shift test and arthroscopy are useful in revealing ligamentous insufficiency. The MRI usually shows abnormality, but its specificity is not reliable. Arthrography is helpful in identifying capsular and bursal conditions as well. Reoperation, if well planned in carefully selected patients, may be anticipated to be successful in as many as 85% of patients.
1 Abrahamsson S.O., Sollerman C., Söderberg T., Lundborg G., Rydholm U., Pettersson H. Lateral elbow pain caused by anconeus compartment syndrome: a case report. Acta Orthop. Scand. 1987;58:589.
2 Bosworth D.M. The role of the orbicular ligament in tennis elbow. J. Bone Joint Surg. 1955;37A:527.
3 Boyd H.B., McLeod A.C. Tennis elbow. J. Bone Joint Surg. 1973;55A:1183.
4 Briggs C.A., Elliott B.G. Lateral epicondylitis: A review of structures associated with tennis elbow. Anat. Clin. 1985;7:149.
5 Capener N. The vulnerability of the posterior interosseous nerve of the forearm: a case report and an anatomical study. J. Bone Joint Surg. 1966;48B:770.
6 Coonrad R.W., Hooper W.R. Tennis elbow: its course, natural history, conservative and surgical management. J. Bone Joint Surg. 1973;55A:1177.
7 Cushing M., Lourie G.M., Miller D.V., Hohn J.A. Heterotopic ossification after lateral epicondylectomy. J. Southern Orthop. Assoc. 2001;10:63.
8 Cyriax J.H. The pathology and treatment of tennis elbow. J. Bone Joint Surg. 1936;18:921.
9 Degreef I., Van Raebroeckx A., De Smet L. Anconeus muscle transposition for failed surgical treatment of tennis elbow: preliminary results. Acta Orthop. Belg. 2005;71:154.
10 Dellon A.L., Kim J., Ducic I. Painful neuroma of the posterior cutaneous nerve of the forearm after surgery for lateral humeral epicondylitis. J. Hand Surg. 2004;29A:387.
11 Dewey P. The posterior interosseous nerve and resistant tennis elbow. J. Bone Joint Surg. 1973;55B:435.
12 Gaede F. Adipofascial radial forearm flap after failed surgical treatment of lateral epicondylitis. Acta Orthop. Belg. 2006;72:761.
13 Garden R.S. Tennis elbow. J. Bone Joint Surg. 1961;43B:100.
14 Gardner R.C. Tennis elbow: Diagnosis, pathology and treatment. Nine severe cases treated by a new reconstructive operation. Clin. Orthop. Relat. Res. 1970;72:248.
15 Goldie I. Epicondylitis lateralis humeri. Acta Chir. Scand. 1964;339(suppl):7.
16 Henry M., Stutz C. A unified approach to radial tunnel syndrome and lateral tendinosis. Tech. Hand Up. Extrem. Surg. 2006;10:200.
17 Jalovaara P., Lindholmj R.V. Decompression of the posterior interosseous nerve for tennis elbow. Arch. Orthop. Trauma Surg. 1989;108:243.
18 Luchetti R., Atzei A., Brunelli F., Fairplay T. Anconeus muscle transposition for chronic lateral epicondylitis, recurrences, and complications. Tech. Hand Up. Extrem. Surg. 2005;9:105.
19 Morrey B.F. Reoperation for failed surgical treatment of refractory lateral epicondylitis. J. Shoulder Elbow Surg. 1992;1:47.
20 Morrison D.L. Tennis elbow and radial tunnel syndrome: differential diagnosis and treatment. J. Aust. Orthop. Assoc. 1981;80:823.
21 Neviaser T.J., Neviaser R.J., Neviaser J.S., Ain B.R. Lateral epicondylitis: results of outpatient surgery and immediate motion. Contemp. Orthop. 1985;11:43.
22 Nirschl R.P., Pettrone F.A. Tennis elbow and the surgical treatment of lateral epicondylitis. J. Bone Joint Surg. 1979;61A:832.
23 Organ S.W., Nirschl R.P., Kraushaar B.S., Guidi E.J. Salvage surgery for lateral tennis elbow. Am. J. Sports Med. 1997;25:746.
24 O’Driscoll S.W., Bell D.F., Morrey B.F. Posterolateral rotatory instability of the elbow. J. Bone Joint Surg. 1991;73A:440.
25 Posch J.N., Goldberg V.M., Larrey R. Extensor fasciotomy for tennis elbow: a long-term follow-up study. Clin. Orthop. 1978;135:179.
26 Regan, W., Wold, L. E., Coonrad, R., and Morrey, B. F.: Microscopic histopathology of lateral epicondylitis. Presented at the Annual Meeting of the Canadian Orthopaedic Association, Toronto, Ontario, June 3, 1989.
27 Roles N.C., Maudsley R.H. Radial tunnel syndrome: resistant tennis elbow as a nerve entrapment. J. Bone Joint Surg. 1972;54B:499.
28 Rossum J.V., Buruma J.S., Kamphuisen H.A.C., Onvlee G.J. Tennis elbow: a radial tunnel syndrome? J. Bone Joint Surg. 1978;60B:197.
29 Ruch D.S., Papadonikolakis A., Campolattaro R.M. The posterolateral plica: a cause of refractory lateral elbow pain. J. Shoulder Elbow Surg. 2006;15:367.
30 Smola C. About the problem of radial tunnel syndrome or “where does the tennis elbow end and where does the radial tunnel syndrome begin”? Handchir. Mikrochir. Plast. Chir. 2004;36:241.
31 Stovall P.B., Beinfield M.S. Treatment of resistant lateral epicondylitis of the elbow by lengthening of the extensor carpi radialis brevis tendon. Surg. Gynecol. Obstet. 1979;149:526.
32 Svernlöv B., Adolfsson L. Outcome of release of the lateral extensor muscle origin for epicondylitis. Scand. J. Plast. Reconstr. Surg. Hand Surg. 2006;40:161.
33 Werner C.O. Lateral elbow pain and posterior interosseous nerve entrapment. Acta Orthop. Scand. 1979;114(suppl):174.
34 Yerger B., Turner T. Percutaneous extensor tenotomy for chronic tennis elbow: an office procedure. Orthopedics. 1985;8:1261.