Chapter 29 Treatment of Psychotic Disorders
| Abbreviations | |
|---|---|
| ACh | Acetylcholine |
| DA | Dopamine |
| 5-HT | Serotonin |
Therapeutic Overview
| Therapeutic Overview |
|---|
| Typical Antipsychotics |
| Alleviate positive symptoms |
| Bind to and block 70% to 80% of D2 receptors at clinically effective doses |
| Atypical Antipsychotics |
| Alleviate positive and may improve negative symptoms |
| May improve cognitive impairments |
| Bind to and block 40% to 60% of D2 receptors at clinically effective doses |
| Bind to and block 70% to 90% of 5-HT2A receptors at clinically effective doses |
Mechanisms of Action
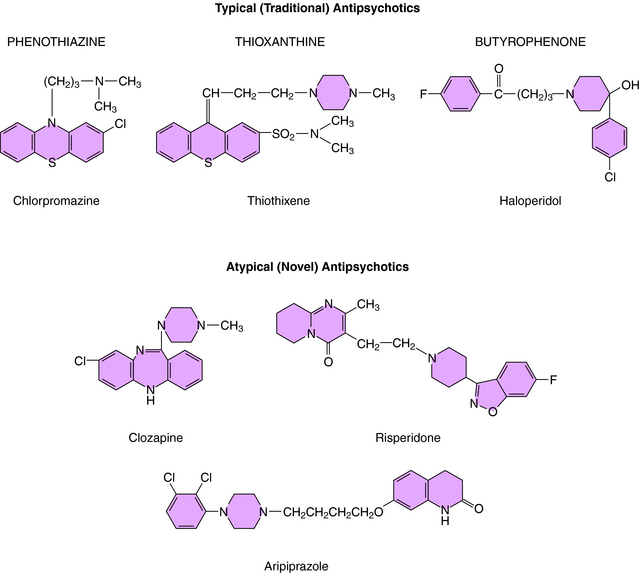
The typical antipsychotics comprised the first group of compounds developed for the treatment of schizophrenia. Based on chemical structure, these compounds fall into three groups (Fig. 29-1):
The effects of the typical antipsychotics are due to blockade of postsynaptic DA receptors, specifically D2 receptors. Indeed, a positive linear correlation exists between the therapeutic potency of typical antipsychotics and their ability to bind to and block D2 receptors (Fig. 29-2). Inhibition of these receptors in mesolimbic and mesocortical regions (see Fig. 27-8) is believed to mediate the ability of these compounds to relieve some behavioral manifestations of schizophrenia. On the other hand, blockade of these receptors in the basal ganglia underlies the motor side effects of these compounds, and inhibition of these receptors in the tuberoinfundibular pathway in the hypothalamus leads to increases in prolactin secretion from the pituitary gland.
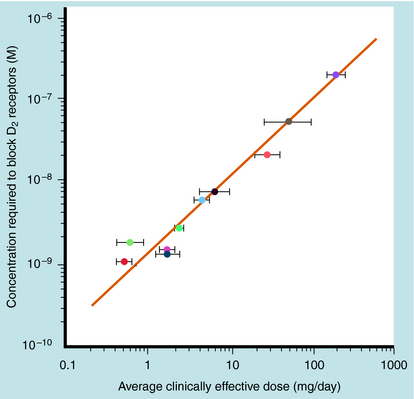
FIGURE 29–2 Correlation between the therapeutic dose of antipsychotics and the concentration to block D2 receptors.
Acute administration of the typical antipsychotics increases the firing rate of both mesolimbic and nigrostriatal DA neurons as a compensatory response to DA receptor blockade. However, long-term administration inactivates these pathways via depolarization blockade. Because the therapeutic effects of the typical antipsychotics require several weeks to become apparent, it is believed that this inactivation of mesolimbic DA neurons mediates the time-dependent amelioration of psychotic symptoms. Long-term administration of antipsychotics also leads to an up regulation of DA receptors as a consequence of the depression of DA activity.
The atypical antipsychotics represent a somewhat heterogeneous group of compounds with large differences in chemical structure (see Fig. 29-1), receptor antagonist activity, and therapeutic and side effect profiles. These compounds vary more in potency and range in treating specific symptoms as compared with the typical compounds. As heterogeneous as the group is, however, these compounds share several commonalities. They all occupy and block fewer D2 receptors than the typical antipsychotics (40% to 60% as compared with >70% to 80%), and they all block a high number (70% to 90%) of 5-HT2A receptors. Because of their lower occupancy of D2 receptors, the atypical antipsychotics have a lower propensity than the typical compounds to induce motor side effects. In addition, they may have an increased ability to alleviate the negative symptoms of schizophrenia, and the rate of relapse is lower than that after administration of typical antipsychotics.
Pharmacokinetics
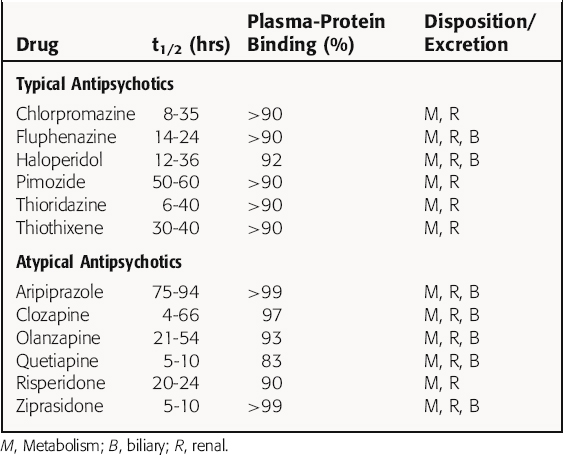
The antipsychotics are readily but erratically absorbed after oral administration, and most undergo significant first-pass metabolism. Most of these compounds are highly lipophilic and protein bound, with variable half-lives after oral administration. In general, most antipsychotics are oxidized by hepatic microsomal enzymes to inactive metabolites and are excreted as glucuronides. Major exceptions are thioridazine and risperidone. Thioridazine is metabolized to the active product mesoridazine, which is more potent than the parent compound. Interestingly, the primary active metabolite of risperidone, paliperidone, was approved by the United States Food and Drug Administration in 2007 in an extended-release formulation.
Depot formulations of some antipsychotics (e.g., fluphenazine decanoate, haloperidol decanoate, and risperidone) are available and can be used for maintenance therapy administered intramuscularly at 2- to 4-week intervals. For patients who have difficulty taking oral medications, risperidone and olanzapine are available as rapidly dissolving oral wafers. In addition, for management of acute psychotic episodes, antipsychotics can be administered intramuscularly, although ziprasidone and olanzapine are currently the only atypical antipsychotics available in this formulation. The risperidone-dissolving wafer provides rapid relief of symptoms as well. Haloperidol is available in an intravenous form, which is commonly used in intensive care settings. However, because intravenous haloperidol bypasses first-pass metabolism, it is effectively twice as potent as oral haloperidol dosing. In general, once an effective dose is established, a regimen of single daily oral dosing is effective for symptomatic treatment. Pharmacokinetic parameters are summarized in Table 29-1.
Relationship of Mechanisms of Action to Clinical Response
The DA hypothesis of psychotic behavior is based on findings that the chronic administration of amphetamine and other compounds that increase DA release leads to psychotic behaviors, the administration of compounds that enhance dopaminergic activity such as L-DOPA can induce psychotic behaviors, and a linear correlation exists between the therapeutic efficacy of the typical antipsychotics and their ability to block DA receptors (see Fig. 29-2). Similarly, a role for 5-HT in schizophrenia is based on evidence that many hallucinogens are structurally related to 5-HT. The newer atypical antipsychotics block 5-HT2 receptors with high potency, leading to a reduction or resolution of the hallucinations. Thus both DA and 5-HT clearly play a role in the manifestations of psychotic behavior.
Based on evidence that the atypical antipsychotics may improve the cognitive impairment exhibited by schizophrenics, in concert with their ability to increase blood flow and enhance ACh release in prefrontal cortex, studies have suggested a role for altered cholinergic systems in the cognitive impairment in psychotic behavior. This idea is underscored by the vast literature supporting a role for ACh in learning and memory and the role of impaired cholinergic activity in Alzheimer’s disease (see Chapter 28).
The choice of antipsychotic drug is based on the particular symptoms manifested by the patient as well as on sensitivity to undesirable side effects and previous therapeutic response to a particular agent. Although the typical antipsychotics have been first-line compounds, the use of atypicals is increasing because of their limited side effect profile, leading to better compliance. Although clozapine has not been considered a first-line drug because of multiple significant side effects (including agranulocytosis, seizures, and myocarditis), it is clearly of tremendous benefit for patients who fail to respond to other antipsychotics.
In addition to their use in schizophrenia, several antipsychotics have been of therapeutic benefit in other neuropsychiatric disorders. Many of the atypical antipsychotics (including risperidone, quetiapine, and olanzapine) are effective as the primary treatment or as an augmenting agent with mood stabilizers in the treatment of bipolar disorder, regardless of whether psychotic features were present at the time. The antipsychotics are often prescribed concomitantly with antidepressants and mood stabilizers for schizoaffective disorder (see Chapter 30). Haloperidol and pimozide are used to treat behavioral syndromes accompanied by motor disturbances, specifically Gilles de la Tourette’s syndrome.
Pharmacovigilance: Side Effects, Clinical Problems, and Toxicity
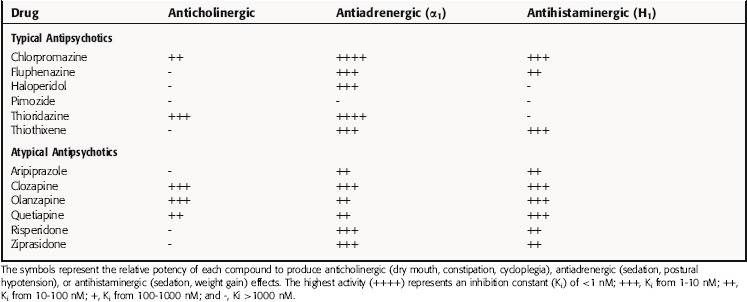
Although most antipsychotics are relatively safe, they can elicit a variety of neurological, autonomic, neuroendocrine, and metabolic side effects. Many side effects are an extension of the general pharmacological actions of these drugs and result from the blockade of receptors for several neurotransmitters (Table 29-2), whereas other side effects are specific to particular compounds.
All typical antipsychotics block muscarinic cholinergic receptors, leading to dry mouth, urinary retention, and memory impairment (see Chapter 10). These effects are more common with the lower-potency agents such as chlorpromazine and thioridazine. They also block α1 adrenergic and histamine (H1) receptors, producing orthostatic hypotension and reflex tachycardia, and sedation, respectively. Blocking DA receptors in the pituitary gland results in elevated prolactin secretion, and this hyperprolactinemia may lead to menstrual irregularities in females and breast enlargement and galactorrhea in both sexes. In addition, thioridazine has a propensity to prolong the cardiac QT interval, predisposing to a risk for ventricular arrhythmias. High-dose thioridazine therapy (>800 mg/day) has been associated with the development of retinitis pigmentosa. Thioridazine should be used with caution at all times, whether it is used as monotherapy or with other agents. As thioridazine is metabolized by CYP2D6, using it concurrently with a CYP2D6 inhibitor (such as paroxetine or fluoxetine) could greatly increase serum thioridazine levels, leading to an increase in adverse events.
Blocking DA receptors in the basal ganglia leads to acute extrapyramidal symptoms including dystonia, parkinsonism, and akathisia. Acute dystonic reactions, characterized by spasms of the facial or neck muscles, may be evident, as well as a parkinsonian syndrome characterized by bradykinesia, rigidity, tremor, and shuffling gait. Akathisia or motor restlessness may also be apparent. These symptoms occur early (1 to 60 days) after initiation of drug treatment, improve if the antipsychotic is terminated, and if severe enough to cause noncompliance, may be treated with centrally active anticholinergic compounds such as those used for Parkinson’s disease (see Chapter 28).
In general, the high-potency butyrophenones such as haloperidol are associated with a greater incidence of extrapyramidal side effects, whereas the low-potency phenothiazines such as chlorpromazine are associated with a greater incidence of autonomic side effects and sedation.
An idiosyncratic and potentially lethal effect of the typical antipsychotics is known as neuroleptic malignant syndrome, which occurs in 1% to 2% of patients and is fatal in almost 10% of those affected. It is most commonly seen in young males recently treated with an intramuscular injection of a typical antipsychotic agent. This syndrome is observed early in treatment and is characterized by a near-complete collapse of the autonomic nervous system, causing fever, muscle rigidity, diaphoresis, and cardiovascular instability. Immediate medical intervention with the DA receptor agonist bromocriptine (see Chapter 28) and the skeletal muscle relaxant dantrolene (see Chapter 12) is recommended to treat this condition.
the development of diabetes mellitus is believed to be caused by all atypical antipsychotics, it has been most commonly observed with olanzapine and clozapine. The atypical antipsychotics also cause increased plasma lipids, with as much as a 10% increase in cholesterol levels. Olanzapine and, to a lesser extent, quetiapine are the atypical agents most likely to induce hyperlipidemia. Like the typical antipsychotic thioridazine, the atypical compound ziprasidone can also increase the cardiac QT interval predisposing to arrhythmias. Quetiapine is very sedating and has also been associated with significant hypotension, especially during the titration phase of treatment.
New Horizons
Although much attention has focused on the role of DA and 5-HT in schizophrenia, recent studies have begun to focus on glutamatergic neurotransmission. The glutamate N-methyl-D-aspartate receptor antagonist phencyclidine (“angel dust”) mimics schizophrenia more accurately than any other compound. The behavioral effects of phencyclidine prompted investigators to postulate a glutamatergic deficiency in the etiology of schizophrenia, and recent studies have demonstrated that partial deletion of the gene encoding these receptors leads to the same behavioral abnormalities observed after phencyclidine. Thus attempts to enhance the activity of the N-methyl-D-aspartate receptor in schizophrenics with glycine or serine, both of which stimulate allosteric sites on the receptor, have resulted in some symptomatic improvement. In addition, preliminary data from a recent clinical trial have suggested that glutamate metabotropic receptor agonists may also be of benefit.