Chapter 31 Treatment of Anxiety and Insomnia
| Abbreviations | |
|---|---|
| CNS | Central nervous system |
| GABA | γ-Aminobutyric acid |
| 5-HT | Serotonin |
| IM | Intramuscular |
| IV | Intravenous |
Therapeutic Overview
Each disorder has its own distinct features, but they are all bound together by the common theme of excessive, irrational fear of impending doom, loss of control, nervousness, and dread. Depression often accompanies anxiety disorders, and when it does, it should be treated (see Chapter 30).
In addition to their use as anxiolytics, the benzodiazepines are also used for the treatment of insomnia, which often accompanies anxiety and depression. It has been estimated that 30% of all adults in the United States have insomnia, characterized by difficulty both initiating and maintaining sleep. Although the benzodiazepines were the mainstay for the treatment of insomnia for many years, newer agents have been developed including the benzodiazepine receptor agonists eszopiclone, zaleplon, and zolpidem, and the melatonin receptor agonist ramelteon. In addition, several over-the-counter antihistamine preparations are useful for insomnia including hydroxyzine and diphenhydramine (see Chapter 14).
This chapter focuses on the pharmacology of the benzodiazepines and related compounds. The pharmacology of the antidepressants is discussed in Chapter 30 and that of β adrenergic receptor antagonists in Chapter 11.
Therapeutic issues related to both anxiety and insomnia are summarized in the Therapeutic Overview Box.
| Therapeutic Overview | |
|---|---|
| Anxiety Disorders | Insomnia |
| Benzodiazepines | Benzodiazepines |
| Non-benzodiazepine anxiolytics | Benzodiazepine receptor agonists |
| • Buspirone | Melatonin receptor agonists |
| • β Adrenergic receptor antagonists | Antihistamines |
| Antidepressants | |
| • Antidepressants | |
Mechanisms Of Action
The benzodiazepines exert their effects through allosteric interactions at the γ-aminobutyric acid type A (GABAA) receptor. GABAA receptors are pentameric ligand-gated ion channels, and stimulation of these receptors by GABA leads to the influx of Cl– and a resultant hyperpolarization of the postsynaptic cell (see Chapter 1). This hyperpolarization renders the cell less likely to fire in response to an incoming excitatory stimulus, thus mediating the inhibitory effects of GABA throughout the central nervous system (CNS).
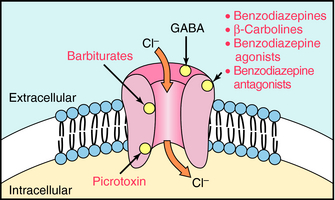
GABAA receptors contain primary agonist binding sites for GABA and multiple allosteric sites that can be occupied by numerous pharmacological compounds, as depicted in Figure 31-1. Benzodiazepines bind to one of these modulatory sites, often referred to as the benzodiazepine binding site or benzodiazepine receptor, whereas compounds such as the barbiturates and the poison picrotoxin bind to other sites on the receptor. When benzodiazepines bind to the benzodiazepine binding site, they induce a conformational change in the receptor, resulting in an increased frequency of chloride ion channel opening upon stimulation of the receptor by GABA. They are referred to as positive allosteric modulators because they increase the effect of the natural agonist but have no effect in the absence of agonist.
Benzodiazepines are not the only group of compounds that bind to this allosteric site. The β-carbolines such as harmine and harmaline also interact with this site. However, when these compounds bind, they allosterically reduce Cl– conductance by decreasing the affinity of GABA for its binding site. Because the β-carbolines increase CNS excitability and may produce anxiety and precipitate panic attacks, effects opposite to those of the benzodiazepines, they are called inverse agonists (see Chapter 1). The inverse agonists block the effects of the benzodiazepines but have no therapeutic use. However, they are found in nature and are thought to be responsible for the psychedelic properties of some plant species.
Non-Benzodiazepine Anxiolytics
β Adrenergic Receptor Antagonists
In addition to the benzodiazepines, buspirone, and the antidepressants, β adrenergic receptor antagonists such as propranolol (see Chapter 11) are useful for the treatment of performance anxiety. These compounds suppress the sympathetically-mediated somatic and autonomic symptoms of anxiety.
Benzodiazepine Receptor Agonists
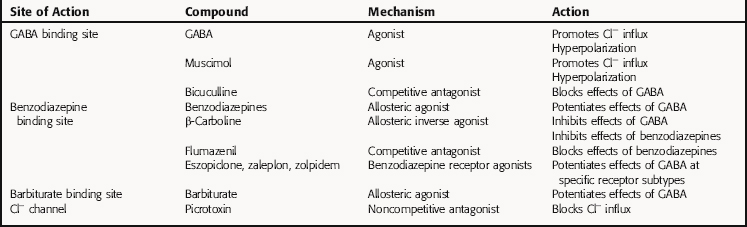
The benzodiazepine receptor agonists eszopiclone, zaleplon, and zolpidem, which are used to treat insomnia, are chemically unrelated to the benzodiazepines but bind to the same site as the benzodiazepines on the GABAA receptor. However, in contrast to the benzodiazepines, which bind to all GABAA receptors irrespective of their subunit composition, the benzodiazepine agonists bind only to a subset of GABAA receptors containing a specific subunit composition. Thus these compounds have a different pharmacological profile than the benzodiazepines (see Relationship of Mechanisms of Action to Clinical Response). A summary of the mechanisms of action of compounds affecting the GABAA receptor is presented in Table 31-1.
Ramelteon is the first and only melatonin receptor agonist approved for the treatment of insomnia characterized by difficulty falling asleep. Ramelteon, like the hormone melatonin, has high affinity for both melatonin type 1 (MT1) and type 2 (MT2) receptors, both of which are G-protein coupled receptors. MT1 and MT2 are expressed throughout the brain and highly abundant in the suprachiasmatic nucleus of the hypothalamus, an area that is intimately involved in regulating circadian rhythms and sleep and is often referred to as the circadian pacemaker or “master clock.” As a pacemaker, the suprachiasmatic nucleus exhibits an intrinsic rhythm of activity that is inhibited at night as a consequence of the release of melatonin from the pineal gland. Studies suggest that ramelteon, like melatonin, activates melatonin receptors to inhibit the activity of the suprachiasmatic nucleus, leading to the induction of sleep.
Pharmacokinetics
The duration of action of the benzodiazepines varies considerably, and the formation of active metabolites plays a major role in the effects of these compounds (Table 31-2). The benzodiazepines and their active metabolites are highly bound to plasma proteins, being greatest for diazepam (99%) and lowest for alprazolam (70%). The distribution of diazepam and other benzodiazepines is complicated somewhat by a considerable degree of biliary excretion, which occurs early in their distribution. This enterohepatic recirculation occurs with metabolites and parent compounds and may be important clinically for compounds with a long elimination half-life. The presence of food in the upper bowel delays reabsorption and contributes to the late resurgence of plasma drug levels and activity.
TABLE 31–2 Pharmacokinetic Parameters for Representative Benzodiazepines After Oral Administration
| Drug | Onset of Action* | t1/2† |
|---|---|---|
| Alprazolam | Intermediate | Intermediate |
| Chlordiazepoxide | Intermediate | Long |
| Clorazepate | Rapid | Long |
| Diazepam‡ | Rapid | Long |
| Flurazepam | Rapid | Long |
| Halazepam | Intermediate | Long |
| Lorazepam‡ | Intermediate | Intermediate |
| Oxazepam | Slow | Short |
| Prazepam | Slow | Long |
| Temazepam | Slow | Intermediate |
| Triazolam | Rapid | Short |
* Rapid = 15-30 min; Intermediate = 30-45 min; Slow = 45-90 min.
† Short, <10 hours; Intermediate, 10-36 hours; Long >48 hours.
‡ Also administered by injection.
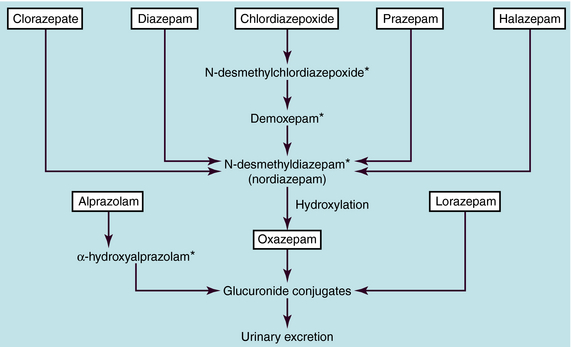
The benzodiazepines are metabolized extensively by hepatic microsomal enzymes (Fig. 31-2). The major biotransformation reactions are N-dealkylation and aliphatic hydroxylation, followed by conjugation to inactive glucuronides that are excreted in the urine. The long-acting benzodiazepines clorazepate, diazepam, chlordiazepoxide, prazepam, and halazepam are dealkylated to the active compound N-desmethyldiazepam (nordiazepam). This compound has an elimination half-life of 30 to 200 hours and is responsible for the long duration of action of these compounds. N-desmethyldiazepam is hydroxylated to oxazepam, which forms a glucuronide conjugate. Alprazolam undergoes hydroxylation followed by glucuronidation, and lorazepam is directly glucuronidated.
Relationship of Mechanisms of Action to Clinical Response
Anxiety is managed effectively with the benzodiazepines, particularly alprazolam, lorazepam, and clonazepam. Their intermittent use for acute attacks or limited long-term use (4 to 8 weeks) for recurring symptoms is often beneficial. However, all benzodiazepines should be used cautiously in patients with a history of addiction or more chronic and severe emotional disturbances. Panic attacks respond favorably to alprazolam, which has been shown to possess antidepressant activity similar to that of the tricyclic antidepressants, which are also used for the treatment of panic attacks (see Chapter 30). A debilitating anxiety caused by another illness can be controlled by short-term treatment with anxiolytic drugs while treatment for the primary condition is implemented.
Sedation is the most common effect of the benzodiazepines, and its intensity and duration depend on the dose and concentration of drug in plasma and brain. Although flurazepam, temazepam, and triazolam are used for the treatment of insomnia, they may lead to daytime sedation because of their long duration of action. Oxazepam has a shorter duration of action and would be less likely to cause this problem. The benzodiazepines decrease the latency of sleep onset (time to go to sleep), increase the amount of time spent in stage 2 sleep, and increase total sleep time. However, REM sleep and stage 4 (slow wave) sleep are depressed. If the benzodiazepines are discontinued, a rebound increased REM sleep occurs, characterized by bizarre dreams. Tolerance occurs to the sedative, but not the anxiolytic effect of the benzodiazepines.
Owing to their ability to produce sedation and anterograde amnesia and reduce the anxiety, stress, and tension associated with surgical or diagnostic procedures, benzodiazepines are used both as preanesthetic medications and for induction and maintenance of anesthesia (see Chapter 35). For procedures that do not require anesthesia, such as endoscopy, cardioversion, cardiac catheterization, specific radiodiagnostic procedures, and reduction of minor fractures, benzodiazepines may be administered orally, IM, or IV.
In addition to these major indications, the benzodiazepines have also been found to be of use for treatment of alcohol withdrawal. Because the benzodiazepines exhibit cross-tolerance with alcohol, have anticonvulsant activity, and do not have major respiratory depressant effects, they have become drugs of choice for treatment of acute alcohol withdrawal symptoms (see Chapter 32). In particular, chlordiazepoxide, lorazepam, and diazepam have now replaced other drugs for this purpose. Choosing between these medications for alcohol withdrawal is often based on metabolic considerations. If a patient has hepatic impairment, lorazepam is often preferred to treat the symptoms of alcohol withdrawal, because it is metabolized in both liver and kidney. If hepatic dysfunction is not an issue, the use of drugs primarily metabolized by the liver (such as chlordiazepoxide and diazepam) would be appropriate.
Non-Benzodiazepine Anxiolytics
β Adrenergic Receptor Antagonists
In addition to the benzodiazepines, buspirone, and the antidepressants, β adrenergic receptor antagonists such as propranolol (see Chapter 11) are useful for the treatment of performance anxiety or “stage fright.” These compounds are effective in suppressing the somatic and autonomic symptoms of anxiety but do not alter emotional symptoms. Interestingly, the α2 adrenergic receptor agonist, clonidine, has also been reported to have anxiolytic properties.
Pharmacovigilance: Side Effects, Clinical Problems, and Toxicity
Drug Withdrawal and Dependence
The benzodiazepines have been reported to have a high abuse potential. However, evidence suggests that psychological dependence occurs mainly in people with a history of drug abuse; appropriate therapeutic use by persons not predisposed to drug abuse should not lead to abuse of the benzodiazepines.
Benzodiazepine Receptor Agonists
The abuse liability of zaleplon and zolpidem is less than that of the benzodiazepines when used at the doses recommended. However, when used at higher doses, zolpidem may lead to some physical dependence, and abrupt discontinuation may lead to withdrawal, although less severe than that observed with the benzodiazepines. There is no evidence for abuse liability with eszopiclone.