Chapter 175 Transoral Approaches to the Cervical Spine
Pathology
Numerous pathologies of the anterior craniocervical junction have been approached surgically. Degenerative conditions leading to basilar invagination, odontoid fractures or nonunion, C1-C2 instability with pannus formation of basilar invagination with brain stem compression, odontoid hypoplasia, and tumors involve the majority of such surgically treatable lesions.1,2 Understanding the pathology to be treated at the ventral craniocervical junction is critical in determining the optimal surgical approach. In general, the ideal surgical approach to this area is dictated by whether a particular pathological entity is extradural and whether it will be optimally treated in a piecemeal fashion or as an en bloc resection. Most degenerative conditions, for instance, are extradural and can be treated anteriorly with piecemeal decompression of the brain stem and spinal cord. This may also be the case for small, benign, extradural lesions. En bloc resections, however, are reserved mainly for primary tumors in which long-term local control may improve survival or neurological function, such as with primary bone tumors. En bloc resections require more extensive exposure to allow the surgeon access to the entire pathology and thus may be associated with significant morbidity.
Anatomy
Knowledge of the course of the vertebral artery in the upper cervical spine as it enters the foramen magnum is critical during anterior approaches to the craniocervical junction. The vertebral artery enters the osseous cervical spine, typically at C5, and is encased in transverse foramina as it ascends to C2. It then runs posterolaterally and enters the C1 transverse foramen. The artery continues medially along the vertebral artery groove that lies on the superior aspect of the posterior atlas posteriorly. It then advances superiorly and enters the foramen magnum.
It is important to note that the C2 segment of the vertebral artery lies more anteromedially than the C1 segment.3 This should be kept in mind when drilling C1 and C2 to avoid vertebral artery injury. However, it is also critical to acknowledge that the course of the vertebral artery in the craniocervical junction can be anomalous, and all imaging studies should be reviewed carefully to avoid encountering the vertebral artery unexpectedly.
Transoral-Transpharyngeal Approach With or Without Palatotomy
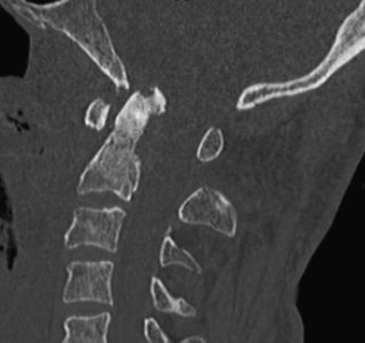
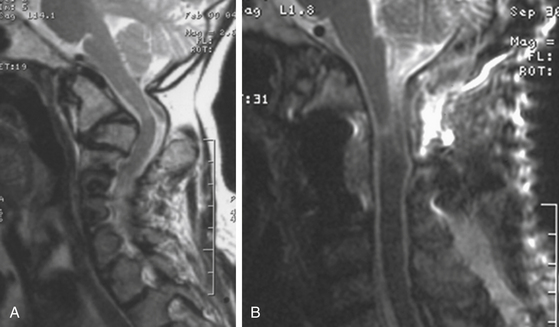
Traditionally, the anterior craniocervical junction has been approached by using a transoral-transpharyngeal route, known also as the “buccopharyngeal approach.” This approach provides access to the lower clivus, foramen magnum, anterior arch of C1, and the underlying odontoid process of C2, and down to the C3 vertebral body in some patients. The general goal of transoral operations is to correct irreducible anterior compression at the cervicomedullary junction (Figure 175-1).4–7 In this way, it may provide the most direct approach to an abnormality ventral to the brain stem and upper cervical cord. Since 1917, when Kanavel first described the removal of a bullet lodged at the craniocervical junction by using the transoral-transpharyngeal approach,8 transoral approaches have been used extensively for a wide range of pathological entities. Largely due to advancements in imaging techniques and improved availability of the operating microscope, there have been significant improvements in the efficacy and safety of the transoral approach over the past several decades.2,4,7,9
Technique
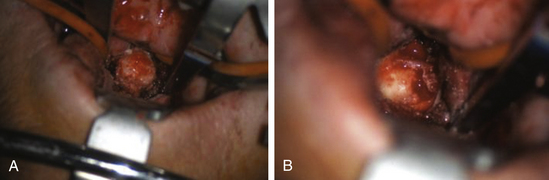
The patient is placed supine on the operating table. This should be done while the patient is awake to monitor for neurological changes. Intubation can proceed orotracheally or by tracheostomy. Orotracheal intubation should be performed fiberoptically in patients with cervical instability or cervicomedullary compression, and the tube must be retracted away, out of view. After inducing general anesthesia, a feeding tube is placed to allow for enteral nutrition postoperatively. The neck is placed in gentle extension, and the head is supported on a horseshoe support or rigidly held in place with a Mayfield skull clamp. It is our practice to continuously monitor the motor evoked potentials and somatosensory potentials if possible throughout the operation. Direct palpation of the posterior oropharynx can allow identification of the anterior arch of C1 and the body of C2, thus defining the operative anatomy. Gauze throat packs are placed to occlude the larynx and esophagus to prevent leakage of blood into the stomach. The oral cavity is then cleansed with chlorhexidine gluconate oral solution, and intravenous antibiotics are provided. The patient’s face is draped to allow access to the mouth and the nasal cavity. A self-retaining oral retractor is then placed over the teeth and expanded to keep the mouth open. Self-retaining retractors are then attached to the retractor to keep the tongue depressed (Figure 175-2). Tongue retraction should be released at 30-min intervals to prevent lingual congestion from venous and lymphatic compression.
A red rubber catheter can be placed through the nose and then sutured to the uvula. The catheter can then be withdrawn through the nose to retract the uvula out of the field. If further exposure is necessary, the soft palate can be split at the midline to extend the superior and lateral exposure and prevent obscuration by the uvula. This procedure allows for improved exposure of the lower clivus. The soft palate is divided at its midline extending from the junction with the hard palate to the base of the uvula with deviation off the midline to preserve the uvula itself. Silk sutures are placed and fastened to the mouth gag to provide retraction of the soft palate flaps. The posterior pharyngeal mucosa is infiltrated with 1% lidocaine with 1:100,000 epinephrine, and a midline posterior incision is made extending from the base of the clivus to the upper border of the third cervical vertebra. The anterior tubercle of C1 can help determine the midline, although this landmark is misleading in cases of rotational subluxation. The extent of this incision can be guided by using lateral fluoroscopy or frameless navigation systems.2 Some authors suggest creating an inferiorly based, U-shaped pharyngeal flap such that the apex of the flap lies just above the superior aspect of the anterior arch of C1. This incision can be extended superiorly if more rostral clivus must be exposed. The pharyngeal mucosa, pharyngeal constrictor musculature, and longus colli and longus capitis musculature are then elevated as a single myomucosal flap from the underlying anterior longitudinal ligament. The anterior ligaments of the spine are then coagulated with an insulated electrocautery device and dissected off the inferior clivus, the anterior arch of C1, and the anterior bodies of C2 and C3. The pharyngeal flaps are retracted using Crockard self-retaining retractors.
The transoral-transpharyngeal approach allows lateral exposure of roughly 15 to 20 mm bilaterally off the midline from the inferior clivus to the C3 body (Figure 175-3 and 175-4). Further lateral exposure risks trauma to the Eustachian tube orifice, hypoglossal nerve, Vidian nerve, and carotid artery as it passes in front of the C1 arch laterally.
Several complications that may be encountered during the transoral-transpharyngeal approach deserve specific attention. Cerebrospinal fluid (CSF) leaks can lead to devastating complications, should be avoided when possible, and should be managed aggressively when encountered. The treatment of certain spinal pathologies is more likely to lead to inadvertent dural transgression. For example, during transoral odontoidectomies for basilar invagination, as the dens migrates further rostrally, the apical aspect of the dens may erode through the dura and may lead to CSF leaks. The posterior longitudinal ligament and tectorial membrane may be thinned by the dens or a pannus and be more susceptible to inadvertent violation. Because the pannus may resolve after posterior fusion, aggressive resection of the pannus may not be necessary. If the dura is transgressed, primary closure is performed with placement of fascia and bovine pericardium if possible, and the dural closure is reinforced with fat and/or fibrin glue as needed. In such cases, a lumbar subarachnoid drain is placed for CSF diversion. Watertight closure of the posterior pharynx should be performed in two layers (pharyngeal musculature and pharyngeal mucosa), as a single-layer closure may be susceptible to dehiscence.10 Continued leakage of CSF can be difficult to manage and may lead to meningitis.
The soft palate (if sectioned) is then carefully approximated in three layers (nasal mucosa, muscularis, and oral mucosa), all with the use of interrupted absorbable sutures. Triamcinolone acetonide cream USP 0.025% (E. Fougera & Co., Melville, NY, USA) may be applied to the tongue to reduce postoperative swelling.11 The patient should be left intubated for 24 to 48 hr postoperatively to allow for resolution of airway edema.
Velopalatine incompetence after palate-splitting techniques is a well-known complication.12 Clinical symptoms include nasal speech, dysphagia, and regurgitation of liquids. It is attributed to fibrosis of the soft palate or the pharyngeal wall. Use of a dental obturator and pharyngeal retraining may help to improve clinical symptoms.
Recent advances may potentially allow surgeons to stabilize the cervical spine using the same exposure provided by the transoral-transpharyngeal approach. For example, transoral atlantoaxial reduction plate systems3 may allow for stabilization of C1 and C2 using the same surgical exposure required for the treatment of common craniocervical junction pathology. Long-term follow-up and biomechanical studies are needed to support the efficacy of these new technologies.
Endoscopy in Transoral Surgery
Continuing advances in endoscopic surgery with respect to both technique and technology may potentially benefit surgeons during transoral approaches to the cervical spine. Endoscopic approaches have the benefit of allowing the surgeon to obtain the same, if not better, visualization of the operative field while minimizing the extent of surgical exposure. For example, the ability to visualize the lower and middle clivus is limited with the transoral approach. Improved visualization may necessitate full soft palate splitting, hard palate splitting, or extended maxillotomy procedures. Since such procedures may increase operating time, prolong recovery, and increase patient morbidity, a 30° endoscope may be used to avoid the need for these additional procedures.10,11 By using the endoscope, the operator is able to look in all directions by rotating the instrument. Because the light source is at the level of the abnormality, superior illumination can be obtained. With the aid of the endoscope, abnormalities extending as high as midclivus can be visualized without extensive soft or hard palate manipulation. The drawbacks of using such techniques are the learning curve required for surgeons unfamiliar with endoscopy and the loss of three-dimensional visualization. As surgeons gain skills in using endoscopic techniques, the ability to limit the morbidity associated with transoral techniques may be improved.
Although the transoral approach to the cervicothoracic junction is considered the gold standard, innovators are harnessing endoscopic techniques to find alternative avenues to approaching the anterior cervicothoracic junction. By utilizing endoscopic techniques, surgeons can traverse the endonasal cavity as an alternative to traditional transoral techniques. Kassam and colleagues13 were the first to report the clinical application of this technique, which was used during an operation on a patient with rheumatoid arthritis and cervicomedullary compression. With the use of a fully endoscopic endonasal approach, a complete odontoidectomy was performed successfully. The pharyngeal incision was made above the soft palate, which afforded the surgeon the theoretical advantages of limiting postoperative swallowing dysfunction in the patient and minimizing the patient’s exposure to oral bacterial flora. By potentially obviating the need for soft palate manipulation that is often required during transoral approaches, the risk of regurgitation, hypernasal speech, and dysphagia may also be minimized. Furthermore, because the surgical trajectory is more caudal than in the traditional transoral route, it is possible to remove the odontoid process without disturbing the C1 ring.13 Long-term follow-up of a larger series of patients will elucidate the potential benefits of the endonasal approach to the craniocervical junction.
Transoral-Transpharyngeal Plus Maxillary Osteotomy
Le Fort I maxillary osteotomies have traditionally been performed to correct midfacial deformities and to gain access to nasopharyngeal tumors. With regard to the craniocervical junction, Le Fort I approaches can provide wide exposure to the midline extracranial compartment of the cranial base. The inferior and middle clivus is made more accessible with the use of such approaches. Although considered a standard and relatively straightforward operation by the oral and maxillofacial surgeon, this procedure may not be familiar to otolaryngologists and spine surgeons. The standard transoral approach may be combined with a unilateral Le Fort I osteotomy, bilateral Le Fort I osteotomies, or a unilateral extended maxillectomy. In general, if exposure of the midline compartment of the extracranial skull base without exposure of the C1-C2 joints is all that is required, then the Le Fort I approach may be useful. Swallowing and speech difficulties can be quite frequent with maxillary osteotomies, especially when soft palate division is involved.
Although any of the above three variations can be used, the transoral-transpharyngeal approach combined with a unilateral Le Fort I osteotomy midline hard palate osteotomy often provides adequate exposure with the least potential for morbidity.3 For instance, the unilateral Le Fort I osteotomy has been shown to lead to more rapid recovery of oropalatal function, which is likely due to preservation of the soft palate and one half of the maxilla.16 In addition, when bilateral Le Fort I osteotomies are performed without a midline split of the hard palate, the inferiorly displaced maxillae and hard palate can obscure the lower operative field. Although bilateral Le Fort I osteotomies may provide the greatest exposure of the three approaches, they are associated with greater oropalatal morbidity and dental malocclusion. The technique used for a unilateral Le Fort I osteotomy is described below. If the exposure gained by this approach is limited, the same sequence of steps can be repeated on the contralateral side, thus creating a bilateral approach.
Transoral-Transpharyngeal Plus Transmandibular Circumglossal Approach
Just as Le Fort maxillotomies can be performed to extend the upper limit of the transoral approach, mandibular splitting can be used to extend the lower limits of the transoral approach. Jaw-splitting approaches may also extend superior access by allowing surgeons to drop their hands inferiorly and work superiorly.14,15
Technique
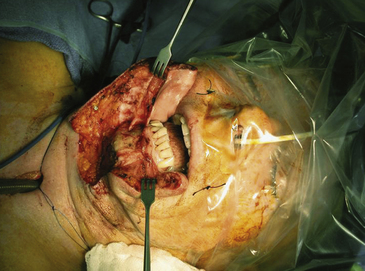
Patients undergoing transmandibular procedures require a preoperative tracheostomy. A curvilinear incision is made starting from the mastoid and extending inferomedially along a skin crease to reach the cervical midline at the level of the thyroid cartilage. The incision is then curved vertically to the mentum and through the lower lip. The platysma is identified and elevated to expose the mandible (Figure 175-5). This provides adequate exposure for the identification and preservation of the lingual and hypoglossal nerves, the internal carotid artery, the external carotid artery, and the jugular vein. A mandibulotomy between the lower middle incisors is marked using a surgical marker. A preoperative dental radiograph is useful for the detection of aberrant dentition that may potentially be injured during the mandibulotomy. Before performing the mandibular osteotomy, it is crucial to plan the location of the mandibular fixation plate. Marking and drilling holes for the plate allow for optimal fixation of the mandible and normal postoperative mouth closure.
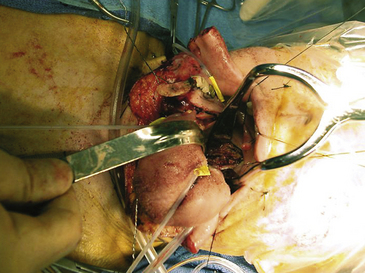
After the mandibular osteotomy is performed, the floor of the mouth is dissected posteriorly and care is taken to identify and preserve the hypoglossal nerve (cranial nerve XII) (Figure 175-6). The ipsilateral 12th nerve will be displaced with the tongue. This allows for medial retraction of the tongue and lateral retraction of the mandible. Cranial nerves IX through XII as well as the internal carotid artery and internal jugular vein are then identified and traced to the skull base. As the dissection proceeds toward the anterior tonsillar pillar, the incision divides into two limbs. The superior limb transects the soft palate to reach the hard palate. The incision follows the medial border of the alveolar ridge to the contralateral hard palate. The inferior limb extends laterally to the opening of the Eustachian tube. The Eustachian tube, as well as the levator and tensor veli palatini muscles, are transected, and the pharynx is then dissected away from the longus colli muscles to expose the cervical spine and clivus (Figure 175-7). If necessary, the hard palate can be resected to allow for exposure of the sphenoid sinus and upper clivus.
Transcervical Endoscopic Odontoidectomy
One limitation of transpharyngeal and endonasal approaches is that the pharynx and/or oral mucosa are traversed, which inherently contaminates the operative field with oral flora. The risks for infection, poor pharyngeal healing, and meningitis (if the dura is transgressed) can all be increased. In addition, such exposures often require extended periods of postoperative intubation and/or tube feeding to allow both the oropharynx and the jaw to heal. An alternative route to the anterior craniocervical junction is the endoscopic transcervical approach to the craniocervical junction.2 This approach is based on a traditional Smith-Robinson anterior cervical approach17 and follows the same trajectory as that used with a transodontoid screw (see Chapter 176), thus allowing exposure from the cervical spine (C7) to the inferior clivus. In this way, the approach and anatomy are familiar to spine surgeons. More importantly, the oral cavity is completely isolated from the surgical field. No tracheostomy or feeding tube needs to be placed, permitting early postoperative extubation and initiation of oral feeding. However, because surgery must be performed via a tubular retractor, the approach allows only piecemeal removal of craniocervical pathology and is not recommended for resecting large tumors. In addition, as is the case for transodontoid screw placement, an ideal trajectory may not be achieved in patients who are obese, barrel-chested, or have severe cervical spine kyphosis.
Technique
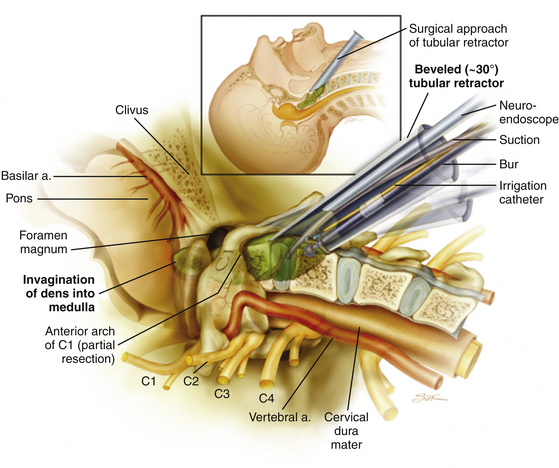
The patient is positioned supine on a radiolucent operating table. The head position is fixed with a halo ring through a Mayfield adapter to the table. After the patient is properly positioned, a frameless stereotactic reference frame is attached to the halo ring. A computed tomography–like image is acquired by using isocentric fluoroscopy, thus registering the patient’s anatomy in the current position into the navigation system. After image acquisition, the neck is prepared and draped, and preoperative intravenous antibiotics are administered. The approach is based on the standard Smith-Robinson approach to the cervical spine.17 An incision is made on the right-hand side (by right-handed surgeons) at approximately the C4-C5 level, starting in the midline and heading transversely for 3.5 cm. An avascular plane is opened with blunt finger dissection between lateral neck structures (sternocleidomastoid muscle, carotid sheath and its contents), the medial neck structures (trachea, esophagus), and the omohyoid muscle at the caudal border. When the spine is encountered, dissection proceeds rostrally until the anterior tubercle of C1 is identified. A beveled tubular retractor is then inserted and rigidly secured to the bed such that it is docked in the midline with the rostral tip of the retractor on the C1 tubercle and the caudal aspect over the C2-C3 disc. A 30° endoscope is placed down the retractor such that the endoscope lies in the superior aspect of the retractor field. At this point, endoscopic visualization of anatomic landmarks is corroborated using the frameless stereotactic system. With the use of a high-speed diamond bur, the bony resection starts at the C2-C3 disc level. Following the ventral margin of C2, the bone is drilled away in a caudal-to-rostral direction (Figure 175-8). The lateral margins of bone removal are toward the lateral aspects of the odontoid. The bony removal advances rostrally, posterior to the arch of C1, until the most superior point of the odontoid is reached. The odontoid is then resected in a “top-down” fashion as described above. If a dural violation is encountered, the dura can be repaired with DuraGen collagen matrix (Integra LifeSciences Corp., Plainsboro, NJ, USA) and fibrin glue. As there is no communication with the oropharynx, the risks of bacterial contamination and meningitis are low. If DuraGen and fibrin glue fail to close the CSF leak, a contained pseudomeningocele may form in the neck. This is usually asymptomatic and normally resolves without operative intervention.
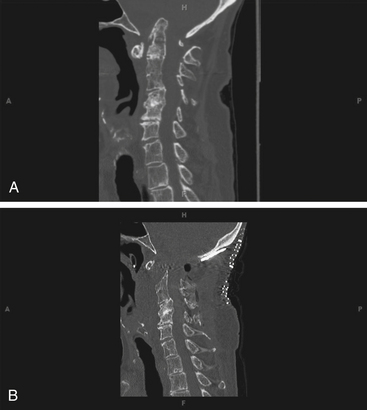
Following such decompression, the incision is closed in a standard, multilayered fashion as would be done for a Smith-Robinson cervical exposure. The halo ring is secured to the halo vest with the neck in a neutral position, and the patient is repositioned for a posterior cervical or occipital cervical fusion. Postoperatively, the patient is left intubated overnight. Following extubation, the patient can resume oral nutrition intake (Figure 175-9).
Discussion
The transoral-transpharyngeal approach has been the gold standard for surgical approaches to treat pathologies of the anterior craniocervical junction. However, it requires an understanding of the oral and pharyngeal anatomy and demands technical skills generally used by oromaxillofacial surgeons and otolaryngologists, but not spine surgeons. Drawbacks of the standard transoral approaches include a limited intraoperative view, a deep working distance, contamination by normal oral flora, posterior pharyngeal wound complications, oropalatal dysfunction, tongue edema, the potential need for prolonged intubation, and tube feeding to allow the pharynx to heal. An alternative to the transoral approach is the endoscopic transcervical approach. Limitations on the extent of exposure with these two different approaches can potentially be resolved by extending the transoral approach via a maxillary osteotomy or transmandibular circumglossal approach. The addition of such procedures may significantly increase morbidity, however. Specifically, postoperative complications may include malocclusion; injury to the hypoglossal and lingual nerves with accompanying neurological deficits in the lower face, oral cavity, and tongue; mandibular pseudarthrosis; mandibular osteonecrosis (especially with postoperative irradiation); scarring of the lip and face; periodontal disease, temporomandibular joint dysfunction; conductive hearing loss and serous otitis media resulting from sectioning of the Eustachian tube; and swallowing and speech difficulties.18 In addition, such procedures often require tracheostomy and percutaneous endoscopic gastrostomy tubes to facilitate enteral feeding.
The risks and consequences of such approaches are great. However, given the high morbidity of pathological conditions of the craniocervical junction in general and the possibility of improving local control over large tumors in this area, these complex anterior approaches can be used with good overall success in the correctly chosen patient. In terms of comparing the various approaches, Ammirati et al19 conducted an anatomical study to help determine the surgical access provided by some of the complex anterior approaches discussed in this chapter. Interestingly, they concluded that good exposure of the midline compartment of the extracranial cranial base is provided by the median mandibulotomy-glossotomy (70% of the total achievable exposure), a Le Fort I approach with splitting of the hard palate (80% of the total achievable exposure), and mandibular swing transcervical resection (96% of the total achievable exposure), with stepwise concomitant increases in the morbidity and complexity of the approaches. For this reason, they recommend the use of median mandibulotomy-glossotomy or the Le Fort I approach with incorporation of hard palate splitting for extracranial midline access if access to the atlanto-occipital and C1-C2 joints is not necessary. If such joint exposure is necessary, however, the mandibular swing transcervical approach should be considered. In addition, when wide exposure of the lateral compartment of the extracranial cranial base is necessary, the mandibular swing transcervical technique (100% of the total achievable exposure) has substantial advantages over the other approaches.
Ai F., Yin Q., Wang Z., et al. Applied anatomy of transoral atlantoaxial reduction plate internal fixation. Spine. 2006;31:128-132.
Ammirati M., Bernardo A. Analytical evaluation of complex anterior approaches to the cranial base: an anatomic study. Neurosurgery. 1998;43:1398-1408.
Apuzzo M.L.J., Weiss M.H., Heiden J.S. Transoral exposure of the atlantoaxial region. Neurosurgery. 1978;3:201-207.
Arbit E., Patterson R.H.Jr. Combined transoral and median labiomandibular glossotomy approach to the upper cervical spine. Neurosurgery. 1981;8:672-674.
Bertrand J., Luc B., Philippe M., Philippe P. Anterior mandibular osteotomy for tumor extirpation: a critical evaluation. Head Neck. 2000;22:323-327.
Blazier C.J., Hadley M.N., Spetzler R.F. The transoral surgical approach to craniovertebral pathology. J Neurosci Nurs. 1986;18:57-62.
Crockard H.A. Ventral approaches to the upper cervical spine [in German]. Orthopade. 1991;20:140-146.
Fang H.S.Y., Ong G.B. Direct anterior approach to the upper cervical spine. J Bone Joint Surg Am.. 1962;44A:1588-1604.
Frempong-Boadu A.K., Faunce W.A., Fessler R.G. Endoscopically assisted transoral-transpharyngeal approach to the craniovertebral junction. Neurosurgery. 2002;51(suppl 5):S60-S66.
Husain M., Rastogi M., Ojha B.K., et al. Endoscopic transoral surgery for craniovertebral junction anomalies. J Neurosurg Spine. 2006;5:367-373.
Kanavel A.B. Bullet located between the atlas and the base of the skull: technique of removal through the mouth. Surg Clin Chicago. 1917;1:361-366.
Kassam A.B., Snyderman C., Gardner P., et al. The expanded endonasal approach: a fully endoscopic transnasal approach and resection of the odontoid process. Technical case report. Neurosurgery. 2005;57(suppl 1):E213.
Menezes A. Surgical approaches: postoperative care and complications “transoral-transpalatopharyngeal approach to the craniocervical junction.”. Childs Nerv Syst. 2008;24:1187-1193.
Menezes A.H., Graf C.J., Hibri N. Abnormalities of the cranio-vertebral junction with cervico-medullary compression: a rational approach to surgical treatment in children. Childs Brain. 1980;7:15-30.
Menezes A.H., VanGilder J.C., Graf C.J., McDonnell D.E. Craniocervical abnormalities: a comprehensive surgical approach. J Neurosurg. 1980;53:444-455.
Robinson R.A., Southwick W.O. Surgical approaches to the cervical spine. Instr Course Lect. 1960;17:299-330.
Ryu S.I., Kim D.H. Surgical approaches for decompression and fixation of the craniovertebral junction. In: Dickman C.A., Fehlings M.G., Gokaslan Z.L. Spinal Cord and Spinal Column Tumors. New York, NY: Thieme; 2006:420-436.
Sandor G.K., Charles D.A., Lawson V.G., Tator C.H. Transoral approach to the nasopharynx and clivus using the Le Fort I osteotomy with midpalatal split. Int J Oral Maxillofac Surg. 1990;19:352-355.
Wolinsky J.P., Sciubba D.M., Suk I., Gokaslan Z.L. Endoscopic image-guided odontoidectomy for decompression of basilar invagination via a standard anterior cervical approach: technical note. J Neurosurg Spine. 2007;6:184-191.
1. Fang H.S.Y., Ong G.B. Direct anterior approach to the upper cervical spine. J Bone Joint Surg Am.. 1962;44A:1588-1604.
2. Wolinsky J.P., Sciubba D.M., Suk I., Gokaslan Z.L. Endoscopic image-guided odontoidectomy for decompression of basilar invagination via a standard anterior cervical approach: technical note. J Neurosurg Spine. 2007;6:184-191.
3. Ai F., Yin Q., Wang Z., et al. Applied anatomy of transoral atlantoaxial reduction plate internal fixation. Spine. 2006;31:128-132.
4. Apuzzo M.L.J., Weiss M.H., Heiden J.S. Transoral exposure of the atlantoaxial region. Neurosurgery. 1978;3:201-207.
5. Crockard H.A. Ventral approaches to the upper cervical spine [in German]. Orthopade. 1991;20:140-146.
6. Menezes A.H., Graf C.J., Hibri N. Abnormalities of the cranio-vertebral junction with cervico-medullary compression: a rational approach to surgical treatment in children. Childs Brain. 1980;7:15-30.
7. Menezes A.H., VanGilder J.C., Graf C.J., McDonnell D.E. Craniocervical abnormalities: a comprehensive surgical approach. J Neurosurg. 1980;53:444-455.
8. Kanavel A.B. Bullet located between the atlas and the base of the skull: technique of removal through the mouth. Surg Clin Chicago. 1917;1:361-366.
9. Blazier C.J., Hadley M.N., Spetzler R.F. The transoral surgical approach to craniovertebral pathology. J Neurosci Nurs. 1986;18:57-62.
10. Husain M., Rastogi M., Ojha B.K., et al. Endoscopic transoral surgery for craniovertebral junction anomalies. J Neurosurg Spine. 2006;5:367-373.
11. Frempong-Boadu A.K., Faunce W.A., Fessler R.G. Endoscopically assisted transoral-transpharyngeal approach to the craniovertebral junction. Neurosurgery. 2002;51(suppl 5):S60-S66.
12. Menezes A. Surgical approaches: postoperative care and complications “transoral-transpalatopharyngeal approach to the craniocervical junction.”. Childs Nerv Syst. 2008;24:1187-1193.
13. Kassam A.B., Snyderman C., Gardner P., et al. The expanded endonasal approach: a fully endoscopic transnasal approach and resection of the odontoid process. Technical case report. Neurosurgery. 2005;57(suppl 1):E213.
14. Arbit E., Patterson R.H.Jr. Combined transoral and median labiomandibular glossotomy approach to the upper cervical spine. Neurosurgery. 1981;8:672-674.
15. Sandor G.K., Charles D.A., Lawson V.G., Tator C.H. Transoral approach to the nasopharynx and clivus using the Le Fort I osteotomy with midpalatal split. Int J Oral Maxillofac Surg. 1990;19:352-355.
16. Ryu S.I., Kim D.H. Surgical approaches for decompression and fixation of the craniovertebral junction. In: Dickman C.A., Fehlings M.G., Gokaslan Z.L. Spinal Cord and Spinal Column Tumors. New York, NY: Thieme; 2006:420-436.
17. Robinson R.A., Southwick W.O. Surgical approaches to the cervical spine. Instr Course Lect. 1960;17:299-330.
18. Bertrand J., Luc B., Philippe M., Philippe P. Anterior mandibular osteotomy for tumor extirpation: a critical evaluation. Head Neck. 2000;22:323-327.
19. Ammirati M., Bernardo A. Analytical evaluation of complex anterior approaches to the cranial base: an anatomic study. Neurosurgery. 1998;43:1398-1408.