Chapter 170 Transforaminal Lumbar Interbody Fusion
Indications and Techniques
Lumbar fusion is an accepted treatment for spinal deformity, iatrogenic instability following decompressive procedures, and more controversially refractory axial back pain caused by degenerative disease of the spine.1 Lumbar interbody fusion yields certain advantages over posterolateral fusion alone, particularly because of higher rates of fusion.2 Segmental motion still exists with posterolateral fusion alone, but this motion is significantly reduced with fusion techniques through the intervertebral disc space.3,4 Biomechanically, the disc contributes significantly to anterior column stability, and the stabilizing influence of a posterolateral fusion depends on an intact anterior column.5 Transforaminal lumbar interbody fusion (TLIF) reestablishes anterior column support while allowing for posterior fixation, thereby imparting improved fusion rates because of circumferential support.6 Furthermore, as an interbody technique, TLIF helps restore disc and foraminal height and promotes lumbar lordosis.7 TLIF obviates the morbidity from the retroperitoneal dissection and subsequent posterior fixation required from anterior lumbar interbody fusion (ALIF). And unlike posterior lumbar interbody fusion (PLIF), TLIF requires minimal to no retraction on the thecal sac and nerve roots while still providing 360 degrees of support. In addition, because TLIF utilizes a more lateral trajectory, it can be performed in the setting of previous surgery with identifiable landmarks and a cleaner plane of dissection.
Surgical Technique
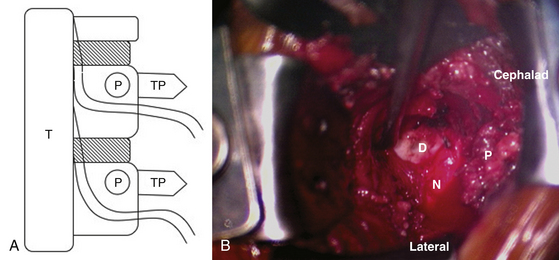
In general, TLIF utilizes an imagined quadrangular space between the transverse processes of the vertebral bodies adjacent to the affected disc space and the traversing nerve root medially (Fig. 170-1). Both open and minimally invasive techniques are utilized. The open technique is described stepwise, followed by modifications for the minimally invasive procedure.
Positioning
A Foley catheter, sequential compression devices, and stockings are placed on the patient. Depending on the surgeon’s experience, autologous blood and a cell saver can be available. The patient is placed in prone position on a radiolucent frame. Use of a Jackson table allows decompression of the abdomen to decrease epidural bleeding. Positioning of the patient is performed to facilitate encouragement of lordosis. Fluoroscopy or plain films are used to localize the affected level.
Minimally Incisional TLIF
Because of its posterolateral approach, TLIF is amenable to minimally incisional techniques. Minimal-access TLIF requires less tissue retraction and avoids the harmful effects of prolonged muscle retraction on truncal strength and postoperative back pain.8,9 There is also less blood loss with the technique.10 Anecdotally, after the initial learning curve, we found the minimally incisional version of this procedure easier and faster to perform, and the large dissection required for the open procedure is skipped.
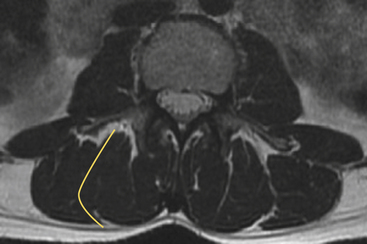
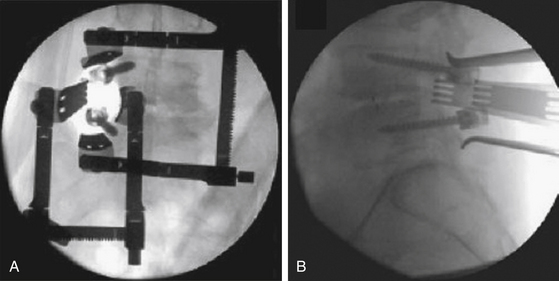
Modifications from the previously described open approach lie mainly in exposure and fixation. The incision is paramedian, approximately 4 to 5 cm off the midline and lateral to the pedicular line. Review of the preoperative magnetic resonance image may reveal an intermuscular septum that may be exploited to expose the facet joint with virtually no muscle dissection. Fluoroscopy is used to center the incision over the disc space to be fused. The incision is carried to the dorsal lumbar fascia. The fascia is opened, and finger dissection is used to identify the facet. Multiple tubular or bladed retractor systems are available to facilitate exposure. Some employ the use of sequential soft-tissue dilators (e.g., METRx, Medtronic Sofamor Danek) to expose the overlying facet complex. With this system, a 20-mm working channel is necessary for placement of an interbody graft.11 The system we advocate takes advantage of the fascial interval between the longissimus and the iliocostalis (erector spinae) muscle bellies at the level of the tips of the transverse processes.7 Blunt dissection is performed in this avascular plane to the facet complex and transverse processes (Fig. 170-2). A ventral cervical retractor system (e.g., Black Belt, T. Koros Surgical Instruments) is utilized to maintain exposure (Fig. 170-3).
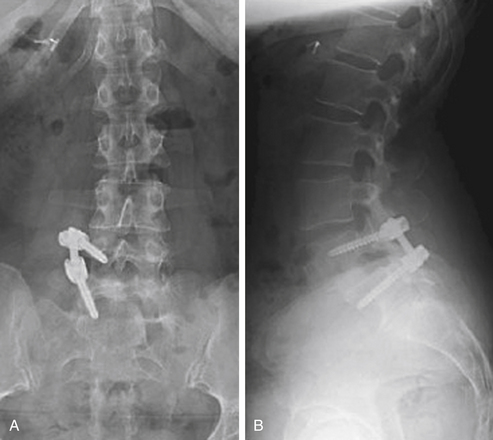
After exposure, the bony decompression, pedicle screw placement, disc preparation, and interbody graft follow in a similar fashion, with the exception that only unilateral pedicle screws are utilized (Fig. 170-4). Because of this, it requires a bit more carpentry of the disc space to get an appropriately sized graft in place. If necessary, contralateral screws may be placed percutaneously and used for interval distraction. However, unilateral pedicle screws are effective for stabilization of the lumbar spine in many patients following TLIF.12–14 Avoiding bilateral exposure limits potential morbidity and preserves the contralateral facet capsule. Unilateral fixation is inappropriate for patients with significant preoperative instability because of increased segmental range of motion.15
Outcomes
While there are only a few long-term studies, TLIF seems durable in mid- to long-term follow-up. One study notes a statistically significant change in the VAS by 2.4 points and a 10.5% drop in the ODI score.16 Durability of fusion at 2 years ranged between 80% and 98%.17,18 The average length of stay for both minimally invasive and open TLIF ranged between 3 and 6 days.17,18 Average blood loss in minimally invasive TLIF was 150 ml compared to 680 ml in the open group.18 Compared to the ALIF procedure, TLIF was just as effective in deformity correction for degenerative lumbar scoliosis.19,20 The most frequent complications noted during TLIF include blood loss requiring transfusion, lumbar wound infection, postoperative radiculitis, cage subsidence or extrusion, and pseudoarthrosis.17,18,21
Chastain C.A., Eck J.C., Hodges S.D., et al. Transforaminal lumbar interbody fusion: a retrospective study of long-term pain relief and fusion outcomes. Orthopedics. 2007;30(5):389-392.
Crandall D.G., Revella J. Transforaminal lumbar interbody fusion versus anterior lumbar interbody fusion as an adjunct to posterior instrumented correction of degenerative lumbar scoliosis: three year clinical and radiographic outcomes. Spine. 2009;15(34(20)):2126-2133.
Deutsch H., Musacchio M.J.Jr. Minimally invasive transforaminal lumbar interbody fusion with unilateral pedicle screw fixation. Neurosurg Focus. 2006;15(20(3)):E10.
Dhall S.S., Wang M.Y., Mummaneni P.V. Clinical and radiographic comparison of mini–open transforaminal lumbar interbody fusion with open transforaminal lumbar interbody fusion in 42 patients with long-term follow-up. J Neurosurg Spine. 2008;9(6):560-565.
Gejo R., Matsui H., Kawaguchi Y., et al. Serial changes in trunk muscle performance after posterior lumbar surgery. Spine. 1999;24(10):1023-1028.
Holly L.T., Schwender J.D., Rouben D.P., Foley K.T. Minimally invasive transforaminal lumbar interbody fusion: indications, technique, and complications. Neurosurg Focus. 2006;20(3):E6.
Isaacs R.E., Podichetty V.K., Santiago P., et al. Minimally invasive microendoscopy-assisted transforaminal lumbar interbody fusion with instrumentation. J Neurosurg Spine. 2005;3(2):98-105.
Jagannathan J., Sansur C.A., Oskouian R.J.Jr., et al. Radiographic restoration of lumbar alignment after transforaminal lumbar interbody fusion. Neurosurgery. 2009;64(5):955-963.
Kabins M.B., Weinstein J.N., Spratt K.F., et al. Isolated L4-L5 fusions using the variable screw placement system: unilateral versus bilateral. J Spinal Disord. 1992;5(1):39-49.
Mayer T.G., Vanharanta H., Gatchel R.J., et al. Comparison of CT scan muscle measurements and isokinetic trunk strength in postoperative patients. Spine. 1989;14(1):33-36.
Moskowitz A. Transforaminal lumbar interbody fusion. Orthop Clin North Am. 2002;33(2):359-366.
Peng C.W., Yue W.M., Poh S.Y., et al. Clinical and radiological outcomes of minimally invasive versus open transforaminal lumbar interbody fusion. Spine. 2009;34(13):1385-1389.
Resnick D.K. Lumbar interbody fusion: current status. Neurosurg Q. 2008;18:77-82.
Resnick D.K., Choudhri T.F., Dailey A.T., et al. American Association of Neurological Surgeons/Congress of Neurological Surgeons. Guidelines for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 7: intractable low-back pain without stenosis or spondylolisthesis. J Neurosurg Spine. 2005;2(6):670-672.
Rihn J.A., Patel R., Makda J., et al. Complications associated with single-level transforaminal lumbar interbody fusion. Spine J. 2009;9(8):623-629.
Rolander S.D. Motion of the lumbar spine with special reference to the stabilizing effect of posterior fusion. An experimental study on autopsy specimens. Acta Orthop Scand Suppl. 1966;90:1-144.
Rosenberg W.S., Mummaneni P.V. Transforaminal lumbar interbody fusion: technique, complications, and early results. Neurosurgery. 2001;48(3):569-574.
Slucky A.V., Brodke D.S., Bachus K.N., et al. Less invasive posterior fixation method following transforaminal lumbar interbody fusion: a biomechanical analysis. Spine J. 2006;6(1):78-85.
Steinmetz M.P., Resnick D.K. Use of a ventral cervical retractor system for minimal access transforaminal lumbar interbody fusion: technical case report. Neurosurgery. 2007;60(2 Suppl 1):175-176. ONSE
Suk K.S., Lee H.M., Kim N.H., Ha J.W. Unilateral versus bilateral pedicle screw fixation in lumbar spinal fusion. Spine. 2000;15(25(14)):1843-1847.
Zdeblick T.A. A prospective, randomized study of lumbar fusion. Preliminary results. Spine. 1993;18(8):983-991.
1. Resnick D.K., Choudhri T.F., Dailey A.T., et al. American Association of Neurological Surgeons/Congress of Neurological Surgeons. Guidelines for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 7: intractable low-back pain without stenosis or spondylolisthesis. J Neurosurg Spine. 2005;2(6):670-672.
2. Resnick D.K. Lumbar interbody fusion: current status. Neurosurg Q. 2008;18:77-82.
3. Rolander S.D. Motion of the lumbar spine with special reference to the stabilizing effect of posterior fusion. An experimental study on autopsy specimens. Acta Orthop Scand Suppl. 1966;90:1-144.
4. Zdeblick T.A. A prospective, randomized study of lumbar fusion. Preliminary results. Spine. 1993;18(8):983-991.
5. Moskowitz A. Transforaminal lumbar interbody fusion. Orthop Clin North Am. 2002;33(2):359-366.
6. Rosenberg W.S., Mummaneni P.V. Transforaminal lumbar interbody fusion: technique, complications, and early results. Neurosurgery. 2001;48(3):569-574.
7. Steinmetz M.P., Resnick D.K. Use of a ventral cervical retractor system for minimal access transforaminal lumbar interbody fusion: technical case report. Neurosurgery. 2007;60(2 Suppl 1):175-176. ONSE
8. Gejo R., Matsui H., Kawaguchi Y., et al. Serial changes in trunk muscle performance after posterior lumbar surgery. Spine. 1999;24(10):1023-1028.
9. Mayer T.G., Vanharanta H., Gatchel R.J., et al. Comparison of CT scan muscle measurements and isokinetic trunk strength in postoperative patients. Spine. 1989;14(1):33-36.
10. Holly L.T., Schwender J.D., Rouben D.P., Foley K.T. Minimally invasive transforaminal lumbar interbody fusion: indications, technique, and complications. Neurosurg Focus. 2006;20(3):E6.
11. Isaacs R.E., Podichetty V.K., Santiago P., et al. Minimally invasive microendoscopy-assisted transforaminal lumbar interbody fusion with instrumentation. J Neurosurg Spine. 2005;3(2):98-105.
12. Deutsch H., Musacchio M.J.Jr. Minimally invasive transforaminal lumbar interbody fusion with unilateral pedicle screw fixation. Neurosurg Focus. 2006;15(20(3)):E10.
13. Kabins M.B., Weinstein J.N., Spratt K.F., et al. Isolated L4-L5 fusions using the variable screw placement system: unilateral versus bilateral. J Spinal Disord. 1992;5(1):39-49.
14. Suk K.S., Lee H.M., Kim N.H., Ha J.W. Unilateral versus bilateral pedicle screw fixation in lumbar spinal fusion. Spine. 2000;15(25(14):1843-1847.
15. Slucky A.V., Brodke D.S., Bachus K.N., et al. Less invasive posterior fixation method following transforaminal lumbar interbody fusion: a biomechanical analysis. Spine J. 2006;6(1):78-85.
16. Chastain C.A., Eck J.C., Hodges S.D., et al. Transforaminal lumbar interbody fusion: a retrospective study of long-term pain relief and fusion outcomes. Orthopedics. 2007;30(5):389-392.
17. Dhall S.S., Wang M.Y., Mummaneni P.V. Clinical and radiographic comparison of mini–open transforaminal lumbar interbody fusion with open transforaminal lumbar interbody fusion in 42 patients with long-term follow-up. J Neurosurg Spine. 2008;9(6):560-565.
18. Peng C.W., Yue W.M., Poh S.Y., et al. Clinical and radiological outcomes of minimally invasive versus open transforaminal lumbar interbody fusion. Spine. 2009;34(13):1385-1389.
19. Crandall D.G., Revella J. Transforaminal lumbar interbody fusion versus anterior lumbar interbody fusion as an adjunct to posterior instrumented correction of degenerative lumbar scoliosis: three year clinical and radiographic outcomes. Spine. 2009;15(34(20):2126-2133.
20. Jagannathan J., Sansur C.A., Oskouian R.J.Jr., et al. Radiographic restoration of lumbar alignment after transforaminal lumbar interbody fusion. Neurosurgery. 2009;64(5):955-963.
21. Rihn J.A., Patel R., Makda J., et al. Complications associated with single-level transforaminal lumbar interbody fusion. Spine J. 2009;9(8):623-629.