Transesophageal echocardiography: Anatomic considerations
Anatomic correlations
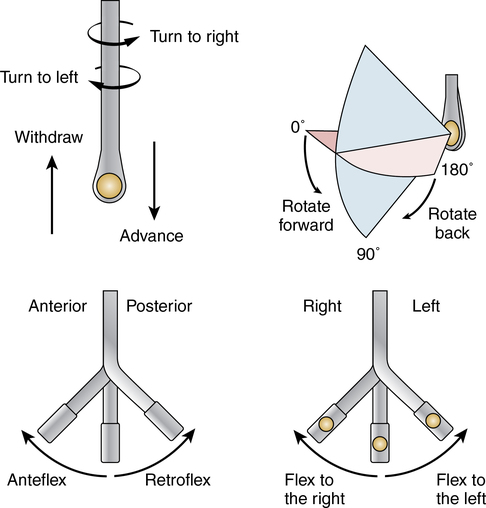
Basic probe movements
To generate desired images, manipulation of the TEE probe is required in addition to changing the multiplane or biplane angle (Figure 53-1). The basic probe movements include insertion or withdrawal of the probe within the esophagus or stomach. Anteflexion and retroflexion of the probe tip are controlled with the large wheel on the probe and result in cephalad or caudad angulation of the imaging plane, respectively. Left-side and right-side flexion can be achieved by manipulating the smaller wheel on the probe and cause deflection of the probe tip within a coronal plane. Rotation of the probe refers to clockwise or counterclockwise spinning of the probe shaft.
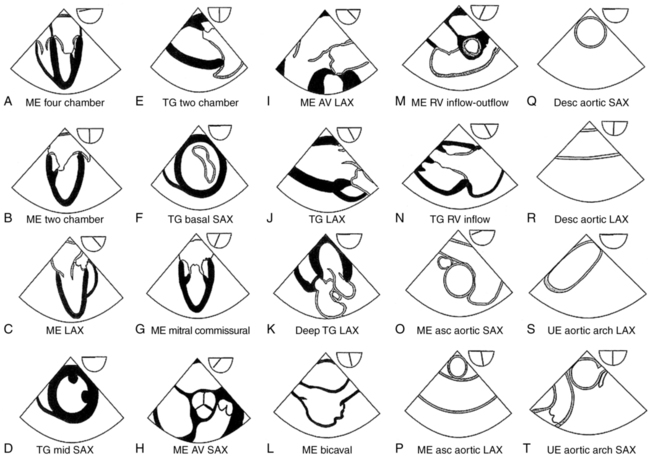
Standard views
The American Society of Echocardiography and Society of Cardiovascular Anesthesiologists consensus task force defined the minimum recommended views that make up the standard intraoperative TEE examination. These standard views have been pictorially displayed, along with the associated icon depicting a typical multiplane angle at which the image may be generated, in Figure 53-2. It is important to remember that additional “off-axis” or nonstandard views may be required to adequately examine specific findings in any given patient. Furthermore, the multiplane angles suggested by the images should be considered a rough guide; the precise multiplane angle at which a given structure is best imaged varies among patients. A complete description of the probe maneuvers necessary to obtain these views is beyond the scope of this chapter. Readers are referred to the task force consensus statement.