Tracheal and tracheostomy tubes and airways
Tracheal tubes
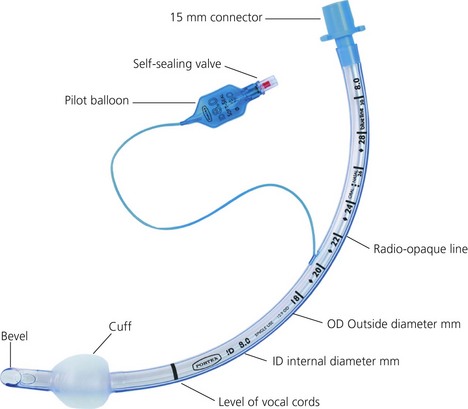
Features of tracheal tubes (Fig. 5.1)
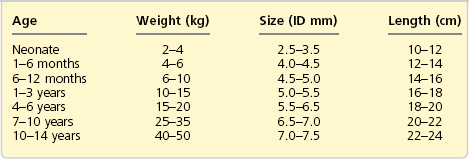
1. The ‘size’ of a tracheal tube refers to its internal diameter which is marked on the outside of the tube in millimetres. Narrower tubes increase the resistance to gas flow, therefore the largest possible internal diameter should be used. This is especially important during spontaneous ventilation where the patient’s own respiratory effort must overcome the tube’s resistance. A size 4-mm tracheal tube has 16 times more resistance to gas flow than a size 8-mm tube. Usually, a size 8.5–9-mm internal diameter tube is selected for an average size adult male and a size 7.5–8-mm internal diameter tube for an average size adult female. Paediatric sizes are determined on the basis of age and weight (Table 5.1). Tracheal tubes have both internal diameter (ID) and outside diameter (OD) markings. There are various methods or formulae used to determine the size of paediatric tracheal tubes. A commonly used formula is:
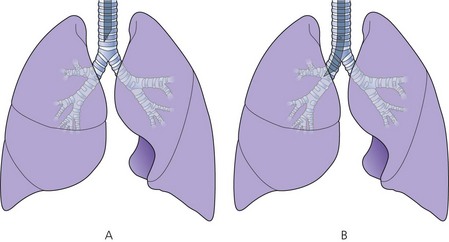
2. The length (taken from the tip of the tube) is marked in centimetres on the outside of the tube. The tube can be cut down to size to suit the individual patient. If the tube is cut too long, there is a significant risk of it advancing into one of the main bronchi (usually the right one, see Fig. 5.2). Black intubation depth markers located 3 cm proximal to the cuff can be seen in some designs (Fig. 5.1). These assist the accurate placement of the tracheal tube tip within the trachea. The vocal cords should be at the black mark in tubes with one mark, or should be between marks if there are two such marks. However, these are only rough estimates and correct tracheal tube position depth should always be confirmed by auscultation.
The bevel
1. The bevel is left-facing and oval in shape in most tube designs. A left-facing bevel improves the view of the vocal cords during intubation.
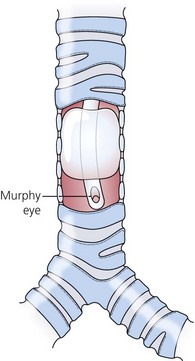
2. Some designs have a side hole just above and opposite the bevel, called a Murphy eye. This enables ventilation to occur should the bevel become occluded by secretions, blood or the wall of the trachea (Fig. 5.3).
The cuff
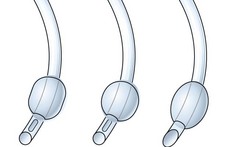
Tracheal (oral or nasal) tubes can be either cuffed or uncuffed. The cuff, when inflated, provides an air-tight seal between the tube and the tracheal wall (Fig. 5.4). This air-tight seal protects the patient’s airway from aspiration and allows efficient ventilation during IPPV.
1. The cuff is connected to its pilot balloon which has a self-sealing valve for injecting air. The pilot balloon also indicates whether the cuff is inflated or not. After intubation, the cuff is inflated until no gas leak can be heard during intermittent positive pressure ventilation (IPPV).
2. The narrowest point in the adult’s airway is the glottis (which is hexagonal). In order to achieve an air-tight seal, cuffed tubes are used in adults.
3. The narrowest point in a child’s airway is the cricoid cartilage. Since this is essentially circular, a correctly sized uncuffed tube will fit well. Because of the narrow upper airway in children, post-extubation subglottic oedema can be a problem. In order to minimize the risk, the presence of a small leak around the tube at an airway pressure of 15 cm H2O is desirable.
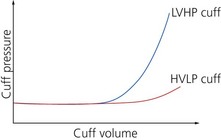
High-pressure/low-volume cuffs
Low-pressure/high-volume cuffs
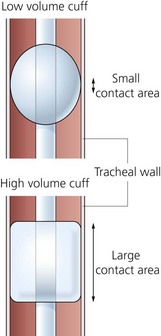
1. These exert minimal pressure on the tracheal wall as the pressure equilibrates over a wider area (Fig. 5.6). This allows the cuff to remain inflated for longer periods.
2. They are less capable of preventing the aspiration of vomitus or secretions. This is due to the possibility of wrinkles forming in the cuff.
The pressure in the cuff should be checked at frequent and regular intervals (Fig. 5.7 and 5.8). The pressure may increase mainly because of diffusion of nitrous oxide into the cuff. Expansion of the air inside the cuff due to the increase in its temperature from room to body temperature and the diffusion of oxygen from the anaesthetic mixture (about 33%) into the air (21%) in the cuff can also lead to increase in the intracuff pressure. An increase in pressure of about 10–12 mmHg is expected after 30 minutes of anaesthesia with 66% nitrous oxide. A more recent design cuff material (Soft Seal, Portex) allows minimum diffusion of nitrous oxide into the cuff with a pressure increase of 1–2 mmHg only. The pressure may decrease because of a leak in the cuff or pilot balloon’s valve.
Route of insertion
1. Tubes can be inserted orally or nasally (Fig. 5.9).
2. The indications for nasal intubation include:
a) surgery where access via the mouth is necessary, e.g. ENT or dental operations
b) long-term ventilated patients on intensive care units. Patients tolerate a nasal tube better, and cannot bite on the tube. However, long-term nasal intubation may cause sinus infection.
3. Nasal intubation is usually avoided, if possible, in children up to the age of 8–11 years. Hypertrophy of the adenoids in this age group increases the risk of profuse bleeding if nasal intubation is performed.
4. Ivory PVC nasotracheal tubes cause less trauma to the nasal mucosa.
Connectors
These connect the tracheal tubes to the breathing system (or catheter mount). There are various designs and modifications (Fig. 5.10). They are made of plastic or metal and should have an adequate internal diameter to reduce the resistance to gas flow.
Specially designed tracheal tubes
This anatomically L-shaped tracheal tube is used in anaesthesia for head and neck surgery because it is non-kinking (Fig. 5.11). The tube can be made of rubber or plastic and can be cuffed or uncuffed. The bevel is oval in shape and faces posteriorly and an introducing stylet is supplied to aid the insertion of the tube. Its thick wall adds to the tube’s external diameter making it wider for a given internal diameter. This is undesirable especially in paediatric anaesthesia.
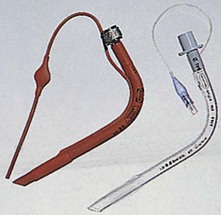
Armoured tracheal tube
Armoured tracheal tubes are made of plastic or silicone rubber (Fig. 5.12). The walls of the armoured tube are thicker than ordinary tracheal tubes because they contain an embedded spiral of metal wire or tough nylon. They are used in anaesthesia for head and neck surgery. The spiral helps to prevent the kinking and occlusion of the tracheal tube when the head and/or neck is rotated or flexed so giving it strength and flexibility at the same time. An introducer stylet is used to aid intubation.
Polar and RAE tracheal tubes
The polar tube is a north- or south-facing preformed nasal cuffed or uncuffed tracheal tube (Fig. 5.13). It is used mainly during anaesthesia for maxillofacial surgery as it does not impede surgical access. Because of its design and shape, it lies over the nose and the forehead. It can be converted to an ordinary tracheal tube by cutting it at the scissors mark just proximal to the pilot tube and reconnecting the 15-mm connector. An oral version of the polar tube exists.
The tube can be temporarily straightened to insert a suction catheter.
Laser resistant tracheal tubes
These tubes are used in anaesthesia for laser surgery on the larynx or trachea (Fig. 5.14). They are designed to withstand the effect of carbon dioxide and potassium-titanyl-phosphate (KTP) laser beams, avoiding the risk of fire or damage to the tracheal tube. One design has a flexible stainless steel body. Reflected beams from the tube are defocused to reduce the accidental laser strikes to healthy tissues (Fig. 5.15). Other designs have a laser resistant metal foil wrapped around the tube for protection. The cuff is filled with methylene blue coloured saline. If the laser manages to damage the cuff, the colouring will help identify rupture and the saline will help prevent an airway fire.
Fig. 5.15 The reflected laser beam is defocused.
Tracheostomy tracheal tubes
These are curved plastic tubes usually inserted through the second, third and fourth tracheal cartilage rings (Fig. 5.18).
Components
1. An introducer used for insertion.
2. Wings attached to the proximal part of the tube to fix it in place with a ribbon or suture. Some designs have an adjustable flange to fit the variable thickness of the subcutaneous tissues (Fig. 5.19).
3. They can be cuffed or uncuffed. The former have a pilot balloon.
4. The proximal end can have a standard 15-mm connector.
5. The tip is usually cut square, rather than bevelled. This is to decrease the risk of obstruction by lying against the tracheal wall.
6. A more recent design with an additional suctioning lumen which opens just above the cuff exists. The cuff shape is designed to allow the secretions above it to be suctioned effectively through the suctioning lumen (Fig. 5.20).
7. Some tubes have an inner cannula. Secretions can collect and dry out on the inner lumen of the tube leading to obstruction. The internal cannula can be replaced instead of changing the complete tube in such cases. The cannula leads to a slight reduction of the internal diameter of the tube.
8. There are different sizes of tracheostomy tubes to fit neonates to adults.
9. Older uncuffed metal tracheostomy tubes made of a non-irritant and bactericidal silver are rarely used in current practice. Some designs have a one-way flap valve and a window at the angle of the tube to allow the patient to speak.
Tracheostomy tubes are used for the following
1. Long-term intermittent positive pressure ventilation.
2. Upper airway obstruction that cannot be bypassed with an oral/nasal tracheal tube.
3. Maintenance of an airway and to protect the lungs in patients with impaired pharyngeal or laryngeal reflexes and after major head and neck surgery (e.g. laryngectomy).
4. Long-term control of excessive bronchial secretions especially in patients with a reduced level of consciousness.
5. To facilitate weaning from a ventilator. This is due to a reduction in the sedation required, as the patients tolerate tracheostomy tubes better than tracheal tubes. Also, there is a reduction in the anatomical dead space.
Problems in practice and safety features
The complications can be divided into:
b) tube misplacement (e.g. into a main bronchus)
c) occlusion of tube by cuff herniation
d) occlusion of the tube tip against carina or tracheal wall
a) blockage of the tube by secretions which can be sudden or gradual; this is rare with adequate humidification and suction
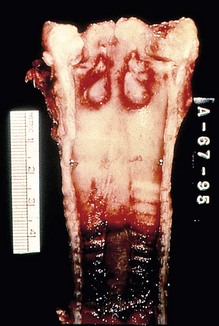
c) overinflation of the cuff leads to ulceration and distension of the trachea
d) mucosal ulceration because of excessive cuff pressures, asymmetrical inflation of the cuff or tube migration.
The fenestrated tracheostomy tube (Fig. 5.21)
1. The fenestration (window) in the greater curvature channels air to the vocal cords allowing the patient to speak.
2. After deflation of the cuff, the patient can breathe around the cuff and through the fenestration as well as through the stoma. This reduces airway resistance and assists in weaning from tracheostomy in spontaneously breathing patients.
Laryngectomy (montandon) tube
This is a cuffed tube inserted through a tracheostomy to facilitate intermittent positive pressure ventilation during neck surgery (Fig. 5.22). It has the advantage of offering better surgical access by allowing the breathing system to be connected well away from the surgical field. Usually, it is replaced with a tracheostomy tube at the end of operation.
Percutaneous tracheostomy tubes
1. If the patient is intubated, the tracheal tube is withdrawn until the tip is just below the vocal cords. Then the cuff is inflated and rested on the vocal cords. A laryngeal mask can be used instead.
2. Through an introducing needle, a Seldinger guidewire is inserted into the trachea. A fibreoptic bronchoscope should be used throughout the procedure. It helps to ensure the initial puncture of the trachea is in the midline and free of the tracheal tube. It can also ensure that the posterior tracheal wall is not damaged during the procedure. Finally, it can assess the position of the tracheostomy tube relative to the carina.
3. A pair of specially designed Griggs forceps are inserted over the guidewire. These forceps are used to dilate the trachea. A tracheostomy tube is threaded over the guidewire and advanced into the trachea. The guidewire is then removed (Fig. 5.25).
4. A series of curved dilators can be used instead of the dilating forceps. The diameter of the stoma is serially increased until the desired diameter is achieved. A single curved dilator of a graduated diameter can be used instead (Fig. 5.26). A tracheostomy tube can then be inserted.
5. An adjustable flange percutaneous tracheostomy is available. The flange can be adjusted to suit the patient’s anatomy, e.g. in the obese patient. The flange can be moved away from the stoma site to aid in cleaning around the stoma.
6. The procedure can be performed in the intensive care unit with a lower incidence of complications than the conventional open surgical method (infection rate, subglottic stenosis and bleeding problems). The operative time is about half that of a formal surgical procedure.
7. Percutaneous tracheostomy can be performed faster using the dilating forceps technique compared to the dilator technique.
8. There is an increased risk of surgical emphysema due to air leaks from the trachea to the surrounding tissues. Loss of the airway, bleeding and incorrect placement of the needle are potential difficulties during the procedure. The risk of aspiration is increased when the tracheal tube has to be withdrawn at the start of the procedure.
9. Relative contraindications include enlarged thyroid gland, non-palpable cricoid cartilage, paediatric application, previous neck surgery and positive end expiratory pressure (PEEP) of more than 15 cm H2O. The latter is because of the difficulty in applying a high PEEP during the process of insertion.
10. Reinsertion of a percutaneously fashioned tube can be more difficult than the surgical one as the stoma may close immediately. A track is formed after long-term intubation and the tracheostomy tube can be removed. In order to protect the patency of the tract, a tracheostomy button is inserted into the stoma. It also acts as a route for tracheal suction. Tracheostomy buttons are made of straight rigid plastic.
Minitracheostomy tube
This tube is inserted percutaneously into the trachea through the avascular cricothyroid membrane (Fig. 5.27).
Components
1. A siliconized PVC tube 10 cm in length with an internal diameter of 4 mm. Some designs have lengths ranging from 3.5 to 7.5 cm with internal diameters from 2 to 6 mm.
2. The proximal end of the tube has a standard 15-mm connector that allows attachment to breathing systems. The proximal end also has wings used to secure the tube with the ribbon supplied.
3. A 2-cm, 16-G needle is used to puncture the cricothyroid cartilage. A 50-cm guidewire is used to help in the tracheal cannulation. A 10-mL syringe is used to aspirate air to confirm the correct placement of the needle.
4. A 7-cm curved dilator and a curved introducer are used to facilitate the insertion of the cricothyrotomy tube in some designs.
Cricothyrotomy tube (Fig. 5.28)

Fig. 5.28 Smith’s Portex cricothyrotomy set.
Mechanism of action
1. After a 2-cm horizontal skin incision has been made, the needle is inserted perpendicular to the skin.
2. As the needle enters the trachea, the red indicator disappears. The needle is advanced carefully until the red reappears, indicating contact with the posterior wall of the trachea.
3. As the cricothyrotomy tube is advanced into the trachea, the needle and the dilator are removed.
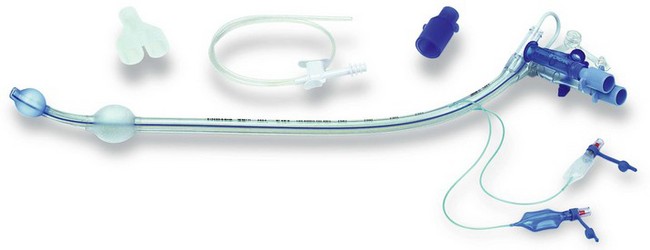
Double lumen endobronchial tubes
Components
1. The Mallinckrodt Bronchocath double lumen tube has two separate colour-coded lumens, each with its own bevel (Fig. 5.29). One lumen ends in the trachea and the other lumen ends in either the left or right main bronchus.
2. Each lumen has its own cuff (tracheal and bronchial cuffs) and colour-coded pilot balloons. Both lumens and pilot balloons are labelled.
3. There are two curves to the tube: the standard anterior curve to fit into the oropharyngeal laryngeal tracheal airway and the second curve, either to the right or left, to fit into the right or left bronchus respectively.
4. The proximal end of these tubes is connected to a Y-shaped catheter mount attached to the breathing system.
Mechanism of action
1. Because of the differing anatomy of the main bronchi and their branches, both right and left versions of any particular double lumen tube must exist.
2. Once the tubes are correctly positioned, the anaesthetist can selectively ventilate one lung. So, for operations requiring that the right lung is deflated, a left-sided double lumen tube would be used that enabled selective ventilation of the left lung alone and vice versa.
3. It is desirable, when possible, to insert a left double lumen tube instead of a right one. This reduces the risk of upper lobe bronchus obstruction by the bronchial cuff in the right-sided version.
4. The right-sided version has an eye in the bronchial cuff to facilitate ventilation of the right upper lobe. The distance between the right upper lobe bronchus and the carina in an adult is only 2.5 cm, so there is a real risk of occluding it with the bronchial cuff. There is no eye in the left-sided version because the distance between the carina and the left upper lobe bronchus is about 5 cm, which is adequate to place the cuff.
5. The tubes come in different sizes to fit adult patients, but not in paediatric sizes.
Tube positioning
1. The position of the tube should be checked by auscultation immediately after intubation and after positioning the patient for the operation. It is also recommended to use a fibreoptic bronchoscope to confirm correct positioning of the double lumen tube.
2. The tracheal cuff is inflated first until no leak is heard. At this point, both lungs can be ventilated. Next, the tracheal limb of the Y-catheter mount is clamped and disconnected from the tracheal lumen tube. Then, the bronchial cuff is inflated with only a few millilitres of air until no leak is heard from the tracheal tube. At this stage, only the lung ventilated via the bronchial lumen should be ventilated. The ability to selectively ventilate the other lung should also be checked by clamping the bronchial limb of the Y-catheter mount and disconnecting it from the bronchial lumen having already reconnected the tracheal lumen. At this stage, only the lung ventilated via the tracheal lumen should be ventilated.
The commonly used double lumen bronchial tubes are:
1. Robertshaw (rubber) tubes (Fig. 5.30).
2. Single-use plastic tubes. These tubes require an introducer for insertion. A more recent version of the single use has the facility of applying continuous positive airway pressure (CPAP) to the deflated lung to improve arterial oxygenation (Fig. 5.31).
3. Carlens (left-sided version) and White (right-sided version) tubes that use a carinal hook to aid final positioning of the tube (Fig. 5.30). The hook can cause trauma to the larynx or carina. Because of the relatively small lumens (6 and 8 mm), the Carlens tube causes an increase in airway resistance and difficulty in suctioning thick secretions.
Endobronchial blocker
The endobronchial blocker is an alternative means to the double lumen tube for providing one-lung ventilation (Fig. 5.32).
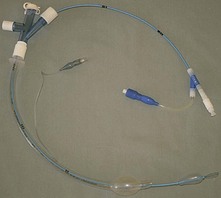
Fig. 5.32 The Arndt endobronchial blocker set.
Oropharyngeal airway
This anatomically shaped airway is inserted through the mouth into the oropharynx above the tongue to maintain the patency of the upper airway (Fig. 5.34) in cases of upper airway obstruction caused by a decreased level of consciousness in a patient. Decreased consciousness can lead to loss of pharyngeal tone that can result in airway obstruction by the tongue, epiglottis, soft palate or pharyngeal tissues. There are various regularly used types of oropharyngeal airway. The most common type is the Guedel airway, named after its developer Arthur Guedel, an American anaesthetist who served in France during the First World War. It is available in up to nine sizes, which have a standardized number coding (the smallest ‘000’ to the largest ‘6’).
Components
1. The curved body of the oropharyngeal airway contains the air channel. It is flattened anteroposteriorly and curved laterally.
2. There is a flange at the oral end to prevent the oropharyngeal airway from falling back into the mouth so avoiding further posterior displacement into the pharynx.
3. The bite portion is straight and fits between the teeth. It is made of hard plastic to prevent occlusion of the air channel should the patient bite the oropharyngeal airway.
Mechanism of action
1. The patient’s airway is kept patent by preventing the tongue and epiglottis from falling backwards.
2. Oropharyngeal airways are designed in different sizes to fit the majority of patients from neonates to adults.
3. The air channel should be as large as possible in order to pass suction catheters.
4. As a good indication, a suitable Guedel airway size can be equivalent to either distance from the patient’s incisors to the angle of the mandible, or corner of the patient’s mouth to the tragus.
5. In adults, the Guedel airway is initially inserted upside down, with the curvature facing caudad. Once partially inserted, it is then rotated through 180° and advanced until the bite block rests between the incisors. This method prevents the tongue being pushed back into the pharynx, causing further obstruction.
6. In children, it is often recommended that the Guedel airway is inserted the right way round, using a tongue depressor or laryngoscope to depress the tongue. This is done to minimize the risk of trauma to the oropharyngeal mucosa. The same technique can also be used in adults.
7. Bermann airway is another type of oropharyngeal airway, designed to assist with oral fibreoptic intubation (Fig. 5.35). It acts to guide the fibreoscope around the back of the tongue to the larynx, with the purpose of both maintaining the patient’s airway and acting as a bite block, thus preventing damage to the fibrescope. Unlike a Guedel airway, it has a side opening which allows it to be removed from the fibrescope, prior to the railroading of the tracheal tube into the trachea.
Problems in practice and safety features
1. Trauma to the different tissues during insertion.
2. Trauma to the teeth, crowns/caps if the patient bites on it.
3. If inserted in a patient whose pharyngeal reflexes are not depressed enough, the gag reflex can be induced that might lead to vomiting and laryngospasm.
4. They confer no protection against aspiration.
5. The degree to which airway patency has been increased after insertion of a Guedel airway should be assessed, not assumed. It should also always be remembered that a badly inserted Guedel airway can make airway patency worse rather than better.
Nasopharyngeal airway
This airway is inserted through the nose into the nasopharynx, bypassing the mouth and the oropharynx. The distal end is just above the epiglottis and below the base of the tongue (Fig. 5.36).
Mechanism of action
1. It is an alternative to the oropharyngeal airway when the mouth cannot be opened or an oral airway does not relieve the obstruction.
2. Nasotracheal suction can be performed using a catheter passed through the nasal airway.
3. It is better tolerated by semi-awake patients than the oral airway.
4. A lubricant is used to help in its insertion.
5. The size inserted can be estimated as size 6 for an average height female and size 7 for an average height male.
6. Once lubricated, it can be inserted through either nares, although the left-facing bevel is designed to ease insertion into the right nostril. On insertion, it should be passed backwards through the nasopharynx, such that its distal end lies beyond the pharyngeal border of the soft palate but not beyond the epiglottis.
Problems in practice and safety features
1. Its use is not recommended when the patient has a bleeding disorder, is on anticoagulants, has nasal deformities or sepsis.
2. Excess force should not be used during insertion as a false passage may be created.
3. An airway that is too large can result in pressure necrosis of the nasal mucosa, while an airway that is too small may be ineffective at relieving airway obstruction.
Supraglottic (or extraglottic) airway devices
These devices provide the following:
1. The ability to be placed without direct visualization of the larynx.
2. Increased speed and ease of placement when compared with tracheal intubation, both by experienced and less experienced operators.
3. Increased cardiovascular stability on insertion and emergence.
4. During emergence, improved oxygen saturation and lower frequency of coughing.
5. Minimal rise in intraocular pressure on insertion.
6. When the device is properly placed, it can act as a conduit for oral tracheal intubation due to the anatomical alignment of its aperture with the glottic opening.
7. In the ‘can’t intubate, can’t ventilate’ scenario, the decision to use such devices should be made early to gain time while attempts are made to secure a definite airway.
8. Such devices normally provide little or no protection against aspiration of refluxed gastric contents, and are therefore contraindicated in patients with full stomachs or prone to reflux. However, second-generation devices (e.g. LMA-ProSeal™, LMA-Supreme™, and i-gel (see later)) offer many improvements such as high cuff seal, second seal, gastric access and drain tube. These allow for rapid drainage of gastric fluids or secretions and reduce the risk of gastric gas insufflation during ventilation. Future indications might even be in emergency medicine, where gastric vacuity is unknown, and in cases of increased risk of regurgitation.
9. Extraglottic airways would normally elicit airway reflexes such as the gag reflex, and therefore require depression of pharyngeal reflexes by general or topical anaesthesia.
10. These devices are increasingly used in a variety of settings, including routine anaesthesia, emergency airway management and as an aid to intubation.
Laryngeal mask
This very useful device is frequently used as an alternative to either the face mask or tracheal tube during anaesthesia (Fig. 5.37).
Components
1. A transparent tube of wide internal diameter. The proximal end is a standard 15-mm connection.
2. An elliptical cuff at the distal end. The cuff resembles a small face mask to form an air-tight seal around the posterior perimeter of the larynx and is inflated via a pilot balloon with a self-sealing valve. A non-metallic self-sealing valve is available for use during magnetic resonance imaging (MRI) scans.
3. The original design (Intavent Classic LMA™) had two slits or bars at the junction between the tube and the cuff to prevent the epiglottis from obstructing the lumen of the laryngeal mask. Newer designs, such as Portex SoftSeal™ and Intersurgical Solus™, omit the bars with no adverse clinical effects.
4. A modified design (LMA-ProSeal™) has an additional lumen (drain tube) lateral to the airway tube and traverses the floor of the mask to open in the mask tip opposite the upper oesophageal sphincter allowing blind passage of an orogastric tube and helps in the drainage of gastric air or secretions. Both tubes are contained within an integrated bite block. The cuff inflates in a three-dimensional manner with the elliptical cuff augmented by a second cuff behind the bowl, known as the rear boot or dorsal cuff. This design improves the seal pressure. A single-use version, LMA Supreme™, is available which combines the best features of previous LMA versions, and contains an elliptical and anatomically shaped curve, which facilitates insertion success and provides a double seal. A first seal is important for adequacy of gas exchange, better known as the oropharyngeal seal (Fig. 5.38). It also incorporates a second seal, designed to reduce the risk of stomach insufflation during ventilation, to provide a passive conduit for (unexpected) regurgitation or active suctioning of gastric content and enhances the effectiveness of the first seal.

Fig. 5.38 LMA-Supreme™. Note the drainage lumen.
5. Low-cost disposable laryngeal masks have been introduced and are widely used (Fig. 5.39).
Mechanism of action
1. A variety of techniques have been described for the insertion of the laryngeal mask. It should provide an adequate seal for spontaneous and mechanical ventilation with a minimal leak, at a pressure of 20–25-cm H2O. A seal pressure of up to 35 cm H2O can be achieved with the LMA-Proseal™.
2. The cuff is deflated and lubricated before use. It is inserted through the mouth. The cuff lies over the larynx.
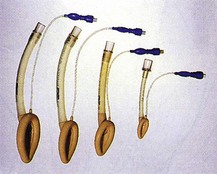
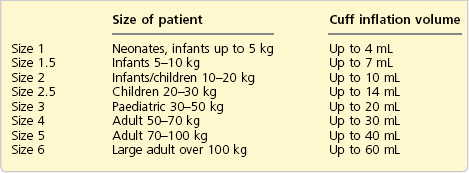
3. Once the cuff is in position, it is inflated (Table 5.2).
4. Partial inflation of the cuff before insertion is used by some anaesthetists.
5. The laryngeal masks have wide internal diameters in order to reduce the flow resistance to a minimum (e.g. the internal diameters of sizes 2, 3, 4 and 5 are 7, 10, 10 and 11.5 mm respectively). This makes them suitable for long procedures using a spontaneous ventilation technique.
6. It also has a role as an aid in difficult intubation. Once in position, it can be used to introduce a bougie or a narrow lumen tracheal tube into the trachea. Alternatively, the laryngeal mask may be used to guide passage of a fibreoptic bronchoscope into the trachea, thus allowing intubation of the trachea.
The reinforced version of the laryngeal mask is used for head and neck surgery (Fig. 5.40).
1. The tubes, although flexible, are kink and crush resistant, because of a stainless steel wire spiral in their wall. The tube can be moved during surgery without loss of the cuff’s seal against the larynx. The breathing system can easily be connected at any angle from the mouth.
2. A throat pack can be used with the reinforced version.
3. The reinforced laryngeal masks have smaller internal diameters and longer lengths than the standard versions, causing an increase in flow resistance. This makes their use with spontaneous ventilation for prolonged periods less suitable.
The intubating laryngeal mask airway (ILMA™)
This is a modification of the laryngeal mask designed to facilitate tracheal intubation with a tracheal tube either blindly or in conjunction with a fibrescope while minimizing the requirements for head and neck manipulation. The specially designed laryngeal mask is inserted first (Fig. 5.41). A specially designed tracheal tube is then passed through the laryngeal mask through the vocal cords into the trachea (Fig. 5.42). Single-use ILMA™ is available (Fig. 5.43).

Fig. 5.41 The intubating LMA.

Fig. 5.42 The intubating LMA.
Problems in practice and safety features
1. The laryngeal mask does not protect against the aspiration of gastric contents.
2. Despite the presence of the slits or bars, about 10% of patients develop airway obstruction because of down-folding of the epiglottis. Although clinically often insignificant, a higher proportion of obstructions by the epiglottis can be observed endoscopically.
3. The manufacturers recommend using the laryngeal masks for a maximum of 40 times. The cuff is likely to perish after autoclaving. A record card that accompanies the laryngeal mask registers the number of autoclaving episodes.
4. Unlike the tracheal tube, rotation of the laryngeal mask may result in complete airway obstruction. In order to assess the laryngeal mask’s orientation when inserted, a black line is present on the tube. This should face the upper lip of the patient when the laryngeal mask is in position.
5. Cricoid pressure may prevent correct placement of the laryngeal mask.
6. A common cause of airway obstruction during laryngeal mask anaesthesia is down-folding of the epiglottis, which occurs in 20–56% of patients.
I-gel airway
The i-gel airway is a single-use extraglottic airway that uses an anatomically designed mask to fit the perilaryngeal and hypopharyngeal structures without the use of an inflatable cuff (Fig. 5.44). It also incorporates a second drain tube.
Components
1. The large lumen is for ventilation with a proximal 15-mm connector. Distally, it ends in a non-inflatable gel-like cuff with a ridge at the superior anterior edge.
2. Two separate ventilation and gastric channels or lumens. The distal end of the integrated gastric lumen is positioned in the upper oesophagus.
Mechanism of action
1. The soft, gel-like plastic from which the i-gel is manufactured is intended to mould into place without the use of an inflatable cuff.
2. The gastric channel allows direct suctioning or passage of a gastric tube.
3. The wide oval-in-cross-section body is designed to prevent rotation and to act as an integral bite block.
4. The epiglottic blocking ridge is intended to reduce the possibility of epiglottic down-folding.
5. It is available in adult, paediatric and neonatal sizes (1, 1.5, 2, 2.5, 3, 4, and 5).
6. It is intended for use with fasted patients, with both spontaneous and controlled ventilation, and can be used as a conduit for tracheal intubation.
COBRA perilaryngeal airway (PLA™)
It is available in eight sizes. Paediatric models have a distal gas sampling port in the COBRA head, which minimizes sampling dead space increasing the accuracy of capnometry. COBRA Plus models include a temperature probe on the lateral posterior part of the cuff for core temperature monitoring (Fig. 5.45).
Brimacombe J. Laryngeal mask anesthesia: principles and practice, second ed. Philadelphia: WB Saunders; 2004.
Gothard J.W.W. Anaesthetic equipment for thoracic surgery. Anaesthesia and Intensive Care Medicine. 2005;6(12):425–427.
MHRA. Medical device alert: endotracheal (ET) tubes, adult and paediatric sizes manufactured by Unomedical (a ConvaTec company) (MDA/2011/025). Online. Available at http://www.mhra.gov.uk/Publications/Safetywarnings/MedicalDeviceAlerts/CON111625?tabName=Device, 2011.
In the following lists, which of the statements (a) to (e) are true?
a) The RAE tracheal tube is ideal for microlaryngeal surgery.
b) Preformed tracheal tubes have a higher risk of bronchial intubation.
c) Laryngeal masks can be used in nasal surgery.
d) RAE tubes stand for reinforced anaesthetic endotracheal tubes.
a) They can prevent aspiration of gastric contents.
b) The bars at the junction of the cuff and the tube prevent foreign bodies from entering the trachea.
c) Because of its large internal diameter, it can be used in spontaneously breathing patients for long periods of time.
d) It can be autoclaved and used repeatedly for an unlimited number of times.
3. Double lumen endobronchial tubes:
a) Robertshaw double lumen tubes have carinal hooks.
b) The left-sided tubes have an eye in the bronchial cuff to facilitate ventilation of the left upper lobe.
c) Carlens double lumen tubes have relatively small lumens.
d) CPAP can be applied to the deflated lung to improve oxygenation.
e) Fibreoptic bronchoscopy can be used to ensure correct positioning of the tube.
4. Concerning the tracheal tube cuff during anaesthesia:
a) Low-pressure/high-volume cuffs prevent aspiration of gastric contents.
b) The intracuff pressure can rise significantly because of the diffusion of the anaesthetic inhalational vapour.
c) High-pressure/low-volume cuffs may cause necrosis of the tracheal mucosa if left in position for long periods.
d) Low-volume cuffs have a smaller contact area with the tracheal wall than high-volume cuffs.
e) The pressure in the cuff may decrease because of the diffusion of nitrous oxide.
a) False. An RAE tube is a normal size preformed tracheal tube. It does not allow good visibility of the larynx because of its large diameter. A microlaryngeal tracheal tube of 5–6 mm ID is more suitable for microlaryngeal surgery, allowing good visibility and access to the larynx.
b) True. Because the shape of these tubes is fixed, they might not fit all patients of different sizes and shapes; e.g. a small, short-necked patient having an RAE tube inserted is at risk of an endobronchial tube position.
c) True. Some anaesthetists use the laryngeal mask in nasal surgery with a throat pack. This technique has a higher risk of aspiration.
d) False. RAE stands for the initials of the designers (Ring, Adair and Elwyn).
e) False. The Oxford tube is one of the few tracheal tubes with a front-facing bevel. This might make intubation more difficult as it obscures the larynx.
a) False. Laryngeal masks do not protect the airway from the risks of aspiration.
b) False. The bars in the cuff are designed to prevent the epiglottis from blocking the lumen of the tube.
c) True. The laryngeal mask has a large internal diameter, in comparison with a tracheal tube. This reduces the resistance to breathing which is of more importance during spontaneous breathing. This makes the laryngeal mask more suitable for use in spontaneously breathing patients for long periods of time.
d) False. The laryngeal mask can be autoclaved up to 40 times. The cuff is likely to perish after repeated autoclaving. A record should be kept of the number of autoclaves.
e) False. The standard laryngeal mask has a metal component in the one-way inflating valve. This makes it unsuitable for use in MRI. A specially designed laryngeal mask with no metal parts is available for MRI use.
3. Double lumen endobronchial tubes:
a) False. The Robertshaw double lumen tube does not have a carinal hook. The Carlens double lumen tube has a carinal hook.
b) False. Left-sided tubes do not have an eye in the bronchial cuff to facilitate ventilation of the left upper lobe. This is because the distance between the carina and the upper lobe bronchus is about 5 cm, which is enough for the bronchial cuff. Right-sided tubes have an eye to facilitate ventilation of the right upper lobe because the distance between the carina and the upper lobe bronchus is only 2.5 cm.
c) True. Carlens double lumen tubes have relatively small lumens in comparison to the Robertshaw double lumen tube.
d) True. CPAP can be applied to the deflated lung to improve oxygenation during one lung anaesthesia.
e) True. It is sometimes difficult to ensure correct positioning of the double lumen endobronchial tube. By using a fibreoptic bronchoscope, the position of the tube can be adjusted to ensure correct positioning.
4. Concerning the tracheal tube cuff during anaesthesia:
a) False. The design of the low-pressure/high-volume cuff allows wrinkles to be formed around the tracheal wall. The presence of the wrinkles allows aspiration of gastric contents to occur.
b) False. The rise in the intracuff pressure is mainly due to the diffusion of N2O. Minimal changes are due to diffusion of oxygen (from 21% to say 33%) and because of increase in the temperature of the air in the cuff (from 21° to 37°C). The diffusion of inhalational agents causes minimal changes in pressure due to the low concentrations used (1–2%). New design material cuffs prevent the diffusion of gases thus preventing significant changes in pressure.
c) True. The high pressures achieved by the high-pressure/low-volume cuffs, especially during nitrous oxide anaesthesia, can cause necrosis to the mucosa of the trachea if left in position for a long period.
d) True. Because of the design of the low-volume cuffs, a seal can be maintained against a relatively small area of the tracheal wall. In the case of the high-volume/low-pressure cuffs, a large contact area on the tracheal wall is achieved.
e) False. The pressure in the cuff may decrease because of a leak in the cuff or pilot balloon’s valve.
a) False. The ID is measured in millimetres.
c) False. An armoured tube should not be cut, as that will cut the spiral present in its wall. This increases the risk of tube kinking.
d) False. A Murphy eye allows pulmonary ventilation in the situation where the bevel of the tube is occluded.
e) False. The bevel of the tube is usually left-facing to allow easier visualization of the vocal cords. The tracheostomy tube has a square-cut tip.