Chapter 23 Total Spondylectomy for Subaxial Cervical Spine Tumors
INTRODUCTION
Subaxial cervical tumors are relatively uncommon compared with those involving the thoracic and lumbar regions, and represent less than 10% of spinal metastases.1 The surgical treatment of these tumors is often complicated by functional nerve root and brachial plexus involvement, vertebral artery (VA) encasement, and the need for multilevel reconstruction after anterior-posterior decompression.
PREOPERATIVE ASSESSMENT
RADIOLOGICAL ASSESSMENT
NEUROLOGICAL ASSESSMENT
POSTERIOR APPROACH (FOR C5–7 LESIONS)2
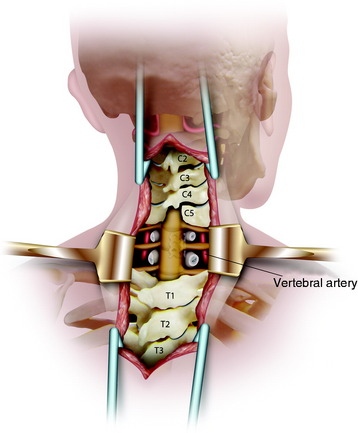
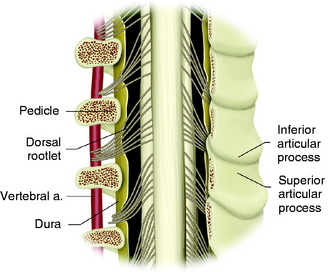
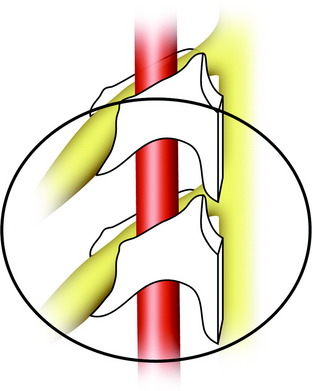
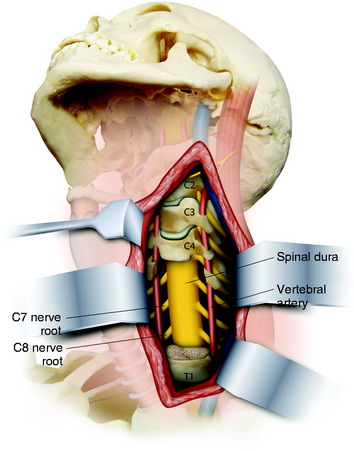
The patient is placed in a prone position with skeletal fixation. A midline skin incision is made from C2 to T4 and a paraspinal muscle dissection is performed (Fig. 23-1). Wide exposure is necessary to access the lateral margin of the facet joints. Total laminectomies are performed from C5 to C7, and bilateral facetectomies are completed at C4–5, C5–6, and C6–7. The facet removal is made from the spinal canal side to the lateral side. After the facet removal, the C5, C6, and C7 nerve roots are seen and the VA posterior surface is exposed (Fig. 23-2). The posterior bony capsules of the VA are continued through the pedicle to the VB. They are removed with a punch, and the pedicles are drilled away to the VB so that the partial removal of the VB can be attempted via the transpedicular route. When transpedicular VB removal is attempted, the upper roots are retracted to the cephalad direction and the VA is retracted to the lateral side.3 This maneuver provides a wider operative field to the VB.
ANTERIOR APPROACH (C5–7 COMPLETE VERTEBRECTOMY)
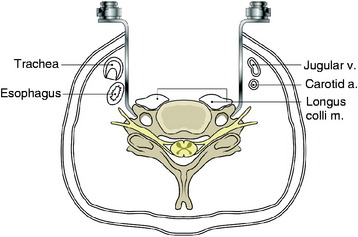
The retractors should be located beside the transverse process along the lateral side of the longus colli muscle (Fig. 23-3). The cephalad retractor is positioned on the C4 transverse process, and the caudal retractor is on the T1 transverse process. In the middle of the field, the self-retractor is laid over the muscles.
The longus colli muscle should not be dissected on the VB surface. The longus colli muscles are sectioned over the entire width at the C4–5 intervertebral disc level and the C7–T1 intervertebral disc level (Fig. 23-4). The resected segments are swept away from the VB surface. When the muscles are removed at the C7 VB level, the VA is located anterior to the transverse process of C7 and enters the C6 vertebral foramen. Great care should be taken to prevent injury to the VA.
CORPECTOMY
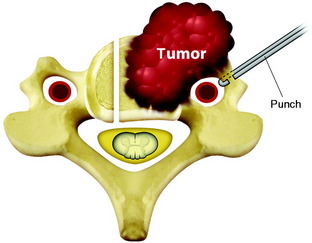
The uncinate processes are identified and used as reference points for establishing the width of the corpectomy required (Fig. 23-5).4 Posterior cortical bone and osteophytes are removed microsurgically with the aid of the microscope. Decompression is considered to be successful when the surgeon can directly visualize a protruding, pulsating dural sac.
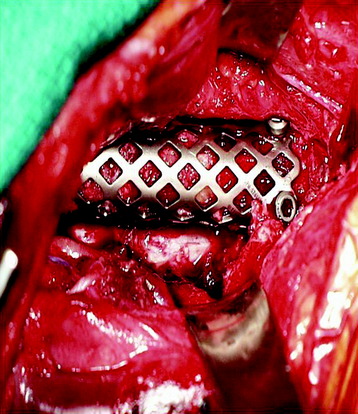
ANTERIOR RECONSTRUCTION
After the primary tumor is removed, reconstruction is done with a Harm’s cage packed with iliac crest graft (Fig. 23-6). This cage can be cut with flanges that extend over the adjacent VBs and secured with cancellous screws. When this type of non-constrained screw is used, it should be augmented with posterior fixation. In other cases, allograft and plating may be used. Supplementary posterior stabilization is indicated for corpectomies that involve more than two levels. It is helpful even after single-level VB resection in cases of the progression of the remaining tumor.
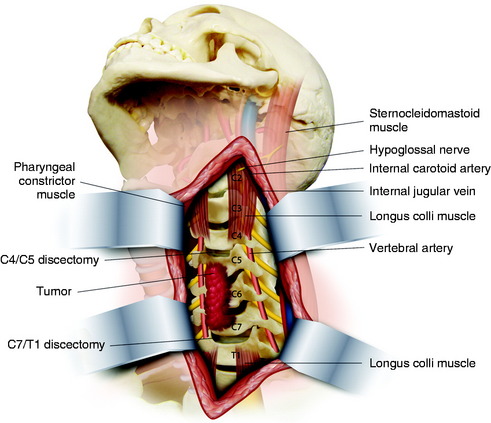
MARGINAL EXCISION OF LOWER CERVICAL (C5) TUMOR WITH UNILATERAL VERTEBRAL ARTERY LIGATION
The usual anterior approach is done medial to the carotid sheath to expose the VBs from C3 to T1.5 The left transverse processes of C4 to C6 are exposed cephalocaudally by retracting the carotid sheath and the sternocleidomastoid muscle. The tumor mass, covered with longus capitis muscle and a pseudocapsule, is exposed. A preoperative occlusion test of the left VA showed that this vessel could be ligated safely. The artery is ligated at C6–7 proximally and C3–4 distally (Fig. 23-7).
The right lateral margin for resection is determined with a tumor margin, and a trough is made in the C5 VB with a cutting diamond burr. Complete discectomy for C4–5 and C5–6 is done with a PLL resection. After the left margin of the tumor mass is dissected, the anterior wall of the transverse foramen is unroofed with the punch (Fig. 23-8). Although the anterior wall is open, perivascular venous bleeding is not significant as a result of the VA ligation. With a lateral transposition of the VA, the pedicle is resected with the punch. When the pedicle is removed, the nerve root and lateral dural margin are exposed.
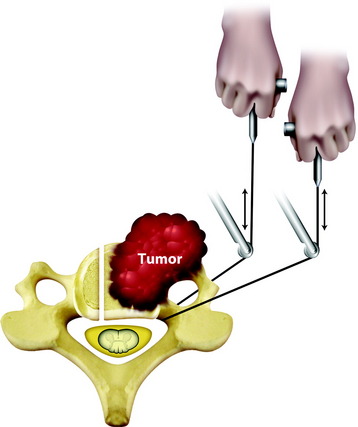
Fig. 23-8 Tumor removal with a threadwire saw. The saw should be slanted toward the lateral direction.
Modified from Fukita T, Kawahara N, Matsumoto T, et al. Chordoma in the cervical spine managed with en bloc excision. Spine 1999;24:1848–1851.
If small pieces of tumor mass remain on the epidural space, they are removed in a piecemeal fashion. Although the surgical margin in this procedure is intralesional in a small area, the recurrence rate will be reduced more than if a curettage operation was performed.5
NEURAL COMPLICATION AFTER SUBAXIAL CERVICAL SPINE OPERATION
CASE ILLUSTRATION
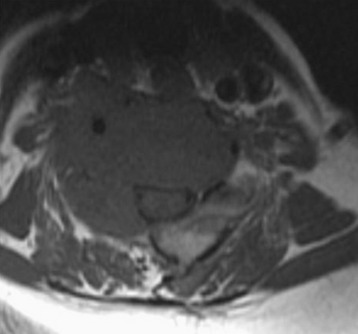
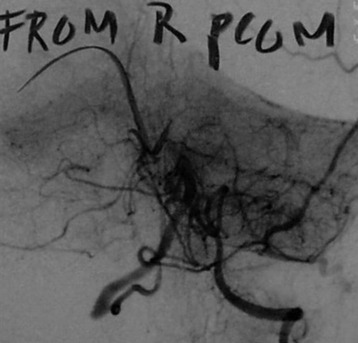
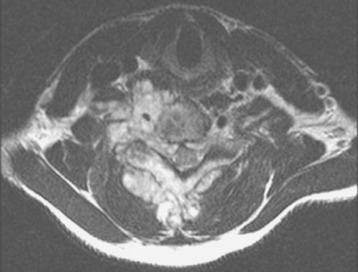
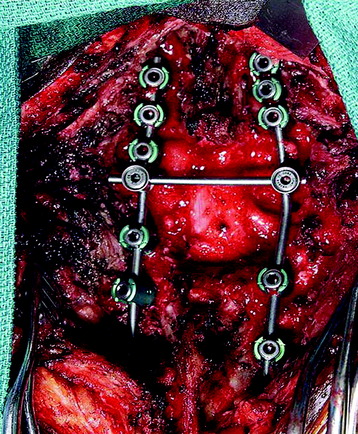
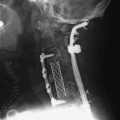
This patient is a 76-year-old woman who was diagnosed with a chondroblastoma. MRI demonstrated a C4–7 VB tumor extending to the right facet joint (Figs. 23-9 and 23-10). The right VA, which appeared dominant, was encased in tumor and the left VA was abutted. Preoperatively, a balloon occlusion test was performed. It showed that the distal segment of the right VA was filled from the right posterior communicating artery (Fig. 23-11). The operative approach was done first with anterior side. The paraspinal mass was initially removed lateral to the carotid artery sheath and brachial plexus. The VA was dissected from the paraspinal mass for the length of involvement (Fig. 23-12). The VA was readily dissected from the periphery of the paraspinal mass using tenotomy scissors for intralesional dissection. The periosteum of the VA is typically intact and serves as a barrier to tumor penetration. The disc spaces were removed to the PLL and the tumor mass, replacing the VBs, was then removed. The PLL was stripped from the dura, and the nerve roots were laterally dissected. After vertebrectomy, reconstruction was performed anteriorly with a Harm’s cage cut with flanges and secured to the VB (Fig. 23-13). Anterior screws were fixed to the flattened portion of the cage. No additional plate was used (Fig. 23-14). Posterior decompression with multilevel facetectomy was performed, and a screw/rod construct was placed (see Fig. 23-14).
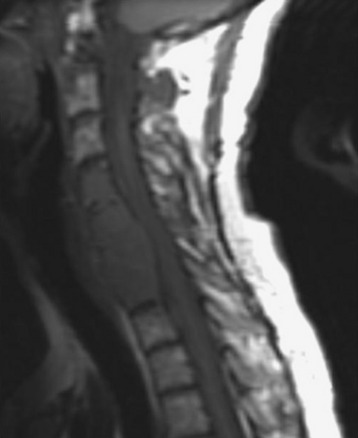
Fig. 23-9 T1-weighted sagittal MRI. Low signal mass involving C4–7 VB is seen to compress the spinal cord.
This is a 22-year-old patient who previously had undergone excision of a left chest wall mass consistent with a high-grade malignant peripheral nerve sheath tumor (PNST). The lesion recurred 2 years later with neck pain and right bicep weakness. MRI showed C6 VB destruction with enhancement. Subsequent spread to the epidural space was seen at C5–7 levels with cord compression. The mass infiltrated into the neural foramen of C6–7, right C6, C7 laminae, and right C6–7 facet joint (Figs. 23-15 and 23-16). The encased right VA appeared hypoplastic, and, on a balloon occlusion test, showed retrograde filling from the left VA. Via posterior approach first, total laminectomies of C6 and C7 were performed with total facetectomy of C6–7. After decompression, the C6 nerve root is seen (Fig. 23-17). Posterior instrumentation was performed with a screw/rod system from C3 to T2. Then an anterior approach was performed with a C6 corpectomy. After corpectomy, the ventral dura was visualized. The allograft bone grafting was done and the plate was applied (Figs. 23-18 and 23-19).