CHAPTER 35 Total Hip Arthroplasty in the Young Active Patient With Arthritis
Introduction
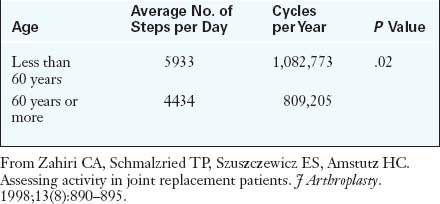
Although indicating a young patient for THA is always disheartening, the good news is that patients can usually expect excellent pain relief and a high level of performance in a reproducible and predictable manner. Long-term results are tempered by wear-induced failures, which are a function of the increased number of loading cycles as a result of increased activity levels (Table 35-1) and increased life expectancies (Table 35-2). This data shows that there is a higher risk of failure in a younger patient during the subsequent 15 years after THA.
Table 35–2 15-Year Survival of Patients with Total Hip Arthroplasties
| Age at Surgery | Percentage of Patients Still Alive | Percentage of Arthroplasties Still in Place |
|---|---|---|
| 45 years | 96% | 77% |
| 65 years | 72% | 92% |
From Berry DJ, Harmsen WS, Cabanela ME, Morrey BF. Twenty-five-year survivorship of two thousand consecutive primary Charnley total hip replacements: factors affecting survivorship of acetabular and femoral components. J Bone Joint Surg Am. 2002;84-A:171–177.
This chapter will discuss the inherent challenges involved when performing a THA in a young patient.
Imaging and diagnostic studies
We prefer to routinely obtain five radiographs for preoperative evaluation:
Anesthesia and surgical technique
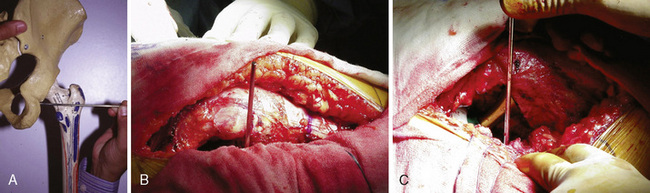
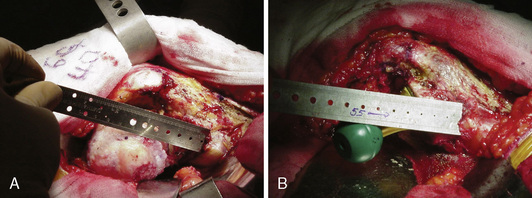
For the assessment of limb-length discrepancy, we prefer the method described by Ranawat and colleagues. This technique involves the use of the posterior approach. After the initial dissection and release of the short external rotators, the inferior capsule is incised at the 6-o’clock position to expose the posteroinferior lip of the acetabulum. A  -inch Steinmann pin is inserted into the posterior infracotyloid groove (Figure 35-1, A through C); this represents the bony groove inferior to the posteroinferior lip of the acetabulum. The pin is placed initially at an angle of approximately 60 degrees until it touches the ischium, and it is then made vertical and allowed to slide along the bone into the infracotyloid groove. The pin is kept vertical and viewed end-on from above, and then a mark is made on the greater trochanter before hip dislocation (see Figure 35-1, B). The hip is then dislocated. The center of the femoral head is marked with electrocautery, and the distance between the center and the lesser trochanter is noted and compared with the calculation made during the preoperative planning (Figure 35-2, A). The neck resection is now completed in accordance with preoperative templating.
-inch Steinmann pin is inserted into the posterior infracotyloid groove (Figure 35-1, A through C); this represents the bony groove inferior to the posteroinferior lip of the acetabulum. The pin is placed initially at an angle of approximately 60 degrees until it touches the ischium, and it is then made vertical and allowed to slide along the bone into the infracotyloid groove. The pin is kept vertical and viewed end-on from above, and then a mark is made on the greater trochanter before hip dislocation (see Figure 35-1, B). The hip is then dislocated. The center of the femoral head is marked with electrocautery, and the distance between the center and the lesser trochanter is noted and compared with the calculation made during the preoperative planning (Figure 35-2, A). The neck resection is now completed in accordance with preoperative templating.
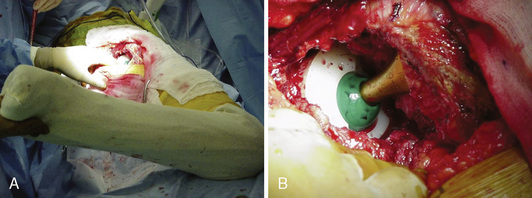
After bone preparation and the placement of the trial implants, the offset and the distance from the center of the head to the lesser trochanter are assessed (see Figure 35-2, B). After reduction, the component position is assessed with the use of the combined anteversion test (Figure 35-3, A and B). This test measures the angle of internal rotation required for the femoral head to be coplanar with the face of the acetabulum with 10 degrees of flexion and 10 degrees of adduction. Normally, the angle is between 35 degrees and 45 degrees of internal rotation for women and between 25 degrees and 35 degrees for men.
It should be emphasized that all of these soft-tissue tension tests are subjective and depend on the muscle relaxation at that point in the operation, the amount of effective force applied to distract the joint, the muscularity and habitus of the patient, and the extent of soft-tissue release that occurred during surgery. Moreover, because these tests provide an assessment of stability, they may sometimes encourage increased neck lengths, which leads to potential limb lengthening. Thus, these tests should be used in conjunction with each other along with the preoperative template to determine the appropriate construct. After an adequate soft-tissue balance is achieved around the hip, the Steinmann pin is reinserted, with the pin and the patient’s leg kept in the same position (see Figure 35-1, C). The difference in the leg length is measured by noting whether the point on the trochanter has moved up or down, which is indicative of shortening or lengthening, respectively. If lengthening of the limb (especially of more than 2 cm) is anticipated, the sciatic nerve must be palpated to determine whether it is excessively taut before the length that has been gained is accepted.
Technical Pearls
Pain management and rehabilitation
A local periarticular injection has been shown to have a significant effect on the reduction of immediate postoperative pain. We perform two such injections: 1) one before the final reduction in the anterior capsule, the iliopsoas tendon, and the insertion site; and 2) one after the final reduction in the abductors, the fascia lata, the gluteus maximus and its insertion, the posterior capsule, the short external rotators, and the synovium (Table 35-3).
| Medication | Strength/Dose | Amount |
|---|---|---|
| First Injection | ||
| Bupivacaine | 0.5% (200 mg to 400 mg) | 24 ml |
| Morphine sulfate | 8 mg | 0.8 ml |
| Epinephrine (1:1000) | 300 μg | 0.3 ml |
| Methylprednisolone acetate | 40 mg | 1 ml |
| Cefuroxime | 750 mg | 10 ml (reconstituted in normal saline) |
| Sodium chloride | 0.9% | 22 ml |
| Second Injection | ||
| Bupivacaine | 0.5% | 20 ml |
| Sodium chloride | 0.9% | 20 ml |
A clonidine transdermal patch is applied in the operating department (100 μg/24 hours). No steroid is given to diabetic, immunocompromised, elderly, or revision patients. Vancomycin is used if the patient is allergic to penicillin.
From Parvataneni HK, Ranawat AS, Ranawat CS. The use of local periarticular injections in the management of postoperative pain after total hip and knee replacement: a multimodal approach. Instr Course Lect. 2007;56:125–131.
Sports and total hip arthroplasty
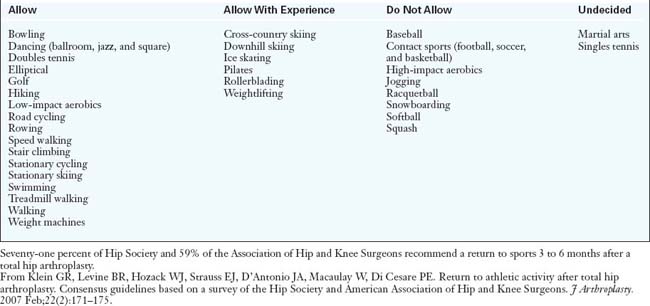
Generally, high-contact, high-impact activities are discouraged after THA. Current recommendations are shown in Table 35-4. Improving function is an increasing indication for THA, and we believe that athletic activity is important to many of our patients. We prefer to educate our patients regarding the risks associated with athletic activity rather than to directly discourage the practice. Some patients accept this risk, whereas others choose to avoid sports.
Results and outcomes
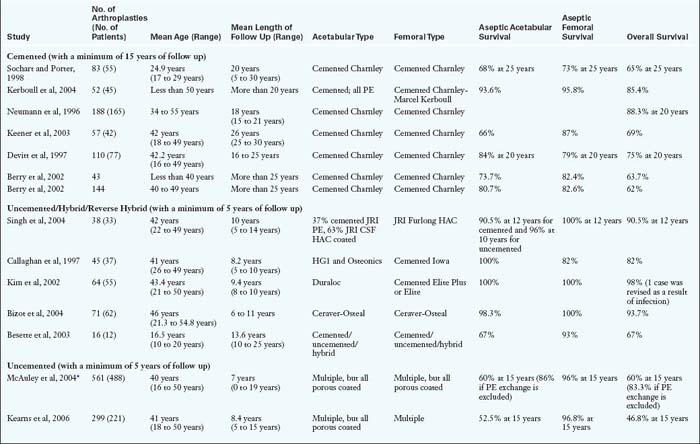
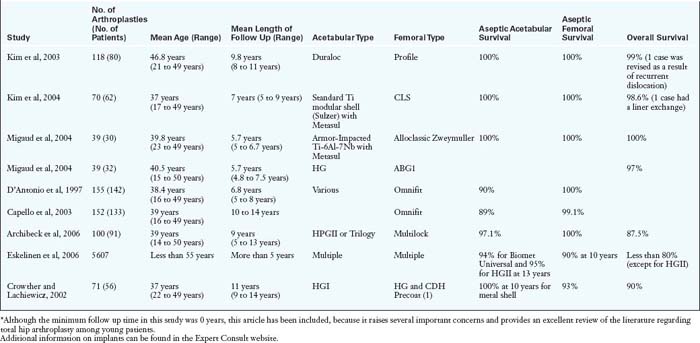
The results of THA in the young patient require careful evaluation. The factors to be considered are the length of follow up, the definition of failure (e.g., any revision, aseptic loosening, septic revision, radiographic loosening), the method of obtaining fixation, the underlying diagnosis, and the bearing surface. Diagnosis (e.g., osteoarthritis as compared with rheumatoid arthritis, avascular necrosis as compared with osteoarthritis), male sex, accelerated wear, and varus position of the femur have been linked to the decreased survival of the prosthesis. According to the National Institute for Health and Clinical Excellence, with the use of the most recently available evidence of clinical effectiveness, the best prosthesis (when considering long-term viability as the determinant) should demonstrate a survival rate of more than 90% at 10 years. Although there are not many studies among young patients that fulfill the National Institute for Health and Clinical Excellence criteria, certain trends are evident (Table 35-5).
The results of non-cemented THA will always lag behind those of cemented THA in terms of follow up duration for historic reasons. The long-term results of cemented THA and the mid- to long-term results of uncemented fixation are shown in Table 35-5. Early reports of disappointing clinical results of cemented THA in young patients caused concern and prompted some authors to recommend alternative procedures. Dorr and colleagues found revision rates of 12% at 4.5 years, 33% at 9.2 years, and 67% at 16.2 years. However, recent reports have been more encouraging, with long-term survival rates of 65% to 88% (see Table 35-5). Better survival outcomes have been reported for the femoral stem as compared with the acetabular cup.
Uncemented fixation is growing in popularity, especially for younger patients in most parts of the world. Modern uncemented stems have also shown a good survival rate of 90% to 100% at 10 to 15 years (see Table 35-5). However, the weak link with either type of fixation is the acetabular side: aseptic loosening with cemented components and wear and osteolysis with uncemented modular components. In a study of uncemented THA by McAuley and colleagues, the overall survival rate dipped dramatically from 89% at 10 years to 60% at 15 years. However, if liner exchange was excluded, the survival rate at 15 years was 83.3%. In a report from the Finnish registry about 4661 primary THA cases in young patients who were followed up for 0 years to 22 years, modern uncemented stems and cups fared better than cemented ones in term of aseptic loosening. However, when all revisions were considered (including liner exchange), the survival of uncemented cups was no better than that of all polyethylene (PE) cemented cups. Because of this, alternate options should be considered. Three possible solutions include a reverse hybrid construct, an uncemented cup with improved liner congruence and diminished wear (i.e., a highly cross-linked PE), or a hard-on-hard articulation (Table 35-6).
Table 35–6 Bearing Combinations for Total Hip Arthroplasty Among Young Patients
| Bearing Surface | Advantages | Disadvantages |
|---|---|---|
| Highly cross-linked polyethylene | Improved wear properties, no systemic toxicity, multiple liner options (e.g., elevated rim), lower cost | Compromise with other material properties, increased bioactivity of wear particles |
| Metal on metal | Higher wear resistance, allows for bigger diameters | Increased ion levels with concerns for carcinogenesis, delayed hypersensitivity, position sensitive |
| Ceramic on ceramic | Highest wear and corrosion resistance, no systemic toxicity | Position sensitive, fracture risk, liner chipping, increased synovitis, stripe wear, squeaking, difficult revision if Morse taper is damaged, higher cost |
Metal-on-polyethylene and ceramic-on-polyethylene bearing surfaces may combine some of the advantages of each, but they demonstrate higher wear than metal-on-metal or ceramic-on-ceramic bearing surfaces.
The use of newer combinations (e.g., ceramic-on-metal) requires further research. In preliminary studies, theses combinations have shown lower wear, absence of stripe wear, and lower metal ions.
From Williams S, Schepers A, Isaac G, Hardaker C, Ingham E, van der Jagt D, Breckon A, Fisher J. The 2007 Otto Aufranc Award. Ceramic-on-metal hip arthroplasties: a comparative in vitro and in vivo study. Clin Orthop Relat Res. 2007;465:23-32; Heisel C, Silva M, Schmalzried TP. Bearing surface options for total hip replacement in young patients. Instr Course Lect. 2004;53:49-65; and Fisher J, Jin Z, Tipper J, Stone M, Ingham E. Tribology of alternative bearings. Clin Orthop Relat Res. 2006;453:25-34.
Annotated references and suggested readings
Archibeck M.J., Surdam J.W., Schultz S.C.Jr, Junick D.W., White R.E. Cementless total hip arthroplasty in patients 50 years or younger. J Arthroplasty.. 2006;21:476-483.
Berry D.J., Harmsen W.S., Cabanela M.E., Morrey B.F. Twenty-five-year survivorship of two thousand consecutive primary Charnley total hip replacements: factors affecting survivorship of acetabular and femoral components. J Bone Joint Surg Am.. 2002;84-A:171-177.
Bessette B.J., Fassier F., Tanzer M. Brooks CE. Total hip arthroplasty in patients younger than 21 years: a minimum, 10-year follow-up. Can J Surg.. 2003;46:257-262.
Bizot P., Hannouche D., Nizard R., Witvoet J., Sedel L. Hybrid alumina total hip arthroplasty using a press-fit metal-backed socket in patients younger than 55 years. A six- to 11-year evaluation. J Bone Joint Surg Br.. 2004;86:190-194.
Callaghan J.J., Forest E.E., Sporer S.M., Goetz D.D., Johnston R.C. Total hip arthroplasty in the young adult. Clin Orthop Relat Res.. 1997;344:257-262.
Capello W.N., D’Antonio J.A., Feinberg J.R., Manley M.T. Ten-year results with hydroxyapatite-coated total hip femoral components in patients less than fifty years old. A concise follow-up of a previous report. J Bone Joint Surg Am.. 2003;85:885-889.
Charles M.N., Bourne R.B., Davey J.R., Greenwald A.S., Morrey B.F., Rorabeck C.H. Soft-tissue balancing of the hip: the role of femoral offset restoration. Instr Course Lect.. 2005;54:131-141.
Charnley J. Low friction arthroplasty of the hip. In In Theory and practice.. New York:: Springer Verlag; 1981.
Clohisy J.C., Keeney J.A., Schoenecker P.L. Preliminary assessment and treatment guidelines for hip disorders in young adults. Clin Orthop Relat Res.. 2005;441:168-179.
Crowther J.D., Lachiewicz P.F. Survival and polyethylene wear of porous-coated acetabular components in patients less than fifty years old: results at nine to fourteen years. J Bone Joint Surg Am.. 2002;84:729-735.
D’Antonio J.A., Capello W.N., Manley M.T., Feinberg J. Hydroxyapatite coated implants. Total hip arthroplasty in the young patient and patients with avascular necrosis. Clin Orthop Relat Res.. 1997;344:124-138.
Devitt A., O’Sullivan T., Quinlan W. 16- to 25-year follow-up study of cemented arthroplasty of the hip in patients aged 50 years or younger. J Arthroplasty.. 1997 Au;12(5):479-489.
Dorey F.J. Survivorship analysis of surgical treatment of the hip in young patients. Clin Orthop Relat Res.. 2004;418:23-28.
Dorr L.D. Hip arthroplasty. Minimally invasive techniques and computer navigation. Philadelphia, PA: Saunders Elsevier, 2006.
Dorr L.D., Kane T.J.3rd, Conaty J.P. Long-term results of cemented total hip arthroplasty in patients 45 years old or younger. A 16-year follow-up study. J Arthroplasty.. 1994;9(5):453-456.
Eggli S., Pisan M., Müller M.E. The value of preoperative planning for total hip arthroplasty. J Bone Joint Surg Br.. 1998;80(3):382-390.
Eskelinen A., Remes V., Helenius I., Pulkkinen P., Nevalainen J., Paavolainen P. Total hip arthroplasty for primary osteoarthrosis in younger patients in the Finnish arthroplasty register. 4,661 primary replacements followed for 0–22 years. Acta Orthop.. 2005;76(1):28-41.
Eskelinen A., Remes V., Helenius I., Pulkkinen P., Nevalainen J., Paavolainen P. Uncemented total hip arthroplasty for primary osteoarthritis in young patients: a mid to long-term follow-up study from the Finnish Arthroplasty Register. Acta Orthop.. 2006;77(1):57-70.
Furnes O., Lie S.A., Espehaug B., Vollset S.E., Engesaeter L.B., Havelin L.I. Hip disease and the prognosis of total hip replacements. A review of 53,698 primary total hip replacements reported to the Norwegian Arthroplasty Register 1987–99. J Bone Joint Surg Br.. 2001;83(4):579-586.
Ganz R., Parvizi J., Beck M., Leunig M., Nötzli H., Siebenrock K.A. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. (417); 2003:112-120.
Geschwend N., Frei T., Morscher E., Nigg B., Loehr J. Alpine and cross-country skiing after total hip replacement: 2 cohorts of 50 patients each, one active, the other inactive in skiing, followed for 5–10 years. Acta Orthop Scand.. 2000;71(3):243-249.
Hardidge A.J., Hooper J., McMahon S. Current attitudes to total hip replacement in younger patients: a comparison of two nations. ANZ J Surg.. 2003;73(5):280-283.
Healy W.L., Iorio R., Lemos M.J. Athletic activity after joint replacement. Am J Sports Med.. 2001;29(3):377-388.
Jäger M., Endres S., Wilke A. Total hip replacement in childhood, adolescence and young patients: a review of the literature. Z Orthop Ihre Grenzgeb.. 2004;142(2):194-212.
Kearns S.R., Jamal B., Rorabeck C.H., Bourne R.B. Factors affecting survival of uncemented total hip arthroplasty in patients 50 years or younger. Clin Orthop Relat Res.. 2006;453:103-109.
Keener J.D., Callaghan J.J., Goetz D.D., Pederson D.R., Sullivan P.M. Johnston RC. Twenty-five-year results after Charnley total hip arthroplasty in patients less than fifty years old: a concise follow-up of a previous report. J Bone Joint Surg Am.. 2003;85:1066-1072.
Kerboull L., Hamadouche M., Courpied J.P., Kerboull M. Long-term results of Charnley-Kerboull hip arthroplasty in patients younger than 50 years. Clin Orthop Relat Res. (418); 2004:112-118.
Kim Y.H., Kook H.K., Kim J.S. Total hip replacement with a cementless acetabular component and a cemented femoral component in patients younger than fifty years of age. J Bone Joint Surg Am.. 2002;84:770-774.
Kim S.Y., Kyung H.S., Ihn J.C., Cho M.R., Koo K.H., Kim C.Y. Cementless Metasul metal-on-metal total hip arthroplasty in patients less than fifty years old. J Bone Joint Surg Am.. 2004;86:2475-2481.
Kim Y.H., Oh S.H., Kim J.S. Primary total hip arthroplasty with a second-generation cementless total hip prosthesis in patients younger than fifty years of age. J Bone Joint Surg Am.. 2003;85:109-114.
Lucas D.H., Scott R.D. The Ranawat sign. A specific maneuver to assess component positioning in total hip arthroplasty. J Orthop Tech.. 1994;2:59-61.
Maheshwari A.V., Malik A., Dorr L.D. Impingement of the native hip joint. J Bone Joint Surg Am.. 2007;89(11):2508-2518.
Malik A., Maheshwari A., Dorr L.D. Impingement with total hip replacement. J Bone Joint Surg Am.. 2007;89(8):1832-1842.
Mancuso C.A., Ranawat C.S., Esdaile J.M., Johanson N.A., Charlson M.E. Indications for total hip and total knee arthroplasties. Results of orthopaedic surveys. J Arthroplasty.. 1996;11(1):34-46.
McAuley J.P., Szuszczewicz E.S., Young A., Engh C.A., Sr Total hip arthroplasty in patients 50 years and younger. Clin Orthop Relat Res. (418); 2004:119-125.
McCarthy J.C., Busconi B. The role of hip arthroscopy in the diagnosis and treatment of hip disease. Orthopedics.. 1995;18(8):753-756.
Migaud H., Jobin A., Chantelot C., Giraud F., Laffargue P., Duquennoy A. Cementless metal-on-metal hip arthroplasty in patients less than 50 years of age: comparison with a matched control group using ceramic-on-polyethylene after a minimum 5-year follow-up. J Arthroplasty.. 2004;19(8 Suppl 3):23-28.
National Institute for Health and Clinical Excellence (NICE). Guidance on the selection of the prosthesis for primary hip replacement. 2003. London www.nice.org.uk
Neumann L., Freund K.G. Sørensen KH. Total hip arthroplasty with the Charnley prosthesis in patients fifty-five years old and less. Fifteen to twenty-one-year results. J Bone Joint Surg Am.. 1996;78:73-79.
Parvataneni H.K., Ranawat A.S., Ranawat C.S. The use of local periarticular injections in the management of postoperative pain after total hip and knee replacement: a multimodal approach. Instr Course Lect.. 2007;56:125-131.
Parvizi J., Campfield A., Clohisy J.C., Rothman R.H., Mont M.A. Management of arthritis of the hip in the young adult. J Bone Joint Surg Br.. 2006;88(10):1279-1285.
Ranawat C.S., Rao R.R., Rodriguez J.A., Bhende H.S. Correction of limb-length inequality during total hip arthroplasty. J Arthroplasty.. 2001;16(6):715-720.
Ranawat C.S., Rodriguez J.A. Functional leg-length inequality following total hip arthroplasty. J Arthroplasty.. 1997;12(4):359-364.
Schreurs B.W., Gardeniers J.W. Factors affecting survival of uncemented total hip arthroplasty in patients 50 years or younger. Clin Orthop Relat Res.. 2006;453:103-109.
Schreurs B.W., Gardeniers J.W. Total hip arthroplasty for primary osteoarthrosis in younger patients in the Finnish arthroplasty register. Acta Orthop.. 2005;76(4):604-605.
Second letter to the editor concerning Total hip arthroplasty for primary osteoarthrosis in younger patients in the Finnish arthroplasty register,” by Eskelinen et al and correspondence. Acta Orthop, 76; 2005:28-41. 604–607. Acta Orthop. 2006;77(2):337–338; author reply 338–341
Singh S., Trikha S.P., Edge A.J. Hydroxyapatite ceramic-coated femoral stems in young patients. A prospective ten-year study. J Bone Joint Surg Br.. 2004;86:1118-1123.
Sochart D.H., Porter M.L. Long-term results of cemented Charnley low-friction arthroplasty in patients aged less than 30 years. J Arthroplasty.. 1998;13(2):123-131.
Tennent T.D., Goddard N.J. Current attitudes to total hip replacement in the younger patient: results of a national survey. Ann R Coll Surg Engl.. 2000;82(1):33-38.