CHAPTER 21 Arthroscopic Synovectomy and Treatment of Synovial Disorders
Imaging and diagnostic studies
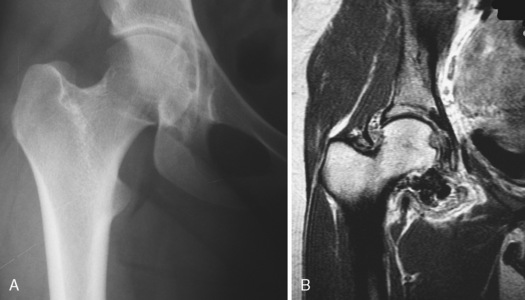
When evaluating a patient with symptoms that are consistent with hip joint pathology, plain radiographs should be obtained first. We typically obtain an anteroposterior radiograph of both hips with 2 cm to 4 cm between the pubic symphysis and the sacrococcygeal junction. A frog-leg lateral radiograph and a cross-table lateral radiograph with 15 degrees of internal rotation complete the initial series. Radiographic abnormalities may include arthritis, arthrosis, dysplasia, femoroacetabular impingement, and loose bodies. It has been reported that radiographs fail to diagnose loose bodies up to 50% of the time; this may be a result of the inconsistent calcification of these loose bodies and because they may be obscured by overlying structures. Large and multiple lucencies on plain radiographs are consistent with PVNS (Figure 21-1, A). Magnetic resonance arthrography (MRA) is the gold standard imaging technique for evaluating the hip joint proper. MRA has been shown to be very sensitive for labral tears and less accurate for chondral pathology. Filling defects can indicate loose bodies, as has been seen with synovial chondromatosis. As a result of hemosiderin deposition, pigmented villonodular synovitis is seen as a spotty or extensive low-signal area within proliferative synovial masses on T1 and T2 images; this condition is best seen on fast-field echo-sequence MRA images (see Figure 21-1, B). MRA imaging will typically reveal an effusion and variable degrees of synovitis in the setting of an acute septic hip; an aspiration can also be performed as part of this imaging. Chronic infection with associated osteomyelitis and adjacent abscesses should be ruled out in this setting before arthroscopic hip irrigation and synovial debridement are performed. MRA has important applications for imaging the rheumatoid joint. Bony erosions are visualized with MRA during the early stages of rheumatoid arthritis, and they are frequently detected before they appear on plain radiographs. MRA also detects bone marrow edema, which is another important feature that is associated with inflammatory joint disease and that may be a forerunner of erosion. Synovial membrane inflammation and hypertrophy are detected after contrast enhancement and also with the use of dynamic MRA techniques, which provide a noninvasive method for accurately measuring the inflammatory process.