CHAPTER 60 Total Elbow Arthroplasty for Primary Osteoarthritis
INTRODUCTION
As discussed in Chapter 76, primary osteoarthritis of the elbow is an uncommon lesion that affects fewer than 2% of the population.18 In recent years, an increased incidence or increased recognition, or both, resulted in a greater experience that has offered an opportunity for a more discrete treatment plan based on the specific features of the presentation. These consist both of subjective reports and objective findings. Based on the features of the presentation, three discrete surgical options have emerged: loose body removal, débridement, and joint replacement. All can be appropriate depending on patient symptoms, expectations and surgeon expertise.2,8
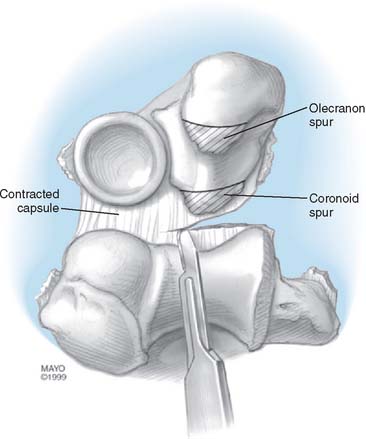
The radiographic features are motonous and generally correlate reasonably well with the patient’s symptoms. The primary pathology includes maintenance of joint space in the presence of osteophyte formation in the olecranon, olecranon fossa, coronoid, and coronoid fossa.9,11 Secondary changes include osteophytes at the margin of the radial head and loose bodies. Occasionally the radiohumeral joint is selectively involved. As implied, all of these characteristics are readily discerned by the plane radiograph. Computed tomography (CT) or magnetic resonance imaging (MRI) scans are not needed or indicated to diagnose or treat this patient.
Selecting the appropriate procedure depends on the clinical and radiographic presentation (Table 60-1). In the early stages, most patients have mild pain and are treated by nonoperative means,13 such as with anti-inflammatory medication and activity modification. Occasionally, removal of loose bodies or débridement with removal of prominent osteophytes is necessary. This can be achieved by arthrotomy or today, most commonly, by arthroscopy. Formal and more aggressive open débridement procedures are employed for extensive involvement, especially with ulnar nerve symptoms.
TABLE 60-1 Treatment Options Based on Presenting Symptoms and Radiographic Features
| Presentation | ||
|---|---|---|
| Clinical | Radiographic | Procedure |
Total elbow arthroplasty is considered an option only after débridement and loose body excision has failed3 or is not appropriate and for older patients. However, some surgeons believe that replacement rarely, if ever, is indicated for advanced primary osteoarthritis of the elbow,19 particularly if using unlinked implants.4,6,7 Still, there are no published reports or detailed clinical data to substantiate any of these positions. Readers may be surprised to learn that, until 1998, there was no information in the literature documenting either technical difficulties or the functional outcome of total joint replacement for primary arthritis of the elbow.10 Since the report in 1998, only a single additional report of a small series of replacements for degenerative disease has appeared.5 For this reason, we are reassessing our experience.
INDICATIONS
Total elbow arthroplasty is rarely indicated for primary osteoarthritis of the elbow, because it typically affects relatively young, active men. For them, several effective options are available to address the various elements of the complaint: locking, stiffness, and impingement pain (see Table 60-1).14 The specific but relative indications for joint replacement for primary arthritis include age older than 65, if possible, and a patient who does not need or expect to make extensive use of the extremity. The other options noted earlier must have failed or have been deemed inappropriate for the lesion. Most important, patients who have pain throughout the arc of motion, especially in the functional range, are the best candidates for joint replacement. Radiographs often show extensive heterotopic changes about the elbow joint (Fig. 60-1). High-grade stiffness in older patients is also a potential setting for joint replacement. The limited arc and hypertrophic changes pose technical challenges to successful replacement.
TECHNICAL CONSIDERATIONS
The technical concerns are derived from the foregoing discussion:
TECHNIQUE: COONRAD-MORREY SEMICONSTRAINED DEVICE
The surgical technique is basically that described in Chapters 53 and 57. Several specific features of the “degenerative elbow” are considered.
AFTERCARE
The arm is elevated in extension with a Cryocuff for compressive cryotherapy for the first 24 hours. If flexion or extension is a problem, splints are used, as described in Chapter 11, and postoperatively, motion is encouraged as tolerated and according to swelling and pain. The patient is usually discharged on day 3.
RESULTS
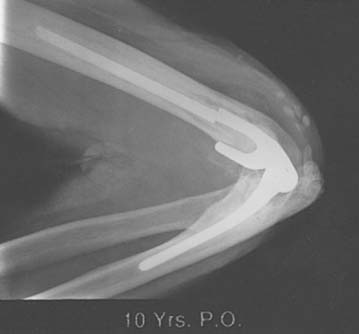
Little has been published on joint replacement for osteoarthritis. Our limited experience with a series of five cases has been reported.10 The mean age of the four men and one woman was 68 years (range 61 to 72 years) with surveillance averaging over 5 years. The mean postoperative arc was 85 degrees (37 to 122 degrees), less than that reported for other diagnoses but better by an average of 20 degrees than the mean 65 degrees (40- to 105-degree) arc preoperatively. One of two patients treated with an unlinked device had an unsatisfactory result (Fig. 60-4), and results in all three of those with the linked device were graded satisfactory. In the experience of Espag et al,5 a Souter-Strathclyde unlinked device was used in six men and four women with a mean age of 66 (range 56 to 79 years). At a mean of 68 months after surgery, one had loosened and was revised. Two additional patients had radiographic evidence of loosening, but nine of 10 were satisfied with the procedure.
COMPLICATIONS
Complications are frequent. In our series, there were four major and two minor complications in four elbows, including fracture of the humeral component with particulate synovitis, implant subluxation, heterotopic ossification, and ulnar neuropathy (Fig. 60-5).
Patients with primary degenerative arthritis of the elbow tend to be active, and most are involved in manual occupations that place greater demands on the prosthesis. One patient returned to his former occupation of carpentry, heavy lifting, and stonework. The humeral component fractured from overuse (Fig. 60-6). Two of the patients had transient postoperative ulnar neuropathy with altered sensation; both cases resolved spontaneously. Ulnar nerve irritation is associated with the development of primary osteoarthritis of the elbow joint.
Two of these elbows required revision of one of the components. In Espag’s report in addition to one revision, two radiographic loose implants, two were documented with ulnar neuropathies and two surgical infections requiring antibiotics. This is a higher rate than that reported at our institution during the same period for total elbow arthroplasty for rheumatoid arthritis (9%),15 post-traumatic arthritis (18%),17 nonunion of the distal humerus (13%),16 and even revision total arthroplasty (17%). The problems encountered, however, are consistent with the relatively high level of activity typical of persons with this diagnosis.
1 Bryan R.S., Morrey B.F. Extensive posterior exposure of the elbow. A triceps-sparing approach. Clin. Orthop. Relat. Res. 1982;166:188.
2 Cheung E.V., Adams R.A., Morrey B.F. Primary osteoarthritis of the elbow: Current treatment options. J. Am. Acad. Orthop. Surg. 2007;16:77.
3 Coonrad R.W. Comments on the historical milestones in the development of elbow arthroplasty: indications and complications. Instruct. Course Lect. 1991;40:51.
4 Dennis D.A., Clayton M.L., Ferlic D.C., Stringer E.A., Bramlett K.W. Capitello-condylar total elbow arthroplasty for rheumatoid arthritis. J. Arthroplasty. 1990;5(suppl):S83.
5 Espag M.P., Back D.L., Clark D.I., Lunn P.G. Early results of the Souter-Strathclyde unlinked total elbow arthroplasty in patients with osteoarthritis. J. Bone Joint Surg. 2003;85B:351.
6 Ewald F.C., Scheinberg R.D., Poss R., Thomas W.H., Scott R.D., Sledge C.B. Capitellocondylar total elbow arthroplasty. J. Bone Joint Surg. 1980;62A:1259.
7 Goldberg V.M., Figgie H.E.III, Inglis A.E., Figgie M.P. Total elbow arthroplasty, current concepts review. J. Bone Joint Surg. 1988;70A:778.
8 Grandstad G.D., Galatz L.M. Management of elbow osteoarthritis. J. Bone Joint Surg. 2006;88A:421.
9 Kashiwagi D. Intraarticular changes of the osteoarthritic elbow, especially about the fossa olecrani. J. Jpn. Orthop. Assn. 1978;52:1367.
10 Kozak T.K.W., Adams R.A., Morrey B.F. Total elbow arthroplasty in primary osteoarthritis of the elbow. J. Arthroplasty. 1998;13:837.
11 Minami M., Kato S., Kashiwagi D. Outerbridge-Kashiwagi’s method for arthroplasty of osteoarthritis of the elbow. 44 elbows followed for 8-16 years. J. Orthop. Sci. 1996;1:11.
12 Morrey B.F. The future of elbow joint replacement. In: Morrey B.F., editor. Joint Replacement Arthroplasty. New York: Churchill Livingstone; 1991:375.
13 Morrey B.F. Primary degenerative arthritis of the elbow. J. Bone Joint Surg. 1992;74B:409.
14 Morrey B.F. Degenerative arthritis of the elbow. In: Morrey B.F., editor. Reconstructive Surgery of the Joints. 2nd ed. New York: Churchill Livingstone; 1996:669.
15 Morrey B.F., Adams R.A. Semiconstrained arthroplasty for the treatment of rheumatoid arthritis of the elbow. J. Bone Joint Surg. 1992;74A:479.
16 Morrey B.F., Adams R.A. Semiconstrained elbow replacement arthroplasty for distal humeral nonunion. J. Bone Joint Surg. 1995;77B:67.
17 Morrey B.F., Adams R.A., Bryan R.S. Total replacement for post-traumatic arthritis of the elbow. J. Bone Joint Surg. 1991;73B:607.
18 Stanley D. Prevalence and etiology of symptomatic elbow osteoarthritis. J. Shoulder Elbow Surg. 1994;3:386.
19 Tsuge K., Mizuseki T. Debridement arthroplasty for advanced primary osteoarthritis of the elbow. J. Bone Joint Surg. 1994;76B:641.