Chapter 74 Timing of Surgery Following Spinal Cord Injury
To date, there have been no level 1 studies to determine the optimal timing of surgery for acute spinal cord injury (SCI). The reasons for this are multifactorial; there are no clear definitions of early or late surgery, every SCI is unique, and designing a randomized prospective clinical trial to determine optimal timing for surgery would be almost impossible. The optimal timing of surgery for SCI remains controversial.1,2
Animal Studies in Timing of Surgery for Spinal Cord Injury
Carlson et al. studied 16 dogs undergoing a sustained spinal cord compression for 30 or 180 minutes using a hydraulic piston.3 Somatosensory-evoked potentials were monitored during a 60-minute recovery period and at 28 days after injury. Functional motor recovery was assessed at 26 days. MRI imaging and histologic analysis were performed to assess the volume of the lesion and tissue damage. Improved motor function and balance were noted in the 30-minute group compared to the 180-minute group. The longer duration of compression produced spinal cord lesions of greater volume, which corresponded to poorer long-term functional outcomes.
Dimar et al. studied the influence of spinal canal narrowing and timing of decompression on neurologic recovery after spinal cord contusion using a spacer model of injury in 40 adult rats.4 The results of this study concluded that there was strong evidence that the prognosis for neurologic recovery was adversely affected by both a higher percentage of canal narrowing and a longer duration of canal narrowing after an SCI. Dimar et al. concluded that the tolerance for spinal canal narrowing with a contused cord appears diminished, indicating that an injured spinal cord may benefit from early decompression. They also demonstrated that the longer the spinal cord compression exists after an incomplete cord injury, the worse the prognosis for neurologic recovery.
Carlson et al. also studied the early time-dependent decompression for SCI in 21 beagles and proposed vascular mechanisms of recovery.5 His results indicated that after precise dynamic spinal cord loading to a point of functional conduction deficit (50% decline in evoked potential amplitude), a critical time period exists during which intervention in the form of early spinal cord decompression can lead to effective recovery of electrophysiologic function in the 1- to 3-hour postdecompression period.
Delamarter et al. also studied spinal cord recovery after immediate and delayed decompression in dogs.6 They studied 30 dogs with a cable constriction SCI model with periods of compression ranging from 1 hour up to 1 week. Somatosensory evoked potentials, neurologic examination, and histologic and electron microscopy studies were performed. All dogs were paraplegic after the compression of the cord, but the dogs that underwent immediate decompression or decompression within 1 hour of compression recovered the ability to walk as well as bowel and bladder control and had improvement in somatosensory evoked potentials. When compression lasted 6 hours or more, there was no neurologic recovery, and progressive necrosis of the spinal cord was observed. Somatosensory evoked potential recovery by 6 weeks after the decompression was significantly related to the duration of the compression.
Delamarter et al. concluded that longer periods of displacement allowed propagation of the chronic axonal response, resulting in lack of recovery of somatosensory evoked potentials, limited functional recovery, and more extensive tissue damage.6
Multiple other animal models of SCI have shown the positive effect of early decompressive surgery to improve neurologic recovery.7–10
Human Studies on Timing of Surgery for Spinal Cord Injury
Retrospective human studies have failed to provide convincing data to support the possibility that the neurologic outcome of early spinal surgery is superior to that of delayed spinal surgery. What has been shown is that earlier surgery can be done more safely than was previously thought. A paper in 1987 by Marshall et al. showed deterioration following SCI in 4.9% of 283 SCI patients in this prospective multicenter study.11 They concluded that early surgery on the cervical spine when cord injury is present appears hazardous. No deteriorations were observed following surgery after the sixth day.
Multiple papers have since been published demonstrating that early spine surgery can be done safely. Mirza et al. studied the changes in neurologic status, length of hospitalization, and acute complications associated with surgery within 3 days of injury versus more than 3 days after the injury.12 Forty-three patients were followed. Surgery within 72 hours of injury in patients with acute cervical cord injuries was found not to have a higher complication rate. Numbers were too small to conclude that there was definite neurologic improvement in the acute surgery group in comparison to the delayed surgery group, but trends indicated that early surgery may be beneficial. Decreased hospitalizations were observed in the early surgery group. The duration of stay in the ICU and on mechanical ventilation was not statistically different between the two groups. The neurologic status was maintained, and the change in Frankel grade from the preoperative level to the postoperative level was statistically significant in the groups of patients who underwent early surgery (P = .0026) but not in the group of patients who underwent late surgery (P = .30).
Croce et al. also studied early surgery (within 3 days) versus late surgery (after 3 days) in a mix of cervical (163: 83 early, 80 late), thoracic (79: 30 early, 49 late), and lumbar (49: 29 early, 20 late) fractures.13 Of the 291 patients, there were no differences in injury severity between the early and late groups for each fracture site. What was identified was that the thoracic fracture group showed that early fixation was associated with a lower incidence of pneumonia, a shorter ICU stay, a decreased number of days on a ventilator, and lower charges. Overall, high-risk patients were found to have had lower pneumonia rates and less hospital resource utilization with early fixation. The neurologic status was not an outcome variable in this study; however, the researchers concluded that early fixation resulted in significant resource reductions for patients with neurologic deficits. They concluded that early fixation resulted in a better outcome (not neurologic outcome) and less resource utilization regardless of neurologic deficit.
A retrospective study by Schlegel et al. of 138 patients with acute spine injuries also addressed the issue of timing of surgery.14 They found no statistically significant difference in the incidence of medical complications in patients with injury severity scores (ISSs) of less than 15 who were operated on within 72 hours or after 72 hours of injury. A separate group of patients with cervical spine injuries with neurologic deficit was analyzed, and it was determined that irrespective of associated injuries, all had fewer complications if they underwent surgery within 72 hours. Morbidity was found to be higher in the neurologic deficit group compared to the neurologically intact group. This study concluded that surgical decompression, reduction, and/or fixation of spine fractures within the first 72 hours are indicated in multiple trauma patients (ISS ≥18) and cervical injuries with neurologic deficits.
A retrospective study by Chipman et al. looked at early surgery for thoracolumbar spine injuries.15 One-hundred forty-six patients were identified (58 with ISS <15, 88 with ISS ≥15). Early surgery was determined to be within 72 hours or less, and late surgery was more than 72 hours following injury. Chipman was able to conclude that early surgery in severely injured patients with thoracolumbar spine trauma was associated with fewer complications and shorter hospital and ICU lengths of stay, required less ventilator support for noninfectious reasons, and did not increase neurologic deficits.
Schinkel et al. analyzed the German National Trauma Database (N = 8057).16 Clinical parameters and outcomes of patients with severe thoracic spine injuries (N = 298) were compared to patients undergoing early (<72 hours) versus late (>72 hours) spine stabilization. They were able to show further evidence that early stabilization of thoracic spine injuries in trauma patients reduces overall hospital and ICU stays and improves outcome. The outcome was, overall, not specific for neurologic function.
Kerwin et al. examined the records of the National Trauma Data Bank (NTDB) to determine the efficacy of early surgery (<72 hours) versus late surgery (>72 hours) of 16,812 patients undergoing operative fixation.17,18 Fifty-nine percent of the surgeries were completed within 3 days of injury. Three hundred seventy-four patients in the late surgery (>72 hours) group were matched to 497 patients in the early surgery group. Kerwin et al. found no significant difference in the presence of SCI between the early and late groups. Complications were significantly higher in the late group (30% vs. 17.5%; P < .0001), yet mortality was similar in the two groups. This study concluded that National Trauma Data Bank records indicate that the majority of patients with spine fractures undergo operative fixation within 3 days and that these patients had fewer complications and required less resources.
A small (N = 27) prospective randomized and controlled study by Cengiz et al. looked at the timing of thoracolumbar spine injuries in early surgery (<8 hours) and late surgery (3 to 15 days) cohorts.19 They determined that the early group (<8 hours) had significantly shorter overall hospital and ICU stays, fewer systemic complications, and better neurologic improvement than the later group (P < .05). They concluded that early surgery may improve neurologic recovery.
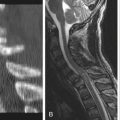
Yamazaki et al. analyzed the prognostic factors affecting the outcome of 47 patients with traumatic central cord syndrome.20 They determined that patient age, admission, Japan Orthopedic Association score, signal change within the cord on MRI, and associated spine diseases were not significant in predicting the patients’ recovery. They determined that the anteroposterior diameter of the spinal canal (P = .0402) and the interval between injury and surgery (P < .0001) were factors that were predictive of excellent recovery. In this series, 13 patients underwent surgery within 2 weeks, and 10 patients underwent surgery after 2 weeks. In the surgical treatment group, timely surgery was found to improve the outcome, while conservative treatment in patients with a low Japan Orthopedic Association score, relatively small anteroposterior diameter of the cord, or signal change within the cord on T2-weighted MRI did not improve.
A small study of 30 patients with spinal cord contusions and complete SCI was done by Zhu et al.21 Patients underwent internal fixation, laminectomy for epidural decompression, separation of the arachnoid adhesions to restore cerebrospinal fluid flow, and debridement of the spinal cord necrotic tissue with concomitant intramedullary decompression. In this study, all patients recovered some ability to walk. The timing of the operation after injury was determined to be important; the optimal operation time window was identified to be 4 to 14 days after injury.
A study from 1994–1995 performed by Tator et al. reviewed the use and timing of surgery in patients with acute SCI at 36 North American centers.22 This retrospective multicenter study concluded that there is little agreement on the optimum timing of surgical treatment for SCI. They identified that approximately 66% of patients with acute SCI undergo surgical treatment. They found that only a minority of patients (23.5%) underwent surgery within 24 hours of trauma, and even surgery that is performed within this interval may be too late to reverse some of the secondary injury mechanisms that are identified after SCI. Tator et al. confirmed the need for a randomized controlled trial to assess the optimum timing of decompressive surgery in SCI. This paper also has an excellent discussion of the difficulties in trying to design and conduct a prospective randomized controlled trial of the timing and effectiveness of decompressive surgery after acute SCI. From these difficulties have come multiple evidence-based reviews.
Evidence-Based Reviews
Fehlings and Tator published their evidence-based review of decompressive surgery in acute SCI.23 The animal model studies that they cited (N = 16) were consistent in demonstrating the beneficial effect of early decompressive surgery. The human clinical studies were primarily class III, N = 17 (retrospective studies), or class II, N = 5 (well-designed comparative clinical studies or prospective series studies). These studies were difficult to compare because of differences in the definitions of early versus late surgeries. The results of the studies of decompressive surgery in patients with acute SCI were mixed, with a trend in the earlier studies (late 1970s to mid-1980s) to favor no difference or late surgery for acute SCI. Since the late 1980s, the results have trended to no difference or early surgery as being possibly beneficial. Multiple class II trials have shown that early decompressive surgery can be performed safely without added morbidity or mortality.
A more recent review by LaRosa et al. using meta-analysis of data obtained through a Medline Search from 1966 to 2000 used a 24-hour window for early surgery compared to those having late surgery or conservative treatment.24 The analysis included 1687 eligible patients and statistically showed that early decompression resulted in better (neurologic) outcome compared to both conservative (P < .001) and late (P < .001) management. However, analysis of homogeneity showed that only data on patients with incomplete neurologic deficits who had early surgery were reliable. From this, they concluded that although statistically the percentage of patients with incomplete neurologic deficits improving after early decompression, 89.7% (95% confidence interval), appears to be better than with other modes of treatment when taking into consideration the material available for analysis and the various other factors including clinical limitations, early surgical decompression can be considered only as a practice option for all groups of patients.
A subsequent systematic review by Fehlings and Perrin published in 2006 summarized the results of studies published within the last 10 years (1995–2005).25 From this review, they had 15 surgical studies and 4 closed reduction studies that provided class II evidence to recommend the following:
• Early surgery (<72 hours) can be performed safely in patients with SCI if they have hemodynamic optimization.
• The data support a recommendation for urgent reduction of bilateral locked facets in a patient with incomplete tetraplegia.
• The data support a recommendation for urgent decompression in a patient with SCI with neurologic deterioration.
Class III evidence was provided to recommend the following:
• Decompression is a reasonable practice option in acute SCI; when possible, except in patients with life-threatening multisystem trauma, it is recommended that urgent decompression be performed within 24 hours of SCI.
• Early (<24 hours) surgery reduces length of stay in patients with acute SCI and may reduce postinjury medical complications. No standard regarding the timing or role of decompression in acute SCI could be determined.
A smaller systematic review by Rutges et al. looked at the neurologic and clinical outcomes with respect to the timing of thoracic and lumbar fracture fixation.26 They reviewed 10 papers and concluded that early fracture fixation is associated with fewer complications and shorter hospital and ICU stays. They noted that the effect of early treatment on the neurologic outcome remains unclear owing to the contradictory results of the included studies. They also concluded that early thoracic and lumbar fracture fixation results in improvement of clinical outcome, but the effect on neurologic outcome remains controversial.
No Difference in Acute versus Delayed Surgery
Multiple studies have determined no effect of the timing of surgery on improvement of neurologic outcomes. One of the larger retrospective case series (class III evidence) is a study by McKinley et al. involving 779 consecutive patients with acute nonpenetrating traumatic SCI.27 These patients were obtained from a multicenter National Spinal Cord Injury Database. This study looked at neurologic, medical, and functional outcomes of acute SCI patients undergoing early (<24 hours, 24 to 72 hours) and late (>72 hours) spine surgery versus those treated medically. McKinley et al. concluded that early versus late spine surgery was associated with shorter lengths of stay and reduced pulmonary complications; however, no differences in neurologic or functional improvements were noted between early and late surgical groups.
A retrospective case series by Sapkas and Papadakis of 67 patients with lower cervical spine fractures or fracture-dislocations showed 87% with neurologic deficit.28 Surgery was early (within 72 hours) in 31 patients and late (>72 hours) in 36 patients. Their results indicated that only patients with incomplete SCI had neurologic improvement after surgery. They found that there were no statistically significant differences in final neurologic outcomes in patients having early surgery compared to delayed surgery; therefore, they concluded that the timing of surgery does not affect neurologic outcomes.
A paper published by Chen et al. in 2009 reviewed 49 patients with surgical treatment for traumatic central cord syndrome.29 They concluded that surgery could safely be performed in patients with traumatic central cord syndrome; however, factors including type of lesion, timing of surgery within or after 4 days, and surgical approach were not associated with a final American Spinal Injury Association (ASIA) score. The improvement in the ASIA motor score was positively correlated with age at injury.
Vaccaro et al. published their prospective randomized (potentially class II data) study of 62 cervical acute SCI patients undergoing early (N = 34, <72 hours) and late (N = 38, >5 days) surgery.30 Unfortunately, 20 patients were lost in follow-up. The results showed no significant difference in length of acute postoperative ICU stay, length of inpatient rehabilitation, or improvement in ASIA grade or motor score between early (mean 1.8 days) and late (mean 16.8 days) surgery. They concluded that there was no significant neurologic benefit when cervical spinal cord decompression after trauma is performed in less than 72 hours after injury compared to waiting longer than 5 days.
Bötel et al. analyzed retrospective data on 255 acute SCI patients of whom 178 had surgical decompression and stabilization.31 Of these, 51.4% had early surgery (<24 hours) and 10.5% had late surgery (>2 weeks). This study did not control for methylprednisolone administration or mechanism of injury (tumor, trauma), and a high reoperation rate of 45.2% was observed, but no neurologic recovery was noted in complete SCI patients. No association of neurologic recovery was associated with the timing of decompressive surgery.
A prospective nonrandomized clinical trial was performed by Vale et al. and published in 1997.32 This study observed 77 patients, of whom 58 had surgery (11, <24 hours; 13 to 24, 72 hours; 34, >72 hours). All patients were managed with Swan-Ganz and arterial catheters, immobilization, and fracture reduction; systolic blood pressure >85 mm Hg was maintained. Surgical treatment was used in 31 of 35 patients with cervical cord injuries and in 27 of 29 patients with thoracic cord injuries. Early surgery (<24 hours) was performed in 11 patients (7 cervical and 4 thoracic), 9 patients had surgery within 24 to 72 hours (9 cervical and 4 thoracic), and 34 patients had delayed surgery (>72 hours) (15 cervical and 19 thoracic). Researchers found no statistically significant differences between the preoperative routine neurologic examination and the selection for, or timing of, surgery in patients with cervical or thoracic SCI in this series. The 12-month follow-up revealed no statistically significant impact on the timing of surgery with respect to outcome.
Cengiz S.L., Kalkan E., Bayir A., et al. Timing of thoracolumbar spine stabilization in trauma patients: impact on neurological outcome and clinical course. A real prospective (RCT) randomized controlled study. Arch Orthop Trauma Surg. 2008;128:959-966.
Chen L., Yang H., Yang T., et al. Effectiveness of surgical treatment for traumatic central cord syndrome. J Neurosurg Spine. 2009;10:3-8.
Chipman J.G., Deuser W.E., Beilman G.J. Early surgery for thoracolumbar spine injuries decreases complications. J Trauma. 2004;56:52-57.
Fehlings M.G., Perrin R.G. The timing of surgical intervention in the treatment of spinal cord injury: a systematic review of recent clinical evidence. Spine (Phila Pa 1976). 2006;31(Suppl 11):S28-S35.
Kerwin A.J., Griffen M.M., Tepas J.J.III, et al. Best practice determination of timing of spinal fracture fixation as defined by analysis of the National Trauma Data Bank. J Trauma. 2008;65:824-831.
McKinley W., Meade M.A., Kirshblum S., Barnard B. Outcomes of early surgical management versus late or no surgical intervention after acute spinal cord injury. Arch Phys Med Rehabil. 2004;85:1818-1825.
Rutges J.P., Oner F.C., Leenen L.P.H. Timing of thoracic and lumbar fracture fixation in spinal injuries: a systematic review of neurological and clinical outcome. Eur Spine J. 2007;16:579-587.
Schinkel C., Anastasiadis A.P. The timing of spinal stabilization in polytrauma and in patients with spinal cord injury. Curr Opin Crit Care. 2008;14:685-689.
1. Kishan S., Vives M.J., Reiter M.F. Timing of surgery following spinal cord injury. J Spinal Cord Med. 2005;28:11-19.
2. Schinkel C., Anastasiadis A.P. The timing of spinal stabilization in polytrauma and in patients with spinal cord injury. Curr Opin Crit Care. 2008;14:685-689.
3. Carlson G.D., Gorden C.D., Oliff H.S., et al. Sustained spinal cord compression: Part I: Time-dependent effect on long-term pathophysiology. J Bone Joint Surg [Am]. 2003;85:86-94.
4. Dimar J.R.II, Glassman S.D., Raque G.H., et al. The influence of spinal canal narrowing and timing of decompression on neurologic recovery after spinal cord contusion in a rat model. Spine (Phila Pa 1976). 1999;24(16):1623-1633.
5. Carlson G.D., Minato Y., Okada A., et al. Early time-dependent decompression for spinal cord injury: vascular mechanisms of recovery. J Neurotrauma. 1997;14(12):951-962.
6. Delamarter R.B., Sherman J., Carr J.B. Pathophysiology of spinal cord injury: recovery after immediate and delayed decompression. J Bone Joint Surg [Am]. 1995;77:1042-1049.
7. Bohlman H.H., Bahniuk E., Raskulinecz G., Field G. Mechanical factors affecting recovery from incomplete cervical spinal cord injury: a preliminary report. Johns Hopkins Med J. 1979;145:115-125.
8. Dolan E.J., Tator C.H., Endrenyi L. The value of decompression for acute experimental spinal cord compression injury. J Neurosurg. 1980;53:749-755.
9. Guha A., Tator C.H., Endrenyi L., Piper I. Decompression of the spinal cord improves recovery after acute experimental spinal cord compression injury. Paraplegia. 1987;25:324-339.
10. Kobrine A.I., Evans D.E., Rizzoli H.V. Experimental acute balloon compression of the spinal cord. Factors affecting disappearance and return of the spinal evoked response. J Neurosurg. 1979;51:841-845.
11. Marshall L.F., Knowlton S., Garfin S.R., et al. Deterioration following spinal cord injury: a multicenter study. J Neurosurg. 1987;66:400-404.
12. Mirza S.K., Krengel W.F.III, Chapman J.R., et al. Early versus delayed surgery for acute cervical spinal cord injury. Clin Orthop Relat Res. 1999;359:104-114.
13. Croce M.A., Bee T.K., Pritchard E., et al. Does optimal timing for spine fracture fixation exist? Ann Surg. 2001;233(6):851-858.
14. Schlegel J., Bayley J., Yuan H., Fredricksen B. Timing of surgical decompression and fixation of acute spinal fractures. J Orthop Trauma. 1996;10(5):323-330.
15. Chipman J.G., Deuser W.E., Beilman G.J. Early surgery for thoracolumbar spine injuries decreases complications. J Trauma. 2004;56:52-57.
16. Schinkel C., Frangen T.M., Kmetic A., et al. Timing of thoracic spine stabilization in trauma patients: impact on clinical course and outcome. J Trauma. 2006;61:156-160.
17. Kerwin A.J., Frykberg E.R., Schinco M.A., et al. The effect of early surgical treatment of traumatic spine injuries on patient mortality. J Trauma. 2007;63:1308-1313.
18. Kerwin A.J., Griffen M.M., Tepas J.J.III, et al. Best practice determination of timing of spinal fracture fixation as defined by analysis of the National Trauma Data Bank. J Trauma. 2008;65:824-831.
19. Cengiz S.L., Kalkan E., Bayir A., et al. Timing of thoracolumbar spine stabilization in trauma patients: impact on neurological outcome and clinical course. A real prospective (RCT) randomized controlled study. Arch Orthop Trauma Surg. 2008;128:959-966.
20. Yamazaki T., Yanaka K., Fujita K., et al. Traumatic central cord syndrome: analysis of factors affecting the outcome. Surg Neurol. 2005;63:95-100.
21. Zhu H., Feng Y.P., Young W., et al. Early neurosurgical intervention of spinal cord contusion: an analysis of 30 cases. Chin Med J. 2008;121(24):2473-2478.
22. Tator C.H., Fehlings M., Thorpe K., Taylor W. Current use and timing of spinal surgery for management of acute spinal cord injury in North America: results of a retrospective multicenter study. J Neurosurg. 1999;91:12-19. Suppl 1
23. Fehlings M.G., Tator C.H. An evidence-based review of decompressive surgery in acute spinal cord injury: rationale, indications, and timing based on experimental and clinical studies. J Neurosurg. 1999;91:1-11. Suppl 1
24. LaRosa G., Conti A., Cardali S., et al. Does early decompression improve neurological outcome of spinal cord injured patients? Appraisal of the literature using a meta-analytical approach. Spinal Cord. 2004;42:503-512.
25. Fehlings M.G., Perrin R.G. The timing of surgical intervention in the treatment of spinal cord injury: a systematic review of recent clinical evidence. Spine (Phila Pa 1976). 2006;31(Suppl 11):S28-S35.
26. Rutges J.P.H.J., Oner F.C., Leenen L.P.H. Timing of thoracic and lumbar fracture fixation in spinal injuries: a systematic review of neurological and clinical outcome. Eur Spine J. 2007;16:579-587.
27. McKinley W., Meade M.A., Kirshblum S., Barnard B. Outcomes of early surgical management versus late or no surgical intervention after acute spinal cord injury. Arch Phys Med Rehabil. 2004;85:1818-1825.
28. Sapkas G.S., Papadakis S.A. Neurological outcome following early versus delayed lower cervical spine surgery. J Orthop Surg. 2007;15(2):183-186.
29. Chen L., Yang H., Yang T., et al. Effectiveness of surgical treatment for traumatic central cord syndrome. J Neurosurg Spine (Phila Pa 1976). 2009;10:3-8.
30. Vaccaro A.R., Daugherty R.J., Sheehan T.P., et al. Neurologic outcome of early versus late surgery for cervical spinal cord injury. Spine (Phila Pa 1976). 1997;22(22):2609-2613.
31. Bötel U., Gläser E., Niedeggen A. The surgical treatment of acute spinal paralysed patients. Spinal Cord. 1997;35:420-428.
32. Vale F.L., Burns J., Jackson A.B., Hadley M.N. Combined medical and surgical treatment after acute spinal cord injury: results of a prospective pilot study to assess the merits of aggressive medical resuscitation and blood pressure management. J Neurosurg. 1997;87:239-246.