CHAPTER 20 Thyroidectomy and Parathyroidectomy
THYROIDECTOMY
Case Study
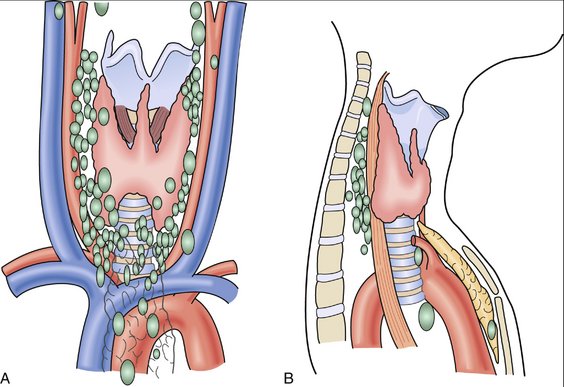
Physical examination reveals a 3-cm nodule in the right thyroid lobe of her neck that moves with swallowing. There is no cervical or supraclavicular adenopathy. An ultrasound of the thyroid shows a dominant 2.6-cm nodule in the right lobe (Fig. 20-1). Results of thyroid function tests, including triidothyronine (T3), thyroxine (T4), and thyroid-stimulating hormone (TSH) levels, are all within normal limits. A fine-needle aspiration biopsy (FNA) of the nodule demonstrates cytology consistent with a follicular neoplasm.
INDICATIONS FOR THYROID SURGERY
PREOPERATIVE EVALUATION
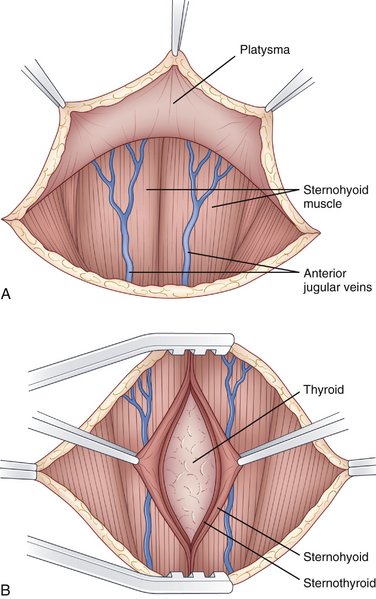
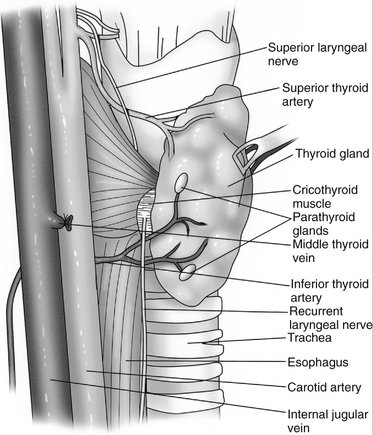
COMPONENTS OF THE PROCEDURE AND APPLIED ANATOMY
COMPLICATIONS
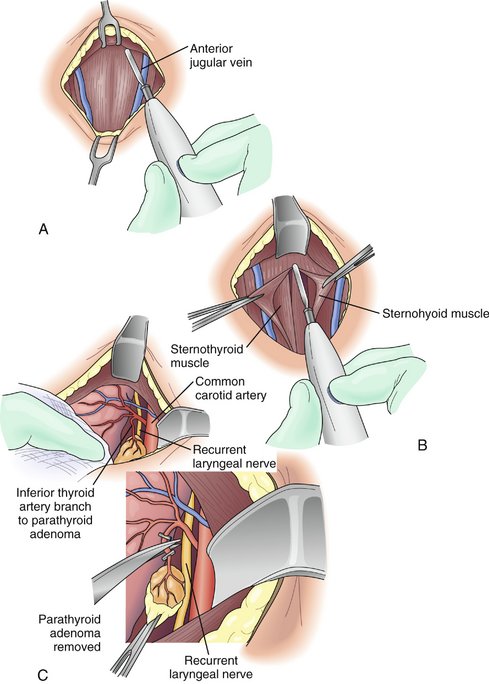
PARATHYROIDECTOMY
Case Study
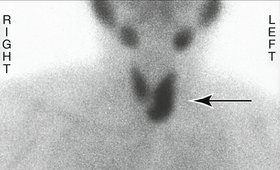
A sestamibi scan is obtained and shows increased uptake in the left side of the neck (Fig. 20-4).