CHAPTER 13 Hepatectomy
BACKGROUND
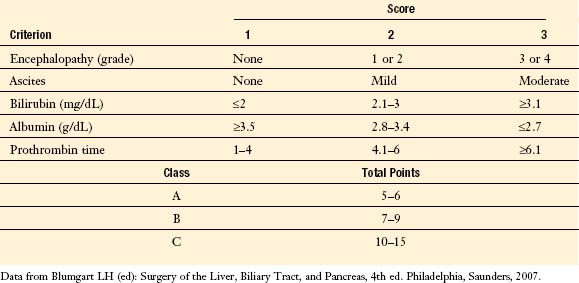
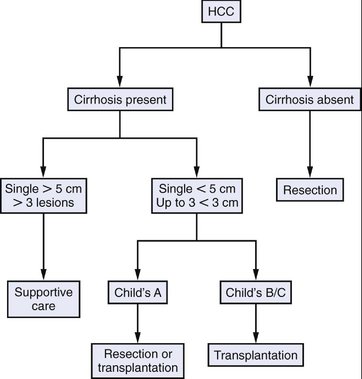
A variety of liver resections are commonly performed, including limited resections (e.g., tumor enucleation or wedge resection) and anatomic resections (i.e., removal of a segment or lobe of the liver). The extent of hepatic resection undertaken is, in part, dictated by the type of pathology and its anatomic location. Additionally, the choice of operation depends on the patient’s hepatic reserve. Up to 80% of the liver parenchyma can be removed from a normal liver because the remaining segment will hypertrophy and hepatic function will be restored within days to weeks. In the presence of underlying liver disease, however, significantly less liver parenchyma can be safely removed. The Child’s classification and its modifications are commonly used to assess a patient’s hepatic functional reserve (Table 13-1). In patients classified as Child’s class C, hepatic resection should not be attempted because of the very high risk of postoperative liver failure. Even in patients with well-compensated cirrhosis who are classified as Child’s class A, only limited hepatic resection should be performed.
INDICATIONS FOR HEPATECTOMY
PREOPERATIVE EVALUATION
COMPONENTS OF THE PROCEDURE AND APPLIED ANATOMY
Resection Nomenclature
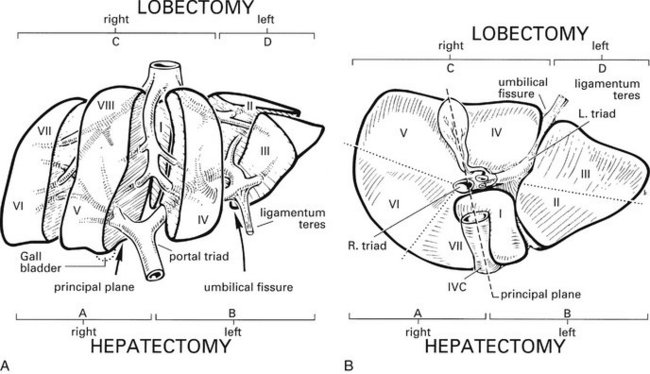
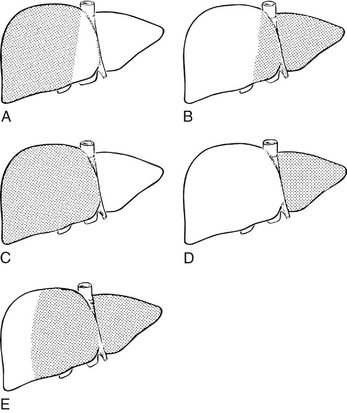
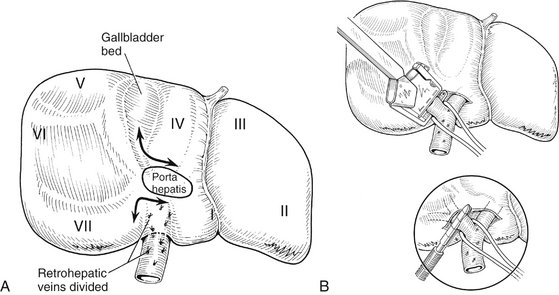
Cantlie’s line divides the liver into the right hemiliver (segments V–VIII) and the left hemiliver (segments II–IV), which are the segments that are commonly resected during right and left hepatectomy, respectively. Resection of the hepatic parenchyma to the left of the falciform ligament (segments II and III) is called left lateral segmentectomy. Resection of the hepatic parenchyma to the right of the falciform ligament (segments IV–VIII) has multiple names, including extended right hepatectomy, right trisegmentectomy, and right lobectomy, depending on which nomenclature system is used (Fig. 13-3 and Box 13-1). Other limited anatomic resections, including specific segmental resections that follow the segmental anatomy of the liver, can be performed as well. During nonanatomic wedge resections, the parenchyma and vessels are divided without consideration of the internal hepatic anatomy. Wedge resections are most commonly used for small peripheral tumors in patients with benign disease or in patients with malignant disease who cannot tolerate a formal lobectomy.
BOX 13-1
Nomenclature of Hepatic Resections
| Couinaud (1957) | Goldsmith and Woodburne (1957) |
|---|---|
| Right hepatectomy (segments V, VI, VII, VIII) | Right hepatic lobectomy |
| Left hepatectomy (segments II, III, IV) | Left hepatic lobectomy |
| Right lobectomy* (segments IV, V, VI, VII, VIII) | Extended right hepatic lobectomy* |
| Left lobectomy (segments II, III) | Left lateral segmentectomy |
| Extended left hepatectomy† (segments II, III, IV, V, VIII) [see Fig. 13-3B] | Extended left lobectomy† |
* Also referred to as a right trisegmentectomy (Starzl, 1975, 1980).
† Also referred to as a left trisegmentectomy (Starzl, 1982).
Data from Blumgart LH [ed]: Surgery of the Liver, Biliary Tract, and Pancreas, 4th ed. Philadelphia, Saunders, 2007.
Preoperative Considerations
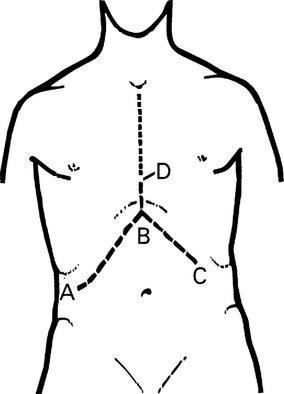
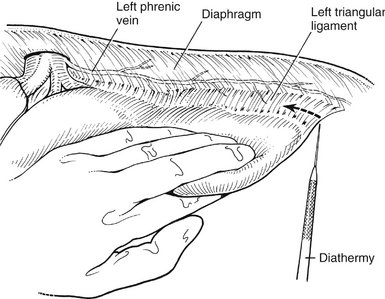
Incision and Exposure
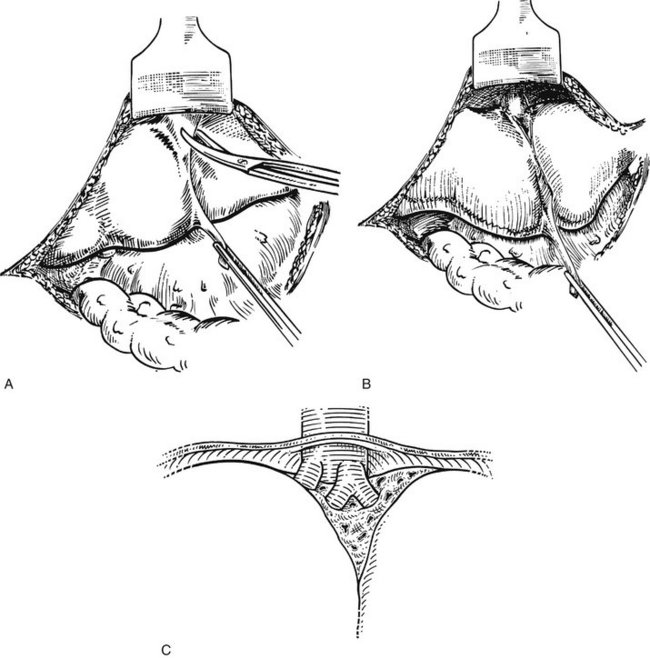
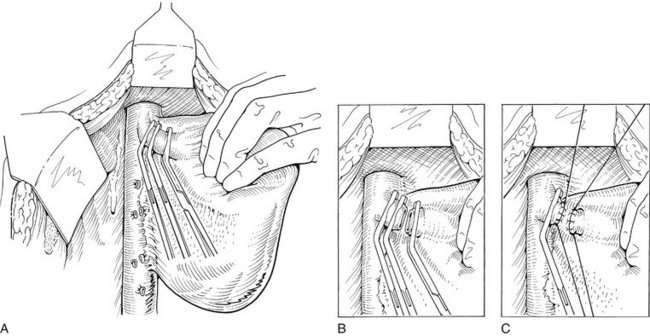
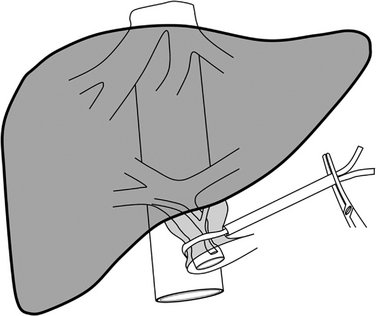
Inflow and Outflow Control
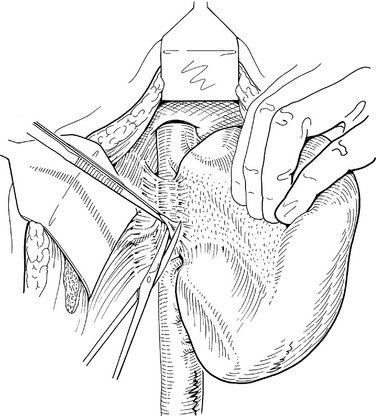
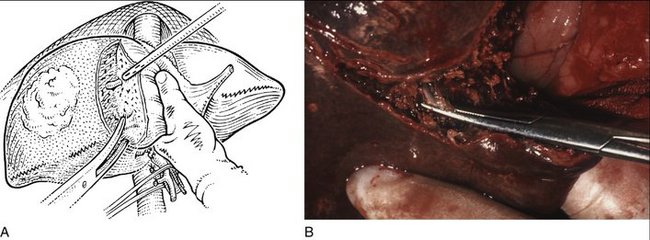
Parenchymal Transection
ADDITIONAL OPERATIVE CONSIDERATIONS
POSTOPERATIVE COURSE
Are C, Gonen M, Zazzali K, et al. The impact of margins on outcome after hepatic resection for colorectal metastasis. Ann Surg. 2007;246:295-300.
Baccarani U, Benzoni E, Adani GL, et al. Superiority of liver transplantation versus resection for the treatment of small hepatocellular carcinoma. Transplant Proc. 2007;39:1898-1900.
Blumgart LH. Surgery of the Liver, Biliary Tract, and Pancreas, 4th ed. Philadelphia: Saunders; 2007.
Mazzaferro V, Regalia E, Doci R, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996;334:693-699.
Olthoff KM, Merion RM, Ghobrial RM, et al. Outcomes of 385 adult-to-adult living donor liver transplant recipients: a report from the A2ALL Consortium. Ann Surg. 2005;242:314-323.
Pawlik TM, Choti MA. Surgical therapy for colorectal metastases to the liver. J Gastrointest Surg. 2007;11:1057-1077.