Chapter 59 Thrombotic Thrombocytopenic Purpura and the Hemolytic Uremic Syndrome
Table 59-1 Proposed Classification Scheme for Thrombotic Microangiopathies
| ADVANCED UNDERSTANDING OF ETIOLOGY |
| ETIOLOGY NOT FULLY UNDERSTOOD |
Adapted from Taylor CM, Machin S, Wigmore SJ, et al: Clinical Practice Guidelines for the management of atypical haemolytic uraemic syndrome in the United Kingdom. Br J Haematol 148:37, 2009.
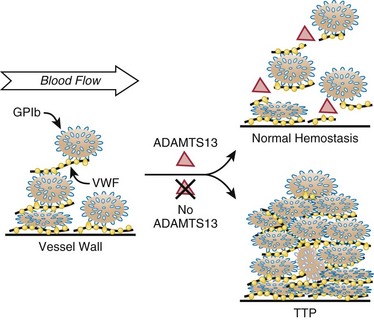
Figure 59-1 PATHOGENESIS OF IDIOPATHIC THROMBOTIC THROMBOCYTOPENIC PURPURA CAUSED BY ADAMTS13 DEFICIENCY.
(Reproduced from Sadler JE: von Willebrand factor, ADAMTS13, and thrombotic thrombocytopenic purpura. Blood 112:11, 2008, with permission.)