Chapter 43 Pain Management and Antiemetic Therapy in Hematologic Disorders
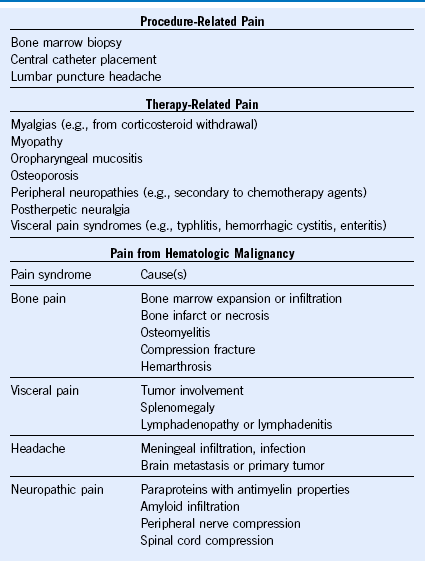
Table 43-2 Classification of Pain Syndromes in Sickle Cell Disease
|
|
Adapted from Ballas SK. Pain management of sickle cell disease. Hematol Oncol Clin North Am 19:785, 2005.
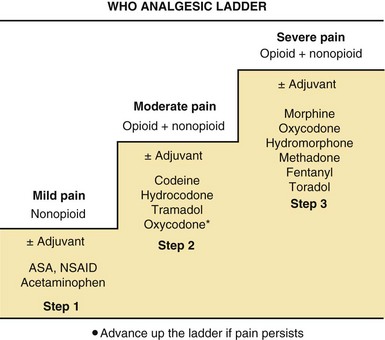
Figure 43-1 STRATEGY FOR PHARMACOLOGIC MANAGEMENT OF PAIN USING THE WORLD HEALTH ORGANIZATION (WHO) ANALGESIC LADDER.
Choice of Medication
Because a wide variety of medications are available, pharmacokinetic considerations and side effect profiles should be considered when choosing opioid agents. Intermittent moderate to severe pain lasting hours to several days is amenable to oral analgesics with short half-lives (3-4 hours) with appropriate potency (e.g., immediate-release oxycodone, morphine, hydromorphone [Dilaudid], or oxymorphone [Opana] when available). Severe pain of relatively constant intensity should be treated with oral sustained-release morphine or oxycodone taken every 8 or 12 hours,1,2 hydromorphone (Exalgo) taken every 24 hours or oxymorphone (Opana ER) taken every 12 hours, methadone taken every 8 hours, or transdermal fentanyl renewed every 48 to 72 hours. Twelve- to 24-hour formulations of oral morphine (e.g., Kadian, Avinza) are available; for patients unable to take pills, the capsule can be opened and the pellets sprinkled on food or suspended in water and given through a feeding tube10.
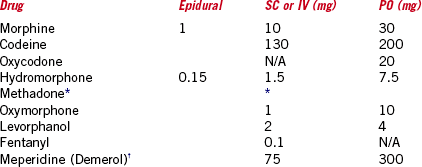
Relative Potencies of Commonly Used Opioids
Conversions Between the Transdermal Fentanyl Patch and Morphine
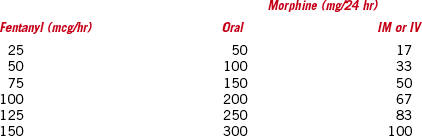
IM, Intramuscular; IV, intravenous.
Data from: Miaskowski C, Cleary J, Burney R, et al: Guideline for the management of cancer pain in adults and children, APS clinical practice guidelines series, No.3. Glenview, Ill, 2005, American Pain Society.
Emetic Risks of Chemotherapy
Moderate (30%–90%)
Low (10%–30%)
Combination Antiemetic Regimens
Low Emetogenic Potential
Dexamethasone 8 mg PO or IV 30 minutes before chemotherapy as needed or
Metoclopramide 10-20 mg PO or IV 30 minutes before chemotherapy as needed or
Compazine 10 mg PO or IV 30 minutes before chemotherapy as needed
IV, Intravenous; PO, oral; 5-HT3 RA, serotonin receptor antagonist.
1 Foley KM. Management of cancer pain. In DeVita VT, Lawrence TS, Rosenberg SA, et al, eds.: DeVita, Hellman, and Rosenberg’s Cancer: Principles and practice of oncology, ed 9, Philadelphia: Lippincott Williams & Wilkins, 2011.
2 Miaskowski C, Cleary J, Burney R, et al. Guideline for the management of cancer pain in adults and children, APS clinical practice guidelines series, No.3. Glenview, Ill: American Pain Society; 2005.