10.2 Pleural cavities, tracheobronchial tree, lungs71
10.3 Heart and pericardial cavity77
10.4 Mediastinum85
10.5 Breast94
Introduction
The thorax consists of:
• the chest wall
• the two pleural cavities surrounding the lungs
• the area between these cavities, the mediastinum, in which are found the heart, great vessels, trachea and oesophagus, vagus and phrenic nerves, thymus gland and the thoracic duct.
On the external surface of the anterolateral chest wall are the breasts (mammary glands), also considered in this chapter.
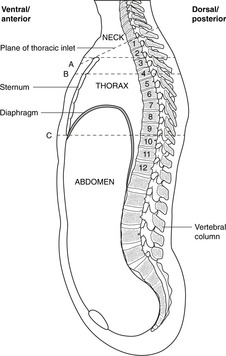
Below, the thorax is separated from the abdomen by the diaphragm; above, it is continuous with the neck at the thoracic inlet (between sternum and vertebra T1) through which structures pass between thorax and neck (Fig. 10.1).
10.1. Chest wall
The chest wall consists of the ribs and sternum laterally and anteriorly, and the vertebral column posteriorly, which provides most of the structural support. Ribs articulate with the vertebral column behind and the sternum in front, these articulations permitting the movements of breathing. Intercostal (between the ribs) spaces are occupied by muscle and a neurovascular bundle that supplies the muscles, the skin over them and the lining of the pleural cavity deep to them. The repeating pattern of vertebrae, ribs and the intercostal neurovascular bundle is an illustration of segmentation.
You should:
• describe the orientation of the ribs
• list the vertebral levels of the suprasternal notch, angle of Louis, and xiphisternum
• describe how ribs articulate with vertebrae and sternum
• describe the structure and contents of an intercostal space
• describe the formation and function of intercostal nerves and the dermatomes of the chest wall
• describe where and how to insert a chest drain.
Vertebral levels and surface markings (Fig. 10.1)
Remind yourself of the significance of vertebral levels and surface markings.
• The suprasternal notch (in which you can palpate the trachea) is at vertebral level T2.
• The sternal angle (of Louis) is at vertebral level T4.
• The xiphisternum (xiphoid process) is at vertebral level T9 (about).
• Note the downwards orientation of the ribs when you consider an anterior view of the rib cage: the second rib articulates with vertebra T2 posteriorly, but with the sternal angle at vertebral level T4 anteriorly. Therefore, a transverse (horizontal) section of the thorax, such as a scan, intersects several ribs.
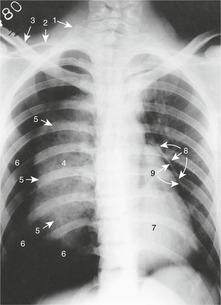
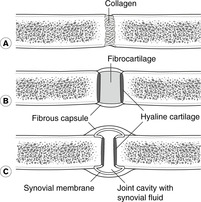
Bones and joints of the chest wall (Fig. 10.2)
The chest wall is made up of the 12 pairs of ribs, the sternum and the intercostal muscles. Ribs are numbered 1–12 from above down and articulate with the vertebral column posteriorly and (mostly) the sternum anteriorly. The ribs are angled with respect to the horizontal plane – the sternal end is lower than the vertebral – and so in horizontal section, or a transverse computerised tomography (CT) or magnetic resonance imaging scan, several ribs will be seen sectioned obliquely. Ribs are united at their anterior end to cartilage: the costal cartilages.
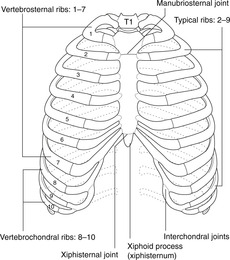 |
| Fig. 10.2 |
Vertebrae
The main features of a typical vertebra are described in Chapter 5. A thoracic vertebra is identifiable because of its facets for articulation with the ribs. Vertebrae T2–9 have two demifacets on each side, other vertebrae having only one.
Ribs
Each rib has a head, neck, tubercle and shaft. Figure 10.3 shows the main features of a typical rib (ribs 2–10). Of the atypical ribs (1, 11, 12), you need only bother with the first.
First rib
• Scalene tubercle on the upper surface, to which is attached scalenus anterior muscle.
• Groove for subclavian vein, anterior to the tubercle.
• Groove for subclavian artery, posterior to the tubercle.
Sternum
There are three parts, from superior to inferior: manubrium, body and xiphoid process (or xiphisternum). There may be a hole in the centre of the body, since it is formed by a number of individual sternebrae that should fuse together, but may fail to do so.
Joints between vertebrae and ribs
Typical ribs have three synovial articulations with the vertebrae.
• The head has upper and lower articular facets set almost at a right angle to one another, the lower articulating with the vertebra corresponding in number to the rib, and the upper with the vertebra above. Ribs 1, 10, 11 and 12 have only one facet and articulate only with the numerically corresponding vertebra.
These joints allow the ribs to move in breathing.
Ligaments
These ligaments are not of great importance. They include:
• triradiate ligament: from the head of the rib to the vertebra above, the intervertebral disc, and the vertebra below
• costotransverse ligaments between the vertebral transverse process and the tubercle of the rib.
Joints between ribs, sternum and vertebral column
• The first costal cartilage is continuous with the manubrium (primary cartilaginous joint) and remains so throughout life, unless it ossifies completely.
• Costal cartilages 2–7 have synovial articulations with the sternum. The second costal cartilage articulates at the sternal angle with the manubrium and the body of the sternum. The sternal angle (of Louis) is easily palpable and when you are counting ribs as part of a physical examination, it is best to start at the sternal angle with the second rib. In any case, the first rib is difficult to find because it is underneath the clavicle.
• Costal cartilages 8–10 have synovial articulations with the costal cartilage immediately above.
• Costal cartilages 11 and 12 are free of any anterior articulations, but provide attachments for muscles.
Articulations are summarised in Table 10.1.
• Ribs 1–7 are vertebrosternal, or true ribs.
• Ribs 8–10 are vertebrochondral or false ribs.
• Ribs 11 and 12 are floating ribs.
| Rib | Posterior articulation | Anterior articulation |
|---|---|---|
| 1 | Vertebra T1 only | Sternum (primary cartilaginous joint, so first rib and sternum move as one) |
| 2–7 | Vertebra of same number and one above | Small synovial cavity between sternum and costal cartilage |
| 8–9 | As above | Costal cartilage articulates with cartilage immediately above |
| 10 | Vertebra of same number only | Costal cartilage articulates with cartilage immediately above |
| 11, 12 | Vertebra of same number only | None |
Muscles of chest wall
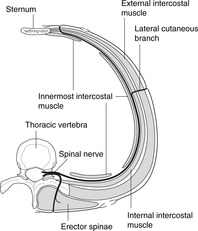
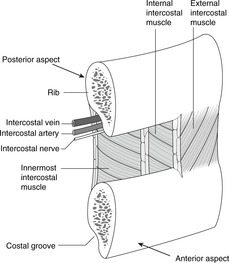
Intercostal muscles and spaces (Fig. 10.4)
There are three layers of tissue between ribs, partly muscle and partly membrane: external, internal and innermost intercostals, with the intercostal neurovascular bundle running between the internal and innermost. The area between ribs, occupied by these intercostal muscles, is the intercostal space.
• External intercostal muscle. Muscle at the back and sides, membrane anteriorly. Fibres pass from the upper rib downwards and forwards to the upper border of the rib below.
• Internal intercostal muscle. Muscle at the front and sides, membrane posteriorly.
 |
| Fig. 10.4 |
Fibres pass upwards and forwards, more or less at right angles to those of the external intercostal.
• Innermost intercostal muscle: as internal intercostal.
• Inside the chest wall there are (usually) muscle fibres that fan out from the sternum to the internal aspect of ribs 3–6. This is transversus thoracis, and it is equivalent to the transversus abdominis in the abdomen. It is not important.
Neurovascular bundle, costal groove
These muscles are supplied by the segmental intercostal nerve corresponding in number to the intercostal space. The rib has a groove underneath most of its length on the internal aspect. This costal groove provides some shelter for the intercostal neurovascular bundle. Within the groove the neurovascular bundle is arranged, from top to bottom, vein, artery, nerve (VAN). In each intercostal space, there are also smaller branches of the intercostal nerve and artery (collateral branches) which run on top of the rib below.
Muscles of the pectoral girdle
Overlying the ribs and intercostal muscles externally are muscles which attach the upper limb (humerus, clavicle and scapula) to the trunk: pectoralis major, pectoralis minor, latissimus dorsi, levator scapulae, rhomboids, and trapezius. These are considered in Chapter 12.
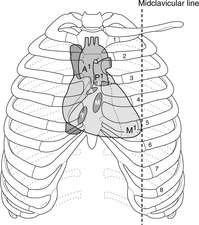
Insertion of chest drains (Fig. 10.5)
It is occasionally necessary to insert a chest drain (a hollow tube) through the chest wall into the pleural cavity. This procedure, properly termed thoracocentesis (also thoracentesis, pleurocentesis), is performed to remove either fluid (excess pleural fluid, blood) or air that had collected in the pleural cavity (see Pneumothorax, p. 72). The position of various structures which should be avoided (heart, liver, spleen, etc.) means that there are two places on either side where this may most safely be done:
• second intercostal space in the midclavicular line
• fourth or fifth space in the midaxillary line.
To avoid any risk of damage to the main intercostal neurovascular bundle, it is better to insert the chest drain in the lower half of an intercostal space.
Blood supply of chest wall
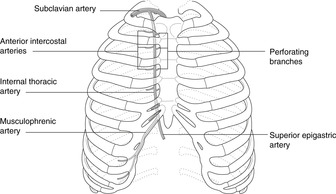
Arteries: branches of the aorta and the subclavian/axillary artery
• Anterior intercostal arteries (Fig. 10.7). These arise from the right and left internal thoracic arteries, branches of the subclavian which run internally down the chest wall 1 or 2cm lateral to the sternal border. They are important in supplying the breast. Anterior and posterior intercostal arteries anastomose with each other in the intercostal space, and this potential route between the internal thoracic artery and the aorta is important in congenital aortic coarctation (narrowing) as a bypass for the narrowing (see later and Fig. 10.25, p. 88).
• Lateral thoracic artery. Again, this is important for the breast.
• Other branches of the subclavian/axillary arteries: thoracoacromial (acromiothoracic), superior (or supreme or highest) thoracic (don’t bother with these).
Veins
• Anterior intercostal veins drain to the internal thoracic veins, thence to the subclavian – brachiocephalic – superior vena cava (SVC).
• Posterior intercostal veins drain to the azygos system and the SVC. As the first one or two posterior intercostal arteries arise differently from the rest, so the posterior intercostal veins of the first few spaces drain differently: to the brachiocephalic veins (see later).
Intercostal nerves (Fig. 10.8)
Intercostal nerves are ventral rami of the thoracic segmental nerves (see Ch. 6). Having been formed in the region of the intervertebral foramen, they run in the costal groove of each rib and supply the intercostal muscles, a strip of skin overlying the intercostal muscles and a similar strip of parietal pleura on the internal aspect of the chest wall. Anteriorly, when the ribs turn upwards, the neurovascular bundle parts company with the ribs and continues in the direction already established. Lower intercostal nerves therefore also supply skin of most of the anterior abdominal wall and the parietal peritoneum deep to it (the abdominal equivalent of parietal pleura).
Intercostal nerves contain both motor and sensory fibres
• Cell bodies of motor fibres to skeletal muscle (voluntary motor fibres) are in the ventral horn of grey matter of the correspondingly numbered spinal cord segment.
• Cell bodies of sensory fibres in an intercostal nerve are in the dorsal root ganglion of the parent segmental nerve.
This arrangement gives rise to the concept of segmental innervation, and allows automatic reflex action within one segment – a physiological phenomenon particularly important clinically in the limbs.
Intercostal nerves also convey sympathetic fibres (see later)
Segmentation, dermatomes
Segmentation is most obvious in the thorax: segmental bones (ribs), segmental nerves, dermatomes, segmental vessels, and, in a way, the vertebrae. Study Fig. 6.6 (p. 36) again, which shows the dermatome pattern for the whole body, and memorise these dermatomes in the chest:
• skin over the second intercostal space (landmark: sternal angle of Louis): spinal nerve
• T2; and similarly down the chest to skin over the xiphoid process: T7 or 8.
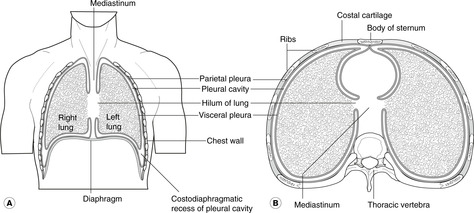
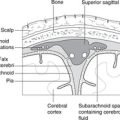
10.2. Pleural cavities, tracheobronchial tree, lungs (Figs 10.9, 10.10)
Pleural cavities, mediastinum
The right and left pleural cavities surround the right and left lungs. The tissue between them that contains heart and great vessels, etc. is the mediastinum.
The pleural cavities are, like the pericardial and peritoneal cavities, serous cavities derived from the embryonic coelom. Serous cavities, which also include synovial cavities, are lined by mesothelium, a simple squamous lining which, with associated connective tissue and basement membrane, makes up the serous membranes (pleura, pericardium, peritoneum, synovium).
They are, strictly speaking, only potential cavities. Each lung invaginates each pleural cavity as it forms in such a way that the serous lining of the cavities, the pleura, is found:
• on the inside of the chest wall – the parietal pleura
• covering the lung – the visceral pleura.
Parietal pleura on the inside of the chest wall is sometimes called the costal pleura, that on the medial side of the pleural cavity the mediastinal pleura, and that on the superior aspect of the diaphragm the diaphragmatic pleura.
The two layers of pleura glide on one another (for movement in breathing), but since there is normally nothing between the visceral and parietal pleura other than a minute amount of lubricating pleural fluid, the two layers do not separate. The surface tension of pleural fluid ensures that the two layers remain adherent. A simple analogy is two sheets of glass with water between them: the two sheets may move on one another but can not easily be separated because of the film of fluid between them.
Pneumothorax, haemothorax
If air finds its way between the visceral and parietal pleura (e.g. a lung alveolus bursts, or a person is stabbed), then the two ‘plates of glass’ separate, the lung does not move with the chest wall and the elastic tissue in the lungs causes them to collapse, thus preventing normal breathing. This is a pneumothorax (Fig. 10.11). If a blood vessel bleeds into the pleural cavity, a haemothorax develops. These conditions are treated by the insertion of a chest drain (Fig. 10.5, see p. 68).
Tracheobronchial tree (Fig. 10.12)
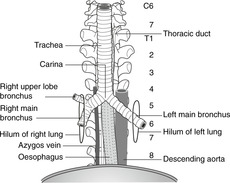 |
| Fig. 10.12 |
Trachea
The trachea begins at the level of the cricoid cartilage (vertebral level C6) and descends to its bifurcation (vertebral level about T4 in the supine position and T5 or 6 in the erect position). Its walls are made up of incomplete rings of hyaline cartilage closed posteriorly by connective tissue and trachealis muscle (involuntary muscle). Behind it is the oesophagus and between the two in the neck are the recurrent laryngeal nerves (see later).
Palpating the trachea
The trachea should be central in the suprasternal notch (vertebral level T2), and palpation of this is a routine part of a thorough clinical examination. If the trachea is deviated to one side or the other, this implies that it has been displaced by disease (e.g. a tumour or a pneumothorax pushing it to the other side).
Tracheal bifurcation and main bronchi
At the bifurcation of the trachea, the two main bronchi arise and these pass into the lungs at the hila with the pulmonary (Latin: pulmo = lung) arteries and veins. At the bifurcation, the internal ridge that separates the two main bronchi is the carina (Latin: keel) and this should be fairly sharp. The area immediately beneath the bifurcation is occupied by tracheobronchial lymph nodes, which are often involved in malignant disease. If, at bronchoscopy, the carina is less than sharp, it is likely that tracheobronchial lymph nodes are enlarged.
The right main bronchus is slightly larger in calibre than the left, and this is one reason why inhaled foreign bodies more often pass into the right main bronchus. Both bronchi pass inferolaterally from the tracheal bifurcation, but the angulation of the bronchi is by no means constant. In some people the arrangement is more or less symmetrical, whereas in others the right main bronchus is more in line with the trachea than the left. The right main bronchus passes directly to the hilum of the right lung. The left main bronchus passes anterior to the oesophagus, which it indents (vertebral level T4/5, see later) and thence to the hilum of the left lung.
Lobar bronchi
The right and left main bronchi each give lobar bronchi to the lobes of the lungs, and these divide into segmental bronchi, each serving its own bronchopulmonary segment (see later). The incomplete cartilaginous rings, like those in the trachea, persist into the lobar bronchi. Structural support to smaller bronchi is provided by randomly arranged plates of cartilage in the wall.
Lungs
Lobes and fissures
The lungs are divided by fissures into lobes. The right lung has three lobes: upper, middle and lower; the left lung has two: upper and lower. The left-sided equivalent of the right middle lobe is the lingula – part of the left upper lobe. The lobes are demarcated by fissures: oblique and horizontal on the right, and oblique only on the left. The horizontal fissure is sometimes incomplete.
Occasionally on the right, the developing azygos vein may invaginate its way into the apical portion of the right upper lobe, thus creating a ‘peninsula’ of lung tissue. This azygos fissure and lobe may be mistaken on a chest radiograph for a pathological condition.
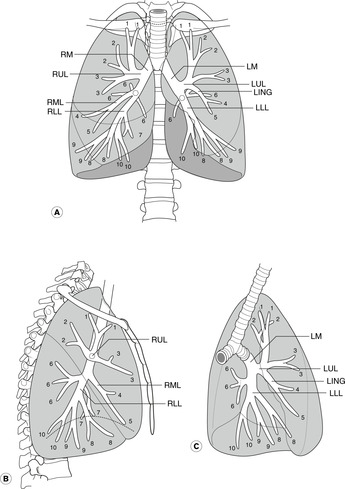
Bronchopulmonary segments (Fig. 10.13)
Each lung is made up of a number of bronchopulmonary segments, each with its own bronchus, its own branch of the pulmonary artery, and its own tributary of the pulmonary vein. These discrete units enable surgeons to excise one or more bronchopulmonary segments when disease is confined to them without compromising the function of other segments. You need to know them.
Right lung
• Upper lobe: apical, posterior and anterior bronchopulmonary segments.
• Middle lobe: lateral and medial bronchopulmonary segments.
• Lower lobe: apical, medial, anterior, lateral and posterior bronchopulmonary segments.
Conventionally, the segments are numbered 1–10 in the order given. To avoid confusion between upper and lower lobes, the lower lobe segments are often called apical basal, medial basal, and so on.
Left lung
The pattern is modified somewhat:
• The middle lobe is replaced by the superior and inferior segments of the lingula (parts of the upper lobe).
• There is no medial basal segmental bronchus and the left medial basal segment may be much reduced in size or even absent as a result of the presence of the heart.
• There may be a common origin from the left upper lobe bronchus for the left upper lobe apical and posterior segmental bronchi, although the segments themselves are separate, as on the right.
You should bear in mind that there is, as usual, some variation in this pattern from person to person. It is interesting, but of no relevance, to know that in pigs, sheep, llamas and tigers one of the right lobar bronchi arises from the trachea itself.
Pulmonary hila
These are the regions where arteries, veins, the bronchial tree, nerves and lymphatics pass between mediastinum and lungs. You need not bother with the precise arrangement of structures at the hilum except to know that the bronchi are posterior and the pulmonary arteries superior. The pulmonary ligament is the narrow inferior extension of the hilum, containing nothing of importance.
Relations of lungs to other organs
A number of important mediastinal structures are intimately related to the lungs and create impressions on the medial aspect of both lungs. On the right lung, those formed by the superior vena cava, the azygos vein and the oesophagus are noteworthy. On the left side, the impressions of the heart, the aortic arch and descending aorta are obvious.
Sensory nerve supply of pleura and lungs
Parietal pleura
• Costal: local intercostal nerves
• Diaphragmatic: local intercostal nerves (peripherally), phrenic nerve (centrally)
• Mediastinal: phrenic (mainly).
Parietal pleural sensation is somatic sensation, and pain from irritation of parietal pleura will be sharp and well localised by the patient.
Lungs and visceral pleura
The lungs and visceral pleura, like all internal organs, are supplied by visceral sensory nerves that travel back to the central nervous system in nerves also conveying sympathetic and/or parasympathetic fibres. Visceral pain is much more vague and poorly localised by the patient. Inflammation of the pleura is called pleurisy and the sharp pain commonly associated with it arises not from irritation of the visceral pleura but from irritation of parietal pleura to which the disease has spread.
Movements of breathing
Normal breathing is the result of movement of the diaphragm. The diaphragm descends, the diaphragmatic parietal pleura descends and, since the two layers of pleura can not separate, this pulls the visceral pleura down so that the lung alveoli and airways expand and air is sucked in. In expiration, the diaphragm relaxes and the elastic tissue in the lung recoils, thus expelling air in the airways. In forced inspiration other muscles are used and these include any muscles that will enlarge the rib cage in any way. Neck muscles (sternocleidomastoid) will pull it up, abdominal muscles (quadratus lumborum) will pull it down, and by fixing the upper limbs, pectoral girdle muscles (pectoralis major, latissimus dorsi) will pull it out. These are accessory muscles of respiration and you will see them in action in any patient suffering a bronchitic or asthmatic attack. The function of the intercostal muscles is not fully understood, despite what anyone may tell you, but obviously they afford a degree of flexibility between the more rigid ribs.
The shape of the costotransverse joints allows the lateral aspect of the lower ribs to swivel up and out, thus increasing the lateral diameter of the chest. The anterior ends of all ribs can swing up and out, thereby increasing the anteroposterior diameter of the chest. Disease resulting in limitation of movement at these joints can be a cause of respiratory distress.
Lymphatics of the thorax
Chest wall
Both these lymphatic channels communicate with those of the breast and may be involved in the spread of breast disease.
Lungs and trachea
There are communicating lymph plexuses immediately under the visceral pleura and around the bronchial tree. From here lymph passes to the hilum where hilar nodes are found and thence to the mediastinal nodes and the thoracic duct.
Tracheobronchial nodes
These are the mediastinal lymph nodes immediately beneath the carina. They constitute the largest collection of lymph nodes in the body and receive lymph from heart, lungs and mediastinal structures such as the oesophagus. Enlargement of these nodes will cause a widening of the carina when viewed at bronchoscopy (see above).
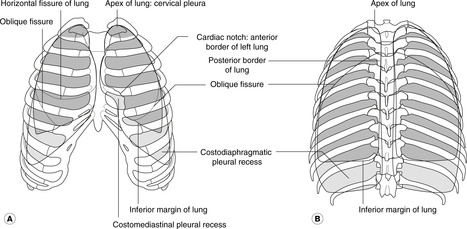
Surface markings of lungs (Fig. 10.14)
Pleural cavities and reflections
These are important. The pleura extends above the clavicle into the neck where it is vulnerable to stab wounds, so do not be surprised if a patient who has been stabbed above the clavicle is breathless: there may be a pneumothorax. In this region the superior limit of the pleural cavity is formed by the suprapleural membrane, a half-tent of membrane suspended from the transverse process of vertebra C7 to attach to the inner aspect of the first rib.
Remember 2, 4, 6, 8, 10, 12. From about 2cm above the clavicle, the line of pleural reflection passes behind the sternoclavicular joint and almost meets its fellow of the other side behind the sternal angle (level of second costal cartilage), then down to the level of the fourth costal cartilage where the left line passes laterally but the right continues down to the sixth. The lines then pass obliquely laterally across the sixth cartilage, crossing the eighth rib in the midclavicular line, the tenth rib in the midaxillary line and the twelfth rib (behind now) in the midscapular line, or even lower.
Costodiaphragmatic recess
Note that at the back the costodiaphragmatic recesses of the pleural cavities are behind the upper poles of the kidneys.
Pleura below the ribs
The three sites where the pleural reflection is below the costal margin are:
• right costosternal region (not the left, because of the heart)
• between the twelfth rib and the vertebral column on the right
• between the twelfth rib and the vertebral column on the left.
In these places abdominal incisions may enter the pleural cavity.
Lungs
These are similar to the pleura except that lung tissue does not normally extend much below vertebral level T10, and of course the extent of the lungs varies during breathing with inspiration and expiration.
• Oblique fissure (both sides): spine of vertebra T2 or T3 – sixth costal cartilage.
• Horizontal fissure (right lung only): level of fourth costal cartilage, sternal edge – line of oblique fissure.
Variations in position depending upon posture and breathing
You should bear in mind that structures move during breathing. Vertebral levels are given in Table 10.2.
| Structure | In forced expiration | In forced inspiration |
|---|---|---|
| Bifurcation of trachea | T4 | T5/6 or lower |
| Hilum of lung | T5 | T6 or lower |
| Lower border of lung | T8 (med.) to T9 (lat.) | T9 (med.) to T12 (lat.) |
Finally, it should be obvious that everything will be lower when you are standing erect than when you are lying down. For these reasons, surface markings and vertebral levels are only approximate.
Listening to (auscultating) the lungs
From a clinical point of view you should note the following:
• When you place your stethoscope on a patient’s back, you are listening mainly to the lower lobe. There is a small area of upper lobe, but no middle lobe at all.
• When you place your stethoscope on a patient’s anterior chest wall, you are listening mainly to the upper and middle lobes.
• You will listen to the middle lobe best by placing the stethoscope at the side and in the axilla.
• You can not listen to individual bronchopulmonary segments, or even to individual lobes.
• When a patient is lying in bed on his back, the most dependent bronchopulmonary segments are the apical and posterior segments of the lower lobe. These segments are most often affected by lung infections in ill, bedridden patients.
• In normal breathing, lung tissue does not occupy the lower extremities of the costodiaphragmatic recesses, but it may in deep inspiration. This means that in this region the surface markings of the extent of the lungs is different from the surface markings for the extent of the pleural cavities.
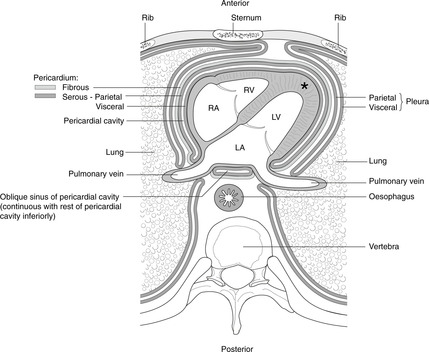
10.3. Heart and pericardial cavity
The heart is surrounded by visceral and parietal layers of serous pericardium (equivalent to the pleura), and external to these the fibrous pericardium. The heart and pericardial cavity are in the anterior mediastinum, behind the sternum slightly to the left of the midline. The heart is oriented such that the right chambers of the heart are more anterior, and the left chambers more posterior. The outflow from each chamber is guarded by a valve: right atrium–tricuspid; right ventricle–pulmonary; left atrium–mitral; left ventricle–aortic. The cardiac conducting system is the means by which contraction is coordinated. Right and left coronary arteries from the ascending aorta supply heart muscle with freshly oxygenated blood. The inherent rhythmicity of cardiac muscle is modulated by the autonomic innervation of the heart, amongst other things.
You should:
• describe the arrangement of the pericardium around the heart, and the importance of cardiac tamponade
• list the surface markings of the heart and its borders as seen on a posteroanterior chest radiograph
• describe the route taken by blood as it passes through the chambers and valves of the heart, and know how to perform external cardiac massage
• list the position, surface anatomy and importance of the cardiac valves
• describe the disposition and importance of the conducting system
• describe the anatomy of the right, left, circumflex, anterior interventricular and posterior interventricular coronary arteries
• describe where to place your stethoscope in order to listen to the various elements of cardiac function.
Pericardium
Serous pericardium (Fig. 10.15)
Fibrous pericardium (Fig. 10.15)
The serous pericardium, and the heart inside it, are then enclosed in a sac of tough fibrous tissue, the fibrous pericardium. It is simply like a plastic bag closed round the ‘neck’ of the heart (the great vessels) and is firmly attached to the underlying parietal layer of serous pericardium.
So, there are two types of pericardium, fibrous and serous, and there are two layers of serous pericardium. Note that it is the serous pericardium that is equivalent to the pleura. As in the pleural cavity, the pericardial cavity is only a potential cavity: it contains a minute amount of pericardial fluid and is there to facilitate gliding movements such as occur during the beating of the heart, but it does not allow separation of the two layers of serous pericardium.
Pericardial cavity and sinuses
The cardiac equivalent of the hilum of the lung, that is the place where structures pass between the heart and the rest of the mediastinum, is not as ‘tidy’ as the pulmonary hilum. The embryology of the great arteries (aorta, pulmonary) and veins (inferior vena cava, superior vena cava and pulmonary veins) results in the area posterior to the heart being complex.
• That part of the pericardial cavity behind the heart is the oblique sinus separating the left atrium (the original left side of the heart is now at the back) from the oesophagus.
• The transverse sinus is the potential communication between the right and left sides of the pericardial cavity found behind the great arteries (ascending aorta, pulmonary artery) and in front of the superior vena cava.
Cardiac tamponade
It is important to realise that the fibrous pericardium is indeed fibrous and not elastic. If fluid were to collect in the pericardial cavity, the pericardial covering would not be able to expand to accommodate it and the beating of the heart would become increasingly compromised. This is cardiac tamponade – a potentially fatal emergency. It may arise from pericarditis (inflammatory fluid in the pericardial cavity) or from rupture of one of the coronary vessels or even of the heart wall itself, resulting in blood in the pericardial cavity (haemopericardium).
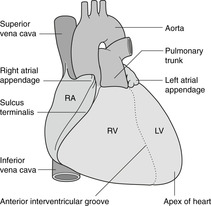
Heart
Surfaces and borders
The heart develops as a midline structure. It subsequently shifts so that the left side becomes posterior and the right side anterior. Despite this, the terms left and right are used and you might bear in mind that right can often, but not always, be translated as anterior, and left as posterior.
Surfaces of the heart
The most superior aspect of the heart is the area of origin of the great vessels. The term ‘base’ of the heart is used differently by different groups of people – there are three usages – and so is best avoided altogether.
Borders of the heart (Fig. 10.16)
• Right.
• Inferior or diaphragmatic, at the left extremity of which is the apex, so called for obvious reasons.
• Left, which slopes upwards and medially from apex towards root of great vessels.
Chambers of the heart, septum, conducting system
The heart has four chambers: right and left atria and right and left ventricles. The atria receive blood from veins and have little work to do, so their walls are thin. The right ventricle must contract with sufficient force to propel blood through the lungs and back to the heart, and its walls are significantly thicker than atrial walls. The left ventricle must propel blood throughout the body, and so its walls are much thicker again. The tissue separating the two atria is the atrial (or interatrial) septum, and that separating the two ventricles is the ventricular (or interventricular) septum.
Atria and ventricles are separated by a fibrous skeleton that provides a structural framework for the atrioventricular valves and an anchoring apparatus for contracting ventricular muscle. It is important in the electrical isolation of the ventricles from the atria and it is marked on the external aspect of the heart by the atrioventricular sulcus.
Atria
The left atrium receives blood from the lungs and the right from the rest of the body. Part of each atrial wall is rough owing to the pectinate muscles, and part is smooth. The rough-walled part includes the atrial appendage. Other terms that you may hear used are:
• atrium = auricle
• atrial appendage = auricle = auricular appendage.
The term auricle is ambiguous: do not use it.
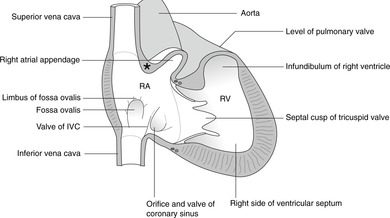
Right atrium, fossa ovalis (Fig. 10.17)
This forms the right heart border. It receives blood from the superior vena cava (SVC) and inferior vena cava (IVC) and may be thought of as being stretched vertically between the two venae cavae. It also receives most of the venous blood from the heart muscle itself through the coronary sinus, the opening of which is adjacent to that of the IVC. The smooth-walled part, which receives the venae cavae, and the rough-walled part are separated by the sulcus terminalis externally (crista terminalis internally).
At the lower end of the crista (internally) are two folds: the ‘valves’ (non-functional) of the IVC and the coronary sinus which guard the orifices of these vessels. The valve of the IVC is continuous superiorly with the limbus (edge) of the fossa ovalis, a crescentic ridge on the atrial septum marking the site of the prenatal foramen ovale by which means blood passed from right to left atria, bypassing the non-functional lungs. The thicker part of the atrial septum, which ends inferiorly in the limbus of the fossa ovalis, is formed from embryological septum secundum; the thinner part in the floor of the fossa is from septum primum. The two septa normally unite, but they may remain separate forming a probe-patent (that is, a probe may be inserted) foramen ovale. This is not normally a problem because the higher venous pressure in the left atrium normally pushes over the thinner septum primum on the left so that it remains in contact with the thicker septum secundum.
The crista terminalis marks the junction between the two embryological parts of the right atrium. Since the smooth-walled portion is from the sinus venosus (receiving SVC, IVC, coronary sinus) and the rough-walled part is from the primitive atrium, the crista marks the sinuatrial (or sinoatrial, SA) junction. At its upper end, just to the left of the entry of the SVC, is the sinuatrial node or cardiac pacemaker. Despite the importance of the SA node, there is nothing to see with the naked eye.
The outflow valve of the right atrium is the tricuspid (see later).
Left atrium (Fig. 10.15)
This is at the back of the heart and receives blood from the pulmonary veins (usually two right, two left). It may be thought of as being stretched from side to side between the right and left pulmonary veins. Behind the left atrium is the oesophagus, and an enlarged left atrium may result in a narrowing of the lower part of the thoracic oesophagus visible on a barium swallow investigation. The left atrial appendage may be apparent on the left heart border between the left ventricle (below) and the pulmonary artery (above). The smooth-walled part of the atrium is derived from incorporation of pulmonary veins and the rough-walled part from the primitive cardiac atrium. The outflow valve of the left atrium is the mitral (see later).
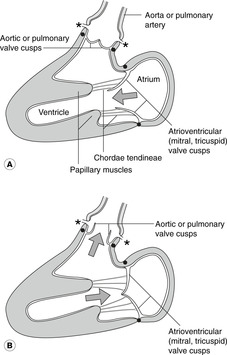
Ventricles
These are the chambers that do the work: they have thick muscular walls. In the fetus both ventricles share the work more or less equally and their walls are of equal thickness, but after birth the left ventricular walls, which propel blood round the body (as opposed to simply having to propel it through the lungs) become and remain much thicker. In both ventricles the internal surface has many fleshy trabeculations (ridges) and papillary muscles like stalagmites projecting into the ventricular lumen. Attached to the end of the papillary muscles are chordae tendineae – thin fibrous cords attached to the ventricular aspect of the atrioventricular valves. These are important during systole in preventing ‘blowback’ of the atrioventricular valves.
Right ventricle
The only noteworthy feature is the septomarginal (moderator) band that contains the right bundle of the conducting system. The outflow valve is the pulmonary valve, and the part of the ventricle immediately beneath it is the conus arteriosus or infundibulum.
Left ventricle
There is nothing noteworthy about the interior of this chamber. The outflow valve is the aortic.
Ventricular septum
Most of this is thick and highly muscular as befits part of the wall of the left ventricle, but near the atrioventricular junction, part is membranous (pars membranacea), in effect a continuation of the atrial septum. If during development the membranous portion and the muscular portion fail to fuse, a ventricular septal defect results. Neural crest cells contribute to the membranous portion of the septum, and ventricular septal defects may be associated with other anomalies of neural crest origin.
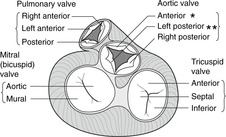
Valves
In the order in which blood flows through the heart, the valves are: tricuspid, pulmonary (lungs), mitral, aortic. The positions of the valves in diastole and systole are shown in Fig. 10.18. The mitral valve has two large cusps and the other valves each have three (Fig. 10.19). You should know the cusps of the aortic valve because of their relationship to the origin of the coronary arteries.
Cusps of the aortic valve and the coronary arteries (Figs 10.18, 10.19)
• The right coronary artery arises from the dilatation of the aorta immediately above the anterior cusp of the aortic valve. This dilatation is the anterior aortic sinus. The anterior cusp and anterior sinus are sometimes known as the right cusp and sinus because of the origin of the right coronary artery, but this ignores their actual position in the chest.
• The left coronary artery arises from the left posterior aortic sinus immediately above the left posterior cusp of the aortic valve. Both cusp and sinus are sometimes known as left cusp and left sinus because of the origin of the left coronary artery, but again this ignores their actual position.
• The right posterior aortic cusp and sinus are not associated with a coronary artery, and so may be referred to as the non-coronary cusp and sinus.
Valve disease
Valve disease is generally of two types: stenosis and incompetence. In stenosis the valves do not open fully, and in incompetence they do not shut properly. One cause of incompetence of the atrioventricular valves you have already met is rupture of the chordae tendineae. Symptoms and signs will vary depending upon which valve is involved.
In stenosis there will be turbulent flow as blood is squeezed as if through a nozzle. This will lead to an audible murmur which will occur in systole if the aortic or pulmonary valve is involved (since blood flows through these during systole) or in diastole if the mitral or tricuspid is involved.
In mitral or tricuspid incompetence, blood will flow back into the atria, leading to a systolic murmur. In mitral incompetence the volume of blood gushing back into the left atrium with each left ventricular contraction will cause significant dilatation of the atrium. This may lead to a sensation of discomfort from pressure on the oesophagus. In aortic or pulmonary incompetence, blood will flow back into the ventricles during diastole, leading to a diastolic murmur. Combinations of sounds and symptoms can be used to diagnose the problem although, in truth, modern diagnostic methods involving ultrasound and pressure transducers are (regrettably) rendering this kind of intellectual detective work redundant.
Conducting system and fibrous skeleton
The pacemaker is the SA node in the wall of the right atrium at the top of the crista terminalis. From the SA node the impulse passes to the atrioventricular (AV) node in the lower end of the atrial septum beside the coronary sinus opening. There are probably several distinct routes along which impulses pass in the atrial wall, although they are not histologically distinct. From the AV node specialised cardiac muscle fibres, Purkinje fibres, form the bundle of His. This penetrates the fibrous skeleton that separates the atria from the ventricles, and it passes into the ventricular septum (ventricular septal defects may interfere with it, leading to cardiac dysrhythmias). About half way down the septum it divides into right and left branches. The left bundle passes to the apex and up the left side of the heart. The right bundle crosses to the inferior (embryonic right) side of the ventricle in the septomarginal (moderator) band, an identifiable ridge in the wall of the right ventricle.
Why do ventricles have bundles when atria do not?
Simply because ventricular contraction needs to be coordinated in a specific manner to give rise to the ‘wringing’ action of ventricular contraction. Should the right and left bundles function imperfectly (e.g. in right and/or left bundle branch block), then ventricular function is impaired. The action of the ventricular muscle requires that some structure in the heart will provide a measure of rigidity that is lacking in the atria. This is the fibrous skeleton referred to earlier in which are embedded the AV valves. It has another very important function. Being fibrous, it is impervious to the electrical impulse and so isolates electrically the atria from the ventricles, except where the bundle of His penetrates it. This isolation is very important: were it not so, and electrical impulses could spread unchecked from atria to ventricles, ventricular contraction would be entirely uncoordinated. This may in fact happen if the fibrous skeleton is damaged in disease. In this circumstance, the electrical impulse may pass as normal from atria to ventricles in the bundle of His but then return to the atria through the ‘electrical opening’ in the fibrous skeleton produced by disease, thus setting up extrasystoles in the atria. These may then travel back into the ventricles, completely disrupting the normal rhythm. These, for obvious reasons, are called re-entry phenomena.
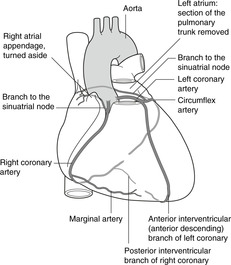
Coronary arteries (Fig. 10.20)
Heart muscle requires an extensive supply of freshly oxygenated blood. This is provided by the right and left coronary arteries arising from the aorta immediately above the aortic valve.
• The right coronary artery arises from the anterior aortic sinus (slight dilatation) above the anterior cusp of the aortic valve. It passes inferiorly in the anterior AV groove and gives off the marginal branch as it approaches the diaphragmatic (inferior) surface of the heart. The main trunk passes under the heart on the diaphragmatic surface and then turns to the left, running in the posterior interventricular groove towards the apex as the posterior interventricular artery. Branches of the right coronary artery supply both atria, most of the right ventricle, the posterior part of the ventricular septum and the posterior part of the left ventricle, and usually there is a branch to the SA (pacemaker) node.
• The left coronary artery arises from the left posterior aortic sinus above the left posterior cusp of the aortic valve. It passes forwards behind the origin of the pulmonary trunk for about 2cm and then divides into the circumflex and anterior interventricular arteries. The circumflex passes posteriorly in the AV groove behind the heart to anastomose with branches of the right coronary artery. The anterior interventricular artery passes down on the anterior aspect of the heart to the apex. Its alternative name, therefore, much used by clinicians, is the left anterior descending artery. Branches of the left coronary supply both atria, the anterior part of the left ventricle, the anterior ventricular septum and some adjacent right ventricle.
There are extensive anastomoses between the territories of the two arteries and variations are common. For example, the posterior interventricular artery may be a continuation of the circumflex (thus from the left coronary) rather than of the right coronary artery.
Coronary vessels fill during diastole. A little thought will confirm that when the cusps of the aortic valve are open during systole, blood can not enter the coronary vessels, and it is propelled quickly past their openings by the force of ventricular contraction. During diastole with the cusps of the aortic valve in the closed position, the elastic recoil of the aortic wall provides helpful propulsion forcing blood from the aortic sinuses into the coronary vessels. Blood flow through coronary vessels is maximal during diastole: obviously, when heart muscle is contracting, coronary vessels are narrowed and blood flow impeded. Here is another good reason why the openings of the coronary vessels should be outside, rather than in, the myocardium.
Cardiac veins (Fig. 10.21)
A knowledge of these is less important. Most veins are tributaries of the coronary sinus so most venous blood drains into the right atrium through the coronary sinus, but veins from the anterior wall of the heart drain directly into the right atrium. Many small veins in the myocardium open directly into all chambers of the heart (Thebesian veins).
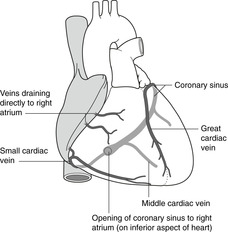 |
| Fig. 10.21 |
Cardiac autonomic innervation
• Sympathetic: cardiac branches of the sympathetic chain arise from the cervical and thoracic regions of the sympathetic chain on both sides. Sympathetic stimulation results in tachycardia (increase in heart rate) and increased contractility.
What does the autonomic supply to the heart actually do?
At heart transplant operations, you can be sure that the surgeon makes no effort to reconnect sympathetic or parasympathetic connections. However, the heart usually works well enough (given that it is not rejected). You might then wonder about the importance of what physiology textbooks tell you. Heart muscle possesses inherent rhythmicity: its innervation merely modulates this.
Surface markings of the heart (Fig. 10.22)
These are very important: they form the basis of the clinical examination of the heart. Here is a fairly reliable scheme: 2 × 3 = 6:
(a) second intercostal space near the left sternal edge
(b) third intercostal space near the right sternal edge
(c) sixth intercostal space at the right sternal edge
(d) fifth intercostal space in the midclavicular line (the apex).
Back to (a).
Position of the heart valves (Fig. 10.22)
All the heart valves are retrosternal. The highest is the pulmonary at about the level of the third costal cartilage, then the aortic at the third space, then the mitral at the fourth costal cartilage, and finally the tricuspid at the fourth space. This may be conveniently remembered as PAMT 3344 – but remember, all retrosternal, close to the midline.
Coronary artery bypass graft (CABG)
Heart disease is sometimes caused by narrowing or blockage of coronary arteries. Once located, the areas of narrowing can be bypassed by grafting material from elsewhere to form a replacement segment of artery. A section of great saphenous vein from the lower limb is sometimes used (but remember to orient it so that the valves in the vein allow blood to flow in the required direction). There is another option for the anterior interventricular (anterior descending) artery. This vessel runs more or less parallel to, and not far distant from, the left internal thoracic artery, which may be anastomosed to it.
Cardiac pain
Visceral sensory fibres pass back to the central nervous system in sympathetic nerves. They enter the spinal cord in lower cervical and upper thoracic spinal nerves and so (see Referred pain, p. 38) it is not surprising that cardiac pain is felt in the dermatomes of these segments: upper chest, upper limb, possibly neck. But it is not easy to explain why, given that the heart is a midline structure and (presumably) innervated equally by nerves from both sides, cardiac pain should be predominantly left sided.
Apex beat (Fig. 10.22)
The apex beat is the most inferolateral point on the chest wall at which the heartbeat may be palpated. Should it be found other than in the normal position of the apex (see above), then you may assume that the heart is either enlarged or displaced. This may not necessarily indicate disease: for example, an athlete may have an enlarged heart.
Listening to (auscultating) the heart valves (Fig. 10.22)
Blood passing through the valves transmits the sounds away from the valves themselves, and this means that the valves are best heard at places other than their surface markings (Table 10.3).
| Valve | Position | Best heard |
|---|---|---|
| Pulmonary | Retrosternal, level of 3rd rib | 2nd space just to left of sternal edge |
| Aortic | Retrosternal, level of 3rd space | 2nd space just to right of sternal edge |
| Mitral | Retrosternal, level of 4th rib | Apex (5th space, midclavicular line) |
| Tricuspid | Retrosternal, level of 4th space | Lower sternal edge, side depending upon the condition |
External cardiac massage
The object of external cardiac massage as used in cardiopulmonary resuscitation is to empty the blood from the ventricles by compressing the heart between the sternum and the spinal column (see Fig. 10.15). The compression of the chest also forces blood from the lung capillaries through the heart into the aorta. It is attempted by laying the patient on his back on a hard surface, and vigorously compressing the lower sternum at the rate of 80–100 per minute with sufficient force to produce pulsations in the carotid and femoral arteries. This force may fracture ribs, but being alive with fractured ribs is probably better than being dead with intact ones.
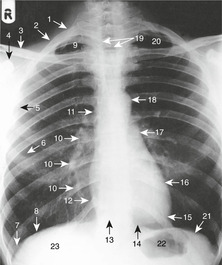
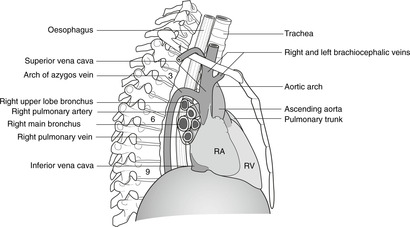
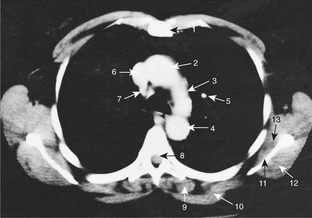
Radiology of the heart (Fig. 10.10)
PA view, inspection of the cardiac outline
Right border, from above down:
• right brachiocephalic vein
• SVC
• right atrium.
Diaphragmatic surface, right to left:
• right ventricle
• very small portion of left ventricle
• apex.
Left border, from apex up:
• left ventricle
• (left atrial appendage, sometimes)
• pulmonary artery
• aortic knuckle (junction of aortic arch with descending aorta).
10.4. Mediastinum
The mediastinum is the area between the two pleural cavities. It is divided into the superior mediastinum above vertebral level T4 and, below this, the anterior mediastinum (in front of the pericardial cavity), middle mediastinum (pericardial cavity and contents) and posterior mediastinum (behind the pericardial cavity). The organs of significance are the oesophagus, trachea, great arteries and veins, thoracic duct, vagus nerve, phrenic nerve and sympathetic chain. The arch of the aorta gives rise to the great arteries supplying the head, neck and upper limbs. The tributaries of the superior vena cava are important clinical access routes. The trachea, oesophagus and vagus and phrenic nerves are closely interrelated and may be affected in malignant tumours of the lung. The sympathetic chains are found in the superior and posterior divisions of the mediastinum, and give rise to the cardiac branches and splanchnic nerves supplying thoracoabdominal viscera.
You should:
• describe the subdivisions and contents of the mediastinum
• describe the disposition of the great arteries and veins and their principal branches and tributaries
• describe the anatomy of insertion of catheters, etc. into the right brachiocephalic vein
• describe the formation, course and functions of the phrenic nerves
• describe the formation, course and functions of the vagus nerves and branches
• explain how thoracic disease may give rise to signs and symptoms in the head, neck and upper limb
• describe the basic anatomy of the sympathetic nervous system in the thorax.
Parts of the mediastinum
The mediastinum is divided horizontally by the plane from the sternal angle (of Louis) to vertebra T4 into:
• the inferior mediastinum below this plane, which is itself divided into:
– anterior mediastinum: anterior to the heart and pericardium
– middle mediastinum: the heart and pericardium
– posterior mediastinum: behind the heart and pericardium, containing the oesophagus, trachea, vagus and phrenic nerves, thoracic duct, and sympathetic chain.
There is nothing in the anterior mediastinum worthy of attention other than the thymus gland extending down from the superior mediastinum, and the internal thoracic vessels. Having considered the heart, only the superior and posterior compartments remain to be considered in any detail.
Thymus gland
This is found in children anterior to the trachea, extending from the level of the cricoid cartilage (vertebral level C6) down to the retrosternal area. Thymic tumours may compress the tributaries of the superior vena cava leading to venous engorgement in the neck. During childhood the thymus gradually regresses so that in the adult thymic tissue is more or less confined to the retrosternal connective tissue.
Great arteries
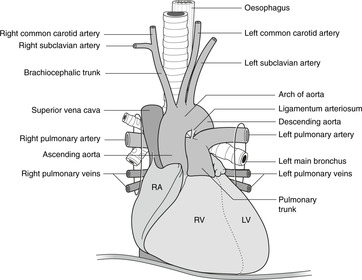
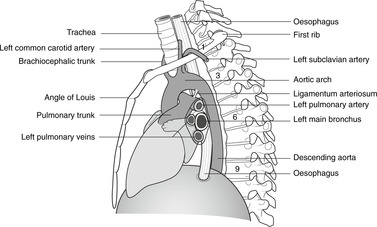
Ascending aorta, pulmonary trunk, arch of the aorta (Figs 10.23, 10.24)
The aorta is divided into three parts: ascending, arch, and descending. At its origin the aorta is behind the pulmonary trunk, but as they ascend they spiral round each other: the pulmonary trunk passes to the left of the aorta, bifurcating behind it into the right and left pulmonary arteries which pass to the pulmonary hila. The ascending aorta and the pulmonary trunk arise from a single embryonic artery, the truncus arteriosus, which is divided into two vessels by the growth of a spiral septum. This accounts both for the spiral arrangement and the fact that they are inseparable.
 |
| Fig. 10.24 |
The aorta then arches posteriorly and to the left, over the bifurcation of the pulmonary trunk and the left main bronchus, to the posterior mediastinum where it descends on the left of the midline towards the diaphragm. It leaves the thorax, passing behind the diaphragm, at vertebral level T12.
Branches of the ascending aorta and aortic arch are, in order:
• coronary vessels
• brachiocephalic artery, which gives rise to the right common carotid and right subclavian
• left common carotid
• left subclavian.
Branches of the descending aorta are the posterior intercostal arteries from the third onwards (the first two are branches of the costocervical trunk).
Brachiocephalic and subclavian arteries
The asymmetric origins of these arteries is readily explained embryologically and you should bear in mind that anomalies in these arrangements may arise. For example, the right subclavian artery may arise independently from the aorta on the left of the midline, and as it passes to the right it may compress the oesophagus, passing either in front of or behind it, causing dysphagia (discomfort on swallowing or an uncomfortable feeling of oesophageal obstruction).
From its origin on each side, the subclavian artery passes laterally, grooving the superior surface of the first rib behind the scalene tubercle (the attachment of scalenus anterior muscle), to reach the lateral border of the first rib where it becomes the axillary artery.
The subclavian artery is divided into three parts for descriptive purposes: first part medial to the scalenus anterior, second part behind the muscle, and third part between the muscle and the first rib.
Branches of the first part are important:
• the vertebral artery
• the internal thoracic artery
• the thyrocervical trunk.
Branches of the second and third parts are unimportant: they supply the top of the rib cage and scapular region, and one of them, the costocervical trunk, gives rise to the first one or two posterior intercostal arteries.
Internal thoracic artery
From its origin from the first part of the subclavian artery, this descends on the internal aspect of the rib cage, just lateral to the sternal edge.
• It gives rise to the anterior intercostal arteries, branches to the medial portion of the breast, and the pericardiophrenic artery that accompanies the phrenic nerve as it runs on the pericardium.
• It terminates by dividing into:
– superior epigastric artery: continues down to the anterior abdominal wall and anastomoses with the inferior epigastric artery
– musculophrenic artery: runs laterally in the angle formed between the trunk wall and the diaphragm, giving branches to both.
These arteries are accompanied by veins draining into the brachiocephalic veins.
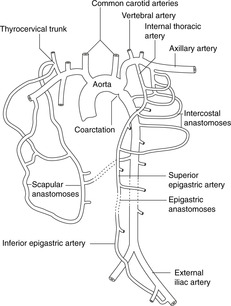
Bypassing a blocked aorta (Fig. 10.25)
In a blockage of the descending aorta, such as a coarctation (narrowing), blood may bypass the blockage as follows:
• Ascending aorta–subclavian arteries–internal thoracic arteries–superior epigastric arteries–inferior epigastric arteries (retrograde flow)–femoral arteries, thence down to the lower limb and up (retrograde) to the iliac arteries and abdominal aorta. In this case the internal thoracic arteries will be much enlarged.
• Ascending aorta–subclavian arteries–scapular anastomosis–posterior intercostal arteries (retrograde flow)–descending aorta. In this case the intercostal arteries will be much enlarged leading to deepening of the costal grooves in which the arteries run. This may be evident on a chest radiograph as ‘notching of the ribs’.
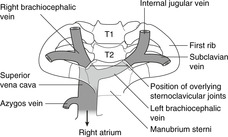
Great veins (Fig. 10.26, Fig. 10.27 and Fig. 10.28)
Superior vena cava
 |
| Fig. 10.26 |
 |
| Fig. 10.28 |
The SVC has three tributaries: the right and left brachiocephalic veins and the azygos vein.
Brachiocephalic veins
The brachiocephalic veins are formed by the junction of the internal jugular and subclavian veins immediately posterior to the sternoclavicular joints (vertebral level about T2): this is an important surface marking. The left brachiocephalic vein crosses the midline to join the right, forming the SVC just behind the right sternal edge at the angle of Louis (vertebral level T4). The SVC receives the azygos vein and drains into the smooth-walled part of the right atrium deep to the right third costal cartilage.
Insertion of catheters and central lines, mediastinoscopy
There is almost a straight line from the formation of the right brachiocephalic vein behind the right sternoclavicular joint to the right atrium and beyond into the IVC. Catheters and central lines can be inserted into the venous system either directly into the formation of the right brachiocephalic vein from above (between the two heads of sternocleidomastoid) or through the right subclavian vein, a little more laterally.
The subclavian and brachiocephalic veins are anterior to the arteries. To all intents and purposes they are directly behind the sternum and are therefore in danger in mediastinoscopy when a scope is inserted in the suprasternal notch.
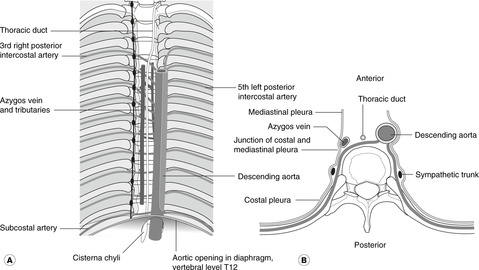
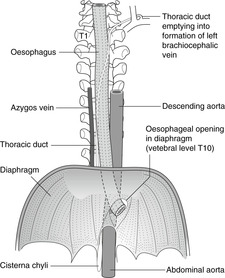
Azygos venous system and intercostal veins
The azygos vein receives blood from the posterior intercostal veins and from the segmental veins of the abdomen (connecting veins from the abdomen ascend behind the diaphragm). Veins on the right drain directly into the azygos vein but on the left side the pattern is variable: all you need to know is that segmental veins in the thorax and upper abdomen drain into the azygos system of veins, which ultimately empty into the SVC.
The termination of the azygos vein arches over the hilum of the right lung, on which there is an azygos impression, and the azygos vein enters the SVC about 2cm above the right atrium.
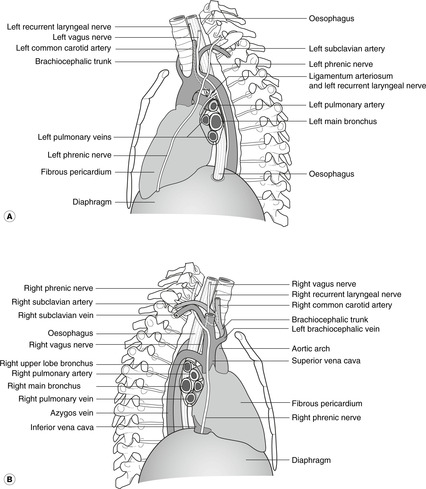
Superior intercostal veins
Since the azygos vein is found no higher than about vertebral level T4, the first one or two posterior intercostal veins on each side unite to form a superior intercostal vein that drains into the brachiocephalic veins. The left superior intercostal vein is important to thoracic surgeons since it is vulnerable as it crosses the arch of the aorta between the phrenic and vagus nerves (Fig. 10.28).
Nerves in the mediastinum (Fig. 10.29)
The phrenic and vagus nerves pass down from the neck. The phrenic descends on the pericardium to the diaphragm, so remaining anterior in the chest, and the vagus descends to form a plexus around the oesophagus, so being closer to the vertebral column. The sympathetic chain is found on the internal aspect of the ribs close to the vertebral column. It is intimately related to the intercostal neurovascular bundle and has connections (rami communicantes) with intercostal nerves. Also in this region are branches of the sympathetic chain, the splanchnic nerves, which pass medially and descend towards the diaphragm on their way to the abdomen. For more detailed consideration of the autonomic nervous system in the thorax, see later (p. 93).
Phrenic nerve
This arises from the ventral rami of segmental nerves C3, 4 and 5 and passes down the neck on the anterior aspect of scalenus anterior muscle. At the first rib, the nerve passes medially, between the subclavian vein (anterior) and the subclavian artery (posterior), just lateral to the origin of the thyrocervical trunk. The asymmetrical arrangement of the great vessels in this region means that from this point, the right and left sides must be considered separately.
• The right phrenic runs on the right wall of the SVC and directly to the right side of the fibrous pericardium. It passes directly down on the pericardium over the right atrium to the diaphragm near the orifice for the IVC.
• The left phrenic, having passed deep to the formation of the left brachiocephalic vein, passes over the left side of the arch of the aorta and the pulmonary trunk before descending on the pericardium over the left ventricle to the diaphragm near the cardiac apex.
The phrenic nerves innervate mediastinal pleura (sensory), pericardium (sensory) and diaphragm (motor to the entire diaphragm, sensory from the central tendon region).
Vagus and recurrent laryngeal nerves in the thorax
The vagus on each side enters the thorax from the carotid sheath in the neck, between the common carotid artery (medially) and the internal jugular vein (laterally). Again, the asymmetry of the great vessels requires that the two sides be considered separately.
• The left vagus remains on the lateral wall of the common carotid artery all the way to the aortic arch. It passes between the descending aorta and the left pulmonary artery and then forms the oesophageal plexus with its fellow of the other side. As it crosses the arch of the aorta it gives the left recurrent laryngeal nerve which passes medially, below the ligamentum arteriosum, before going back up (recurring) to the larynx.
The origin of the left recurrent laryngeal nerve is thus about two vertebral levels lower than the origin of the right. The reasons for this are easily understood. The recurrent laryngeal nerves innervate muscles of the sixth branchial arch (laryngeal muscles). They are intimately related to the sixth branchial arch arteries and when both of these arteries are present in the embryo, the arrangement of the recurrent laryngeal nerves is symmetrical. However, during subsequent development, the right sixth arch artery degenerates, thus allowing the right sixth arch nerve to take a shorter course to its destination, so on the right the nerve is held down by the next most cranial branchial arch artery, the fourth (there being no fifth) which becomes the subclavian. On the left, the sixth arch artery persists as the pulmonary artery and the ductus arteriosus, and since after birth the ductus becomes the ligamentum, this continues to pin down the left recurrent laryngeal nerve.
The recurrent laryngeal nerves may be involved in lung tumours, resulting in voice changes. Indeed, hoarseness of the voice thus caused may be a presenting sign of a lung tumour. This is more common as a result of a left-sided lesion than a right-sided lesion since there is more scope for lung disease to affect the left recurrent laryngeal nerve, the thoracic course of the nerve being longer on the left than the right.
Having formed the oesophageal plexus, the vagus nerves continue through the oesophageal opening in the diaphragm (vertebral level T10) into the abdomen as the anterior and posterior vagal trunks. The vagus nerve transmits parasympathetic and visceral sensory fibres to and from the heart (cardiac branches), the lungs, the oesophagus and abdominal organs.
Intercostal nerves (see p. 70; Fig. 10.8)
These lie immediately under the mediastinal pleura between the vertebral column and the point at which they enter the costal groove with the posterior intercostal arteries and veins. The intercostal nerves are connected to the sympathetic chains by means of grey and white rami communicantes.
Intercostal nerves carry:
• motor fibres to intercostal muscles and (in the case of lower intercostal nerves) muscles of the abdominal wall
• sensory fibres from skin, muscle spindles, parietal pleura and (in the case of lower intercostal nerves) parietal peritoneum
• postganglionic sympathetic fibres to blood vessels and sweat glands in the territory of the nerve.
Structures related to the neck of the first rib, Pancoast’s tumour
A tumour of the apex of the lung may present with symptoms arising from damage by the tumour to nerves related to the neck of the first rib. These are:
• fibres of T1 nerve which contribute to the brachial plexus to supply the upper limb; involvement of these may mean that the small muscles of the hand are weakened or paralysed, leading to clumsiness and a loss of manual dexterity
• the sympathetic chain; involvement of this may interrupt efferent sympathetic impulses to the head and this would result in Horner’s syndrome:
– pupilloconstriction because of unopposed parasympathetic action
– facial anhidrosis because of denervation of sweat glands
– ipsilateral ptosis (drooping of the upper eyelid) because of partial denervation of levator palpebrae superioris muscle.
Such a tumour was described by Professor H.K. Pancoast and is now commonly known as Pancoast’s tumour.
Posterior mediastinum (Fig. 10.30, Fig. 10.31 and Fig. 10.32)
Trachea and oesophagus
The trachea and oesophagus descend in the midline of the superior mediastinum, parting company at the bifurcation of the trachea at about vertebral level T4 (surface marking: sternal angle). At the tracheal bifurcation, the oesophagus is slightly to the left of the trachea and the left main bronchus crosses anterior to it, giving rise to a slight indentation of the anterior wall of the oesophagus. The oesophagus descends to penetrate the diaphragm at vertebral level T10.
 |
| Fig. 10.30 |
The lower portion of the oesophagus in the thorax is the site of anastomosis between systemic venous drainage (to the azygos system) and portal venous drainage (to the liver). It is here that in liver disease these anastomoses may enlarge to provide a roundabout route for venous blood to bypass the liver. These may have important clinical effects (see section 11.7, p. 129).
Although the oesophagus meets the diaphragm slightly to the left of the midline, the muscle fibres that surround it arise from the right diaphragmatic crus. These form the gastro-oesophageal sphincter. This may be the site of a hiatus hernia (see Ch. 11, p. 118).
Thoracic duct
This is the main lymphatic channel receiving lymph from the entire body apart from the right arm, right side of the head and neck and right upper thorax. The thoracic duct, or the upper part of the cisterna chyli in the abdomen from which it extends, enters the thorax from below by passing behind the diaphragm with the aorta. It ascends anterior to the azygos system of veins, gradually crosses to the left and at the root of the neck drains into the superior aspect of the junction of the internal jugular and subclavian veins. Abdominal malignancy may give rise to enlarged left supraclavicular lymph nodes (Virchow’s node – see Ch. 11, p. 126).
Diaphragmatic orifices
| T8 | IVC, branches of right phrenic nerve. Note that this orifice is in the central tendon, not a muscular portion, and so the IVC is not compressed with each muscular contraction. |
| T10 | Oesophagus, vagus nerves. |
| T12 | Aorta, tributaries of the azygos venous system, thoracic duct. |
The sympathetic chains and splanchnic nerves penetrate the diaphragm independently: you do not need to know the details.
More details of the diaphragm are given with the posterior abdominal wall, from which it arises.
Autonomic nervous system in the thorax
Thoracic sympathetic chain (trunk) and its connections
First, read Chapter 6 again.
The thoracic portion of the sympathetic chain (trunk) on each side runs from the neck of the first rib superiorly to the side of vertebra T12 inferiorly. It continues up into the neck behind the carotid sheath and down into the abdomen. It lies between the intercostal nerves and the parietal pleura. A sympathetic ganglion is present at each segment, grey and white rami communicantes connecting each ganglion to its intercostal nerve. Arising from the ganglia and passing medially and towards the midline are the greater, lesser and least splanchnic nerves. These nerves convey impulses between the sympathetic chains and the abdominal sympathetic plexuses. These will be considered in more detail in Chapter 11 (Autonomic nervous system in the abdomen and pelvis, p. 151).
Sympathetic impulses to heart and lungs
Preganglionic sympathetic impulses to the heart and lungs originate in the lateral grey horns of upper thoracic spinal cord segments. Axons of these neurons pass in the ventral roots of upper thoracic spinal nerves to the spinal nerves themselves and thence through white rami communicantes to the sympathetic chain where some of them ascend to the lowest of the cervical ganglia of the sympathetic chain, the inferior cervical ganglion. From here, and from the upper few thoracic ganglia, they continue into cardiac and pulmonary branches: in effect the cervical and thoracic splanchnic nerves (although they are not called this). These pass to intercommunicating sympathetic plexuses on and around the great vessels and the bifurcation of the trachea – the cardiac and pulmonary plexuses. The precise location of synapses, whether in the sympathetic chain, in the cardiac plexus, or somewhere between, has not been fully elucidated. Postganglionic fibres pass directly to the heart and lungs.
Parasympathetic impulses to heart
Preganglionic parasympathetic fibres originate from the brain and are conveyed in the vagus (tenth cranial) nerve. They leave the vagus nerve in the neck and travel down as cardiac branches of the vagus to contribute to the cardiac and pulmonary plexuses before reaching the heart. Synapses are generally found in the wall of the destination organ: postganglionic parasympathetic fibres are very short.
Important vertebral levels in the mediastinum
| T2 | Suprasternal (jugular) notch, formation of brachiocephalic veins, highest point of arch of aorta. |
| T3 | Junction of brachiocephalic veins to form SVC. |
| T4 | Sternal angle (of Louis), bifurcation of trachea, aortic impression on oesophagus. |
| T5 | (about) Left main bronchus impression on oesophagus. |
| T8 | IVC passes through diaphragm. |
| T10 | Oesophagus passes through diaphragm. |
| T12 | Aorta, thoracic duct and azygos system pass behind diaphragm. |
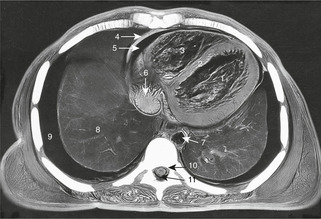
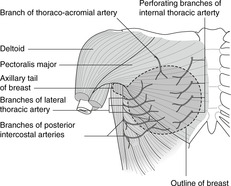
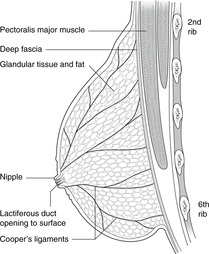
10.5. Breast (Fig. 10.33, Fig. 10.34 and Fig. 10.35)
The postpubertal female breast is composed of 15–20 independent exocrine secretory units opening around the nipple. It overlies ribs 2–6. It is part of the superficial layer of the chest wall and should not be firmly tethered to underlying muscle. Its arterial supply comes from branches of the subclavian and axillary arteries, and its lymph drains principally to the axilla. Accessory breast tissue may be found in a line from axilla to groin.
 |
| Fig. 10.33 |
 |
| Fig. 10.34 |
 |
| Fig. 10.35 |
Position and structure
The breast (mammary gland) is a group of 15–20 exocrine glands arranged radially around the nipple. These individual units are separated by fibrous septa and the duct of each opens independently. The nipple is surrounded by an area of pigmented skin about 3cm in diameter, the areola. On it are numerous small swellings, Montgomery’s tubercles, which become prominent and reddened in pregnancy but are otherwise of no great clinical significance.
The maximum extent of the breast is roughly circular, overlying ribs 2–6 vertically, and sternal edge to midaxillary line horizontally, but an axillary tail (of Spence) extends upwards and laterally into the axilla. The glandular tissue is confined to the superficial layers of the chest wall, but the axillary tail may penetrate the deep fascia.
The glandular tissue overlies pectoralis major and serratus anterior muscles but, being confined to the superficial fascia, is not attached to these muscles. Any clinical indication of its tethering to these muscles should be treated with the utmost seriousness: it may well be an indication of malignant disease. Asking the patient to raise the arm and observing the way in which the breast moves may reveal tethering. The breast tissue is, however, connected to the overlying skin by fibrous strands, the suspensory ligaments of Cooper. These are more numerous in the upper part of the breast than in the lower. These may become stretched with advancing years and fat deposition.
Arteries and veins (Fig. 10.33)
Arterial blood supply comes mainly from branches of the subclavian artery: the internal thoracic supplies the medial portion, the lateral thoracic the lateral portion. Other arteries that contribute are the thoracoacromial and intercostal arteries 2–5. Venous drainage is by corresponding veins to the subclavian and brachiocephalic veins.
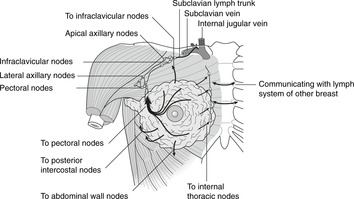
Lymph (Fig. 10.35)
The lymph drainage of the breast is of great importance. It obeys the general rule that lymphatic drainage mirrors arterial supply.
There are two main lymph plexuses in the breast:
• subareolar, immediately under the skin around the nipple
• submammary (or retromammary), between breast and pectoralis major muscle. It is involvement of this that may tether the breast to the muscle.
There are numerous connecting channels running between these two plexuses, each with many tributaries. From these plexuses, lymph drains as follows:
• From the lateral two-thirds: to axillary lymph nodes, thence in lymph vessels alongside the axillary artery to the terminations of the thoracic ducts.
• A small amount of lymph passes to posterior intercostal nodes, and some to nodes of the anterior abdominal wall.
• From the medial portion: to parasternal nodes along the internal thoracic artery, thence up alongside the artery to the terminations of the thoracic ducts. It is possible for lymph from the medial side of one breast to drain to the opposite side, which means that malignant disease of the medial portion of the breast may spread to the other side.
Blockage of lymph channels in the breast (for example by a tumour) can lead to engorgement of the breast tissue by lymph unable to drain away and a particular appearance of the skin of the breast ‘stretched’ over the engorged tissue. This is known as peau d’orange appearance because of its similarity to orange skin with its multiple pits.
Clinical examination of the breast is not complete without palpation of the axilla and the breast of the other side. Axillary lymph nodes are often removed during surgery and this may result in lymph flow from the upper limb being disrupted.
Nerve supply
The skin over the breast is supplied by intercostal nerves T2–6, which also convey postganglionic sympathetic fibres to the vessels within the breast.
Male breast and age changes in the female breast
The male breast and the prepubertal female breast are much the same: the glands are rudimentary. It is possible for carcinoma of the male breast to arise. It is much less common than carcinoma of the female breast, but its survival rate is poorer, probably because the possibility of this condition is overlooked and so by the time the condition has been diagnosed, it will have spread elsewhere.
At puberty in the female, fat deposition takes place together with some proliferation of the secretory units and at lactation there is substantial proliferation of the secretory components. After the menopause, secretory units atrophy and fat deposition continues. Most breast lumps are innocent tumours of fatty tissue: lipomas.
Cooper’s ligaments and disease
Involvement of Cooper’s ligaments in malignant disease may lead to their shortening as they become caught up in the tumour. This can cause dimpling of the overlying skin or even, in extreme cases, inversion of the nipple (but note that inversion of the nipple is by no means always a sign of disease).
Accessory nipples
Breast tissue in other mammals is found along a line extending from axilla to groin, the milk or mammary line. In humans breast tissue is limited to one organ on each side. Nevertheless, accessory nipples, and even accessory breast tissue, are found in both sexes anywhere along the mammary lines, most commonly in the thorax and abdomen. Accessory nipples are harmless but may be confused with a mole or suspected as a melanoma; they were once most definitely life-threatening: the unfortunate possessor was regarded as a witch.
Single best answer questions
For each numbered question, only ONE of the options lettered a–d is correct.
21. The brachiocephalic trunk:
a. gives its terminal branches behind the right sternoclavicular joint.
b. gives the right vertebral artery.
c. is anterior to the brachiocephalic vein.
d. lies on the left side of the trachea.
22. The bifurcation of the trachea is found in or at:
a. sternal angle of Louis.
b. suprasternal notch.
c. vertebral level T2.
d. vertebral level T5.
23. All the following are true of the hilum of the right lung EXCEPT:
a. azygos vein is posterior and superior.
b. bronchi are posterior.
c. phrenic nerve is posterior.
d. pulmonary ligament allows distension of pulmonary veins.
24. The surface marking of the oblique pulmonary fissure runs from the:
a. inferior angle of the scapula to the sixth costal cartilage.
b. spinous process of vertebra T2 or 3 to the sixth costal cartilage.
c. root of the spine of the scapula to the fifth costal cartilage.
d. spinous process of vertebra T2 or 3 to the fourth costal cartilage.
25. Concerning the lungs and pleural cavities:
a. lung tissue normally occupies the costodiaphragmatic recess.
b. the right upper lobe has five bronchopulmonary segments.
c. an inhaled object is more likely to enter the right main bronchus than the left.
d. the pleural cavities do not extend above the clavicles.
26. Concerning the mediastinum:
a. the right main bronchus indents the oesophagus.
b. serous pericardium has visceral and parietal layers.
c. the vagus is the eleventh cranial nerve.
d. the azygos vein empties into the inferior vena cava.
27. Concerning the coronary vessels and conducting system:
a. blockage of a coronary artery may cause referred pain in the neck.
b. the anterior interventricular artery is a branch of the right coronary artery.
c. the coronary sinus runs in the posterior interventricular groove.
d. the moderator band contains the left bundle branch.
28. The anterior interventricular (anterior descending) artery of the heart:
a. is a branch of the left coronary artery.
b. is accompanied by the coronary sinus.
c. supplies both right and left atria.
d. supplies the SA node.
29. The mitral valve:
a. if incompetent, would allow the passage of blood during diastole.
b. is also known as the bicuspid valve.
c. is best heard at the left sternal edge.
d. is the most superior cardiac valve.
Matching item questions
Questions 30–34: coronary vessels
Match the numbered item to the lettered response. Each lettered response may be used once, more than once, or not at all.
a. on the diaphragmatic surface of the heart
b. left coronary artery
d. superior vena cava
e. circumflex artery
30. coronary sinus
31. supplying sinoatrial node
32. above anterior cusp of aortic valve
33. above left posterior cusp of aortic valve
34. marginal artery
Questions 35–39: surface anatomy
Match the numbered item to the lettered response. Each lettered response may be used once, more than once, or not at all.
a. left fifth intercostal space, midaxillary line
b. left fifth intercostal space, midclavicular line
c. retrosternal about level of fourth costal cartilage
d. bifurcation of trachea
e. suprasternal notch
35. position of mitral valve
36. best place to listen to mitral valve
37. normal position of cardiac apex beat
38. vertebral level T4
39. sternal angle of Louis
Questions requiring short answers
40. List the bronchopulmonary segments of the right lung. How do they differ on the left? Which segments are most likely to be affected in a bedridden supine patient who develops pneumonia?
41. Describe or draw:
a. the surface markings of the right lung, and its fissure(s)
b. the surface markings of the heart and the heart valves. Indicate where you would place your stethoscope to listen to these valves.
42. Where might you insert a chest drain? Explain your choice. What would the needle penetrate? What would happen if you inserted a needle into a normal pleural cavity?
43. A 65-year-old man develops cancer of the oesophagus at about vertebral level T4 which invades neighbouring structures. What is at risk? Why might such a patient in the advanced stages of the disease cough up fluid that had been drunk?
44. Describe or draw the arterial supply and venous drainage of the heart.
45. List the chambers and valves of the heart in order as a blood cell makes its way from the superior vena cava to the right subclavian artery. Explain the terms incompetence and stenosis as applied to heart valves.
46. Describe the conducting system of the heart. What is the significance of the fibrous skeleton of the heart in this context?
47. You note on a routine chest radiograph that the ribs have much larger than normal costal grooves. How may this be relevant to a narrowing of the aorta, and which other arterial channels may be enlarged? In such a patient, what would you expect to find when you palpated simultaneously the femoral and radial pulses?
48. A 45-year-old woman tells you she has had a lump in the breast which has been present for several months, is hard and is getting larger. Upon examination you note that the skin over the lump is dimpled and that lymph nodes in the axilla are enlarged. Explain the dimpling, explain the enlarged lymph nodes, state which other lymph nodes might be involved and explain why you wish to know if the breast is fixed to pectoralis major muscle. Add any other information you like.
Self-assessment on Chapter 10: answers
True/false answers
1.
a. True.
b. False. They are normally empty, with diaphragmatic pleura and costal pleura separated only by a thin layer of pleural fluid. Lung tissue may enter the recesses in deep inspiration, but even then it does not completely fill the available ‘space’.
c. True. They are: apical basal, medial basal, anterior basal, lateral basal, and posterior basal – AMALP.
d. False. It is more likely to enter the right main bronchus: it is wider.
e. True. Vertebral level T4 (or thereabouts).
2.
a. True.
b. True.
c. False. U-shaped cartilaginous rings.
d. False. They are much the same.
e. True.
3.
a. True.
b. False.
c. True. See Chapter 14. The apex of the lung is vulnerable in the supraclavicular region.
d. False. The pleural cavity is more extensive than the lungs.
e. False. Visceral pleura.
4.
a. True (usually). Dermatomes of C5–T1 are in the upper limb.
b. False. The second rib articulates here.
c. True.
d. False. They are anterior.
e. False. This is a symphysis or secondary cartilaginous joint (most midline joints are).
5.
a. True. They form a plexus around the oesophagus.
b. False.
c. False.
d. True. Mitral valve disease leading to enlargement of the left atrium may give rise to dysphagia.
e. False. See (b) above. How could it?
6.
a. True. Leakage of lymph is difficult to deal with.
b. False. With the aorta.
c. True.
d. False. Everything except right upper limb, right upper thorax and right head and neck.
e. False. Left.
7.
a. True.
b. True.
c. True. PAMT 3344 (see text).
d. False. It is the outflow valve of the left atrium.
e. False. It is best heard at the apex.
8.
a. False. Atrioventricular valves only.
b. True. Useful in bypass operations.
c. False. Inferior.
d. False. Right atrium.
e. True.
9.
a. True.
b. False. It runs in the atrioventricular groove.
c. True. Cardiac pain may also be felt in the chest and left arm.
d. False. This is the SA node.
e. True.
10.
a. False. From the ascending aorta, anterior aortic sinus.
b. False. This comes from the left.
c. False.
d. True.
e. True.
11.
a. False. Apex.
b. True.
c. True. See above.
d. False. PAMT from top to bottom.
e. False. During systole.
12.
13.
a. False.
b. True.
c. False. This comes from the brachiocephalic trunk.
d. True.
e. True.
14.
a. True.
b. False.
c. True.
d. False.
e. True.
15.
a. False. The vagus passes posterior to the hilum, the phrenic anterior.
b. False. The left main bronchus indents the oesophagus.
c. True. Serous pericardium is equivalent to pleura and peritoneum.
d. False. The vagus is the tenth cranial nerve.
e. False. It empties into the superior vena cava.
16.
a. True.
b. False. Right crus.
c. True.
d. True.
e. False.
17.
a. False. It should never be. If it is, it is likely that malignant disease has caused it to be.
b. False. Lymphatics drain most importantly to the axilla, but not entirely. Lymph also drains to the parasternal nodes (with the internal thoracic arteries) and various others.
c. False. The breast also receives blood from lateral thoracic and thoracoacromial arteries. In any case, a question in which the words ‘only’, ‘always’, ‘never’ appear is always (!) false. Nothing is ever so definite.
d. False. It extends usually to the level of the sixth rib.
e. True. They may be found on the milk lines.
18.
a. True.
b. True.
c. True.
d. True.
e. True.
19.
a. False. It is formed by the ventral ramus of the main trunk (this is a ‘nit-picking’ question, but you will meet plenty of these).
b. False. It is formed by the ventral ramus, not root. This is not so ‘nit-picking’ because ventral roots carry motor fibres, whereas the nerve itself carries both sensory and motor fibres: clinically, a lesion of the roots causes symptoms distinguishable from those of a lesion of a nerve.
c. True!
d. False. It runs between the internal and innermost intercostal muscles (who cares?).
e. True.
20.
a. True.
b. True.
c. True.
d. True.
e. False. Autonomic impulses supply involuntary muscle.
Single best answers
21. a.
22. a.
23. c.
24. b.
25. c.
26. b.
27. a.
28. a.
29. b.
Matching item answers
30. a.
31. c. (usually)
32. c.
33. b.
34. c.
35. c.
36. b.
37. b.
38. d.
39. d.
Short answers
40. The bronchopulmonary segments of the right lung are: upper lobe – apical, posterior, anterior; middle lobe – lateral, medial; lower lobe – apical basal, medial basal, anterior basal, lateral basal, posterior basal (APALM, AMALP). The medial basal lobe is absent on the left. Lateral and medial segments of the right middle lobe are replaced on the left by the superior and inferior lingular segments, part of the left upper lobe, which thus has five segments. In a bedridden patient lying on his back, fluid is most likely to drain to the most dependent parts: these would be, in this position, the apical basal and posterior basal segments of the lower lobe. This is why regular physiotherapy and bronchial hygiene in seriously ill patients who can not be moved from the supine position is so important.
41.
a. The lobes of the right lung are demarcated by two fissures:
• oblique fissure: a line from the spine of vertebra T2 or T3 round the chest wall to the sixth costal cartilage (there are other ways of describing this)
• horizontal fissure: a line from about the fourth costal cartilage laterally until it meets that for the oblique fissure.
What this means is that when you place your stethoscope on the right anterior chest wall, you are listening to the upper and middle lobes, but not the lower lobe. On the left, of course, it is all upper lobe at the front.
b. Heart surface markings are: (a) second intercostal space at the left sternal edge, to (b) third space at the right sternal edge, to (c) sixth space at the right sternal edge, to (d) left fifth space in the midclavicular line (apex), back to (a). Heart valves are all retrosternal: from top to bottom, pulmonary, aortic, mitral, tricuspid – levels respectively third costal cartilage, third space, fourth cartilage, fourth space (PAMT 3344). They are best heard, though, elsewhere, since sounds are transmitted by blood flow: aortic – second space, right sternal edge; pulmonary – second space, left sternal edge; tricuspid – lower sternal edge, the side depending upon the condition; mitral – apex.
42. A chest drain is usually inserted into the second intercostal space in the midclavicular line, or the fourth or fifth space in the midaxillary line. You must avoid the heart at the front, so you need to remain fairly high. At the side, you need to avoid the axilla and arteries and nerves in that region, so not too high, but on the other hand you need to avoid the risk of damage to abdominal structures, so not too low or too far posterior. If a needle is inserted into a normal pleural cavity, air will enter the cavity, pushing the visceral and parietal layers of pleura leading to a pneumothorax. Chest drains are normally used to drain fluid that has collected in the pleural cavity, or, in a pneumothorax, the drain will be attached to a vacuum so that the air in the cavity will be sucked out.
43. At and around vertebral level T4 the oesophagus is related to the arch of the aorta and the left main bronchus as well as the azygos venous system and the thoracic duct. Erosion of the tumour into the bronchial tree will result in ingested fluids passing into the bronchi, initiating coughing and/or causing pneumonia. Erosion into the arch of the aorta may result in death by massive haemorrhage into the oesophagus.
44. See Figures 10.20 and 10.21 (p. 83).
45. The blood cell travels as follows: SVC→RA→tricuspid valve→RV→pulmonary valve→pulmonary trunk, lungs, pulmonary veins→LA→mitral valve→LV→aortic valve→aorta→brachiocephalic artery→right subclavian artery. In valvular incompetence the valves do not close properly, leading to leakage of blood. In stenosis the valves do not open fully.
46. The pacemaker node is the SA node in the right atrial wall at the top of the crista terminalis, to the left of the SVC orifice. There are no specialised conducting fibres in the atrial walls. The electrical impulse spreads to the AV node in the lower end of the atrial septum beside the coronary sinus opening. From here, Purkinje fibres form the bundle of His, which penetrates the fibrous cardiac skeleton separating atria from ventricles, enters the ventricular septum, and divides about half way down the ventricular septum into right and left bundle branches. The left bundle branch passes to the apex and up the left side of the heart. The right bundle branch crosses to the inferior side of the ventricle in the septomarginal (moderator) band. The fibrous skeleton does not conduct electrical impulse except where pierced by the bundle of His. If the skeleton is damaged (disease), it may allow electrical impulse back into the atria (re-entry phenomena), thus initiating extra beats (extrasystoles).
47. This is notching of the ribs and it is a sign of enlarged intercostal arteries. This may indicate that the intercostal arteries are being used as part of a pathway bypassing a blocked aorta. Blood would pass as follows: ascending aorta→subclavians→scapular anastomosis→intercostals (retrograde flow)→descending aorta. Other bypass channels that may develop include the internal thoracic-superior and inferior epigastric channel (see Fig. 10.25, p. 88). In a normal person the femoral and radial pulses are approximately synchronous, their being similar distances from the heart. But in patients with an aortic coarctation, the femoral pulse is weaker and later than the radial.
48. This sounds like a breast tumour that involves suspensory ligaments (of Cooper) leading to shortening of the ligaments and dimpling of the overlying skin. It also sounds like a malignant tumour, and enlargement of the axillary lymph nodes lends weight to this opinion. Other lymph nodes that might be involved are: parasternal (not normally palpable), nodes of the anterior abdominal wall and possibly even inguinal nodes (if the tumour is low in the breast). A tumour that had involved the pectoralis major muscle would result in fixation of the breast to the muscle – most definitely abnormal and suspicious of malignant disease.