Chapter 25 Thoracic Trauma
All types and severity of trauma can involve thoracic injury, and the mechanism of injury often provides little guidance to the nature of the injury that has been sustained. Acutely life-threatening thoracic injuries include tension pneumothorax, large open pneumothorax, massive hemothorax, and cardiac tamponade.
CHEST WALL INJURIES
Rib Fractures
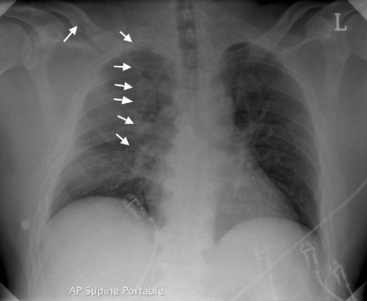
Rib fractures are the most common significant injury to the thorax. They occur after a wide range of injuries and become increasingly common as age increases and the flexibility of the rib cage decreases. Diagnosis is largely clinical because one or two fractures are not always apparent on a chest radiograph. Multiple rib fractures usually can be seen (Fig. 25-1). Rib fractures may be associated with underlying lung injury such as pneumothorax, hemothorax, or pulmonary contusion.
Flail Chest
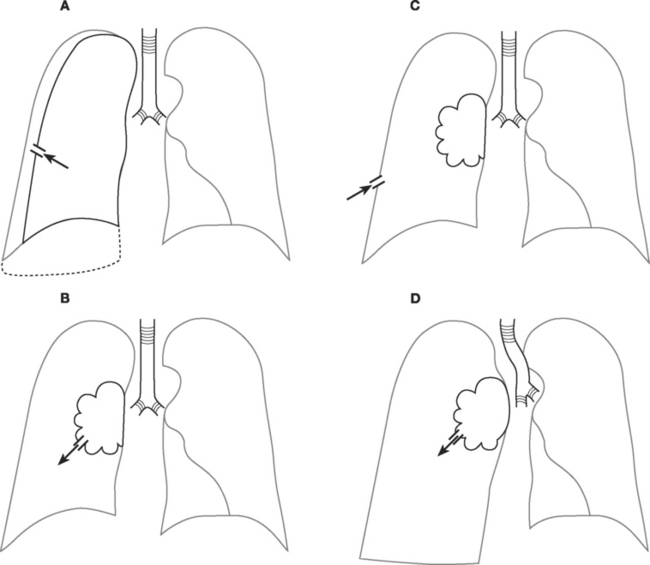
Multiple rib fractures may result in a flail chest (Fig. 25-2), in which a section of the chest wall moves paradoxically with respiration. Flail chest is almost always associated with significant underlying pulmonary contusion and severe respiratory compromise. Treatment is supportive: oxygen or ventilatory support for hypoxemia and respiratory distress along with physical therapy and adequate analgesia. Some data show that open reduction and internal fixation of the flail segment is associated with less pain and a shorter hospital stay than is a conservative approach.1
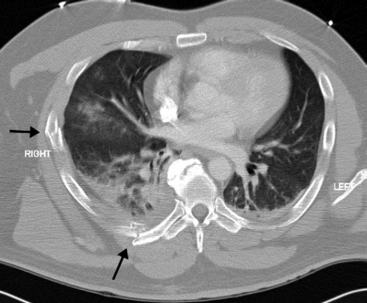
Figure 25.2 Transverse CT scan of the patient in Figure 25-1. On the right side, posteriorly, a fractured rib is seen. This fracture is seen on the radiograph. However, laterally a further fracture is seen, which is not apparent on the plain radiograph. This patient has a substantial flail segment of the right chest wall. A small right pleural collection and contusion of the right lung is also seen.
LUNG INJURIES
Pulmonary Contusion
Pulmonary contusion is common following severe blunt thoracic trauma and blast injury. The presence of a significant chest wall injury indicates a high likelihood of an underlying pulmonary contusion. Radiographically, pulmonary contusion appears as a region of dense alveolar shadowing (see Fig. 25-1), often underlying chest wall soft-tissue swelling and rib fractures. Treatment is supportive.
Pneumothorax
Pneumothoraces may be open or closed, large or small, simple or under tension (Fig. 25-3). With an open pneumothorax, there is a breach in the chest wall that allows air to enter the chest cavity through the defect (rather than through the trachea, as occurs with a closed pneumothorax). Patients present with a “sucking” chest wound and severe respiratory distress. The pneumothorax is likely to be large and there may be an associated hemothorax and flail segment. Immediate intubation and invasive ventilation may be required. Treatment involves urgent surgical repair. If immediate surgical repair is not possible, the wound should be covered with an impermeable dressing and a thoracostomy tube should be inserted and connected to an underwater seal drain. The dressing should be sealed on only three sides, with the lower side left unsealed to allow air under tension to escape from the chest while preventing air entrainment through the wound. Once the thoracostomy tube is inserted, the dressing should be completely sealed. Surgical repair should be arranged as soon as possible.
Tension and large simple pneumothoraces are usually diagnosed clinically. Both present with respiratory distress, reduced breath sounds on the affected side, and hyperresonance to percussion. With a tension pneumothorax (Fig. 25-4), the patient may be in shock because of compression of the mediastinal structures and obstruction to venous return. The trachea may be deviated to the unaffected side and there may be displacement of the apex beat. A simple pneumothorax (see Fig. 6-21) may be converted into a tension pneumothorax with the institution of positive pressure ventilation. With severe respiratory distress or shock, needle thoracocentesis should be performed without delay, commonly before the chest radiograph is available. Needle thoracocentesis should be followed immediately by tube thoracostomy and underwater seal drainage (see Chapter 40). With simple pneumothoraces, lung reinflation is usually rapid and, providing there is no ongoing air leak, the tube can be removed in as short a time as a few hours in cases of penetrating trauma or in 1 to 2 days after blunt trauma.2 Whenever a large pneumothorax occurs after penetrating trauma, the possibility of an airway injury must be considered.
Small, simple pneumothoraces are commonly diagnosed incidentally on a chest radiograph or on an abdominal computed tomogram (CT).3 Whether these incidentally identified pneumothoraces require tube thoracostomy is debatable. As a general rule, if positive pressure ventilation is required4 or if the patient is to be transported by air, drainage is mandatory.
Hemothorax
Isolated hemothorax typically presents with hypovolemic shock, with or without respiratory distress. Breath sounds are reduced on the affected side but, unlike in pneumothorax, the chest is dull to percussion. The diagnosis is confirmed by chest radiography (see Fig. 6-26). Initial treatment involves ensuring that large-bore intravenous cannulas are placed above and below the diaphragm. Insertion of at least one and sometimes two thoracostomy tubes is necessary, and they should be of large size (28F or larger) so as to reduce the chances of their occlusion by clot. The initial and subsequent blood loss must be carefully monitored. When initial blood loss is more than 1500 ml in penetrating trauma or 2000 ml in blunt trauma, immediate thoracotomy should be considered.5 If the patient is grossly unstable or moribund, thoracotomy should be undertaken in the emergency department. Regardless of the initial amount of blood loss, thoracotomy should be considered if blood loss exceeds 800 ml in 4 hours. If the placement of one or more thoracostomy tubes fails to clear the thoracic cavity of blood in 2 to 3 days, surgical evacuation should be considered. This can often be performed thoracoscopically,6 but if the clot is well organized, thoracotomy will be required.
Surgical exploration of thoracic stab wounds (unlike abdominal stab wounds) is not mandatory. Similarly, there is no indication for thoracotomy to remove bullets unless they have embolized to pulmonary vessels or are lodged in the myocardium in a way likely to cause functional problems.
Lung Laceration
Lung laceration is common in penetrating trauma and has also been described after major blunt trauma. It is difficult to diagnose but is often associated with ongoing blood loss or air leak, in which case thoracotomy is indicated. At the time of surgery there is no need to repair the laceration specifically, but there should be no ongoing air leak or bleeding from the cut surface of the lung. If the lung laceration results from penetrating trauma, “tractotomy” may be required, in which the lung tissue overlying the penetrating tract is divided by a cutting stapler so that the bleeding and air leak from the deep parts of the tract can be seen and dealt with.7
Tracheal Injury
Tracheal injury is rare in blunt trauma but may occur in penetrating trauma. It represents a life-threatening airway problem. Depending on the location of the injury, it may present with dramatic subcutaneous or mediastinal emphysema or with a profuse air leak into one or both hemithoraces. In cases of nonpenetrating trauma, tracheal injury may be difficult to diagnose because the signs—respiratory distress, cough, hemoptysis, and subcutaneous emphysema—are relatively nonspecific.
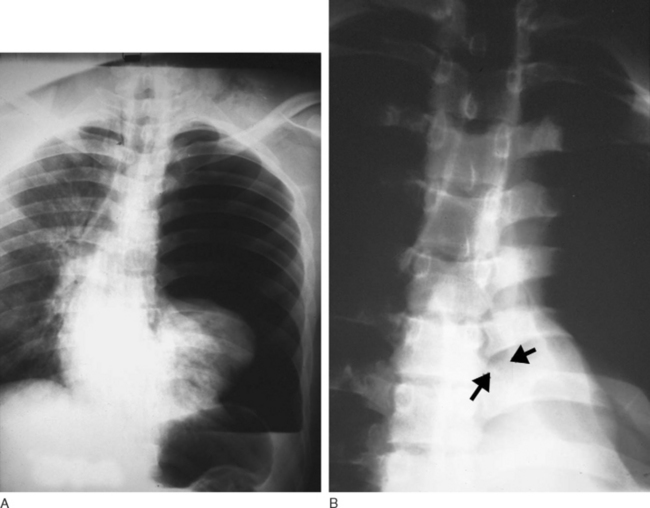
Bronchial Injury
Bronchial injury may occur after penetrating trauma, but it also occurs with blunt trauma in which there is severe deceleration. Penetrating injuries are commonly associated with great-vessel and cardiac injury. Bronchial disruption presents with cough, hemoptysis, subcutaneous emphysema, and pneumothorax. The finding of a large air leak after insertion of chest tubes, in association with lobar collapse, is suggestive of the diagnosis. With complete bronchial disruption, the “dropped lung” sign may be present on the chest radiograph (Fig. 25-5). The institution of positive pressure ventilation in this circumstance can precipitate a tension pneumothorax. If suspected, the diagnosis may be confirmed by bronchoscopy. Surgical repair is usually indicated, and that requires lung isolation (e.g., via a double lumen endotracheal tube, see Chapter 40).
CARDIAC INJURIES
Blunt Cardiac Injury
Cardiac rupture after blunt thoracic trauma is usually fatal. Occasionally, sudden compression of the chest results in the blowout of the left atrial appendage or pulmonary veins, and the outcome is cardiac tamponade rather than immediate exsanguination. Because this is a low-pressure bleed, the heart may be able to function adequately with the tamponade and sustain life. The patient usually presents with shock and distended neck veins. The differential diagnosis includes tension pneumothorax, preinjury myocardial dysfunction, and severe cardiac contusion. Initial clinical examination should rapidly diagnose or exclude tension pneumothorax. The diagnosis of tamponade is reliably confirmed by a focused assessment by sonography for trauma (FAST) ultrasound scan.8 Immediate transfer to the operating room for median sternotomy and surgical repair is required.
Less severe forms of blunt cardiac injury are not associated with cardiac tamponade but can cause cardiac dysfunction due to myocardial contusion, particularly to the anteriorly positioned right ventricle. Severe cardiac contusion involving the right ventricle may resemble cardiac tamponade, with the patient presenting with distended neck veins and hypotension, but profound hypotension is rare. There may be troublesome arrhythmias, including atrial fibrillation, atrial flutter, multifocal ventricular premature beats and, occasionally, ventricular fibrillation. The electrocardiogram (ECG) may show a range of abnormalities, including nonspecific ST and T wave changes, arrhythmias, sinus tachycardia, and right bundle branch block. The diagnosis rests on determining an appropriate mechanism of injury, an elevated plasma troponin level, and the presence of segmental wall motion abnormalities on an echocardiogram. Treatment is supportive and includes control of arrhythmias, fluid and, if necessary, inotropes. Patients should undergo continuous ECG monitoring for at least 24 hours. Rarely, blunt chest trauma causes rupture of a valve leaflet or chorda, resulting in clinical signs of acute valvular regurgitation (see Chapter 10).
Penetrating Cardiac Injury
Penetrating trauma is a much more common cause of cardiac injury than is blunt trauma, and it is commonly fatal. If such patients survive to reach the emergency department, they may have massive hemothorax or cardiac tamponade and be critically unwell. In this situation, thoracotomy in the emergency room is indicated. In less acute situations, pericardiocentesis (see Chapter 40) followed by urgent surgical exploration is appropriate. An intraoperative transesophageal echocardiogram is mandatory once esophageal perforation is excluded, because many patients will have suffered disruption of the intracardiac anatomy.
GREAT VESSEL INJURIES
Traumatic Aortic Rupture
One of the most feared complications of major blunt thoracic trauma is aortic rupture. In more than 90% of cases, the site of rupture is the aortic isthmus, the region of the aorta just distal to the origin of the left subclavian artery at the site of attachment of the ligamentum arteriosum.9 Less commonly, rupture of the aorta occurs at the level of the aortic root or at the diaphragm. Rarely, rupture of the abdominal aorta can occur with severe deceleration injury in motor vehicle accidents; the rupture is caused by the seat belt’s compression of the abdomen. Complete rupture of the thoracic aorta is uniformly fatal. In survivors, the rupture is contained within a pseudoaneurysm formed from the adventitia of the aortic wall and mediastinal tissues.
Traumatic aortic rupture was long considered to be a rapidly fatal condition that took priority over other trauma injuries. However, more recently it has been shown that the risk for death in stable patients who reach hospital and receive appropriate antihypertensive therapy is low.10 Thus, although repair of a ruptured aorta should be undertaken urgently, it should not take priority over other unstable injuries such as abdominal or pelvic bleeding.
Diagnosis and Investigation
Specific clinical signs of aortic rupture are uncommon. Reduced femoral pulses secondary to an obstructive intimal flap are occasionally present. In ruptures that occur at the level of the aortic isthmus, the only finding may be an abnormal appearance of the superior mediastinum on the chest radiograph (Fig. 25-6A). An erect chest radiograph is more likely to be diagnostic than a supine one, but this is not usually possible in patients with severe trauma.
The presence of an abnormal mediastinal contour on the chest radiograph mandates further imaging to confirm or exclude aortic rupture. Historically, this has meant performing an aortogram. Aortography is a highly specific and sensitive diagnostic test for traumatic aortic rupture.11 However, it is invasive and usually takes some time to organize. More recently, CT aortography has become the imaging modality of choice. With modern CT scanners, imaging is rapid and is highly sensitive and specific.12 In addition to conventional axial imaging (Fig. 25-6B), multidetector CT scanning allows for sagittal (Fig. 25-6C) and three-dimensional reconstruction of the aorta (Fig. 25-6D and E).13 CT aortography also provides information about aortic dimensions and defines the relationship of the aortic arch vessels to the rupture, information that is necessary for planning endovascular stent grafting.
Treatment
In patients who are hemodynamically stable and do not have an ongoing source of bleeding, strict control of blood pressure during the period of preoperative investigation helps to reduce shear stress on the aorta and therefore reduces the risk for acute (complete) rupture. Blood pressure control may be achieved by providing adequate analgesia and a combination of intravenous nitroglycerin and a β blocker, aiming for a blood pressure at the lower end of the normal range (e.g., a systolic pressure of approximately 110 mmHg).
The standard surgical treatment for traumatic aortic rupture involves either end-to-end anastomosis or placement of an interposition graft at the site of the rupture. The surgeon may perform a “clamp-and-sew” technique or use some form of bypass support to decompress the proximal aorta and perfuse the distal aorta during the period of aortic cross-clamping. Bypass options include (1) passive aortoaortic shunting across the clamped area with a heparin bonded (Gott) shunt; (2) left heart (atriofemoral) bypass; and (3) partial (femoral-femoral) bypass (see Chapter 11). Left heart bypass or the use of a passive shunt is associated with a reduced incidence of paraplegia and a better overall outcome than the clamp-and-sew technique.14
Open repair is commonly associated with major blood loss and marked hemodynamic instability. Also, there is a requirement for one-lung ventilation and, depending on the technique, partial or full heparinization. These requirements can present serious problems in a patient with polytrauma. Systemic heparinization is contraindicated in patients with intracranial hematoma, solid organ abdominal injury, or major pelvic fractures. The presence of a right-sided pulmonary contusion or acute respiratory distress syndrome may preclude the safe use of right-sided one-lung ventilation. In patients with facial or cervical spine injuries, replacement of a single-lumen by a double-lumen endotracheal tube (and vice versa at the completion of surgery) may be very risky. Endovascular repair offers a safe and effective alternative to open surgical repair,15,16 and in many centers has become the treatment of choice for traumatic aortic rupture. The technique and complications of endovascular stent grafting are described in Chapter 11.
ESOPHAGEAL INJURY
Esophageal injury is almost unknown in blunt trauma but can occur with penetrating trauma. If the injury is missed, fatal mediastinitis usually ensues. Diagnosis requires an appropriate degree of clinical suspicion. If the injury is suspected, investigation should include both an oral contrast study and esophagoscopy. Pneumomediastinum may be seen on chest radiography, but this usually occurs late. Treatment requires a thoracotomy, direct repair and drainage, and consideration of esophageal diversion by way of a cervical esophagostomy. Mortality rates are as high as 20%.17
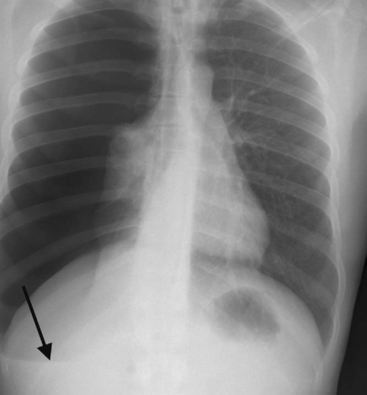
RUPTURED DIAPHRAGM
Ruptured diaphragm involves a tear in the diaphragm, usually secondary to deceleration injury, through which the abdominal contents enter into the chest. The left hemidiaphragm is affected three times more commonly than the right.18 Patients may present with symptoms of respiratory distress, but in some cases the condition is discovered incidentally. On the chest radiography, abdominal contents can usually be seen protruding into the thoracic cavity. If a left-sided rupture is suspected, the diagnosis can be confirmed by passing a nasogastric tube and seeing where it is positioned on a repeat chest radiograph. If there is doubt as to the diagnosis, a CT should be performed. Spontaneous (negative pressure) breathing exacerbates herniation of abdominal contents into the chest. Intubation and positive pressure ventilation should be performed if there is significant respiratory distress. Early surgical repair is performed via a laparotomy. Late surgical repair may require a thoracotomy.
Resuscitative Thoracotomy
If pulseless cardiac arrest develops in the setting of either blunt or penetrating thoracic trauma, outcome is poor unless a reversible cause is immediately identified and treated. Emergency department resuscitative thoracotomy for thoracic trauma has a survival rate of 11% in penetrating trauma but only 1.6% in blunt trauma.19 If an appropriately skilled clinician is present, the American Heart Association advocates resuscitative thoracotomy in the following circumstances.20
1 Lardinois D, Krueger T, Dusmet M, et al. Pulmonary function testing after operative stabilisation of the chest wall for flail chest. Eur J Cardiothorac Surg. 2001;20:496-501.
2 Martino K, Merrit S, Boyakye K, et al. Prospective randomized trial of thoracostomy removal algorithms. J Trauma. 1999;46:369-371.
3 Neff MA, Monk JSJr, Peters K, et al. Detection of occult pneumothoraces on abdominal computed tomographic scans in trauma patients. J Trauma. 2000;49:281-285.
4 Laws D, Neville E, Duffy J. BTS guidelines for the insertion of a chest drain. Thorax. 2003;58(suppl 2):ii53-ii59.
5 American College of Surgeons Committee on Trauma. Advanced trauma life support for doctors. Student Course Manual, ed 6. Chicago, American College of Surgeons, 1997.
6 Heniford BT, Carrillo EH, Spain DA, et al. The role of thoracoscopy in the management of retained thoracic collections after trauma. Ann Thorac Surg. 1997;63:940-943.
7 Asensio JA, Demetriades D, Berne JD, et al. Stapled pulmonary tractotomy: a rapid way to control hemorrhage in penetrating pulmonary injuries. J Am Coll Surg. 1997;185:486-487.
8 Rozycki GS, Feliciano DV, Ochsner MG, et al. The role of ultrasound in patients with possible penetrating cardiac wounds: a prospective multicenter study. J Trauma. 1999;46:543-551.
9 Groskin SA. Selected topics in chest trauma. Radiology. 1992;183:605-617.
10 Pate JW, Fabian TC, Walker W. Traumatic rupture of the aortic isthmus: an emergency ? World J Surg. 1995;19:119-125.
11 Sturm JT, Hankins DG, Young G. Thoracic aortography following blunt chest trauma. Am J Emerg Med. 1990;8:92-96.
12 Fabian TC, Davis KA, Gavant ML, et al. Prospective study of blunt aortic injury: helical CT is diagnostic and antihypertensive therapy reduces rupture. Ann Surg. 1998;227:666-676.
13 Alkadhi H, Wildermuth S, Desbiolles L, et al. Vascular emergencies of the thorax after blunt and iatrogenic trauma: multi-detector row CT and three-dimensional imaging. Radiographics. 2004;24:1239-1255.
14 Fabian TC, Richardson JD, Croce MA, et al. Prospective study of blunt aortic injury: Multicenter Trial of the American Association for the Surgery of Trauma. J Trauma. 1997;42:374-380.
15 Karmy-Jones R, Hoffer E, Meissner MH, et al. Endovascular stent grafts and aortic rupture: a case series. J Trauma. 2003;55:805-810.
16 Thompson CS, Rodriguez JA, Ramaiah VG, et al. Acute traumatic rupture of the thoracic aorta treated with endoluminal stent grafts. J Trauma. 2002;52:1173-1177.
17 Asensio JA, Chahwan S, Forno W, et al. Penetrating esophageal injuries: multicenter study of the American Association for the Surgery of Trauma. J Trauma. 2001;50:289-296.
18 Smithers BM, O’Loughlin B, Strong RW. Diagnosis of ruptured diaphragm following blunt trauma: results from 85 cases. Aust N Z J Surg. 1991;61:737-741.
19 American College of Surgeons Committee on Trauma. Practice management guidelines for emergency department thoracotomy. Working Group, Ad Hoc Subcommittee on Outcomes, American College of Surgeons-Committee on Trauma. J Am Coll Surg. 2001;193:303-309.
20 American Heart Association. Part 10.7: Cardiac arrest associated with trauma. Circulation. 2005;112:IV146-IV149.