Chapter 141 Thoracic and Lumbar Spine Construct Design
Construct design is a process that formulates a specific blueprint for an orderly and thoughtful assembly of implantable spinal instrumentation, designed to correct instability or deformity or both of the spinal column.1 Construct design requires specific understanding of the deformity or instability and the biomechanical forces acting on the pathologic alignment. An understanding of corrective forces and where they must be applied also is required. A keen knowledge of the anatomy and pathoanatomy is required to preserve neuralgic function and avoid adjacent segment injury. Although skillful assembly of the mechanical construct is a definite prerequisite, ultimate success is determined by the orderly thought process for designing the construct, based on personal experience, experience of others, and laboratory data. Creating a preoperative plan, or blueprint, can focus this design process. Spinal instrumentation surgery must not be assumed to be strictly “mechanical” or “routine”; rather, it requires serious and meticulous planning to ensure success.
Construct Types (Modes of Force Application)
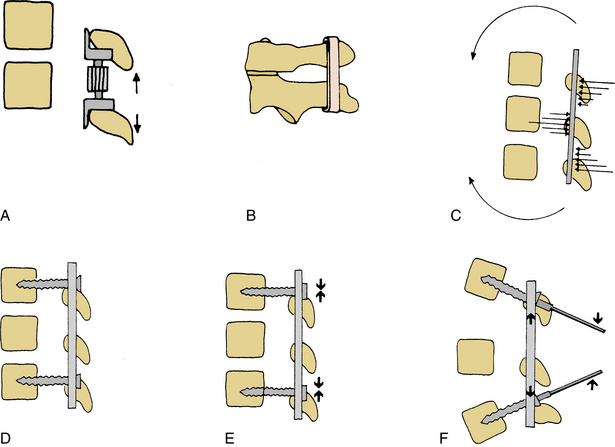
The six fundamental construct types are simple distraction, three-point bending, tension band fixation, fixed-moment arm cantilever-beam fixation, non–fixed-moment arm cantilever-beam fixation, and applied-moment arm cantilever-beam fixation (Fig. 141-1).
Development of Construct Blueprint
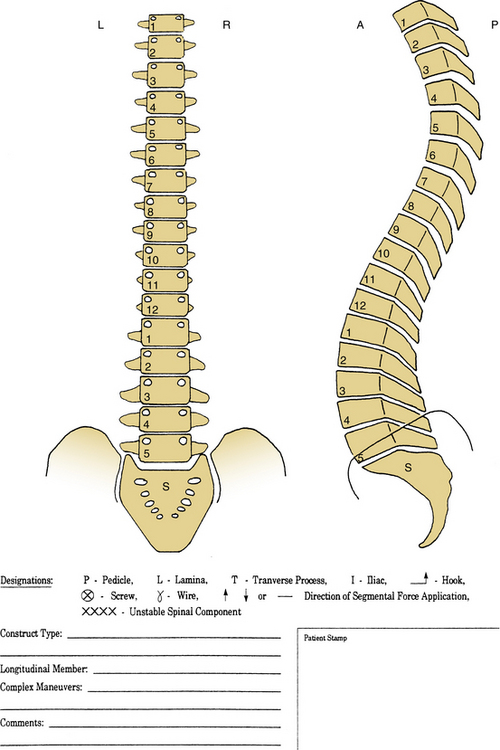
A simple scheme should be used that provides (1) information about the level of the lesion or the level of the unstable segment or segments, (2) the types of implants to be used (anchors, longitudinal members, and cross-connectors), (3) the length of stabilization required on either side of the lesion, and (4) the mode of load bearing by the construct. The scheme guides selection of the appropriate implant components in advance, improves the intraoperative communication between surgeons and assistants, and enhances the chances of success.
Line Drawing of Proposed Construct
A simple dorsoventral or lateral line drawing of the spine provides a framework for the clear definition of the operative plan. Often only a dorsoventral drawing is necessary, although clear consideration of any sagittal plane deformity is vital. The line drawing provides the blueprint for surgery (Fig. 141-2).2 This drawing can be easily obtained from a CT scan or from radiographs.
Level of Lesion and Level of Fusion
Hook constructs, often used in the past throughout the spine and still used at the present time in the thoracic region, should incorporate three spinal levels above and two spinal segments below the limits of the lesion (3A-2B rule). For the past decade or so, hooks have mainly been reserved for situations in which the pedicles are very small or for additional support in osteoporotic patients along with pedicle screws. If the patient has a marked angular kyphotic deformity, and if three-point bending is considered in an attempt to reduce the deformity, inclusion of four or more spinal levels above the lesion is common (4A-2B rule) and may provide a more functional lever arm. Such long constructs are suited mostly for lesions in the middle and upper thoracic regions, although thoracic pedicle screws are widely used even in these regions.
Both segmental pedicle screw and hook instrumentation techniques are successful in obtaining global balance safely. Balance can be accomplished without neurologic injury, even in adolescent idiopathic scoliosis, where neurologic risk is greatest. Segmental pedicle screw instrumentation offers a significantly better overall major and minor coronal curve correction and maintenance without neurologic problems and slightly improved pulmonary function values for the operative treatment of adolescent idiopathic scoliosis. Pedicle screw constructs may also allow for a slightly shorter fusion length than segmental hook instrumentation.3
Construct Design Strategies
Multiple factors should be taken into account in designing a spinal instrumentation construct.4 Consideration should be given specifically to bony integrity, the location of the unstable spinal segment, the implant length with respect to the unstable segment, the need for cross-fixation, the need for dural decompression, the choice of ventral versus dorsal instrumentation, availability of specific instrumentation, metallic composition of instrumentation, and the familiarity of the surgeon with a particular technique. Each factor should be adequately addressed to achieve optimal outcome.
Bony Integrity
Osteoporosis poses a significant problem in spinal instrumentation. Hooks and cables may resist pull-out better than bone screws.5,6 A longer construct is often required in osteoporotic bone. More anchors are needed to distribute the load over more segments, decreasing the load at any single site. Interbody stability, either from fully collapsed discs or interbody implants, may protect the dorsal construct from cantilever pull-out. If pedicle screws are required in a patient with marked osteoporosis, consideration should be given to filling the screw tracks with polymethylmethacrylate (PMMA). Addition of PMMA significantly increases screw pull-out strength and is accomplished by first placing and then removing the pedicle screw. The pedicle must be carefully assessed to ensure no cortical penetration has occurred that would allow the methyl methacrylate to leak. PMMA is placed using a large syringe under minimal pressure, and the pedicle screws are rapidly reinserted. The spinal canal should be inspected to ensure the methyl methacrylate has not inadvertently extruded into the canal with potential compression of neural elements. The instrumentation construct is then completed.
Biomechanical studies have shown that pedicle screw augmentation with PMMA using transpedicular and kyphoplasty techniques increased the pull-out failure load twofold to threefold in osteoporotic vertebrae.7 Pedicle screws augmented using the kyphoplasty technique had significantly greater pull-out strength than screws augmented with the transpedicular augmentation technique.7 Another option for osteoporotic spine fixation is use of expansive pedicle screws. The expansive pedicle screw can progressively compress bone at the screw-bone interface by the expansion of the ventral two thirds of the screw, which is thought to provide greater screw thread engagement of vertebral bone than a conventional pedicle screw of the same size. Biomechanical tests have shown that expansive pedicle screws can significantly improve the axial pull-out force compared with conventional screws in osteoporotic bones.8–10
Location of the Unstable Spinal Segment
The closer the lesion or unstable segment is to the occiput or sacrum, the shorter the applied lever arm is to the terminal end of the construct. More rigid fixation is required at the terminal end of the construct.11 Often, multiple points of fixation are used in the sacrum or occiput. Long constructs that end at the sacrum have a high rate of pseudarthrosis at the terminal end (L5-S1).12 A very high flexion-extension bending moment exists on the S1 screws, which leads to loosening of the screws. The addition of iliac screws, alar screws, or S2 pedicle screws to the construct significantly decreases the bending moment on the S1 pedicle screws and increases the fusion rate.12,13
Implant Length
A long construct may be required to provide greater purchase of adjacent segments and greater stability. In the treatment of gross spinal instability or long curvatures (scoliosis or kyphosis), longer constructs may apply greater force overall and less force at each individual segment. Adding bone anchors, rod diameters, or both can significantly increase overall stiffness.14
Instrumentation Fusion Mismatch (“Rod Long, Fuse Short”)
The rationale for this approach is that a long instrumentation construct is used to achieve reduction and correction of deformity, while fusing only the minimum number of segments necessary. The hardware is later removed (after 1 year), when the fractures have healed, and the fusion has consolidated, releasing the instrumented, but not fused, segments from immobilization. There is some concern that the facet joints included within the instrumented nonfused segments may undergo degenerative arthropathy.15 An additional disadvantage of the “rod long, fuse short” construct is the potential for the implants to loosen. Hooks and cables allow more movement at this juncture than screws and may not pose as great a problem. This design has generally fallen out of favor. If this mode of construct is desired, screws should not be used as anchors in the nonfused segments.
Short-Segment Fixation
Generally, hook and cable constructs require long constructs, three above and two below (3A-2B) the lesion. This design provides a longer and more efficient moment arm and a stronger construct.16 The 3A-2B configuration is a logical compromise between the problems associated with longer constructs and the shorter moment arm achieved with the shorter constructs and has been shown to provide good stability. Pedicle screws may allow for shorter constructs and fewer fusion segments, a single level above and below the lesion (1A-1B). Short-segment fixation provides an increasingly popular alternative, particularly when applied in a compression mode. Reinforcement with fracture-level screw combinations in patients who underwent short-segment fixation can help to provide better kyphosis correction and offers improved biomechanical spinal stability in patients with thoracolumbar burst fracture.17,18 Because of the limited fixation, there may be a higher rate of failure19; this is particularly true if the screw purchase is poor (osteoporosis) or if the loads are too great, secondary to a loss of anterior column stability. Long constructs have been shown to be reliable and effective in treating thoracic injuries, with or without ventral reconstruction. Short-segment pedicle instrumentation constructs have proved to be effective in stabilizing thoracolumbar and lumbar fractures, while limiting the disruption of lower lumbar motion segments. Loss of anterior column integrity leads to fixation failure when short constructs are not supplemented with further fixation or a ventral reconstruction.20 In a very unstable spine, without significant anterior column loss and rotational and shear fractures, pedicle screw fixation with two above and two below should provide adequate stability in most circumstances.
Cross-Fixation
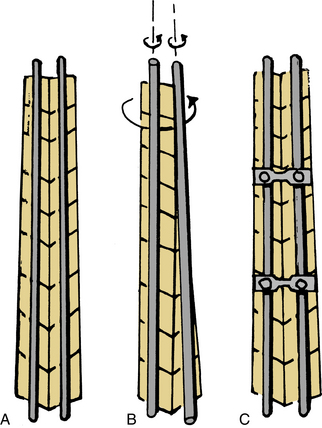
Cross-fixation between longitudinal members generally improves the torsional stability of longer constructs and the lateral bending stiffness (Fig. 141-3).21–23 It is not as critical to use cross-fixation in short-segment constructs. For a short-segment rod construct with a skipped level (nonsegmental fixation), a cross-fixing device improves torsional stability to that of segmental fixation.22 There is little effect of cross-links on flexion-extension stiffness.21 When using long rod constructs with hook anchors, cross-fixation is essential to improve hook stability and torsional and lateral bending stiffness. Interconnecting the hooks on the two longitudinal members with cross-links significantly increases the fixation rigidity and decreases the failure rate. When the distal end is anchored by pedicle screws, the torsional and bending stiffness is much greater and not significantly different with cross-links.24
Axial Load-Bearing Capacity of the Instrumented Spine
Two clinical examples illustrate this point. In a case of grade 1 degenerative spondylolisthesis, there is a long-standing translational deformity (glacial instability) but no problem with axial load bearing. The role of instrumentation is to reduce the deformity, align the spine, and stabilize the motion segment rigidly to facilitate bony fusion. In a patient with a severe burst fracture of the L1 vertebral body with some loss of bone substance, axial load bearing is ineffective. This problem may be corrected by resection of the vertebral body, replacement with a strut graft, and short-segment stabilization with a locking plate or dual-rod device. The goal of spinal reconstruction in the latter case is to restore load-bearing ability and to decompress and stabilize the spine.25 If a short-segment pedicle screw construct is used in such a case without vertebral body reconstruction, there may be significant axial loading of the screws, and they may fail.19,26
Nature of Instability
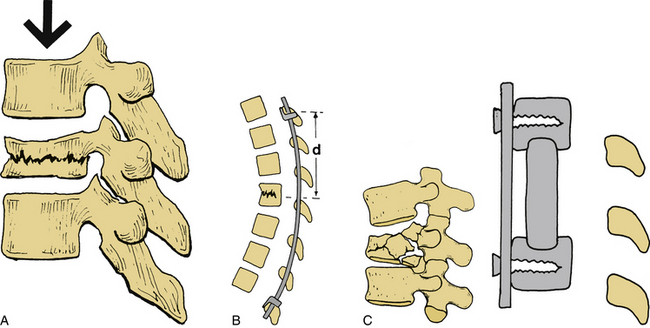
Kyphotic Deformity
Kyphotic deformities of the spine may be corrected in one of two ways: (1) with a dorsal approach, using a three-point bending maneuver through a long rod construct, or (2) via a ventral approach, with the resection of a vertebral body, interbody grafting, and application of a plate or dual-rod device (Fig. 141-4). If the deficit is in the anterior column, such as with compression or burst fracture, the ventral approach may be more appropriate. If the dorsal tension band is lost, which leads to kyphosis, the dorsal approach may work best. Both approaches may be used if the bone quality is poor or if a fixed deformity requires both approaches.
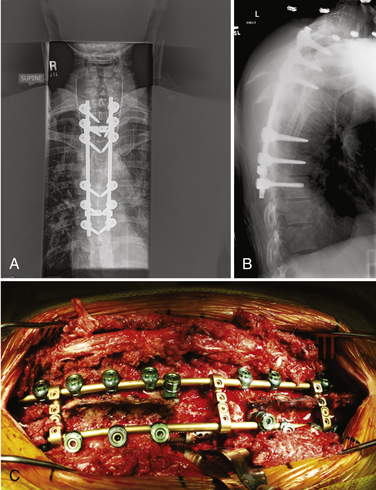
Translational Deformity
Translational deformities (e.g., fracture-dislocation resulting from trauma) are generally corrected from a dorsal orientation (Fig. 141-5). Distraction and three-point bending with long hook-rod constructs often work well, as do shorter constructs (two above and two below) with pedicle screws. Translational deformity of a glacial type from degenerative spondylolisthesis is generally easily reducible by mere positioning or with a pull-back technique, using pedicle screws, although adding an interbody implant significantly improves the overall stability. Translational deformity resulting from isthmic spondylolisthesis is much more difficult to correct. It requires complete discectomy and intervertebral distraction, followed by pull-back with screws. Great care must be taken with any reduction maneuver, and monitoring of the exiting nerve roots with electromyography is recommended.
Axial Loading Deformity (Burst Fracture)
Saving motion segments by limiting the number of the fusion segments is a fundamental principle of spinal surgery. In milder forms of fracture, distraction and extension via pedicle screws restores the alignment. Some authors have used monosegmental pedicle instrumentation with placement of pedicle screws directly into the fractured vertebral body to treat thoracolumbar fractures. Controversy exists over whether monosegmental pedicle instrumentation is a more suitable method for thoracolumbar burst fractures than short-segment fixation. Data from the literature confirm that both monosegmental transpedicular fixation and short-segment transpedicular fixation are effective and reliable operative techniques for selected thoracolumbar burst fractures. The former technique shortened the operative time and decreased the amount of blood loss significantly.27 In severe burst fractures with considerable bone loss, the preferred treatment is ventral excision of the vertebral body, strut grafting, and plating to reconstruct the anterior column.
Scoliotic Deformity
Surgical goals when treating scoliosis include achieving a well-balanced spine in all planes, while working to preserve segments and maintain mobility. Multiple types of instrumentation are available (hooks, sublaminar wires, and screws), although pedicle screws have gained in popularity because they offer superior multiplanar correction, the potential for shorter fusions, and a lower rate of implant failure or pull-out.28 Generally, cantilever bending and rod rotation techniques are employed to reduce the curve magnitude, along with distractive force applied on the concave side of the deformity and compression applied on the convex side of the deformity. In addition, interbody fusions may help in correcting the scoliotic deformity. Spinal cord monitoring is essential because distraction may place the cord at risk. Attention should also be paid to the rotational malalignment, which can often be improved with segmental fixation, using screws, hooks, or wires. Constructs with rostral and caudal pedicle screws were statistically more rigid in torsion than constructs with hooks as distal anchors in scoliosis correction.24
Benzel E.C. Construct design. In: Benzel E.C., editor. Spinal instrumentation. Chicago: AANS Publications; 1994:239-256.
Brodke D.S., Bachus K.N., Mohr R.A., Nguyen B.K., et al. Segmental pedicle screw fixation or cross-links in multilevel lumbar constructs: a biomechanical analysis. Spine J. 2001;1(5):373-379.
Cook S.D., Salkeld S.L., Stanley T., et al. Biomechanical study of pedicle screw fixation in severely osteoporotic bone. Spine J. 2004;4:402-408.
Krag M.H. Biomechanics of thoracolumbar spinal fixation. Spine (Phila Pa. 1991;1976)(16):S84-S99.
McLain R.F. The biomechanics of long versus short fixation for thoracolumbar spine fractures. Spine (Phila Pa 1976). 2006;31(suppl 11):S70-S79.
Zindrick M.R., Wiltse L.L., Windell E.H., et al. A biomechanical study of intrapeduncular screw fixation in the lumbosacral spine. Clin Orthop Relat Res. 1986;203:99-112.
1. Benzel E.C. Construct design. In: Benzel E.C., editor. Spinal instrumentation. Chicago: AANS Publications; 1994:239-256.
2. Benzel E.C. Construct design. In: Benzel E.C., editor. Biomechanics of spine stabilization: principles and practice. New York: McGraw-Hill; 1995:163-172.
3. Kim Y.J., Lenke L.G., Cho S.K., et al. Comparative analysis of pedicle screw versus hook instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2004;29:2040-2048.
4. Krag M.H. Biomechanics of thoracolumbar spinal fixation. Spine (Phila Pa 1976). 1991;16:S84-S99.
5. Butler T.E., Asher M.A., Jayaraman G., et al. The strength and stiffness of implant anchors in osteoporotic spines. Spine (Phila Pa 1976). 1994;19:1956-1962.
6. Halvorson T.L., Kelley L.A., Thomas K.A., et al. Effects of bone mineral density on pedicle screw fixation. Spine (Phila Pa 1976). 1994;19:2415-2420.
7. Burval D.J., McLain R.F., Milks R., Inceoglu S. Primary pedicle screw augmentation in osteoporotic lumbar vertebrae biomechanical analysis of pedicle fixation strength. Spine (Phila Pa 1976). 2007;32:1077-1083.
8. Lei W., Wu Z. Biomechanical evaluation of an expansive pedicle screw in calf vertebrae. Eur Spine J. 2006;15:321-326.
9. Cook S.D., Salkeld S.L., Stanley T., et al. Biomechanical study of pedicle screw fixation in severely osteoporotic bone. Spine J. 2004;4:402-408.
10. Gao M., Lei W., Wu Z., et al. Biomechanical evaluation of fixation strength of conventional and expansive pedicle screws with or without calcium based cement augmentation. Clin Biomech (Bristol, Avon). 2011;26:238-244.
11. Zindrick M.R., Wiltse L.L., Windell E.H., et al. A biomechanical study of intrapeduncular screw fixation in the lumbosacral spine. Clin Orthop Relat Res. 1986;203:99-112.
12. Kuklo T.R., Bridwell K.H., Lewis S.J., et al. Minimum 2-year analysis of sacropelvic fixation and L5-S1 fusion using S1 and iliac screws. Spine (Phila Pa 1976). 2001;26:1976-1983.
13. Alegre G.M., Gupta M.C., Bay B.K., et al. S1 screw bending moment with dorsal spinal instrumentation across the lumbosacral junction after unilateral iliac crest harvest. Spine (Phila Pa 1976). 2001;26:1950-1955.
14. Orchowski J., Polly D.W.Jr, Klemme W.R., et al. The effect of kyphosis on the mechanical strength of a long-segment posterior construct using a synthetic model. Spine (Phila Pa 1976). 2000;25:1644-1648.
15. Gardner V.O., Armstrong G.W. Long-term lumbar facet joint changes in spinal fracture patients treated with Harrington rods. Spine (Phila Pa 1976). 1990;15:479-484.
16. Benzel E.C. Short segment compression instrumentation for selected thoracic and lumbar spine fractures: the short-rod-two claw (SRTC) technique. J Neurosurg. 1993;79:335-340.
17. Guven O., Kocaoglu B., Bezer M., et al. The use of screw at the fracture level in the treatment of thoracolumbar burst fractures. J Spinal Disord Tech. 2009;22:417-421.
18. Mahar A., Kim C., Wedemeyer M., et al. Short-segment fixation of lumbar burst fractures using pedicle fixation at the level of the fracture. Spine (Phila Pa 1976). 2007;32:1503-1507.
19. McLain R.F., Sparling E., Benson D.R. Early failure of short-segment pedicle instrumentation for thoracolumbar fractures: a preliminary report. J Bone Joint Surg [Am]. 1993;75:162-167.
20. McLain R.F. The biomechanics of long versus short fixation for thoracolumbar spine fractures. Spine (Phila Pa 1976). 2006;31(suppl 11):S70-S79.
21. Brodke D.S., Bachus K.N., Mohr R.A., Nguyen B.N. Segmental pedicle screw fixation or cross-links in multilevel lumbar constructs: a biomechanical analysis. Spine J. 2001;1(5):373-379.
22. Dick J.C., Jones M.P., Zdeblick T.A., et al. A biomechanical comparison evaluating the use of intermediate screws and cross-linkage in lumbar pedicle fixation. J Spinal Disord. 1994;7:402-407.
23. Ruland C.M., McAfee P.C., Warden K.E., et al. Triangulation of pedicular instrumentation: a biomechanical analysis. Spine (Phila Pa 1976). 1991;16:S270-S276.
24. Wood K.B., Wentorf F.A., Ogilvie J.W., Kim K.T. Torsional rigidity of scoliosis constructs. Spine (Phila Pa 1976). 2000;25:1893-1898.
25. Shono Y., McAfee P.C., Cunningham B.W. Experimental study of thoracolumbar burst fractures. Spine (Phila Pa 1976). 1994;15:1711-1722.
26. Mann K.A., McGowan D.P., Fredrickson B.E., et al. A biomechanical investigation of short segment spinal fixation for burst fractures with varying degrees of posterior disruption. Spine (Phila Pa 1976). 1990;15:470-478.
27. Wei F.X., Liu S.Y., Liang C.X., et al. Transpedicular fixation in management of thoracolumbar burst fractures—monosegmental fixation versus short-segment instrumentation. Spine (Phila Pa 1976). 2010;35:E714-E720.
28. Erickson M.A., Baulesh D.M. Lowest instrumented vertebra selection in AIS. J Pediatr Orthop. 2011;31(suppl 1):S69-S76.