Chapter 11 Therapeutic Epidural Injections
Interlaminar and Transforaminal
 Best practice of nonsurgical radicular pain syndromes is yet to be defined. Few comparative nonsurgical trials have been conducted.
Best practice of nonsurgical radicular pain syndromes is yet to be defined. Few comparative nonsurgical trials have been conducted. Because of the rare but catastrophic nature of some of these complications with the favorable natural history of discogenic radicular pain, optimization of safety should be of primary concern.
Because of the rare but catastrophic nature of some of these complications with the favorable natural history of discogenic radicular pain, optimization of safety should be of primary concern. Future directions in research could look at alternative pharmacological agents or techniques to address the pathophysiology of radicular pain syndromes.
Future directions in research could look at alternative pharmacological agents or techniques to address the pathophysiology of radicular pain syndromes. Transforaminal epidural techniques place the medication in the anterior epidural space nearer the putative site of pathology.
Transforaminal epidural techniques place the medication in the anterior epidural space nearer the putative site of pathology. Digital subtraction angiography techniques are a simple and inexpensive addition to conventional fluoroscopy and may be useful in complication reduction from inadvertent vascular injection.
Digital subtraction angiography techniques are a simple and inexpensive addition to conventional fluoroscopy and may be useful in complication reduction from inadvertent vascular injection. Infectious risks may be mitigated by strict aseptic technique, including a chlorhexidine-based scrub, mask, hand asepsis (surgical wash), and caution in high-risk patients.
Infectious risks may be mitigated by strict aseptic technique, including a chlorhexidine-based scrub, mask, hand asepsis (surgical wash), and caution in high-risk patients.Introduction
The use of therapeutic epidural injections for the treatment of sciatica with back and leg pain dates back approximately 80 years. Initially, therapeutic epidurals were predominately transsacral (caudal) injections of local anesthetics such as procaine.1 After the introduction of corticosteroids into clinical practice,2 researchers in Europe were the first to inject corticosteroids into the epidural space.3,4 The techniques of administration have gradually been modified, with early use of higher volume caudal epidural injections eventually being largely replaced, first by level-specific interlaminar epidural injections and second by transforaminal epidurals performed with fluoroscopic guidance. Despite the increasing sophistication and advances in the techniques of steroid injection, a number of authors still question the role of these injections for the therapy of sciatica. In particular, two physician specialties (neurology and occupational medicine) have published guidelines or reviews suggesting that these injections are performed too often with uncertain results.5,6 Other authors are beginning to examine the role of alternate compounds such as etanercept for the treatment of sciatica based on the underlying pathophysiology.7 Finally, a recent head-to-head trial of several conservative treatments (including injections in some) compared with surgical therapies was performed demonstrating the superiority of surgery, at least in the first year.8 This trial augmented the previous large-scale trials comparing surgical with nonsurgical therapies.9,10 This chapter discusses the current role of therapeutic epidural injections.
Basic Science
Radiculopathy is most commonly associated with intervertebral disc herniation and likely includes two distinct pathways: mechanical compression and cytokine-mediated radiculitis.11 Mechanical impingement may induce poor tissue oxygen delivery to the spinal (radicular) nerve, resulting in an inadequate nutritional supply and decreasing the vascular perfusion to critical levels. Interestingly, however, mechanical compression alone may not result in pain.12,13 Radiculopathy describes neurological conduction loss (sensory or motor) occurring secondary to mechanical impingement or compression (e.g., disc protrusion, herniation, or extrusion) pressing on the spinal nerve in the foramina. Other common causes of radiculopathy include spondylosis, vertebral subluxation, and ligamentum flavum hypertrophy or thickening.14 Abnormal nerve conduction may manifest as sensory loss, depressed spinal reflexes, or motor deficits. Radicular pain may occur concomitantly with radiculopathy or separately. The pain is thought to be an inflammatory phenomenon induced by neurochemical products such as cytokines. Cytokines are produced by spinal glia. They include tumor necrosis factor-α (TNF-α) and several interleukins. Herniated nucleus pulposus may induce the release of such inflammatory mediators, leading to a chemical radiculitis. Olmarker et al15 found that the application of a homogenate of disc material onto porcine cauda equina induced functional and morphologic changes in those nerves. Then Igarashi and colleagues16 reported that in a rat model, TNF-α applied to the dorsal root ganglia produced functional and morphological changes that were identical to that seen with nucleus pulposus material. Burke et al17 found increased levels of the inflammatory cytokines interleukin-6 (IL-6) and IL-8 in disc material taken from patients with known disc disease. Finally, further study produced compelling evidence that TNF-α inhibitors could reduce the histological and functional changes caused by nucleus pulposus material. These studies cemented the concept that TNF-α and other cytokines were causative agents in the development of radiculitis and further suggested an entirely new pharmacological treatment strategy for patients with sciatica.18
Discogenic pain is another pathological condition for which epidural therapies are occasionally tried. Discogenic pain is unlike radicular pain in that the patient will predominately complain of low back pain without significant leg involvement that is exacerbated by the sitting position, spinal flexion, heavy lifting, or other stresses. The intervertebral disc is a very poorly vascularized structure that receives nutrients primarily by diffusion. Intervertebral disc innervation is complex, arising primarily from nerve ingrowth through the vertebral endplate into the outer third of the disc annulus. Nerve fiber types in the annulus fibrosis are peptidergic, using neurotransmitter substances such as calcitonin gene-related peptide. Nerve fibers are small and follow new blood vessels.19
Indications and Contraindications
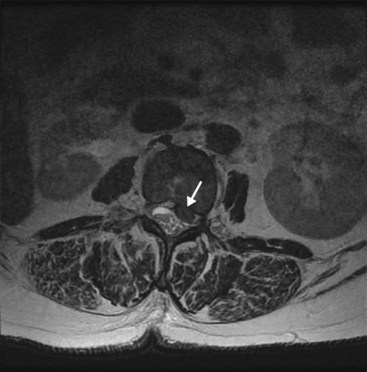
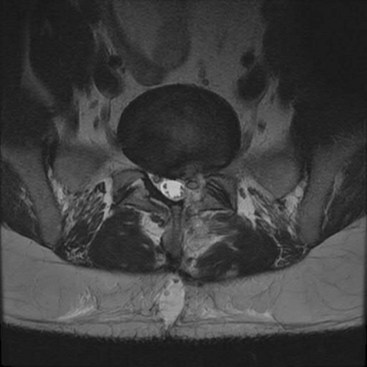
Therapeutic epidurals are generally used in three major instances: (1) for the symptomatic treatment of radicular pain secondary to an intervertebral disc herniation, protrusion, or extrusion causing a combination of back and leg pain in a characteristic dermatomal pattern (Fig. 11-1); (2) spinal stenosis presenting with symptoms of neurogenic claudication, radicular pain, or mixed pain (Fig. 11-2); and (3) postoperative back and leg pain caused by recurrent disc material, granulation tissue or scarring, or other causes (Fig. 11-3). In some cases, therapeutic epidural injections may also be performed in cases of discogenic pain or for tumor-related nerve pain when a radicular syndrome is manifested by the tumor growth into the foramen or around the exiting spinal nerve (Fig. 11-1). How these therapeutic procedures are applied is also somewhat variable depending on regional variations in the use of initial conservative therapies, the specialty of origin of the managing clinician, and the availability of clinicians capable to do therapeutic epidurals. However, population-based examinations of therapeutic epidural injections have not demonstrated any long-term advantage to their use in terms of reduced surgical volumes or enhanced functionality.20
Spinal stenosis is most commonly acquired but can be congenital. Large studies are lacking for results of therapeutic epidural injections. The natural history of spinal stenosis is reassuring, however. Johnsson and colleagues21 demonstrated that older patients with spinal stenosis commonly presented with low back pain (100%), claudication (75%), radicular pain (12.5%), and mixed symptoms (12.5%). Interestingly, the patients with spinal stenosis did not appear to worsen significantly over a 4-year period, with equal numbers showing improvement as progression.
Patients with worse clinical and functional symptoms most often had surgical laminectomy without fusion. At 8 to 10 years, the patients treated with either surgical or nonsurgical approaches had similar rates of satisfaction with current state, back pain incidence, and symptom improvement. Patients with initial surgical treatment had better leg pain and functional status. Overall, the results suggested that patients may be optimally managed in a shared decision model.22
Imaging
Numerous studies have demonstrated that a high percentage of patients who are clinically asymptomatic will have significant findings on magnetic resonance imaging (MRI).23 In most cases, the MRI should be read before proceeding with the injection and is mandatory before cervical epidurals. The size of the spinal canal, presence of intervertebral disc protrusion or extrusion, any neural impingement, presence of degenerative changes, or any possible abnormality in the path of the proposed needle placement will need to be accounted for.
The high rate of false-positive scans mandates an approach to patient evaluation that requires a large degree of concordance among the imaging, electrodiagnostic testing, the history, and the physical examination. In some cases, a diagnostic spinal nerve injection to independently verify which root is involved in pain generation is requested before surgical intervention. Studies performed more than 2 decades ago were the first to suggest that image guidance could significantly improve the accuracy of epidural administration of medication.24 Johnson et al25 later published 5489 consecutive injections performed with fluoroscopic guidance with contrast injection. Their results suggested an extremely safe conduct of these outpatient injections could be accomplished with a high degree of accuracy and precision.
Guidelines
The American Pain Society Clinical Practice Guideline for Low Back Pain is one of the more recent published guidelines.26 The authors reviewed randomized controlled trials and systematic reviews that met the following criteria: (1) published in English language or included in an English language review; (2) evaluated adult patients who were not pregnant and had back or leg pain or both; (3) evaluated a targeted interventional therapy; and 4) reported specific outcomes such as back function, health status, work disability, or patient satisfaction. A total of 1331 study citations were reviewed of which 105 met inclusion criteria. In addition, 58 full text reviews yielded 30 that met inclusion criteria. The guideline statements supported fair evidence that epidural steroid injections yielded short-term benefit for radiculopathy caused by disc prolapse but were inferior to surgery. Chymopapain chemonucleolysis injections for radiculopathy were supported by good evidence, but this therapy is no longer used in the United States because of uncommon severe allergic reactions. The guidelines overall conclusions were that few nonsurgical interventions have been shown to be effective.
The American Society of Interventional Pain Physicians also published guidelines regarding the use of interventional techniques in chronic spinal pain.27 These guidelines also rigorously evaluated available literature using an evidence grading system from the United States Preventative Services Task Force criteria with five levels of evidence. Their findings were supportive of level I for caudal epidural injections for radiculitis or discogenic pain without radiculitis. The level of evidence for cervical thoracic and lumbar epidurals for managing radiculitis was level II-1 or II-2.
The American Society of Anesthesiologists also recently updated its practice guidelines. The purpose of these guidelines is to promote optimized pain control, improved functionality, enhanced quality of life, and minimized adverse effects of therapies. No specific outcomes were warranted by the task force. The guidelines endorse epidural steroids with or without local anesthetic injection for relief of back pain for periods of 2 weeks to 3 months (Category B2 evidence), and neck pain relief for periods of 1 week to 12 months (Category B3 evidence). Image guidance was suggested as representative of current best practice.28
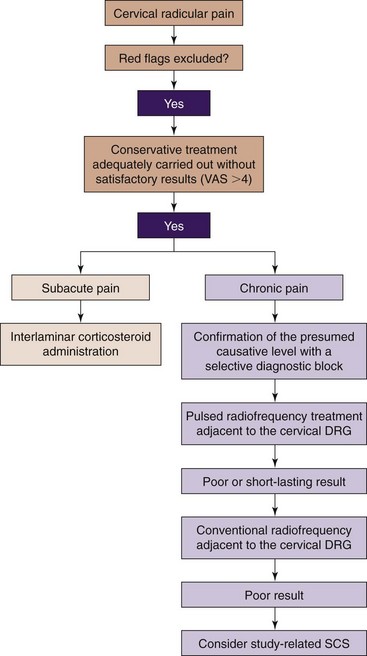
Guidelines have been published for cervical radicular pain as well by the World Institute of Pain. A clinical algorithm for management recommends interlaminar epidural corticosteroid injections for subacute radicular pain and pulsed radiofrequency adjacent to the dorsal root ganglion for more chronic pain (Fig. 11-4).29 Cervical transforaminal epidurals are not recommended because of complications and a small negative controlled trial.30,31
Outcomes Evidence
A study by Carette and colleagues32 has been regarded highly by reviewers in several recent guidelines committees. They performed a randomized, placebo-controlled trial examining up to three lumbar interlaminar epidural steroid injections for sciatica. A total of 158 patients received injections for unilateral or bilateral lower extremity pain. Patients had signs of nerve root irritation or compression and computed tomographic (CT) evidence of appropriate level nerve root compression. Patients received either methylprednisolone or saline. Functionality was the primary outcome measure based on Oswestry Disability Index (ODI). Major criticisms of the study were the lack of fluoroscopic guidance and the large injectate volume (8 mL) compared with 1 mL of isotonic saline in the control epidural injection group. The study demonstrated no statistically significant change in functional improvement using ODI scores but did find that leg pain was reduced at 6 weeks in the corticosteroid treatment group (difference in mean change of −0.11; 95% confidence interval, −21.1 to −0.9; P = .03), with a treatment effect no longer present at 3 months.
Karppinen and colleagues33 performed a randomized, double-blind trial to test the efficacy of periradicular steroid injections for sciatica. A total of 163 patients with unilateral lower extremity pain were studied. Although MRI was recorded, concordant imaging was not a study requirement for inclusion. A total of 80 patients in each group were randomized, and they received either methylprednisolone (80-120 mg) or saline. The primary outcome measure in this study was back and leg pain visual analogue scale. Three patients were not randomized because a contrast outline of the involved spinal nerve could not be obtained. The authors did not comment on contrast spread to the anterior epidural space. The results showed short-term improvement for leg pain in the steroid–bupivacaine group at 2 weeks. Reduced leg pain was 45% versus 24% for the placebo (P <.01) group. Back pain was better in the steroid group at 3 months. No difference between groups was seen at 1 year. Only one injection was evaluated for this study. This has been criticized by some because they theorize that additional injections may have augmented the response.
Riew et al34 performed a randomized controlled trial of fluoroscopically-guided lumbar transforaminal epidural steroid injections compared with local anesthetic injection. The need for lumbar spine surgery was the primary outcome. The 55 patients studied had lower extremity pain and imaging confirmation foraminal impingement. A total of 28 patients received a betamethasone and bupivacaine injection compared with 27 patients who received bupivacaine transforaminal injection only. Patients treated with betamethasone had a reduction in need for surgery compared with the local anesthetic group. A later review of the same cohort of patients revealed that those who did not have surgery during the original study period were still able to avoid surgery several years later.
Manchikanti et al35–38 assessed the utility of adding corticosteroid to local anesthetic for caudal epidural injections in a randomized and blinded fashion. Four patient groups were separately studied according to the etiology of their pain: discogenic, radicular, postlaminectomy, or spinal stenosis. More than 200 patients were included in their four studies. Injections were 10 mL total volume containing lidocaine 0.5% and either 6 mg of betamethasone or 40 mg of methylprednisolone. All injections were performed with fluoroscopic guidance. On average, pain and functional status improved in all four groups at 12 months of follow-up regardless of whether they received corticosteroid. Patients could be divided into responders or nonresponders within two injections, generally. Interestingly, patients with spinal stenosis showed similar improvement to a group receiving lumbar spine surgery in a study by Weinstein et al.39
Ackerman and Ahmad40 randomized 90 patients with lumbar radicular pain caused by disc herniation to receive up to three caudal, interlaminar, or transforaminal epidural injections under fluoroscopic guidance. Each injection included 40 mg of triamcinolone in saline (20 mL total for caudal injections and 4 mL total volume for interlaminar or transforaminal injections). At 6 months, three or fewer patients in the caudal or interlaminar groups had complete pain relief versus nine patients in the transforaminal group with complete relief. Patients with no pain relief were less common in the transforaminal group compared with the other groups. The authors concluded that the transforaminal route was superior because it was more likely to result in placement of the steroid in the anterior epidural space, the putative site of pathology.
Two randomized trials of cervical epidural steroid injections have been performed. Anderberg et al31 compared selective nerve root proven cases of radiculitis that were randomized to either corticosteroid or local anesthetic alone. No significant differences were noted between groups. In an older study of interlaminar epidural corticosteroid administration for cervicobrachial pain, Stav et al41 demonstrated short-term improvement in a small study of patients receiving lidocaine and steroid epidural injections. Range of motion, work status, and pain relief were superior in the epidural steroid group. Vallee et al42 performed fluoroscopically-guided transforaminal epidural steroid injection on 34 levels for 32 patients with radicular pain caused by herniated disc or spinal stenosis. After needle placement, aspiration was performed to assist in the identification of vascular or intrathecal placement, but no contrast dye was injected. Prednisone 100 mg without local anesthetic was then injected. No complications were observed, and patients were improved at 2 weeks and 6 months. This technique is more likely to result in complications and should not be replicated (see Complications section).
Equipment and Technique
Cervical Transforaminal
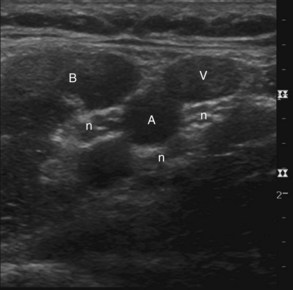
The patient is placed in the supine position with the head turned slightly opposite to the side being targeted. Depending on the angle of the flat detector or image intensifier of the fluoroscope, the optimal angle of skin entry can vary. One should mark the location of the external jugular vein and both carotid artery and internal jugular veins to avoid transgressing these structures. The surface of the skin should be superficially prepared with chlorhexidine and alcohol solution (superior to iodinated agents) and sterilely draped. Some operators choose blunt needles, some use Quincke beveled needles with the distal tip slightly curved, and others use Whitacre pencil point needles. A newer product that has a needle and catheter system designed to avoid vascular penetration has been recently marketed. No studies to date have compared whether one type of needle or whether a needle and catheter combination is superior to another in terms of the incidence of vascular penetration or catastrophic complications. A subcutaneous skin wheal is raised, and either a 25- or 22-gauge needle is selected for a coaxial fluoroscopic technique. The transverse oblique view of the intervertebral foramina should be adjusted to optimize the maximal circumference of the foramina. One approach targets the equatorial posterior aspect of the foramen, touching the superior articular process (SAP) at the posterior aspect of the foramen. The author generally targets the junction of the posterior middle third and posterior superior third of the foramen. From the SAP, the needle is “walked” into the posterior aspect of the foramen as above, making sure that an anteroposterior (AP) projection does not show the needle tip extending beyond the midsagittal plane of the cervical articular pillar.4 The ascending and deep cervical arteries seem to enter in the more inferior aspect of the foramen and are larger at the outer aspect of the foramen. When the needle is in position, various safety measures are used, as discussed in the Complications section, including local anesthetic test dosing, real-time fluoroscopic contrast injections, and digital subtraction techniques.
Transforaminal Lumbar Epidural
The patient is placed in the prone position on the fluoroscopy table, and an oblique view is obtained with the SAP bisecting the vertebral body of the level above. The inferior aspect of the pedicle at the sagittal bisector is targeted, at approximately the 6:00 position of the pedicle at the same level. A chlorhexidine/alcohol-based prep solution is applied to sterilize the area, and sterile drapes are applied around the skin entry site. One issue of importance is the length of the needle. The authors usually use a 22- or 25-gauge 3.5-inch Quincke tip needle with a distal bend. However, many patients require a 5-inch or longer needle depending on body habitus. A skin wheal and subcutaneous infiltration, usually 1% lidocaine, allows initial needle entry, with some opting for blunt needles. Nonionic contrast injection of 0.2 to 1.0 cc should demonstrate a neurogram as well as epidural spread medially and outlining the pedicle. Digital subtraction is used to substantiate lack of vascular uptake (Fig. 11-5). Local anesthetic test dosing with 1 cc of 1% lidocaine is also useful to prevent accidental administration of corticosteroid particulate into a feeder artery to the anterior spinal artery. Nonparticulate steroid may be used to further prevent complications.
Risk and Complication Avoidance
Infectious Complications
In the modern era after the introduction of MRI, the spontaneous risk of epidural abscess has been reported at 0.88 persons per 100,000 per year. Most patients who develop abscesses in the spine are immunocompromised, and Staphylococcus species are most prevalent.43 Gaul et al44 reported on the cases of meningitis admitted to a neurological intensive care unit over an 8-year span during the years 1992 to 2000. Interestingly, eight of 128 patients had recently received corticosteroid spinal injections. Patients usually present within 2 weeks with worsening axial pain. A high degree of suspicion is warranted, and MRI imaging should be arranged in emergent fashion because surgical exploration and decompression may be necessary. Laboratory findings (erythrocyte sedimentation rate and C-reactive protein) may be far more helpful than granulocyte counts in the initial evaluation.
Ischemic Complications
It has become apparent over the past decade that some apparent vascular events may be increasing in frequency and that particulate steroids might be involved through embolization of the spinal cord and brainstem, resulting in brain or spinal cord infarction. Scanlon et al30 performed a survey of members of the American Pain Society in an attempt to glean some idea of how prevalent these complications might be. Several fatalities were reported,45,46 suggesting that caution in performing transforaminal injections should be extremely high. Previous authors had documented that the blood supply is variable and that segmental medullary vessels in the cervical region might arise from the deep or ascending cervical arteries (or both) in addition to the vertebral arteries.47 Baker et al48 were the first to suggest that a sequence of safety measures should be considered, including real-time contrast injection, digital subtraction techniques, and test dosing. A recent case report49 suggests that these cases are indeed embolic events and that they may not be confined to epidural injections but involve virtually any cervical injection in areas of critical arteries.
Needle Injuries
The most dreaded complications in the cervical spine area may well be a needle stick into the cervical spinal cord. Although these are uncommon, one should routinely examine the MRI imaging before performing an interlaminar injection to make sure that there is adequate area for the needle to enter the epidural space. Case reports of spinal injury50 suggest that this is a necessary step. The ligamentum flavum is discontinuous above the upper thoracic region, so a characteristic loss of resistance may be absent.51 A lateral radiograph may be helpful in determining depth of the needle after assuring that the needle is coaxial in the AP image (Fig. 11-6).52
1 Evans W. Intrasacral epidural injection in the treatment of sciatica. Lancet. 1930:1225-1229.
2 Hench PS, Kendall EC, Slocumb CH, et al. The effect of a hormone of the adrenal cortex (17-hydroxy-11-dehydrocorticosterone: Compound E) and of pituitary adrenocorticotropic hormone on rheumatoid arthritis. Proc Staff Meet Mayo Clin. 1949;24:181-197.
3 Robecchi A, Capra R. Ľ idrocortisone (composto F). Prime esperienze cliniche in campo reumatologico. Minerva Med. 1952;98:1259-1263.
4 Li’evre JA, Bloch-Michel H, Pean G, et al. Ľ hydrocortisone en injection locale. Rev Rheum. 1953;20:310-311.
5 Armon C, Argoff CE, Samuels J, Backonja M-M. Assessment: use of epidural steroid injections to treat radicular lumbosacral pain: report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology. 2007;68:723-729.
6 American College of Occupational and Environmental Medicine (ACOEM). Low back disorders. Occupational medicine practice guidelines: evaluation and management of common health problems and functional recovery of workers, ed 2. Elk Grove Village, IL: American College of Occupational and Environmental Medicine. 2007.
7 Cohen SP, Bogduk N, Dragovich A, et al. Randomized, double- blind, placebo-controlled, dose- response, and pre-clinical safety study of transforaminal epidural etanercept for the treatment of sciatica. Anesthesiology. 2009;110:1116-1126.
8 Weinstein JN, Tosteson TD, Lurie JD, et al. Surgical vs nonoperative treatment for lumbar disk herniation The Spine Patient Outcomes research Trial (SPORT): a randomized trial. JAMA. 2006;296:2441-2450.
9 Weber H. Lumbar disc herniation. A controlled, prospective study with ten years of observation. Spine. 1983;8:131-140.
10 Atlas S, Keller R, Wu Y, et al. Long-term outcomes of surgical and nonsurgical management of sciatica secondary to lumbar disc herniation: 10 year results from the Maine Lumbar Spine Study. Spine. 2005;30:927-935.
11 Rhee JM, Schaufele M, Abdu WA. Radiculopathy and the herniated lumbar disc. Controversies regarding pathophysiology and management. J Bone Joint Surg Am. 2006;88:363-370.
12 Kuslich SD, Ulstrom CL, Michael CJ. The tissue origin of low back pain and sciatica: a report of pain response to tissue stimulation during operations on the lumbar spine using local anesthesia. Orthop Clin North Am. 1991;22:181-187.
13 Kawakami M, Tamaki T, Hayashi N, et al. Mechanical compression of the lumbar nerve root alters pain related behaviors induced by the nucleus pulposus in the rat. J Orthop Res. 2000;18:257-264.
14 Bogduk N. Clinical anatomy of the lumbar spine and sacrum, ed 3. Edinburgh: Churchill Livingstone; 1997.
15 Olmarker K, Rydevik B, Nordborg C. Autologous nucleus pulposus induces neurophysiologic and histologic changes in porcine cauda equine nerve roots. Spine. 1993;18:1425-1432.
16 Igarashi T, Kiduchi S, Shubayev V, et al. Exogenous tumor necrosis factor-alpha mimics nucleus pulposus-induced neuropathology. Molecular, histologic, and behavioural comparisons in rats. Spine. 2000;25:2975-2980.
17 Burke JG, Watson RWG, McCormack D, et al. Intervertebral discs which cause low back pain secrete high levels of proinflammatory mediators. J Bone Joint Surg. 2002;84:196-201.
18 Olmarker K, Rydevik B. Selective inhibition of tumor necrosis factor-alpha prevents nucleus induced thrombus formation, intraneural edema, and reduction of nerve conduction velocity: possible implications for future pharmacologic treatment strategy of sciatica. Spine. 2001;26:863-869.
19 Brown MF, Hukkanen MVJ, McCarthy ID, et al. Sensory and sympathetic innervation of the vertebral endplate in patients with degenerative disc disease. J Bone Joint Surgery Br. 1997;79:147-153.
20 Friedly J, Chan L, Deyo R. Increases in lumbosacral injections in the Medicare population: 1994 to 2001. Spine. 2007;32:1754-1760.
21 Johnsson KE, Rosen I, Uden A. The natural course of lumbar spinal stenosis. Clin J Orthop Rel Res. 1992;279:82-86.
22 Atlas SJ, Keller RB, Wu YA, et al. Long term outcomes of surgical and non-surgical management of lumbar spinal stenosis: 8 to 10 year results from the Maine lumbar spine study. Spine. 2005;30:936-943.
23 Boden SD, Davis DO, Dina TS, et al. Abnormal magnetic resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation. J Bone Joint Am. 1990;72:403-408.
24 el-Khoury GY, Ehara S, Weinstein JN, et al. Epidural steroid injection: a procedure ideally performed with fluoroscopic control. Radiology. 1988;168:554-557.
25 Johnson BA, Schellhas KP, Pollei SR. Epidurography and therapeutic epidural injections: technical considerations and experience with 5334 cases. Am J Neuroradiology. 1999;20:697-705.
26 Chou R, Atlas SJ, Stanos SP, Rosenquist RW. Nonsurgical interventional therapies for low back pain: a review of the evidence for an American Pain Society Clinical Practice Guideline. Spine. 2009;34:1078-1093.
27 Manchikanti L, Boswell MV, Singh V, et al. Comprehensive evidence-based guidelines for interventional techniques in the management of chronic spinal pain. Pain Physician. 2009;12:699-802.
28 American Society of Anesthesiologists. Practice guidelines for chronic pain management: an updated report by the American Society of Anesthesiologists Task Force on Chronic Pain Management and the American Society of Regional Anesthesia and Pain Medicine. Anesthesiology. 2010;112:810-833.
29 Van Zundert J, Huntoon M, Patijn J, et al. Cervical radicular pain. Pain Pract. 2010;10:1-17.
30 Scanlon GC, Moeller-Bertram T, Romanowsky SM, Wallace MS. Cervical transforaminal epidural injections: more dangerous than we think. Spine. 2007;11:1249-1256.
31 Anderberg L, Annertz M, Persson L, et al. Transforaminal steroid injections for the treatment of cervical radiculopathy: a prospective and randomized study. Eur Spine J. 2007;16:321-328.
32 Carette S, Leclaire R, Marcoux S, et al. Epidural corticosteroid injections for sciatica due to herniated nucleus pulposus. N Engl J Med. 1997;336:1634-1640.
33 Karppinen J, Malmivaara A, Kurunlahti M, et al. Periradicular infiltration for sciatica: a randomized controlled trial. Spine. 2001;26:1059-1067.
34 Riew KD, Yin Y, Gilula L, et al. The effect of nerve- root injections on the need for operative treatment of lumbar radicular pain: A prospective, randomized, controlled, double-blind study. J Bone Joint Surgery Am. 2000;82:1589-1593.
35 Manchikanti L, Cash KA, McManus CD, et al. Preliminary results of randomized equivalence trial of caudal epidural injections in managing chronic low back pain: part 1. Discogenic pain without disc herniation or radiculitis. Pain Physician. 2008;11:785-800.
36 Manchikanti L, Singh V, Cash KA, et al. Preliminary results of randomized equivalence trial of caudal epidural injections in managing chronic low back pain; part 2. Disc herniation and radiculitis. Pain Physician. 2008;11:801-815.
37 Manchikanti L, Singh VJ, Cash KA, et al. Preliminary results of randomized equivalence trial of caudal epidural injections in managing chronic low back pain: part 3. Post-surgical syndrome. Pain Physician. 2008;11:817-831.
38 Manchikanti L, Cash KA, McManus CD, et al. Preliminary results of randomized equivalence trial of fluoroscopic caudal epidural injections in managing chronic low back pain: part 4. Spinal stenosis. Pain Physician. 2008;11:833-848.
39 Weinstein JN, Tosteson TD, Lurie JD, et al. Surgical versus nonsurgical therapy for lumbar spinal stenosis. N Engl J Med. 2008;358:794-810.
40 Ackerman WE, Ahmad M. The efficacy of lumbar epidural steroid injections in patients with lumbar disc herniations. Anesth Analg. 2007;104:1217-1222.
41 Stav A, Ovadia L, Sternberg A, et al. Cervical epidural steroid injection for cervicobrachialgia. Acta Anaesthesiol Scand. 1993;37:562-566.
42 Vallee JN, Feydy A, Carlier RY, et al. Chronic cervical radiculopathy: lateral-periradicular corticosteroid injection. Radiology. 2001;218:886-892.
43 Ptaszynski AE, Hooten WM, Huntoon MA. The incidence of spontaneous epidural abscess in Olmsted County from 1990-2000: a rare cause of spinal pain. Pain Med. 2007;8:338-343.
44 Gaul C, Neundorfer B, Winterholler M. Iatrogenic (para)spinal abscesses and meningitis following injection therapy for low back pain. Pain. 2005;116:175-176.
45 Brouwers PJAM, Kottink EJBL, Simon MAM, Prevo RL. A cervical anterior spinal artery syndrome after diagnostic blockade of the right C6 nerve rood. Pain. 2001;91:397-399.
46 Rozin L, Rozin R, Koehler SA, et al. Death during transforaminal epidural steroid nerve root block (C7) due to perforation of the left vertebral artery. Am J Forensic Med Pathol. 2003;24(4):351-355.
47 Huntoon MA. Anatomy of the cervical intervertebral foramina: vulnerable arteries and ischemic neurologic injuries after transforaminal epidural injections. Pain. 2005;117:104-111.
48 Baker R, Dreyfuss P, Mercer S, Bogduk N. Cervical transforaminal injection of corticosteroids into a radicular artery: a possible mechanism for spinal cord injury. Pain. 2003;103:211-215.
49 Edlow BL, Wainger BJ, Frosch MP, et al. Posterior circulation stroke after c1-2 intraarticular facet steroid injection: evidence for diffuse microvascular injury. Anesthesiology. 2010;112:1532-1535.
50 Field J, Rathmell JP, Stephenson JH, Katz NP. Neuropathic pain following cervical epidural steroid injection. Anesthesiology. 2000;93:885-888.
51 Lirk P, Kolbitsch C, Putz G, et al. Cervical and high thoracic ligamentum flavum frequently fails to fuse in midline. Anesthesiology. 2003;99:87-90.
52 Huntoon MA. Cervical spine: case presentation, complications and their prevention. Pain Med. 2008;9(suppl):S35-S40.