Chapter 41 The Traumatized Airway
I Defining the Problem
A The Clinical Challenge
2 Early Hospital Care of the Traumatized Patient
Trauma and burn patients frequently undergo surgery that is not related to their acute resuscitation but is required during the first few days of their hospital stay. Burn débridement and grafting, fracture fixation, complex wound revision and repair, and other procedures are often required hours or days after the patient has been stabilized and more acute, life-threatening problems have been controlled. Decision making in this setting is easier with respect to airway management because the decision to intubate is driven by the need for surgery and anesthetic management; however, careful preoperative assessment remains essential. In addition to the usual comorbidities that can make airway management difficult, trauma patients often have other complicating factors, such as direct airway injury, pulmonary injury with rapid oxyhemoglobin desaturation, persistently tenuous hemodynamic status, or cerebral injury with elevated intracranial pressure (ICP). Patients with significant total body surface area burns, crush injuries, or spinal cord injuries develop acetylcholine receptor upregulation, with its attendant risk of hyperkalemia if succinylcholine is administered.1 Although classic teaching posits that this vulnerability to succinylcholine-induced hyperkalemia begins on postinjury day 7, some effect is seen as early as day 3.2 This combination of considerations—specifically unresolved or unrecognized traumatic injuries, the potential for hyperkalemia, and the patient’s preexisting comorbidities—can make airway management in this intermediate-term window anything but routine. A careful approach, including detailed consideration of possible difficult airway management protocols and relevant comorbidities, is essential.
B The Decision to Intubate
Answers to three fundamental questions inform the decision to undertake emergency intubation:
1. Is there a failure to maintain or protect the airway?
2. Is there a failure of oxygenation or ventilation?
3. Is there a need for intubation based on the anticipated clinical course?
The gag reflex is much less reliable than phonation and swallowing, and it is absent in up to 25% of the normal adult population.3 The presence of a gag reflex does not equate to airway protection, nor does its absence indicate a need to intubate. The presence or absence of the gag reflex is better thought of as a neurologic evaluation (i.e., cranial nerves IX and X) rather than as part of an airway evaluation. The Glasgow Coma Scale is a better tool for predicting intubation.4
Most trauma patients can maintain and protect their airways and exhibit adequate or correctable oxygenation and ventilation. For them, it is the anticipated clinical course that guides the decision to intubate. This is the most sophisticated and most important of the decisions facing the airway manager or trauma captain. A patient may appear stable at the time of evaluation, but deterioration can be predicted as a natural course of the injuries. For example, the patient with burns from a closed-space fire with significant inhalation of superheated air (see Chapter 44) may present with a somewhat hoarse voice or a simple cough but has an otherwise patent airway. Failing to recognize the likelihood of progressive obstruction of the airway, which has been subjected to toxic and thermal insults, and to intervene in a timely fashion can lead to disaster. Although the patient may not meet the criteria for emergency intubation related to airway maintenance and protection, oxygenation, or ventilation, the likelihood of deterioration is alone sufficient to warrant airway intervention.5 It is the predictability of the deterioration that determines the decision to intubate. Alternatively, the upper airway can be examined by fiberoptic laryngoscopy, informing the airway manager of the stability or fragility of airway patency. Similarly, the patient with a crushed pelvis, open femur fracture, and hypotension is inevitably intubated, even though there is no immediate threat to airway patency or oxygenation. The need for advanced imaging, aggressive pain control, and operative repair of obvious injuries dictates that the patient be intubated early and in a more controlled fashion than trying to manage a chaotic intubation from behind the computed tomography (CT) scanner.
II Anatomy of the Airway: Trauma Considerations
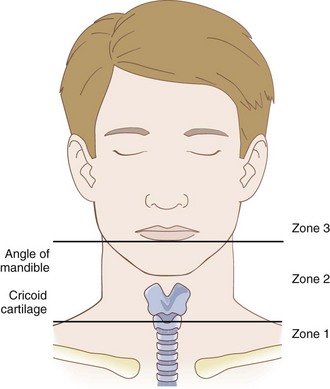
Although airway anatomy is discussed in Chapter 1, the following is a brief description of elements to consider in the trauma setting. The airway begins at the nares or lips and ends with the terminal bronchioles and alveoli of the lungs. The upper airway consists of the oral and nasal cavities and the pharynx, which provide a conduit for the movement of gases to the larynx, through the glottis, and into the trachea. The nasopharynx, oropharynx, and hypopharynx (Fig. 41-1) form a continuous space that conducts air from the outside world to the glottic aperture. The nasopharynx is protected anteriorly and laterally by the maxillary bones, the nasal bones, and nasal cartilage. Direct injury to the face, particularly from an impact with an object of high mass, high velocity, and low surface area (e.g., baseball bat), can collapse the maxillary structures into the nasopharynx and cause extensive hemorrhage, threatening the airway and complicating attempts to manage it. Similarly, the oropharynx is protected by the maxillary bones, alveolar ridges, and mandible but is subject to the same sort of intrusive injuries. Blows to the face producing Le Fort I, II, or III fractures (Fig. 41-2) can simultaneously threaten the airway and complicate airway management.
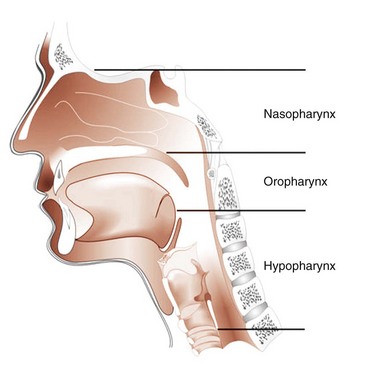
Figure 41-1 Airway anatomy.
(From Redden RJ: Anatomic considerations in anesthesia. In Hagberg CA, editor: Handbook of difficult airway management, Philadelphia, 2000, Churchill Livingstone, p 11.)
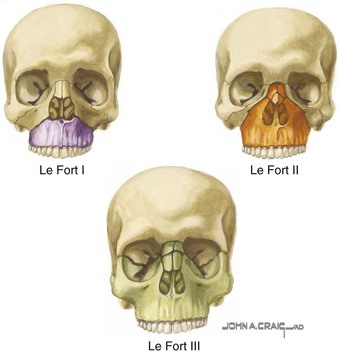
Figure 41-2 Le Fort classification.
(From the Netter Collection of Medical Illustrations: Website. Available at http://www.netterimages.com [accessed February 2012]. Copyright Elsevier Inc.; all rights reserved.)
The larynx and trachea are essentially subcutaneous structures in the anterior neck. The larynx is separated from the skin only by subcutaneous fat and the anterior cervical fascia. The thyroid notch, cricothyroid membrane, and cricoid cartilage can be easily palpated to provide the critical landmarks for surgical access to the airway (see Chapter 31). The airway is mobile in the neck but is fairly firmly anchored by the strap muscles and cervical fascia. Tracheal deviation as a result of pneumothorax or hemothorax may occur in patients who are severely compromised.6 Tracheal deviation is not helpful as a sign of pneumothorax because it usually occurs only when the pneumothorax is at an advanced state and easily identifiable by auscultation. Tracheal deviation can result from disruption of the neck anatomy caused by hemorrhage or extensive subcutaneous emphysema. It is also seen with chronic scarring, such as that related to previous radiotherapy. In any case, palpation of the trachea and larynx is a valuable exercise in the event that surgical airway management becomes necessary. It also can establish the position of the airway in the neck, even if orotracheal intubation is contemplated. Orotracheal intubation can be extraordinarily difficult or impossible when the trachea or larynx is displaced laterally.
III Specific Clinical Considerations in Trauma
A Direct Airway Trauma
1 Penetrating Neck Trauma
Penetrating neck injuries range in scope from stab or other puncture wounds to major lacerations due to both low-velocity (e.g., BBs, pellets) and high-velocity (e.g., crossbows, firearms) projectile injury. The consequences of these various mechanisms can vary drastically. The overall mortality rate due to penetrating neck injuries is 2% to 6%, with a significantly lower mortality rate for low-velocity injuries.7–9 The patient with a stab wound to the neck usually has identifiable anatomy and can undergo a planned airway evaluation and early intubation under controlled circumstances. Patients with high-velocity injuries often have significant vascular and hollow-structure injuries, and anatomic distortion can make airway management challenging.10 These injuries mandate urgent airway management, but the approach is confounded by the myriad injuries caused by the missile.11
For the purposes of classification of penetrating injury, the neck is divided into three zones (Fig. 41-3). Zone 1 extends from the clavicles inferiorly to the level of the cricoid cartilage. Zone 2 extends from the cricoid cartilage to a line drawn through the angles of the mandible, and zone 3 is the area above the angles of the mandible. This classification is most useful for low-velocity penetration, such as from a stab or long-distance birdshot, but it has also been applied to high-velocity injuries, such as rifle wounds.10 These zones were designated because of their unique anatomic characteristics.12 Zone 1 is dominated by the major vascular structures at the root of the neck, specifically the carotid arteries, internal jugular veins, subclavian arteries and veins, and innominate arteries and veins. The airway at this level is relatively inaccessible except by tracheotomy. Zone 1 injuries are relatively uncommon (<10% of penetrating neck injuries) but are often associated with major vascular injuries or injuries to the dome of the lung.13 Patients with zone 1 injuries often require emergency airway management because of direct airway compromise by hemorrhage or the anticipated clinical course predicted by the profound shock that typically develops. There is little literature to guide the selection of airway management techniques for zone 1 penetrating injuries. Most information is limited to small case series of subsets of larger series that are dominated by zone 2 injuries. The approach to airway management is dictated more by the nature of the threat to the airway than by the location of the inciting wound. The overall approach to airway management in penetrating neck injuries is outlined subsequently.
Zone 2 is the most common location for penetrating neck injuries, accounting for most reported cases.14 Zone 2 injuries require emergency airway intervention in approximately one third of the cases, with a large proportion of the remainder undergoing subsequent intubation related to evaluation or surgical repair. The area of concern in zone 2 extends from the anterior margins of the paravertebral muscles bilaterally. In this area, major vascular structures (e.g., common carotid arteries, internal jugular veins) and their associated sympathetic ganglia and the hypopharynx, esophagus, larynx, and trachea are all at risk. The most common cause of airway compromise in zone 2 injuries is external distortion by hemorrhage related to vascular injuries or direct injuries to the airway.15
The best approach is to consider two specific issues. The first is whether there is evidence of a direct injury to an air-containing structure in the neck. Subcutaneous air indicates injury to an air-filled structure in the neck,16 such as the airway (including the hypopharynx or pharynx) or the esophagus. In severe cases, particularly patients with injury to both vascular and air-filled structures, airway obstruction can occur rapidly, requiring emergency cricothyrotomy.17 In less threatening cases, it is virtually impossible to tell whether the esophagus or airway is involved, and early direct or fiberoptic examination of the airway is indicated. Sedation and topical anesthesia allows the operator to determine the severity and location of any airway injury. Preparation with a small to moderate-size endotracheal tube (ETT) (e.g., 6.0- to 7.0-mm inside diameter) mounted on the scope before initiating endoscopy facilitates prompt intubation if the injury is found to be significant. If the scope has been placed successfully distal to the injury, the patient can be gently intubated over the flexible fiberoptic bronchoscope (FFB), because it is best to secure the airway distal to the injury. This at least ensures that the patient is safe until he or she can be transported to the OR for further evaluation by an otolaryngologist or general surgeon. Although tracheostomy is often necessary, in these cases, temporary oral endotracheal intubation over an FFB ensures airway control and minimizes the subsequent leakage of air into the tissues, facilitating later repair.16 If no airway injury is identified and there is no evidence of increase in the subcutaneous emphysema in the neck during spontaneous or assisted ventilation, the injury can be presumed to be esophageal.18 If, however, circumstances change and subcutaneous emphysema begins to increase, even slightly, intubation is recommended since development of large amounts of subcutaneous emphysema can distort airway anatomy such that subsequent intubation or surgical airway management becomes difficult or impossible. As with all penetrating neck injuries, early intubation, even in patients who do not appear to immediately require it, is the most prudent course.
The second issue is whether there is evidence of significant vascular injury to the neck. All penetrating neck wounds have some external bleeding, although it can be surprisingly modest. The issue with respect to airway management is whether injury has occurred to any of the major vascular structures in the neck (e.g., carotid arteries, jugular veins). A hematoma of any size, external hemorrhage, or any evidence of displacement of the airway structures can serve as evidence of direct vascular injury. As soon as it has been established that direct vascular injury has occurred, active airway management should be undertaken.19,20 Most of these patients present early in the course of their injuries, when anatomy is preserved and orotracheal intubation is likely to be relatively easy to achieve. Waiting to determine whether the hematoma is expanding is perilous, because most of the hemorrhage into the neck occurs into the deep tissue planes, distorting and displacing the airway without external evidence until a crisis occurs. The time-honored dictum that hematomas of the neck should be observed to see whether they are expanding is not rational, and any evidence of direct vascular injury to the neck is sufficient justification for intubation. Early intubation can proceed using a rapid-sequence intubation (RSI) technique if a careful examination for difficult airway attributes fails to identify problems and there is a sound rescue strategy planned in the event of intubation failure.21 Early intervention allows the operator to intubate in a controlled fashion rather than scrambling to secure an emergency airway later in the patient’s course, when airway obstruction is imminent or has already occurred.
The third option is to proceed directly with a planned surgical cricothyrotomy. This requires that the airway be identifiable with clear landmarks to permit a surgical approach. Local anesthetic infiltration and direct transcricothyroid puncture for instillation of local anesthesia into the airway are likely to make the procedure easier to perform (see Chapter 31).
In all cases of penetrating neck trauma, early consultation with an otolaryngologist or general surgeon is essential. Initially innocuous injuries may lead to catastrophic consequences for the patient if not identified and managed early.22 Early airway intervention permits controlled resuscitation and prevents major morbidities related to penetrating neck injury, such as airway compromise with resultant hypoxia or anoxia.
2 Blunt Neck Trauma
1. Identification of swelling, hemorrhage, or subcutaneous emphysema
2. Evaluation for tenderness (if possible) of the neck, particularly the airway structures
3. Evaluation of the anatomy of the upper airway for direct airway injury and for the anatomic landmarks that are important if a surgical airway must be placed (see Chapter 31).
Because subcutaneous emphysema may be occult, it requires careful palpation. Extensive ecchymosis suggests blunt vascular injury with free hemorrhage (which is usually venous) or formation of a pseudoaneurysm. Extensive ecchymosis or extensive swelling strongly suggests impending airway compromise, and urgent airway intervention is advisable.23 Infrequently, direct blunt neck trauma can cause laryngeal fracture or tracheal transsection. The latter is often rapidly fatal, but patients may arrive in the trauma resuscitation area alive because of incomplete transsection.24 In these cases, there is usually subcutaneous air, often accompanied by swelling, and pain elicited by palpation of the anterior airway. Although a trial of BMV may be tempting, it is likely to exacerbate the subcutaneous emphysema and accelerate the patient’s deterioration. When such an injury is identified, the best approach is prompt transfer to the OR for surgical exploration of the anterior neck and establishment of the airway by tracheostomy distal to the transsection. Often, however, airway management must be undertaken before the surgery, and careful awake fiberoptic intubation over a small FFB after inhalational induction may be the least of all evils. If the airway must be secured in the ED, for example, before transportation to a level I trauma center, the same approach is used, substituting intravenous sedation and topical anesthesia for inhalational anesthesia because the latter is not available in the ED.
Airway management is complicated by the fact that patients with blunt anterior neck trauma must be presumed to have a C-spine injury. Up to 50% of patients with blunt airway injury have a C-spine injury,25 which is discussed here in the context of airway management.
In clothesline injuries, in which the neck is struck, usually transversely, by a fence wire or similar object, the central neck area may be significantly but deceptively disrupted from the impact.17 Although these injuries can be dramatic and often require immediate airway management, the airway itself is often intact, signified by identification of intact structures and the absence of air bubbling or gurgling during negative-pressure or positive-pressure ventilation. Early intubation from above, preferably over an FFB, is best in these cases. If the airway has been breached, and gurgling or subcutaneous air is evident in the tissues of the neck, positive-pressure BMV is not likely to be successful in oxygenating the patient, and attempts at BMV may result in insufflation of large amounts of air into the soft tissues of the neck, further compromising the airway and the attempts at securing it. The best approach in these cases is to attempt to secure the airway over an FFB using sedation and topical anesthesia, with a plan to progress directly to a cricothyrotomy or emergency tracheostomy, if fiberoptic intubation is unsuccessful.
3 Maxillofacial Trauma
Maxillary fractures usually occur in one of the classically described Le Fort patterns. Although the precise location of the Le Fort fracture pattern is sometimes difficult to remember, the Le Fort I, II, and III fractures can be thought of as follows (see Fig. 41-2). The Le Fort I fracture represents separation of the roof of the mouth from the face, with the fracture extending through the alveolar ridge to the base of the nose and separating the alveolar ridge and hard palate from the rest of the face. The Le Fort II fracture is separation of the central face from the rest of the face and cranium. The fractures extend from the base of the nasal bones through the medial orbits down through the maxilla to the posterior molars, effectively creating a free-floating central face fragment. The Le Fort III fracture is separation of the face from the skull. This fracture extends from the base of the nasal bones through the orbits to the lateral orbital rims and then through the zygomatic arch and down through the pterygoid plate.
An uncommon but disastrous presentation of maxillofacial injury occurs when an attempted suicide fails because the gun (usually a shotgun) is oriented in such a way as to have the mass of the shot pass upward through the face rather than on a posterior trajectory through the brainstem. This often happens when the patient places a rifle or shotgun under the chin and then tries to reach downward for the trigger. This movement naturally leads to extension of the neck, and the trajectory of the missile is altered, causing it to pass upward through the face (Fig. 41-4). Although such injuries occur with massive facial distortion, airway management can range from easy to virtually impossible. Destruction of the mandible, tongue, palate, and nasopharynx often makes orotracheal intubation impossible, and hemorrhage is usually extensive. Primary surgical airway management is usually the method of choice. However, the injury can be predominantly anterior, sparing the airway, and the mandible and tongue can be displaced forward, permitting adequate oral access for orotracheal intubation. Nonetheless, efficient suctioning is usually required because the hemorrhage can be significant.
B Cervical Spine Injury
Unstable injury to the C-spine presents a particular hazard with respect to airway management because of the potential to cause or exacerbate spinal cord injury. C-spine injury usually occurs when there is high-energy transfer, such as in a motor vehicle collision, but it can occur with relatively minor trauma in patients with significant degenerative disease of the C-spine, such as rheumatoid arthritis or osteopenia. Motor vehicle collisions are the greatest cause of spinal injury, accounting for about 50% of these injuries, followed by falls, athletic injury, and interpersonal violence.26
In the trauma resuscitation room, all patients who have been subjected to significant blunt trauma should be assumed to have a C-spine injury until it has been excluded. Penetrating trauma can also cause spinal injury, but creation of an unstable spinal injury without concomitant spinal cord injury is exceedingly rare. With penetrating injury, it is usually apparent whether spinal injury has occurred because the patient sustained a neurologic disability. Barring this finding, C-spine immobilization in a patient with isolated penetrating trauma is typically unnecessary and may even be harmful.27–29
One of the significant challenges related to airway management in patients with blunt trauma is the inability to determine definitively whether the patient has a C-spine injury before intubation is required. Fortunately, most patients with a C-spine injury do not require intubation during the acute phase of resuscitation. However, those who have the most severe trauma are likely to require intubation, and this is the same population who is at highest risk for spinal injury.30 It has been estimated that 2% to 14% of all patients with serious blunt trauma have a significant C-spine injury.31,32
The decision about whether to obtain portable C-spine imaging before intubation must take into account two radiographic principles. First, a single, portable, lateral, cross-table radiograph is highly insensitive for significant C-spine injury. At least 25% of lateral C-spine radiographs fail to visualize the cervical-thoracic junction (C7-T1).33 Even if the lateral radiograph is adequate, it should be considered no more than 80% sensitive for C-spine injury.34 A complete three-view C-spine series fails to identify about 15% of significant C-spine injuries, and it is difficult to obtain adequately for patients in cervical collars.35 In consideration of this information, no plain radiograph should be interpreted as indicating that the C-spine is free of injury and that movement can be undertaken with impunity during intubation.
Second, the severe limitations of portable C-spine radiographs question their value before intubation. Current guidelines recommend the use of CT for C-spine evaluation of patients with trauma.36 Given the limitations of portable cross-table plain radiographs of the spine and the danger of remote imaging before airway management, it is prudent to presume a C-spine injury and intubate with in-line C-spine stabilization without imaging.
Intubation should be performed with the anterior portion of the cervical collar open because it may limit laryngoscopy. Leaving the collar intact has not been shown to reduce significant C-spine movement during intubation, and is not a substitute for manual in-line stabilization.37–39 Although cricothyrotomy can be performed through the openings in most cervical collars, it is often technically challenging, and it is preferable to remove the anterior one half of the collar before undertaking surgical airway management. The debate regarding nasotracheal intubation versus various awake intubation techniques versus RSI in the trauma patient is discussed in “Principles of Airway Management in the Trauma Patient.”
C Intracranial Injury
Airway management in the patient with intracranial injury is dictated by an often-conflicting series of choices between limiting the adverse responses in the brain related to intubation and maintaining overall management of the patient’s hemodynamic status and resuscitation. In patients with an elevated ICP, stimulation of the upper airway structures by a laryngoscope or other device results in an increase in the ICP.40 The ICP appears to increase by two mechanisms: First, a release of sympathetic adrenergic transmitters results in elevation in heart rate and blood pressure, which translates to an elevation in ICP in the nonautoregulated brain.41 Second, a direct reflexive increase in ICP is caused by laryngeal stimulation, although the mechanism is not precisely defined.42
Succinylcholine, which is the drug of choice for RSI of the multitrauma patient, is believed to cause an elevation in ICP, although this has been disputed.43–45 The mitigation of these potential elevations in ICP is an important theme in the airway management of the trauma patient with presumed intracranial injury. Avoidance of hypoxia and hypercarbia and maintenance of adequate perfusion are vital for producing the best possible patient outcome.
Lidocaine has been studied in the context of prevention of the ICP response that is sympathetically mediated and the ICP response that is considered reflexive. Its use during RSI in the context of head injury continues to be controversial. Best-evidence reviews of patient outcomes and lidocaine use during airway management in head injured patients showed that no good evidence exists evaluating this specific issue.46–48 Several small, randomized trials have found conflicting results with respect to the ability of lidocaine to attenuate spikes in ICP during laryngoscopy and intubation.41,49–54 Overall, there is insufficient evidence to strongly recommend the use of lidocaine for the purpose of suppression of sympathetic discharge during intubation. However, lidocaine given intravenously at a dose of 1.5 mg/kg has been shown to blunt the direct ICP response to tracheal suctioning and laryngeal stimulation in hypocarbic patients with elevated ICP.51,53 Lidocaine’s wide therapeutic margin, familiarity, safety profile, and ready availability make it a reasonable choice when administered at 1.5 mg/kg intravenously for 3 minutes before the induction agent when undertaking RSI of a patient with known or presumed elevated ICP. Used in this manner, lidocaine may have a beneficial effect on the direct ICP response to laryngoscopy and intubation.
The sympathetic response to intubation has been extensively studied, and synthetic opioids and beta-blockers have been shown to attenuate the reflex sympathetic response to laryngoscopy. Administration of a beta-blocker to a trauma patient may worsen hemodynamic instability and is rarely desirable, except in certain cases of isolated head trauma. Similarly, administration of full sympathetic-blocking doses of the synthetic opioids, such as fentanyl, can have adverse effects, particularly in patients with hypovolemia, who depend on sympathetic drive. Fentanyl, in a dose of 2 to 3 µg/kg as a pretreatment agent, has been shown to attenuate the reflex sympathetic response to laryngoscopy and should have minimal adverse cardiovascular effects.55 Care must be used, however, to ensure that the fentanyl does not cause respiratory depression with resulting hypercarbia and that the patient has sufficient hemodynamic stability to tolerate even this small dose.
Competitive NMB agents, such as rocuronium, achieve intubating conditions almost as rapidly as succinylcholine, but without the attendant rise in ICP.56,57 However, the duration of paralysis when 1.0 mg/kg of rocuronium is used for intubation is about 45 minutes.58 For this reason, succinylcholine, with its ultrarapid onset and shorter duration of action, remains the drug of choice for emergency intubation of trauma patients, including those with elevated ICP. The exacerbation of the ICP elevation by succinylcholine, however, is clearly not desirable. Evidence is poor supporting the administration of a defasciculating dose of a nondepolarizing NMB before succinylcholine to attenuate an increased ICP and is not recommended.
In summary, when RSI is planned, and there is no contraindication, 1.5 mg/kg of intravenous lidocaine and 3 µg/kg of intravenous fentanyl should be considered before the administration of succinylcholine. Defasciculating doses of non-depolarizing NMB drugs should not be used until further study clarifies their role. Laryngoscopy and intubation should be as gentle and atraumatic as possible. There is evidence that minimizing laryngeal stimulation helps to reduce the hemodynamic and ICP responses to laryngoscopy and intubation. Several devices have been evaluated to see whether they are less traumatic than direct laryngoscopy. Intubations through a laryngeal mask airway (LMA) and with the use of the Trachlight stylet appear to be less stimulating than intubation by direct laryngoscopy.59,60 Studies comparing intubation over a lighted stylet with direct laryngoscopy indicate that the placement of the ETT into the trachea is more stimulating than the laryngoscopy itself.61
D Intraocular Injury
Most patients with open globe injuries can be intubated in the OR under controlled conditions. Penetrating globe injuries usually are isolated and are caused primarily by implements (e.g., sticks, children’s toys) or by low-velocity missiles (e.g., BBs, pellets). Occasionally, open globe injury occurs in the context of multitrauma and requires intubation in the trauma bay. Decisions related to overall management of the patient’s multiple injuries should take precedence over management of the eye injury. Whether the intubation occurs in the trauma resuscitation bay or in the OR, the concern related to managing open globe injuries is whether succinylcholine, which causes a transient rise in intraocular pressure, may cause extrusion of intraocular contents.62 There has never been a single case report of vitreous extrusion after the use of succinylcholine in a patient with an open globe injury.63 The paramount consideration therefore appears to be prevention of straining, coughing, or bucking during the intubation, arguing for RSI. It has been recommended that a defasciculating dose of a competitive NMB agent be given 3 minutes before administration of succinylcholine in patients with open globe injuries to mitigate the elevation of intraocular pressure, but this approach has never been subjected to study. It appears that defasciculation is appropriate for patients with open globe injuries receiving succinylcholine unless there is a contraindication, such as severe respiratory compromise.
E Thoracic Injury
Blunt and penetrating injuries can cause sufficient compromise of respiration or oxygenation to mandate intubation. The extent of injuries associated with penetrating trauma depends on the implement or missile used and the location and path of the object involved. High-velocity gunshot wounds to the chest are often fatal, causing disruption of the major vasculature, main stem bronchi, or the heart.64 Lower-velocity gunshot wounds, especially those more peripherally placed, often cause much less blast injury to the chest, resulting in minor pulmonary contusions and a surprisingly low incidence of hemothorax or pneumothorax.65 Pneumothorax is common in penetrating injury, whether caused by missile or implement, and cardiac injury with pericardial tamponade can occur. Blunt chest trauma tends to be more diffuse and is more often associated with pulmonary contusion, disruption of the chest wall with concomitant rib fractures, costochondral separation, hemothorax or pneumothorax, and if severe, disruption of a main stem bronchus or of the aorta.
F Hemorrhagic Shock
The patient in profound hemorrhagic shock has significant metabolic debt, experiences rapid muscle fatigue, is susceptible to respiratory compromise and failure, and usually requires intubation with positive-pressure ventilation unless the underlying process can be reversed. In addition to contributing to the need for intubation, hemorrhagic shock greatly limits the choice of agents for intubation. Induction agents such as sodium thiopental and propofol have significant adverse hemodynamic consequences.65 These agents should be used in greatly reduced doses or avoided altogether in patients with hemorrhagic shock. Ketamine releases catecholamines and is the most stable of the induction agents. Ketamine can be used in a reduced dose of 1 mg/kg, even in patients with significant hemodynamic compromise. In frank shock, however, ketamine, like every other induction agent, depresses myocardial contractility and must be used with extreme caution.66,67 It has been implicated in transient elevations of ICP, but the evidence in this regard is highly conflicted.68 In the context of head injury with significant hypovolemia, ketamine’s superior hemodynamic characteristics outweigh its potential to cause small, transient rises in ICP. Although caution is advised in administering ketamine to patients with head injury and to those in shock, it may be the least of all evils if given in a reduced dose in these patients.
Etomidate, an imidazole derivative, has remarkable hemodynamic stability.69 In the induction dose of 0.3 mg/kg, it causes virtually no change in mean arterial blood pressure in normal and hypovolemic patients. In very large doses (two or three times the induction dose), etomidate consistently causes hypotension.70 In morbidly obese trauma patients, dosing should be based on their lean body weight, not total body weight. For patients with frank shock, the dose should be reduced to between 0.15 and 0.2 mg/kg. Etomidate appears to have some cerebral protective effect and can significantly lower ICP without adverse effects on perfusion pressure.71 It is therefore a rational agent for use in patients with multisystem trauma and hypovolemic shock.
Midazolam is infrequently used as an induction agent in multitrauma patients. It exhibits many of the same adverse hemodynamic effects as propofol and Pentothal. If it is used, the dose should be greatly reduced to 0.1 mg/kg in patients in frank shock. However, compared with other readily available agents, midazolam has a slower onset and longer clinical half-life, and at greatly reduced doses, it may not provide adequate amnesia for the patient.72
Isotonic fluid resuscitation must occur in parallel with preparation for intubation. The use of a high-flow blood-infusing unit can provide warmed packed red blood cells at a rate as high as 500 mL/min.73 Care must be taken not to overshoot the resuscitation, particularly in the presence of penetrating injuries and those thought to be associated with ongoing bleeding. The goal is maintenance of an adequate perfusion pressure to support the brain and vital organs until surgical repair can be undertaken. There is no evidence that restoration of the blood pressure to a normal range is beneficial, and evidence suggests that permissive hypotension may instead be preferable.74–76 Crystalloid can be infused as the first 2 L of fluid during resuscitation, but it should be rapidly replaced with blood if shock is ongoing. A urinary catheter may be helpful to monitor urine output, and lactic acid or base deficit values can help to monitor the overall treatment of shock.77 If the patient is not going to be transported promptly to the OR, placement of an arterial line is highly advisable.
IV Principles of Airway Management in the Trauma Patient
A Control of the Combative Patient
The decision about whether to sedate a patient or to intubate for behavioral control should be made on the basis of the patient’s overall injuries. If intubation is inevitable, even without combative behavior, based on the patient’s injuries and expected clinical course, early intubation is the best approach. RSI allows protection of the C-spine, complete control of the patient, and treatment of multiple injuries without further disruption or pain. If the patient’s overall injuries are deemed to be relatively modest and intubation would not be indicated in the absence of the combative behavior, chemical restraint without intubation is the best approach. Repeated, titrated doses of a butyrophenone, such as haloperidol, can rapidly achieve control of the patient without compromising respiration or significantly altering the neurologic examination. In the hemodynamically stable patient, 5 mg of haloperidol can be given intravenously in repeated doses every 5 minutes, with observation for effect.78 Most patients calm rapidly under the influence of the haloperidol, and management can then proceed in a more orderly fashion. Haloperidol has been rumored to lower the seizure threshold and therefore be contraindicated in patients with head trauma, but this is close to a medical fairy tale. There are no well-controlled studies proving this association, and the remainder of the literature is a heterogenous mixture of rat studies and case reports.79 There is no human evidence to support this often-cited contraindication. Droperidol was equally effective and commonly used for this purpose before the U.S. Food and Drug Administration (FDA) issued a highly controversial black box warning about QT interval prolongation, which greatly curtailed its use.80
B Prevention of Aspiration
Routine application of posterior cricoid pressure (i.e., Sellick’s maneuver) held throughout laryngoscopy was widely accepted dogma because it was thought to prevent aspiration through compression of the upper esophagus against the anterior cervical vertebral bodies. Although it seemed logical, it was never supported by firm evidence.81,82 Misapplication of cricoid pressure is common among a variety of operators, and it can result in more difficult mask ventilation, direct laryngoscopy, and tracheal tube passage.83–86 Moreover, regurgitation is often seen despite Sellick’s maneuver being applied.87–90 Advanced imaging suggests the cervical esophagus is positioned lateral to the cricoid ring in many patients, a relationship that is exaggerated by posterior pressure rarely resulting in esophageal obstruction.91 C-spine motion may occur during cricoid pressure and introduce unnecessary risk for patients with known or suspected unstable C-spine injuries. If applied correctly however, Sellick’s maneuver may reduce gastric insufflation during BMV.92–94 On balance, the best approach is to consider posterior cricoid pressure optional during laryngoscopy and intubation and to remove it immediately if the laryngeal view is poor or tube passage is difficult. It should be routinely performed during prolonged rescue BMV.
If the patient vomits while on the spine board, the patient and the board should be rolled together into the right lateral decubitus position to permit suctioning and evacuation of the vomitus from the mouth. Vomiting is an indication for early intubation in patients who require immobilization on a spine board and who may be relatively helpless to manage the vomitus after it is in the mouth. When applying awake intubation techniques, adequate sedation and topical anesthesia should be used to prevent gagging and emesis. If the patient vomits during awake intubation, there is increased risk of aspiration because of the topical anesthesia of the supraglottic area and the vocal cords. Prompt suctioning and repositioning of the patient, if necessary, should help reduce this risk. There is no evidence that one particular device or technique is more likely to prevent aspiration than any other. RSI, developed as the cornerstone of emergency airway management because of its ability to reduce aspiration, has recently been challenged in this regard.95
C Choice of Technique
The issues related to approach to the airway are discussed in detail in the individual sections earlier in this chapter. Overall, the choice of technique must balance the physiologic status of the patient, the nature of the injuries, predicted airway difficulty, the urgency of the airway intervention, and the availability of various devices and surgical backup. Historically, the Advanced Trauma Life Support (ATLS) course developed by members of the American College of Surgeons advocated blind nasotracheal intubation for patients with suspected C-spine injuries because it was believed to be less likely to cause C-spine movement. This belief was unfounded, and blind nasotracheal intubation has fallen out of favor as a method of airway management in the trauma patient because of slower intubation times, higher complication rates, and greater O2 desaturation.96–98 RSI is the preferred method for most intubations. There was early objection, however, due to suspicion of dangerous degrees of C-spine motion during unrestricted direct laryngoscopy and that residual muscle tone in nonparalyzed patients provided valuable splinting support. As a result of these two fundamentally incorrect beliefs, trauma intubations through the 1970s and 1980s were largely performed by awake intubation. Cadaver studies and those done in living patients have failed to support this contention. There is no evidence that careful laryngoscopy performed with in-line stabilization subjects the C-spine to any risk, although intubation should not be forceful or prolonged. There is good evidence that manual in-line stabilization combined with a careful oral laryngoscopy and RSI does not pose any risk to the cervical spinal cord.99–101
Unrelaxed patients present the potential for significantly more C-spine motion as a result of coughing, bucking, gagging, or other movement during an awake intubation attempt. RSI has been successful and frequently used during trauma intubations. In a published report of almost 9000 ED intubations from phase II of the National Emergency Airway Registry showed that 82% of trauma patients underwent RSI and 11% were intubated with no medications; they were mostly patients in full arrest or near-full arrest who were completely unresponsive on presentation and underwent immediate direct laryngoscopy with intubation and manual in-line stabilization. Less than 1% of patients underwent unassisted nasotracheal intubation.102
D The Difficult Airway
Trauma patients represent a group with high-risk, exceptionally difficult airways. Acquired characteristics, such as airway trauma, C-spine immobility, hemodynamic compromise, and other potentially life-threatening injuries, can exacerbate inherently difficult airway markers, necessitating clarity of thought and error-free decision making during intubation. An efficient but detailed difficult airway assessment is necessary before NMB in the multitrauma patient. Conventional assessments that occur during a preoperative visit may not be possible in the trauma bay. It is rarely possible to obtain a prior surgical anesthetic history from the patient. Creators of the national Emergency and the Difficult Airway Course: Anesthesia have developed a four-pronged rapid assessment tool that can be quickly applied to virtually any patient.103 Portions of this tool have been externally validated in emergency populations, and it is currently subject to further validation in the third phase of the National Emergency Airway Registry multicenter registry.104 The LEMON mnemonic is used as shown in Box 41-1 to identify one or more attributes of a difficult airway in a patient.
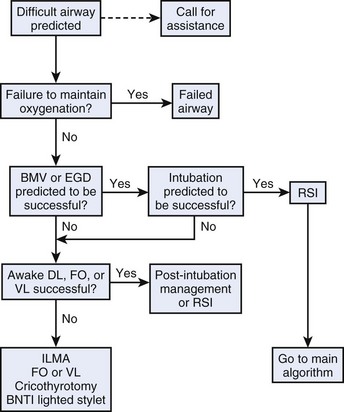
The tool is overly sensitive at the cost of specificity, but that is more desirable than the converse. If a difficult intubation is anticipated, physicians use an algorithmic approach that is dictated by how stable the patient is and how urgently he or she needs to be intubated (Fig. 41-5). The easiest surrogate is the best attainable O2 saturation measurement, because it defines the time available to consider alternative approaches. If the patient is well oxygenated and is reasonably stable (i.e., does not need to be intubated in the next 2 to 3 minutes), a methodic stepwise plan can be made. If the patient is critically desaturated and highly unstable, it is probably necessary to proceed directly with some form of airway intervention promptly without the luxury of a planned approach to the difficult airway. In this scenario, a double-setup RSI, in which the anterior neck is prepared for a surgical airway as RSI drugs are administered, is most appropriate. RSI gives the operator the best chance of intubation success, and if a cannot intubate, cannot ventilate (CICV) scenario develops, a cricothyrotomy should be immediately performed. Primary cricothyrotomy may be the primary method used, usually when orotracheal and nasotracheal intubation is predicted to be difficult or impossible. Rarely, other devices such as the FFB or intubating LMA (ILMA) are useful.
When there is sufficient time (SaO2 > 90%) to plan the intubation approach carefully, the patient should be evaluated for the likelihood of success with BMV and laryngoscopy. Predicted success with BMV is a necessary precursor to consideration of paralysis. The MOANS mnemonic (Box 41-2) contains a well-validated collection of patient attributes that contribute to difficult mask ventilation.105 If it is the intubator’s judgment that the patient cannot be BMV successfully, a technique using NMB is out of the question unless it is part of a double setup with an immediate ability to move to a surgical airway if the first attempt at laryngoscopy is unsuccessful. Next, the operator must decide whether laryngoscopy and intubation are likely to be successful. If it is thought that the patient is likely to be successfully intubated by direct laryngoscopy despite the difficult airway attributes, taking into consideration that the patient should successfully undergo BMV, RSI can be planned with a surgical backup, as necessary. For example, the assault patient requiring strict C-spine precautions because of a dislocated jaw and active upper airway bleeding would be challenging or impossible to manage with direct laryngoscopy because of a severely reduced mouth opening, neutral head position, and airway bleeding. However, a normal-sized patient who was stabbed in the abdomen and was placed in a C-spine collar by emergency medical services but who has little likelihood of a neck injury would routinely warrant a laryngoscopic attempt. Both patients meet criteria for a difficult airway, but successful direct laryngoscopy is reasonable in the second patient but not in the first patient. With the advent of the video laryngoscope, traditional difficult laryngoscopy predictors may not apply, and what constitutes a difficult video laryngoscopic attempt has not been defined. As our knowledge and experience with video laryngoscopy develops, our threshold for NMB in these patients may change.
In most circumstances, difficult airway attributes are identified in trauma patients, but the operator can still be confident that BMV and direct laryngoscopy will be successful, thereby permitting RSI. If, however, in the opinion of the operator, BMV or direct laryngoscopy is unlikely to be possible, it is better to proceed with an awake technique. This involves administration of sedation and use of topical anesthesia to permit awake evaluation of the airway by a direct, video-assisted, or fiberoptic technique (see Chapter 11). Awake laryngoscopy is a common approach that has three possible outcomes: the cords are well visualized, and the patient is intubated; the cords are well visualized, and the decision is made that RSI is possible (in this case, awake laryngoscopy is terminated, and the patient undergoes RSI); or awake laryngoscopy determines that orotracheal intubation will likely be difficult or impossible, and an alternative approach is necessary.
If, after awake direct laryngoscopy, it is determined that the patient cannot be intubated orally, there are several alternative techniques, which are described elsewhere in this textbook. In the trauma patient, the most useful of these is video laryngoscopy. Although it is susceptible to soiling from airway secretions and bleeding, the mechanical limitations inherent in direct laryngoscopy virtually vanish with video laryngoscopy, and glottic visualization nearly always improves.106,107 Surgical cricothyrotomy, flexible fiberoptic intubation, video laryngoscopy, a lighted stylet technique, and an ILMA may be useful in selected cases. Supralaryngeal or retroglottic airways, such as the LMA, King LT, and others, can be used as a rescue device in the setting of a failed airway, but they are rarely preferred as a primary management tool in trauma patients because of the uncertainty about their ability to protect against aspiration. The goal in managing the trauma patient, even with an identified difficult airway, is to achieve endotracheal intubation with an inflated cuff to protect against aspiration. Placement of a device that does not achieve this is normally considered only in circumstances in which there has been a failed airway or the patient has precipitously arrested and definitive airway management is not possible (see “The Failed Airway”).
E Pharmacologic Considerations
Induction agents should be chosen to provide the best possible intubating conditions (used in conjunction with succinylcholine) with the least likelihood for adverse hemodynamic consequences. Etomidate, in a dose of 0.3 mg/kg, is remarkably hemodynamically stable, appears to provide some degree of cerebral protection, and has an onset-duration profile similar to that of succinylcholine. Although etomidate has been associated with adrenal cortical suppression, this is not clinically significant when a single dose is used for induction for intubation.108 Its safety during RSI in trauma patients has been challenged, although these studies have fatally flawed methodology and low patient numbers, making the results hard to interpret and impossible to apply to clinical practice.109,110 Etomidate can cause myoclonic jerks during its onset, but use of a rapidly acting NMB agent, such as succinylcholine, mitigates this effect substantially. Ketamine is an appropriate induction agent for hypotensive trauma patients. Ketamine’s role in head injury has been questioned because of its tendency to cause elevated ICP, but it is likely that the preservation of cerebral perfusion by maintenance of mean arterial blood pressure in hemodynamically unstable patients is more important than any theoretical risk to the brain caused by ketamine’s tendency to increase cerebral activity and ICP.64,111 Other induction agents, such as propofol and pentothal, have much more tendency to cause hypotension and should be used in reduced doses and with caution in compromised or elderly trauma patients. Patients in shock with an immediate need for intubation should be given reduced (one-third to one-half) doses, regardless of the induction agent. Choice of a paralytic is not altered by the presence or absence of trauma. Succinylcholine and rocuronium are both appropriate and result in near-equivalent intubating conditions and first-pass success, depending on the dose used.112,113
The choice of agents for sedation and awake intubation is influenced by the patient’s general status. It is advisable to use the agent with which the operator is most familiar for sedation. For example, if the operator typically sedates patients for painful procedures using propofol, it may be the best choice to sedate the trauma patient for awake laryngoscopy. In the absence of operator preference, ketamine may be ideally suited, especially when combined with an antisialagogue because of its ability to preserve respirations and hemodynamic status.114 Overall, familiarity with the drugs and the ability to titrate them carefully are probably more important than the drug’s pharmacodynamic characteristics.
F The Failed Airway
In managing the severely traumatized patient, it is important to have a clear definition of airway failure and a prepared action plan. The most widely accepted definition of a failed airway and the one used in the Emergency and the Difficult Airway Course: Anesthesia states that a failed airway exists when “(1) there have been three failed attempts by the most experienced operator, or (2) there has been one failed attempt by an experienced intubator combined with an inability to maintain adequate oxygen saturation despite airway adjuncts, maximal supplemental oxygen, and a bag and mask.”115
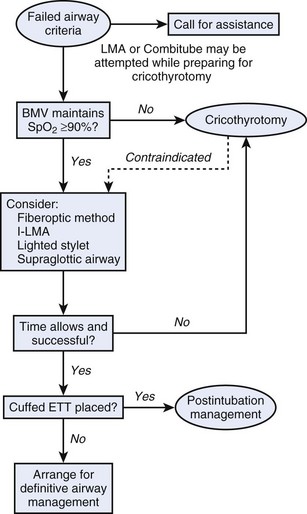
In either case, it is necessary to recognize that, with the current method and device being used, orotracheal intubation is not going to succeed, and the operator must move on to a rescue technique. If three attempts have failed, but oxygenation can be maintained with BMV, the operator should quickly evaluate why intubation was unsuccessful. Despite solid direct laryngoscopic technique, inadequate glottic exposure is often the culprit and results from the additive effect of poor C-spine mobility, reduced mouth opening, and oral secretions and blood. The modern difficult airway manager should have within his or her immediate reach a device designed to overcome these limitations and see around corners. Many options exist, although video laryngoscopy has shown the most promise, resulting in improved laryngeal views in almost every conceivable scenario in OR studies and ED populations.106,107,116,117 In the CICV scenario, the most appropriate rescue device is surgical cricothyrotomy. One parallel attempt at oxygenation may occur by rapid, blind insertion of a rescue supralaryngeal airway, such as a King LT or LMA, but only in concert with preparation for a surgical approach. If the patient’s oxygenation improves, other options can be explored. There should, however, be no hesitation for performing a cricothyrotomy if the slightest hint of supralaryngeal airway failure exists. An algorithm for managing a failed airway was developed for the Emergency and the Difficult Airway Course: Anesthesia and is shown in Figure 41-6.115 The theme of the algorithm is that decisions are driven by whether there is sufficient time to consider alternatives. If a CICV scenario arises at any time, the pathway leads to cricothyrotomy.
G Rescue Techniques
The ultimate rescue technique for a failed airway in the trauma patient is surgical cricothyrotomy (see Chapter 31). When intubation has failed but ventilation is possible (i.e., cannot intubate but can ventilate scenario), several devices warrant consideration. They appear in the central box of the algorithm in Figure 41-6.
If direct laryngoscopy alone has been used, the operator should consider video laryngoscopy. The Glidescope video laryngoscope (GVL) and Macintosh video laryngoscope have been shown to improve laryngeal view compared with direct laryngoscopy in heterogeneous patient populations. Use of the GVL is associated with high levels of intubation success after failed direct laryngoscopy, although it may not be as effective in patients with significantly altered upper airway anatomy.118 Video laryngoscopy should be considered early as a backup or principal intubating device for significantly difficult trauma airways. Optically enhanced devices, such as the Airtraq, are understudied in trauma populations, although, early data suggest the Airtraq may be effective for patients requiring C-spine precautions.119
If these tools are not available, many supralaryngeal airways can be tried. The Combitube has been evaluated as a primary airway management device and as a rescue device. Numerous studies have shown that emergency medical technicians can successfully insert Combitubes with a high likelihood of success.120,121 When studied in a cadaver unstable C-spine model, the Combitube produced more posterior C-spine displacement than the LMA or fiberoptic methods. This suggests that in-line stabilization is equally important during Combitube insertion as during direct laryngoscopy.122 Insertion with a cervical collar in place, however, has yielded mixed results. One study showed a high insertion success rate, and another reported successful blind insertion in only one third of patients with a semirigid collar on.123,124 Ventilation with the Combitube, however, usually is highly successful.124 The primary use of the Combitube is as a rescue device in the cannot intubate but can ventilate scenario in which other airway devices are thought unlikely to be successful. The Combitube is a less desirable choice because it does not place a cuffed ETT in the trachea when located in the esophageal position, but it usually suffices for ventilation and oxygenation. Another role for the Combitube is as a temporizing measure during preparations for cricothyrotomy. In this circumstance, only a single, expeditious attempt at placement is warranted.
Patients may arrive in the trauma bay with the Combitube inserted, inflated, and functioning. Because the Combitube does not provide a definitive airway (defined as a cuffed ETT in the trachea), it is advisable in most circumstances to intubate the patient and remove the Combitube. Details of insertion and use of the Combitube are discussed in Chapter 27, but there is a specific technique that must be used to intubate when the Combitube is in place. The Combitube has two cuffs, which are inflated through two separate channels. The proximal (pharyngeal) cuff is the larger of the two and is indicated by the blue filling valve. After ensuring that the patient is stabilized and adequately preoxygenated, this proximal cuff should be deflated. The Combitube should then be moved to the left corner of the patient’s mouth to permit access from the right side for laryngoscopy. Because the Combitube is almost always placed in the esophagus, it can remain in place while laryngoscopy proceeds. If difficulty arises, video laryngoscopy may be performed.125 After the patient is intubated with the ETT cuff inflated and tube position confirmed by end-tidal CO2 detection, the distal cuff on the Combitube can be deflated, and the Combitube can be removed. In the few cases in which the Combitube is inserted in the trachea, it can serve as a definitive airway, and tracheal placement is identified because successful ventilation and CO2 detection are occurring through its second port. It has been recommended that a nasogastric tube be passed and the stomach decompressed before removal of the Combitube. It is possible for regurgitation to occur after removal of the Combitube, particularly if BMV occurred before placement of the Combitube in the prehospital setting.
In the ED and trauma resuscitation room, the ILMA is preferable to the Classic LMA. The ILMA is equally or more easily inserted and allows a conduit for subsequent intubation, with a significantly higher success rate than for the Classic LMA.126,127 The ILMA has also been used to facilitate fiberoptic intubation and lighted stylet intubation.128 The standard LMA and the LMA ProSeal have reasonable insertion success rates in the context of C-spine immobilization, but this situation has not been evaluated for the ILMA.129 The ILMA has two main uses in the trauma patient. It can be used as the primary intubation method in a patient with an identified difficult airway. In the trauma patient, however, particularly one with an immobilized C-spine, the ILMA typically is not the first device selected. More commonly, the ILMA is used as a rescue device in a cannot intubate but can ventilate scenario. Placement of the ILMA allows ongoing ventilation with a very high success rate and facilitates endotracheal intubation. Like the Combitube, the ILMA can be placed as a temporizing measure during preparation for a cricothyrotomy in a CICV situation, as long as the placement and attempted ventilation through the ILMA do not delay initiation of surgical cricothyrotomy. Although less studied, the King LT shows promise as an effective rescue device and offers advantages of speed and success over the Combitube when used by prehospital providers.130
VI Clinical Pearls
• Many trauma patients may initially appear to be maintaining their airways well, but because of progressive airway obstruction or multisystem traumatic comorbidities, they can deteriorate rapidly.
• Intubating a trauma patient should be part of an overall team-based approach to resuscitation. Although intubation may not be necessary to maintain airway patency, the patient’s expected clinical course or need for emergent surgical intervention may prompt intubation.
• The gag reflex should not be used to gauge airway protection in any patient, especially those with trauma, who are typically secured on a backboard in a cervical collar and prone to aspiration. If these patients do vomit, they should be rolled with the board into a lateral decubitus position.
• Current evidence supports a strategy of not immobilizing the C-spine in patients with isolated penetrating trauma who do not have signs of neurologic compromise.
• CT images, not radiographs, should be obtained for all patients with suspected C-spine injury who are stable enough for travel to a CT scanner.
• Advent of the video laryngoscope has changed the management of difficult airways. Improved glottic visualization and high success rates for intubation support its use as an early rescue tool and principal intubating device.
• Sellick’s maneuver does not prevent aspiration and may make intubation more difficult. It should be routine during bag-mask ventilation (BMV) but optional (at best) during intubation.
• Proceed with caution using induction agents, such as propofol or full-dose benzodiazepines, in patients with significant hemorrhage or shock.
• Predictors of a difficult airway, such as those contained in the LEMON mnemonic, should be applied to all trauma patients.
• A variety of effective rescue airway devices are available for use in trauma patients. Airway specialists should become familiar with and practice several of them to maximize the options available in case of a failed airway.
All references can be found online at expertconsult.com.
40 Adachi YU, Satomoto M, Higuchi H, et al. Fentanyl attenuates the hemodynamic response to intubation more than the response to laryngoscopy. Anesth Analg. 2002;95:233–237.
56 Perry J, Lee J, Wells G. Rocuronium versus succinylcholine for rapid sequence induction intubation. Cochrane Database Syst Rev. (1):2003. CD002788
60 Maharaj CH, Buckley E, Harte BH, et al. Endotracheal intubation in patients with cervical spine immobilization. Anesthesiology. 2007;107:53–59.
82 Ellis DY, Harris T, Zideman D. Cricoid pressure in emergency department rapid sequence tracheal intubations: A risk-benefit analysis. Ann Emerg Med. 2007;50:653–665.
91 Smith KJ, Dobranowski J, Yip G, et al. Cricoid pressure displaces the esophagus: An observational study using magnetic resonance imaging. Anesthesiology. 2003;99:60–64.
95 Neilipovitz DT, Crosby ET. No evidence for decreased incidence of aspiration after rapid sequence induction. Can J Anesth. 2007;54:748–764.
102 Walls RM, Brown CA, III., Bair AE, et al. Emergency airway management: A multi-center report of 8937 emergency department intubations. J Emerg Med. 2011;41:347–354.
103 Murphy MF, Walls RM. Identification of the difficult and failed airway. In: Walls RM, Murphy MF, Luten RC. Manual of emergency airway management. ed 3. Philadelphia: Lippincott Williams & Wilkins; 2008:81–93.
105 Langeron O, Masso E, Hurax C, et al. Prediction of difficult mask ventilation. Anesthesiology. 2000;92:1229–1236.
106 Brown CA, III., Bair AE, Pallin DJ, et al. Improved glottic exposure in adult emergency department tracheal intubations. Ann Emerg Med. 2010;56:83–88.
1 Gronert GA. Cardiac arrest after succinylcholine: Mortality greater with rhabdomyolysis than receptor upregulation. Anesthesiology. 2001;94:523–529.
2 Gronert GA. Succinylcholine hyperkalemia after burns. Anesthesiology. 1999;91:320–322.
3 Mackway-Jones K, Moulton C. Towards evidence based emergency medicine: Best BETs from the Manchester Royal Infirmary. Gag reflex and intubation. J Accid Emerg Med. 1999;16:444–445.
4 Chan B, Gaudry P, Grattan-Smith TM, McNei R. The use of Glasgow Coma Scale in poisoning. J Emerg Med. 1993;11:579–582.
5 Walls RM. The decision to intubate. In: Walls RM, Murphy MF, Luten RC. Manual of emergency airway management. ed 3. Philadelphia: Lippincott Williams & Wilkins; 2008:1–7.
6 Holloway VJ, Harris JK. Spontaneous pneumothorax: Is it under tension? J Accid Emerg Med. 2000;17:222–223.
7 Biffl WL, Moore EE, Rehse DH, et al. Selective management of penetrating neck trauma based on cervical level of injury. Am J Surg. 1997;174:678–682.
8 Kendall JL, Anglin D, Demetriades D. Penetrating neck trauma. Emerg Med Clin North Am. 1998;16:85–105.
9 Mandavia DP, Qualls S, Rokos I. Emergency airway management in penetrating neck injury. Ann Emerg Med. 2000;35:221–225.
10 Sofianos C, Degiannis E, Van den Aardweg MS, et al. Selective management of zone II gunshot injuries of the neck: A prospective study. Surgery. 1996;120:785–788.
11 Demetriades D, Asensio JA, Velmahos G, et al. Complex problems in penetrating neck trauma. Surg Clin North Am. 1996;76:661–683.
12 Asensio JA, Valenziano CP, Falcone RE, et al. Management of penetrating neck injuries: The controversy surrounding zone II injuries. Surg Clin North Am. 1991;71:267–296.
13 Jurkovich GJ, Gussack GS, Luterman A. Laryngotracheal trauma: A protocol approach to a rare injury. Laryngoscope. 1986;96:660–665.
14 Atta HM, Walker ML. Penetrating neck trauma: Lack of universal reporting guidelines. Am Surg. 1998;64:222–225.
15 Bell RB, Osborn T, Dierks EJ, et al. Management of penetrating neck injuries: A new paradigm for civilian trauma. J Oral Maxillofac Surg. 2007;65:691–705.
16 Grewal H, Rao PM, Mukerji S, et al. Management of penetrating laryngotracheal injuries. Head Neck. 1995;17:494–502.
17 Goudy SL, Miller FB, Bumpous JM. Neck crepitance: Evaluation and management of suspected upper aerodigestive tract injury. Laryngoscope. 2002;112:791–795.
18 Bryant AS, Cerfolio RJ. Esophageal trauma. Thorac Surg Clin. 2007;17:63–72.
19 Eggen JT, Jorden RC. Airway management in penetrating neck trauma. J Emerg Med. 1993;11:381–385.
20 Walls RM, Wolfe R, Rosen P. Fools rush in? Airway management in penetrating neck trauma. J Emerg Med. 1993;11:479–480.
21 Walls RM. Airway management. Emerg Med Clin North Am. 1993;11:53–60.
22 Bumpous JM, Whitt PD, Ganzel TM, et al. Penetrating injuries of the visceral compartment of the neck. Am J Otolaryngol. 2000;21:190–194.
23 Keogh IJ, Rowley H, Russell J. Critical airway compromise caused by neck haematoma. Clin Otolaryngol Allied Sci. 2002;27:244–245.
24 Ford HR, Gardner MJ, Lynch JM. Laryngotracheal disruption from blunt pediatric neck injuries: Impact of early recognition and intervention on outcome. J Pediatr Surg. 1995;30:331–334.
25 Crosby ET, Lui A. The adult cervical spine: Implications for airway management. Can J Anaesth. 1990;37:77–93.
26 Burney RE, Maio RF, Maynard F, et al. Incidence, characteristics and outcome of spinal cord injury at trauma centers in North America. Arch Surg. 1993;128:596–599.
27 Vanderlan WB, Tew BE, McSwain NE. Increased risk of death with cervical spine immobilisation in penetrating cervical trauma. Injury. 2009;40:880–883.
28 Vanderlan WB, Tew BE, Seguin CY, et al. Neurologic sequelae of penetrating cervical trauma. Spine. 2009;34:2646–2653.
29 Brywczynski JJ, Barrett TW, Lyon JA, et al. Management of penetrating neck injury in the emergency department: a structured literature review. Emerg Med J. 2008;25:711–715.
30 Walls RM. Airway management in the blunt trauma patient: How important is the cervical spine? Can J Surg. 1992;35:27–30.
31 Berne JD, Velmahos GC, El-Tawil Q, et al. Value of complete cervical helical computed tomographic scanning in identifying cervical spine injury in the unevaluable blunt trauma patient with multiple injuries: A prospective study. J Trauma. 1999;47:896–902.
32 Gonzalez RP, Fried PO, Bukhalo M, et al. Role of clinical examination in screening for blunt cervical spine injury. J Am Coll Surg. 1999;189:152–157.
33 Domenicucci M, Preite R, Ramieri A, et al. Three-dimensional computed tomographic imaging in the diagnosis of vertebral column trauma: Experience based on 21 patients and review of the literature. J Trauma. 1997;42:254–259.
34 Streitwieser DR, Knopp R, Wales LR, et al. Accuracy of standard radiographic views in detecting cervical spine fractures. Ann Emerg Med. 1983;12:538–542.
35 Ross SE, Schwab CW, David ET, et al. Clearing the cervical spine: Initial radiologic evaluation. J Trauma. 1987;27:1055–1060.
36 Griffen MM, Frykberg ER, Kerwin AJ, et al. Radiographic clearance of blunt cervical spine injury: Plain radiograph or computed tomography scan? J Trauma. 2003;55:222–226.
37 Majernick TG, Bieniek R, Houston JB, et al. Cervical spine movement during orotracheal intubation. Ann Emerg Med. 1986;15:417–420.
38 Donaldson WF, Heil BV, Donaldson VP, et al. The effect of airway maneuvers on the unstable C1-C2 segment. A cadaver study. Spine. 1997;22:1215–1218.
39 Brimacombe J, Keller C, Künzel KH, et al. Cervical spine motion during airway management: A cinefluoroscopic study of the posteriorly destabilized third cervical vertebrae in human cadavers. Anesth Analg. 2000;91:1274–1278.
40 Adachi YU, Satomoto M, Higuchi H, et al. Fentanyl attenuates the hemodynamic response to intubation more than the response to laryngoscopy. Anesth Analg. 2002;95:233–237.
41 White PF, Schlobohm RM, Pitts LH, et al. A randomized study of drugs for preventing increases in intracranial pressure during endotracheal suctioning. Anesthesiology. 1982;57:242–244.
42 Yano M, Nishiyama H, Yokota H, et al. Effect of lidocaine on ICP response to endotracheal suctioning. Anesthesiology. 1986;64:651–653.
43 Brown MM, Parr MJ, Manara AR. The effect of suxamethonium on intracranial pressure and cerebral perfusion pressure in patients with severe head injuries following blunt trauma. Eur J Anaesthesiol. 1996;13:474–477.
44 Kirkegaard-Nielsen H, Caldwell JE, Berry PD. Rapid tracheal intubation with rocuronium: A probability approach to determining dose. Anesthesiology. 1999;91:131–136.
45 Stirt JA, Grosslight KR, Bedford RF, et al. “Defasciculation” with metocurine prevents succinylcholine-induced increases in intracranial pressure. Anesthesiology. 1987;67:50–53.
46 Robinson N, Clancy M. In patients with head injury undergoing rapid sequence intubation, does pretreatment with intravenous lidocaine lead to an improved neurologic outcome? A review of the literature. Emerg Med J. 2001;18:453–457.
47 Butler J, Jackson R. Towards evidence based emergency medicine: Best BETs from Manchester Royal Infirmary. Lignocaine premedication before rapid sequence induction in head injuries. Emerg Med J. 2002;19:554.
48 Brooks D, Anderson CM, Carter MA, et al. Clinical practice guidelines for suctioning the airway of the intubated and nonintubated patient. Can Respir J. 2001;8:163–181.
49 Bachofen M. Suppression of blood pressure increases during intubation: Lidocaine or fentanyl? Anaesthesist. 1988;37:156–161.
50 Samaha T, Ravussin P, Claquin C, et al. Prevention of increase of blood pressure and intracranial pressure during endotracheal intubation in neurosurgery: Esmolol versus lidocaine. Ann Fr Anesth Reanim. 1996;15:36–40.
51 Yano M, Nishiyama H, Yokota H, et al. Effect of lidocaine on ICP response to endotracheal suctioning. Anesthesiology. 1986;64:651–653.
52 Bedford RF, Persing JA, Pobereskin L, et al. Lidocaine or thiopental for rapid control of intracranial hypertension? Anesth Analg. 1980;59:435–437.
53 Donegan MF, Bedford RF. Intravenously administered lidocaine prevents intracranial hypertension during endotracheal suctioning. Anesthesiology. 1980;52:516–518.
54 Grover VK, Reddy GM, Kak VK, et al. Intracranial pressure changes with different doses of lignocaine under general anesthesia. Neurol India. 1999;47:118–121.
55 Splinter WM, Cervenko F. Haemodynamic responses to laryngoscopy and tracheal intubation in geriatric patients: Effects of fentanyl, lidocaine and thiopentone. Can J Anaesth. 1989;36:370–376.
56 Perry J, Lee J, Wells G. Rocuronium versus succinylcholine for rapid sequence induction intubation. Cochrane Database Syst Rev. (1):2003. CD002788
57 Schramm WM, Strasser K, Bartunek A, et al. Effects of rocuronium and vecuronium on intracranial pressure, mean arterial pressure and heart rate in neurosurgical patients. Br J Anaesth. 1996;77:607–611.
58 Kirkegaard-Nielsen H, Caldwell JE, Berry PD. Rapid tracheal intubation with rocuronium: A probability approach to determining dose. Anesthesiology. 1999;91:131–136.
59 Kihara S, Brimacombe J, Yaguchi Y, et al. Hemodynamic responses among three tracheal intubation devices in normotensive and hypertensive patients. Anesth Analg. 2003;96:890–895.
60 Maharaj CH, Buckley E, Harte BH, et al. Endotracheal intubation in patients with cervical spine immobilization. Anesthesiology. 2007;107:53–59.
61 Takahashi S, Mizutani T, Miyabe M, et al. Hemodynamic responses to tracheal intubation with the laryngoscope versus lightwand intubating device (Trachlight) in adults with normal airway. Anesth Analg. 2002;95:480–484.
62 Cunningham AJ, Barry P. Intraocular pressure—Physiology and implications for anaesthetic management. Can Anaesth Soc J. 1986;33:195–208.
63 Vachon CA, Warner DO, Bacon DR. Succinylcholine and the open globe. Tracing the teaching. Anesthesiology. 2003;99:220–223.
64 Inci I, Ozcelik C, Tacyildiz I, et al. Penetrating chest injuries: Unusually high incidence of high-velocity gunshot wounds in civilian practice. World J Surg. 1998;22:438–442.
65 Billard V, Moulla F, Bourgain JL, et al. Hemodynamic response to induction and intubation. Propofol/fentanyl interaction. Anesthesiology. 1994;81:1384–1393.
66 Haas DA, Harper DG. Ketamine: A review of its pharmacologic properties and use in ambulatory anesthesia. Anesth Prog. 1992;39:61–68.
67 Waxman K, Shoemaker WC, Lippmann M. Cardiovascular effects of anesthetic induction with ketamine. Anesth Analg. 1980;59:355–358.
68 Albanese J, Arnarud S, Rey M, et al. Ketamine decreases intracranial pressure and electroencephalographic activity in traumatic brain injury patients during propofol sedation. Anesthesiology. 1997;87:1328–1334.
69 Lindeburg T, Spotoft H, Bredgaard Sorensen M, et al. Cardiovascular effects of etomidate used for induction and in combination with fentanyl-pancuronium for maintenance of anaesthesia in patients with valvular heart disease. Acta Anaesthesiol Scand. 1982;26:205–208.
70 Shapiro BM, Wendling WW, Ammaturo FJ, et al. Vascular effects of etomidate administered for electroencephalographic burst suppression in humans. J Neurosurg Anesthesiol. 1998;10:231–236.
71 Modica PA, Tempelhoff R. Intracranial pressure during induction of anaesthesia and tracheal intubation with etomidate-induced EEG burst suppression. Can J Anaesth. 1992;39:236–241.
72 Sagarin MJ, Barton ED, Sakles JC, et al. Underdosing of midazolam in emergency endotracheal intubation. Acad Emerg Med. 2003;10:329–338.
73 Eaton MP, Dhillon AK. Relative performance of the level 1 and ranger pressure infusion devices. Anesth Analg. 2003;97:1074–1077.
74 de Guzman E, Shankar MN, Mattox K. Limited volume resuscitation in penetrating thoracoabdominal trauma. AACN Clin Issues. 1999;10:61–68.
75 Revell M, Greaves I, Porter K. Endpoints for fluid resuscitation in hemorrhagic shock. J Trauma. 2003;54:S63–S67.
76 Kreimeier U, Lackner CK, Prückner S, et al. Permissive hypotension in severe trauma. Anaesthesist. 2002;51:787–799.
77 Husain FA, Martin MJ, Mullenix PS, et al. Serum lactate and base deficit as predictors of mortality and morbidity. Am J Surg. 2003;185:485–491.
78 Durbin CGJ. Sedation of the agitated, critically ill patient without an artificial airway. Crit Care Clin. 1995;11:913–936.
79 Hedges D, Jeppson K, Whitehead P. Antipsychotic medication and seizures: A review. Drugs Today (Barc). 2003;39:551–557.
80 Kao LW, Kirk MA, Evers SJ, et al. Droperidol, QT prolongation, and sudden death: What is the evidence? Ann Emerg Med. 2003;41:546–558.
81 Brimacombe JR, Berry AM. Cricoid pressure. Can J Anaesth. 1997;44:414–425.
82 Ellis DY, Harris T, Zideman D. Cricoid pressure in emergency department rapid sequence tracheal intubations: A risk-benefit analysis. Ann Emerg Med. 2007;50:653–665.
83 Olsen JC, Gurr DE, Hughes M. Video analysis of EM residents performing RSI. J Emerg Med. 2000;18:469–472.
84 Allman KG. The effect of cricoid pressure on airway patency. J Clin Anesth. 1995;7:197–199.
85 Halsam N. Effect of cricoid pressure on the view at laryngoscopy. Anaesthesia. 2005;60:41–47.
86 Aoyama K, Takenaka I, Sata T, et al. Cricoid pressure impedes positioning and ventilation through the laryngeal mask airway. Can J Anaesth. 1996;43:1035–1040.
87 Whittington RM, Robinson JS, Thompson JM. Fatal aspiration (Mendelson’s) syndrome despite antacids and cricoid pressure. Lancet. 1979;2:228–230.
88 Williamson R. Cricoid pressure. Can J Anaesth. 1989;36:601.
89 Howells TH, Chamney AR, Wraight WJ, et al. The application of cricoid pressure. An assessment and a survey of its practice. Anaesthesia. 1983;38:457–460.
90 Kopka A, Crawford J. Cricoid pressure: A simple, yet effective biofeedback trainer. Eur J Anaesthesiol. 2004;21:443–447.
91 Smith KJ, Dobranowski J, Yip G, et al. Cricoid pressure displaces the esophagus: An observational study using magnetic resonance imaging. Anesthesiology. 2003;99:60–64.
92 Salem MR, Wong AY, Mani M, et al. Efficacy of cricoid pressure in preventing gastric inflation during bag-mask ventilation in pediatric patients. Anesthesiology. 1974;40:96–98.
93 Moynihan RJ, Brock-Utne J, Archer JH, et al. The effect of cricoid pressure on preventing gastric insufflation in infants and children. Anesthesiology. 1993;78:652–656.
94 Lawes ED, Campbell L, Mercer D. Inflation pressure, gastric insufflation and rapid sequence intubation. Br J Anaesth. 1987;59:315–318.
95 Neilipovitz DT, Crosby ET. No evidence for decreased incidence of aspiration after rapid sequence induction. Can J Anesth. 2007;54:748–764.
96 Godwin SA. Blind intubation techniques. In: Walls RM, Murphy MF, Luten RC. Manual of emergency airway management. ed 3. Philadelphia: Lippincott Williams & Wilkins; 2008:104–111.
97 Walls RM. Airway management in the blunt trauma patient: How important is the cervical spine? Can J Surg. 1992;35:27–30.
98 Walls RM. Airway management. Emerg Med Clin North Am. 1993;11:53–60.
99 Gerling MC, Davis DP, Hamilton RS, et al. Effects of cervical spine immobilization technique and laryngoscope blade selection on an unstable cervical spine in a cadaver model of intubation. Ann Emerg Med. 2000;36:293–300.
100 Majernick TG, Bieniek R, Houston JB, et al. Cervical spine movement during orotracheal intubation. Ann Emerg Med. 1986;15:417–420.
101 Walls RM. Airway management in the blunt trauma patient: How important is the cervical spine? Can J Surg. 1992;35:27–30.
102 Walls RM, Brown CA, III., Bair AE, et al. Emergency airway management: A multi-center report of 8937 emergency department intubations. J Emerg Med. 2011;41:347–354.
103 Murphy MF, Walls RM. Identification of the difficult and failed airway. In: Walls RM, Murphy MF, Luten RC. Manual of emergency airway management. ed 3. Philadelphia: Lippincott Williams & Wilkins; 2008:81–93.
104 Reed MJ, Dunn MJ, McKeown DW. Can an airway assessment score predict difficulty at intubation in the emergency department? Emerg Med J. 2005;22:99–102.
105 Langeron O, Masso E, Hurax C, et al. Prediction of difficult mask ventilation. Anesthesiology. 2000;92:1229–1236.
106 Brown CA, III., Bair AE, Pallin DJ, et al. Improved glottic exposure in adult emergency department tracheal intubations. Ann Emerg Med. 2010;56:83–88.
107 Tremblay MH, Williams S, Robitaille A, et al. Poor visualization during direct laryngoscopy and high upper lip bite test score are predictors of difficult intubation with the GlideScope videolaryngoscope. Anesth Analg. 2008;106:1495–1500.
108 Schenarts CL, Burton JH, Riker RR. Adrenocortical dysfunction following etomidate induction in emergency department patients. Acad Emerg Med. 2001;8:1–7.
109 Hildreth AN, Mejia VA, Maxwell RA, et al. Adrenal suppression following a single dose of etomidate for rapid sequence induction: A prospective randomized study. J Trauma. 2008;65:573–579.
110 Warner KJ, Cuschieri J, Jurkovich GJ, et al. Single-dose etomidate for rapid sequence intubation may impact outcome after severe injury. J Trauma. 2009;67:45–50.
111 Himmelseher S, Durieux ME. Revising a dogma: Ketamine for patients with neurological injury? Anesth Analg. 2005;101:524–534.
112 Perry JJ, Lee JS, Sillberg VA, et al. Rocuronium versus succinylcholine for rapid sequence induction intubation. Cochrane Database Syst Rev. (2):2008. CB002788
113 Patanwala AE, Stahl SA, Sakles JC, et al. Comparison of succinylcholine and rocuronium for first-attempt intubation success in the emergency department. Acad Emerg Med. 2011;18:10–14.
114 Haas DA, Harper DG. Ketamine: A review of its pharmacologic properties and use in ambulatory anesthesia. Anesth Prog. 1992;39:61–68.
115 Walls RM. The emergency airway algorithms. In: Walls RM, Murphy MF, Luten RC. Manual of emergency airway management. ed 3. Philadelphia: Lippincott Williams & Wilkins; 2008:8–22.
116 Rai M, Dering A, Verghese C. The Glidescope system: A clinical assessment of performance. Anaesthesia. 2005;60:60–64.
117 Kaplan MB, Hagberg CA, Ward DS, et al. Comparison of direct and video-assisted views of the larynx during routine intubation. J Clin Anesth. 2006;18:357–362.
118 Aziz MF, Healy D, Kheterpal S, et al. Routine clinical practice effectiveness of the Glidescope in difficult airway management: An analysis of 2,004 Glidescope intubations, complications, and failures from two institutions. Anesthesiology. 2011;114:34–41.
119 Arslan ZI, Tildiz T, Baykara ZN, et al. Tracheal intubation in patients with rigid collar immobilization of the cervical spine: A comparison of Airtraq and LMA Ctrach devices. Anaesthesia. 2009;64:1332–1336.
120 Davis DP, Valentine C, Ochs M, et al. The Combitube as a salvage airway device for paramedic rapid sequence intubation. Ann Emerg Med. 2003;42:697–704.
121 Yardy N, Hancox D, Strang T. A comparison of two airway aids for emergency use by unskilled personnel. The Combitube and laryngeal mask. Anaesthesia. 1999;54:181–183.
122 Brimacombe J, Keller C, Kunzel KH, et al. Cervical spine motion during airway management: A cinefluoroscopic study of the posteriorly destabilized third cervical vertebrae in human cadavers. Anesth Analg. 2000;91:1274–1278.
123 Mercer MH, Gabbott DA. Insertion of the Combitube airway with the cervical spine immobilised in a rigid cervical collar. Anaesthesia. 1998;53:971–974.
124 Mercer MH, Gabbott DA. The influence of neck position on ventilation using the Combitube airway. Anaesthesia. 1998;53:146–150.
125 Lam NC, Hagberg CA, Bassilli LM. Use of the video laryngoscopy for Combitube exchange in a difficult airway. J Clin Anesth. 2009;21:294–296.
126 Choyce A, Avidan MS, Shariff A. A comparison of the intubating and standard laryngeal mask airways for airway management by inexperienced personnel. Anaesthesia. 2001;56:357–360.
127 Langeron O, Semjen F, Bourgain JL, et al. Comparison of the intubating laryngeal mask airway with the fiberoptic intubation in anticipated difficult airway management. Anesthesiology. 2001;94:968–972.
128 Agro F, Brimacombe J, Carassiti M, et al. The intubating laryngeal mask—Clinical appraisal of ventilation and blind tracheal intubation in 110 patients. Anaesthesia. 1998;53:1084–1090.
129 Brain AI. Use of the LMA in the unstable cervical spine. Singapore Med J. 2001;1:46–48.
130 Russi CS, Miller L, Hartley MJ. A comparison of the King-LT to endotracheal intubation and Combitube in a simulated difficult airway. Prehosp Emerg Care. 2008;12:35–41.