CHAPTER 14 THE PHYSIOLOGY OF SLEEP
Sleep is an essential and appetitive behavior characterized by minimal movement; reduced responsiveness to stimuli; reversibility; and species-specific diurnal timing, duration, and preferred posture.1 The appetitive and essential nature of sleep is clearly evident in the human’s inability to maintain continuous wakefulness for more than 2 to 3 days. As a state of sleep need progressively increases with attempts at prolonged wakefulness, sleep begins to intrude into wakefulness as brief microsleeps occurring during ongoing behavior and as longer episodes of unintended sleep during periods of inactivity.2 The inability to completely deprive oneself of sleep after 2 to 3 days, in contrast to one’s ability to avoid food or fluids and thereby deprive oneself to death, demonstrates the compulsory nature of sleep. In fact, the compulsory nature of sleep accounts for much of the morbidity associated with sleep loss (e.g., car accidents).
Sleep in humans is recognized behaviorally by its recumbence and eye closure, but some mammals sleep with open eyes (e.g., cattle) or while standing (e.g., horse, elephant).1 The immobility of the sleep state is relative in that sleep walking and talking occur in some human sleep disorders and, among animals, some fish swim in place and mammals move about periodically. The two characteristics of arousability and rapid reversibility differentiate sleep from death, coma, and hibernation. Nonvisual sensory monitoring of both exogenous and endogenous stimuli continues during the sleep state. For example, a vital stimulus, hypoxemia, readily arouses even a severely sleep-deprived individual; similarly, a parent is easily aroused by the cry of his or her baby. In fact, sensory discrimination continues during sleep, inasmuch as a parent does not arouse to the cry of another baby, corrected for stimulus intensity differences. Average daily sleep time varies from 2 to 20 hours among mammals, typically being 8 hours for humans.3 The single best correlate of variation in sleep length among mammals appears to be metabolic rate.3 Whereas the major sleep period in humans typically occurs as a single bout during the dark hours, for some mammals sleep is linked to the daylight period and occurs in multiple bouts.
NATURE OF SLEEP
Because sleep would be disrupted if it were assessed behaviorally (e.g., testing arousal threshold), sleep scientists measure sleep electrophysiologically, which is less obtrusive and more precise.4 The simultaneous recording of the electroencephalogram (EEG), the electro-oculogram, and the electromyogram are the accepted standard measures of sleep and waking, a standardized procedure termed polysomnography. The polysomnogram correlates well with behavioral observations. But it also reveals further subtleties not apparent behaviorally or subjectively. Sleep is an active, complex, and highly organized process composed of two distinct brain states of sleep: rapid eye movement (REM) and non-rapid eye movement (NREM).
Electrophysiology of NREM and REM sleep
The electro-oculogram of REM sleep is characterized by rapid conjugate eye movements (hence the name of this sleep state). The cortical EEG of REM sleep reverts to the low-voltage, mixed-frequency pattern of drowsy sleep. The second defining characteristic of REM sleep is its skeletal muscle atonia, which is reflected in the electromyogram achieving its lowest level of the night. The muscle atonia of REM sleep occurs through a process of postsynaptic inhibition of motor neurons at the dorsal horn of the spinal cord. Another important feature of REM sleep is its tonic and phasic components. The tonic components of REM sleep are the persistent muscle atonia and the desynchronized EEG. The phasic components are intermittent and include bursts of eye movements occurring against a background of electro-oculographic quiescence. Coupled with the eye movement bursts are muscle twitches, typically involving peripheral muscles. These twitches are superimposed on the tonic muscle atonia of REM and probably reflect sympathetic drive breaking through the postsynaptic inhibition (see the following discussion of the autonomic nervous system during sleep).
Physiological Function during Sleep
Autonomic Nervous System
The activity of the autonomic nervous system varies between the two sleep states (NREM and REM) and the wakefulness state.5 Parasympathetic activity increases during NREM sleep in relation to wakefulness. It remains relatively increased during both tonic and phasic REM sleep. Sympathetic activity remains constant during wakefulness and NREM sleep and is slightly reduced during tonic REM sleep. Consequently, parasympathetic activity predominates during sleep with the exception of phasic REM sleep. Sympathetic drive is dramatically increased during phasic REM sleep, and it predominates despite the increased parasympathetic activity of phasic REM sleep.
Respiratory System
Breathing patterns and the control of respiration are different in sleep and wakefulness.6 Minute ventilation is decreased from waking levels by 13% to 15% during NREM sleep. Two factors are responsible: First, the nonmetabolic drive to breathe in wakefulness is removed with the onset of NREM sleep; second, airflow resistance is enhanced, as a result of a reduction of upper airway dilator muscle tone that occurs in conjunction with the general reduction of skeletal muscle tone of sleep. During the tonic skeletal muscle atonia of REM sleep, airway resistance is further increased in comparison with that of NREM sleep, resulting in a twofold increase in relation to that of wakefulness. This heightened airway resistance, coupled with the autonomic nervous system sympathetic activation, particularly in phasic REM sleep, leads to irregular breathing patterns and even respiratory pauses during REM sleep.
Thermal Regulation
Altered thermoregulation is also displayed in the NREM and REM sleep states.7 The thermal set point is reduced in NREM sleep in relation to the wakefulness state. Consequently, sweating and shivering occur at lower temperatures during NREM sleep than during wakefulness. Again, REM sleep is unique in that there is no temperature regulation during REM sleep and sweating and shivering cease during REM sleep. If a person remained in REM sleep long enough, body temperature would equilibrate to the ambient temperature. However, REM episodes are never much longer than 30 minutes, and thus noticeable body temperature fluctuations do not occur during REM sleep.
REGULATION OF SLEEP AND WAKEFULNESS
Homeostatic Regulation
Homeostatic regulation of sleep has been inferred from measurement of the amount of electroencephalographic slow-wave activity during the sleep period, the auditory arousal threshold during sleep, the total amount and continuity of sleep, and the speed of falling asleep at night and during the day.8 Reductions of sleep time yield increases in these various measures, whereas increases in sleep time yield reductions in these measures, with two exceptions: sleep continuity and arousal threshold, which behave conversely. For example, computer-assisted quantification of slow-wave activity during sleep shows an increased amount of slow-wave activity during recovery sleep after total or partial sleep deprivation. During normal sleep, in the absence of prior deprivation, the amount of slow-wave activity diminishes in each successive NREM sleep cycle across the night. Measuring the speed of falling asleep throughout the day on a standard measure, the Multiple Sleep Latency Test, also suggests the existence of an underlying homeostatic process for sleep.4 A single night in which sleep time is reduced by 2 to 8 hours produces a linear increase in the speed of falling asleep on the Multiple Sleep Latency Test the following day, and nightly sleep durations reduced by as little as 1 to 2 hours across successive nights accumulate to increase speed of falling asleep the following day. Conversely, extension of sleep duration beyond 8 hours, or a compensatory nap, produces a reduction in the speed of falling asleep on the Multiple Sleep Latency Test.9
Circadian Regulation
In addition to, and independent of, the homeostatic process is a circadian process that organizes sleep and wakefulness according to the 24-hour day and in phase with the light-dark cycle. The suprachiasmatic nucleus is the biological clock.10 It receives input from the retinohypothalamic tract that serves to synchronize the suprachiasmatic nucleus to the light-dark cycle. The suprachiasmatic nucleus efferent fibers then convey circadian timing signals that regulate a variety of physiological rhythms. Circadian phase typically is documented in humans by recording body temperature and in animals by recording wheel running. The daily human body temperature nadir occurs between 3:00 and 5:00 am; a secondary decline in body temperature appears at about midday and peaks between 5:00 and 8:00 pm. The speed of falling asleep and the duration of sleep episodes parallel the body temperature rhythm; rapid sleep onsets and long durations occur over the temperature nadirs, whereas long onsets and short durations occur over temperature peaks.
Hormonal and metabolic rhythms also are driven by the suprachiasmatic nucleus. For example, thyroid-stimulating hormone, cortisol, prolactin, growth hormone, and melatonin all show a circadian rhythm. Some of these hormones are linked to sleep (i.e., prolactin and growth hormone); that is, their release is delayed when sleep is delayed, at least acutely. Other hormones (e.g., cortisol) are directly linked to the light-dark cycle with their basal circadian rhythm remaining regardless of the timing of sleep. Melatonin is considered to be the internal hormonal signal that communicates the light-dark cycle throughout the body.11 Its production and release are controlled by the suprachiasmatic nucleus, and it is expressed during darkness and suppressed during light. The release of melatonin attenuates the alerting pulse of the suprachiasmatic nucleus, thereby facilitating sleep onset in the dark. A brief pulse of light interrupting darkness produces a rapid decline in melatonin levels, which continues for the duration of the light pulse. Its hypnotic capacity, beyond its chronobiotic characteristic, is unclear.
Homeostatic and Circadian Interaction
Models that conceptualize the interaction of the homeostatic and circadian processes have been developed; the most widely cited model is the two-process of Borbely and colleagues.12 In this model, the sleep process (process S) builds during wakefulness and decreases during sleep. The circadian process (process C) promotes wakefulness and gates the expression of sleep at the appropriate circadian phase, if process S has reached its threshold. Another model, the opponent-process model, assigns the role of actively promoting wakefulness to the suprachiasmatic nucleus, the circadian pacemaker, which opposes an accumulating sleep drive.13 The alerting signal of the suprachiasmatic nucleus has a circadian rhythm, which, when absent or low, allows the expression of the sleep drive. When present at its peak, the alerting signal opposes the expression of sleep even when the sleep drive approaches its peak level. Although these models clearly have heuristic value, several critical questions remain. The biochemical or molecular substrates of process S, or the “sleep drive,” are not known, and the neurobiological pathways by which process C interacts with sleep mechanisms have not been identified. On the other hand, an understanding of the neurobiological controls of wakefulness and sleep is emerging, which is discussed as follows.
NEUROBIOLOGICAL CONTROLS OF WAKE AND SLEEP
Wake
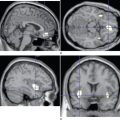
Giuseppe Moruzzi and Horace Winchell Magoun in 1949 identified an ascending arousal system, which they termed the reticular activating system, that regulates the level of forebrain wakefulness, but its origins were not characterized until 2001.15 The system consists of two main pathways: one innervating the thalamus and the other extending into the hypothalamus.15 The thalamic path originates from cholinergic pedunculopontine and laterodorsal tegmental (PPT-LDT) nuclei, and the hypothalamic path consists of noradrenergic locus ceruleus and serotoninergic dorsal and median raphe nuclei projections, which are joined at the hypothalamus by histaminergic tuberomammillary nucleus projections. These all project diffusely to the cortex. Electrophysiological recordings have verified the role of these nuclei in wakefulness.14 The locus ceruleus, dorsal and median raphe, and tuberomammillary nuclei fire at their fastest rate during wakefulness, are slowed in slow-wave sleep, and silent in REM sleep. In contrast, the PPT-LDT nuclei fire at their fastest rate during REM sleep, also fire during wakefulness, and are silent during slow-wave sleep.
Sleep
The critical element in initiating sleep is inhibitory pulses generated by neurons in the ventrolateral preoptic (VLPO) nucleus, which project to the tuberomammillary, locus ceruleus, and dorsal and median raphe nuclei and to the PPT-LDT nuclei.14 The majority of these projections are γ-amino butyric acid mediated (GABAergic) and galaninergic and appear to inhibit the monoaminergic and cholinergic arousal systems. Electrophysiological recordings of neurons in the VLPO nucleus have shown that they fire at highest rates during sleep and are silent during wakefulness. The relation of the VLPO nucleus to monoaminergic and cholinergic arousal systems is reciprocal. The VLPO nucleus receives input from these systems that, during wakefulness, inhibit the VLPO nucleus’s sleep-promoting effect. The VLPO nucleus also receives input from the retina and the suprachiasmatic nucleus, which may provide the circadian signal for sleep initiation. But this step has not been verified.
Bistable Flip-Flop
The reciprocal relation of the VLPO nucleus to monoaminergic and cholinergic arousal systems was characterized as a bistable flip-flop by Saper and colleagues.15 Rapid firing of the VLPO nucleus inhibits the arousal system, which in turn disinhibits its own firing. Similarly, rapid firing of the arousal systems inhibits the VLPO nucleus, which thereby disinhibits the firing of these systems. Such a model, derived from electrical engineering, provides for stability of sleep and wakefulness states, no intermediate states, and rapid transitions between states. Once the sleep or wakefulness threshold is reached, a rapid reversal of firing patterns occurs. Because circadian signals and homeostatic sleep drive change slowly and continuously, a bistable system ensures rapid transitions and no entry into intermediate states.
Saper and colleagues incorporated the recently discovered orexin/hypocretin peptides into the model in the role of stabilizing behavioral state.14 Orexin/hypocretin peptides were discovered in 1998 by two different investigating groups as neurotransmitters synthesized in the lateral hypothalamus. Orexin/hypocretin neurons were found to innervate all the ascending arousal systems and, furthermore, to project to the VLPO nucleus. On the basis of gene knockout studies in mice and genetic studies of humans with narcolepsy, both which show that the absence of orexin/hypocretin signaling via the type 2 receptor leads to intrusions of sleep into wakefulness, it appears that these neurons have an important role in maintaining wakefulness and further stabilizing sleep-wake state.14
SUMMARY
Borbely AA, Achermann PA. Sleep homeostasis and models of sleep regulation. In: Kryger MH, Roth T, Dement WC, editors. Principles and Practice of Sleep Medicine. 4th ed. Philadelphia: WB Saunders; 2005:405-417.
Carskadon MA, Dement WC. Normal human sleep: an overview. In: Kryger MH, Roth T, Dement WC, editors. Principles and Practice of Sleep Medicine. 4th ed. Philadelphia: WB Saunders; 2005:13-23.
Czeisler CA, Turek FW. Melatonin, sleep and circadian rhythms: current progress and controversies [Special Issue]. J Biol Rhythms. 1997;12:485-708.
Roth T, Roehrs T. An overview of normal sleep and sleep disorders. Eur J Neurol. 2000;7(Suppl 4):3-8.
Saper CB, Chou TC, Scammell TE. The sleep switch: hypothalamic control of sleep and wakefulness. Trends Neurosci. 2001;24:726-731.
1 Tobler I. Is sleep fundamentally different between mammalian species? Behav Brain Res. 1995;69:35-54.
2 Roehrs T, Carskadon MA, Dement WC, et al. Daytime sleepiness and alertness. In: Kryger MH, Roth T, Dement WC, editors. Principles and Practice of Sleep Medicine. 4th ed. Philadelphia: WB Saunders; 2005:39-50.
3 Zepelin H, Siegel JM, Tobler I. Mammalian sleep. In: Kryger MH, Roth T, Dement WC, editors. Principles and Practice of Sleep Medicine. 4th ed. Philadelphia: WB Saunders; 2005:91-100.
4 Rechtschaffen A, Kales A. A Manual of Standardized Techniques and Scoring System for Sleep Stages of Human Sleep. Los Angeles: Brain Information Service/Brain Research Institute, University of California at Los Angeles, 1968.
5 Roth T, Roehrs T. An overview of normal sleep and sleep disorders. Eur J Neurol. 2000;7(Suppl 4):3-8.
6 Issa FG, Suratt PM, Remmers JE, editors. Sleep and Respiration. New York: John Wiley, 1990.
7 Heller HC. Temperature, thermoregulation, and sleep. In: Kryger MH, Roth T, Dement WC, editors. Principles and Practice of Sleep Medicine. 4th ed. Philadelphia: WB Saunders; 2005:292-304.
8 Borbely AA, Achermann PA. Sleep homeostasis and models of sleep regulation. In: Kryger MH, Roth T, Dement WC, editors. Principles and Practice of Sleep Medicine. 4th ed. Philadelphia: WB Saunders; 2005:405-417.
9 Roehrs T, Shore E, Papineau K, et al. A two-week sleep extension in sleepy normals. Sleep. 1996;19:576-582.
10 Turek FW, Dugovic C, Laposky AD. Master circadian clock, master circadian rhythm. In: Kryger MH, Roth T, Dement WC, editors. Principles and Practice of Sleep Medicine. 4th ed. Philadelphia: WB Saunders; 2005:318-320.
11 Czeisler CA, Turek FW. Melatonin, sleep and circadian rhythms: current progress and controversies [Special Issue]. J Biol Rhythms. 1997;12:485-708.
12 Achermannn P, Dijk DJ, Brunner DP, et al. A model of human sleep homeostasis based on EEG slow-wave activity: quantitative comparison of data and simulations. Brain Res Bull. 1993;31:97-113.
13 Egar DM, Dement WC, Fuller CA. Effect of SCN lesions on sleep in squirrel monkeys: evidence for opponent processes in sleep-wake regulation. J Neurosci. 1993;13:1065-1079.
14 Moruzzi G, Magoun H. Brain stem reticular formation and activation of the EEG. Electroencephalogr Clin Neurophysiol. 1949;1:455-473.
15 Saper CB, Chou TC, Scammell TE. The sleep switch: hypothalamic control of sleep and wakefulness. Trends Neurosci. 2001;24:726-731.