Chapter 129 The Obese Patient
Obesity is a global issue. An estimated 300 million people throughout the world are obese, defined as having a body mass index (BMI) of 30 kg/m2 or more and 1.5 billion are overweight (BMI ≥25 kg/m2).1 From 2007 to 2008, the prevalence of obesity in the United States was 32.2% among men and 35.5% among women.2 Healthy People 2010 set a goal, in 2001, of lowering the percentage of people in the United States with obesity to 15%. In 2010, Colorado was the only state with an obesity rate below 22%. Thirty-six states had obesity rates of 25% or higher, with the rate in 12 of those 36 states being 30% or above.3 The implications of obesity are far reaching. Medical costs related to obesity accounted for 9.1% of total U.S. medical expenditures in 1998, with total direct and indirect costs estimated to be $147 billion in 2000.4 If the prevalence of obesity currently were the same as it was in 1987, health care spending in the United States would be 10% lower per person, or about $200 billion less each year.5
Obesity is a major risk factor for many diseases and conditions, including type 2 diabetes, hypertension, cardiovascular disease, pulmonary dysfunction, kidney disease, metabolic syndrome, and certain types of cancer. The prevalence of 11 chronic conditions, including those previously mentioned, associated with obesity grew 180% from 1997 to 2005, an increase equal to approximately 29 million additional cases of chronic conditions.5 The implications for spine surgery are multifaceted, including poor wound healing, infection risk, caregiver safety, anesthesia considerations, intraoperative challenges, equipment needs, and biomechanical considerations.
Obesity and Overweight
BMI is defined as the weight in kilograms divided by the square of the height in meters (kg/m2). A BMI over 25 kg/m2 is defined as overweight, and a BMI greater than 30 kg/m2 is defined as obese. Obesity rates, rising threefold or more since 1980 in some areas of North America, the United Kingdom, Eastern Europe, the Middle East, the Pacific Islands, Australasia, and China, is attributed to societal changes that have led to increased consumption of nutrient-poor and energy-dense foods combined with reduced physical activity.1 These changes have dramatically affected children—worldwide it is estimated that 22 million children under age 5 and 18 million children between the ages of 6 to 13 years are overweight or obese. Approximately 30% of Australian, 25.5% of American, and 28.7% of Greek children are overweight or obese.6 The ability to be outdoors is the strongest correlate with physical activity in children. Decreased physical activity and, consequently, decreased energy expenditure, coupled with increased caloric intake, is a major factor in childhood obesity throughout the world.6
Lumbar Spine Disease
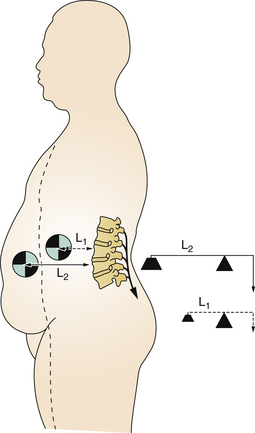
Increasing weight causes increased axial loading on the spine. People with increased abdominal girth experience a ventral shift of the center of gravity, leading to loss of neutral position and sagittal alignment. As a result, the thorax is ventral to the pelvis, dramatically increasing the forces experienced by the spine. The repetitive, usual movements associated with activities of daily living are cumulative, subjecting the spine to excessive loads (Fig. 129-1).
The cumulative effect was demonstrated in a radiographic comparison of range of motion in obese and nonobese patients with chronic back pain. Reduced range of motion in obese participants was found to be due to reduced mobility at the pelvic and thoracic levels as well as an increased ventral pelvic tilt. Obesity in this study also was associated with increased lumbar lordosis.7
Repetitive axial loading and loss of sagittal balance in the obese population is known to lead to degenerative changes in the spine. Degenerative characteristics in the lumbar spine were evaluated in a sample of 187 individuals randomly selected from an ancillary project to the Framingham Study. There was a significantly higher prevalence of facet joint disease in obese subjects.8
Hangai et al. investigated factors associated with lumber intervertebral disc degeneration in the elderly. Aging, high BMI, high levels of low-density lipoprotein cholesterol, occupational lifting, and sport activities were all associated with degenerative disc disease in this group of 51- to 86-year-old subjects.9 High BMI was associated with level 4 degenerative disc disease. Aortic calcification/atherosclerosis and lumbar artery stenosis/occlusion also have been associated with lumbar disc degeneration and low back pain.10
A recent meta-analysis of 33 studies evaluated the association between obesity and low back pain. A statistically significant association between BMI and low back pain was noted by Shiri et al., including seeking care for low back pain and chronic low back pain in persons who are overweight or obese.11 The association between excess weight and a higher prevalence of low back pain was stronger in women than men. Increased BMI was a risk factor for low back pain and low back pain–related disability in women.12 A relationship has been reported between low back pain and obesity in women but not men. Waist circumference has been found to be a more significant factor than BMI.13
Thirty-eight patients (30 women, 8 men) were prospectively assessed for their axial low back pain before and after bariatric surgery. Study participants decreased their BMI from 52.25 ± 12.61 kg/m2 to 38.32 ± 9.66 kg/m2 (P < .0001). Twelve months after surgery, participants’ VAS scale scores had decreased from 5.2 ± 3.35 to 2.9 ± 3.1 postoperatively (P = .006). Patients experienced increases in mean physical health and mental health components on the 36-Item Short Form Health Survey (SF-36). Low back pain disability demonstrated significant improvement postoperatively as noted on participants’ Oswestry Disability Index scores.14
Obesity and Associated Comorbidities
Cardiovascular
The cardiovascular implications of obesity include altered metabolism as well as changes in cardiac structure and function. Risk factors associated with obesity include dyslipidemia, hypertension, glucose intolerance, elevated inflammatory markers, and sleep apnea. Adipose tissue is surrounded by an extensive capillary network and functions as an endocrine organ, synthesizing and releasing a variety of compounds. Approximately 30% of the total circulating concentrations of interleukin-6 (IL-6), which modulates C-reactive protein production, originates from adipose tissue.15
Hypervolemia from increased extracellular volume and increased cardiac output are evident in the hypertensive obese patient. Hypertension leads to left ventricular hypertrophy. As hypertension continues, the left ventricle becomes progressively noncompliant, increasing the risk of heart failure.16
Hemodynamically, obese individuals have an increased total blood volume and cardiac output caused by the metabolic demand of increased BMI. Left ventricular hypertrophy and diastolic dysfunction as well as cardiomyopathy are correlated with obesity, and may be predisposing factors to heart failure.15 However, most of the extra volume is distributed to the adipose tissue, whereas renal and cerebral blood flow are normal.16
Diagnostic electrocardiogram interpretation also is influenced by obesity. Changes that may occur include increased heart rate, increased P-R interval, increased QRS interval, increased or decreased QRS voltage, increased Q-T interval, ST-T abnormalities, left axis deviation, flattening of the T wave in inferolateral leads, left atrial abnormalities, and false-positive criteria for inferior myocardial infarction.15
Hypertension is about six times more common in obese individuals. Cardiovascular dysmetabolic syndrome, also known as metabolic syndrome, associates hypertension with an increase in visceral fat. Additionally, a chronic inflammatory state, as evidenced by elevated C-reactive protein and IL-6 levels, may play a role in elevated blood pressure.15
Obese patients may be quite sedentary, with limited mobility, and may not have subjective complaints of cardiac impairment. Early symptoms usually are exertional dyspnea and orthopnea; however, severely obese individuals often do not sleep in bed, and sleep in a nonrecumbent position, such as in a reclining chair. Electrocardiograms may be low voltage and may underestimate right and left ventricular hypertrophy.16 Careful preoperative assessment is necessary.
Diabetes
A recent meta-analysis found type II diabetes associated with overweight and obese individuals.17 Diabetic patients who underwent cervical fusion secondary to myelopathy were found to be male, older, and have more levels fused. They also were more likely to have respiratory, cardiac, and peripheral vascular complications; hematoma or bleeding; transfusion; and dysphagia, with longer lengths of stay and more nonroutine discharges.18
Olsen et al. found diabetes to be the highest independent risk of spinal surgical site infection, and an elevated preoperative or postoperative serum glucose level was independently associated with increased risk of surgical site infection.19
Infection Risk
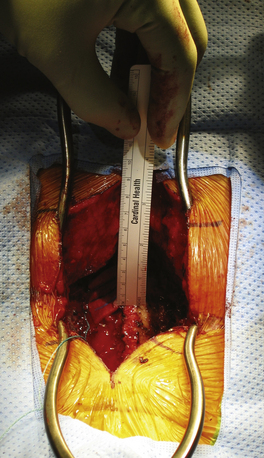
Obesity is associated with a number of changes in skin physiology, including larger skin folds and increased amount of sweating, which increase moisture and skin friction. Lymphedema can occur because of altered lymphatic flow. Lymphedema is associated with reduced tissue oxygenation and a chronic inflammatory state. Subcutaneous fat, made up almost entirely of white adipose tissue, plays a role in endocrine functions and metabolism of lipids and glucose20 (Fig. 129-2).
Obesity is a well-known risk factor for postoperative surgical site infection.21–24 Watters et al. completed an evidence-based clinical guideline for the use of prophylactic antibiotics in spine surgery. Their conclusions were that while the obese patient population is at a higher risk for postoperative infection, the literature did not yield evidence that would support modification of standard therapy.25
Pulmonary
The respiratory consequences of obesity include alterations in lung volumes, lung mechanics, gas exchange, and respiratory control. In short, reduced expiratory reserve volume, reduced functional residual capacity, reduced total lung capacity, and increased residual volume have significant implications for the anesthetized patient. Careful attention is needed during induction, because obese patients rapidly desaturate despite preoxygenation as a result of a smaller functional residual capacity and an increase in oxygen consumption.16
Mechanically, there is reduced lung and chest wall compliance, increased airway resistance and work of breathing, as well as respiratory muscle inefficiency. Total compliance can fall to 30% of predicted normal.16
Obstructive sleep apnea, difficult intubation, risk of aspiration, and positioning during induction can present unique anesthetic challenges.26 Anatomic alterations associated with obesity include increased adipose tissue around the upper airway, and upper airway collapsibility is higher. Central obesity has been associated with reduced lung volumes. Structural alterations are further compounded by neuromuscular control disturbances, which also appear to play a role in sleep apnea.27
Pharmacokinetics
Factors that affect drug dosing in obese patients include increased adipose tissue, renal blood flow, glomerular filtration rate, and total blood volume; elevated cardiac output; altered protein binding; and decreased total body water.28 Both fat and lean masses are increased as compared with nonobese counterparts. The increase in lean body mass is 20% to 40% of total excess weight. However, the fat mass of total body weight increases more than lean mass, resulting in a decreased percentage of lean body mass and water as compared with otherwise similar nonobese patients, with the volume of drug distribution larger in obese individuals.29
Lipophilic drugs such as benzodiazepines, barbiturates, and propofol require larger loading doses in obese patients due to their elevated volume of distribution. However, maintenance dosing should be based on drug clearance. If the drug clearance is similar or reduced in the obese patient, the maintenance dose generally is based on ideal body weight. If drug clearance is increased in the obese person, then the dose is calculated on total body weight. Thus, midazolam used as a loading dose should be calculated on total body weight, whereas maintenance dosing should be calculated on ideal body weight.30
Diagnostic Considerations
The physical examination may be less than optimal due to the patient’s body habitus. Maneuvers such as the straight-leg raise and heel-toe walking may not be possible. Sensory disturbances such as stocking distribution peripheral neuropathy may be present. Diabetic neuropathy also can mask signs of myelopathy.
Caregiver Safety
Nurses’ aides, orderlies, and attendants have the highest rates of work-acquired musculoskeletal disorders.31 In one institution, the rate of work injuries attributed to obese patient handling was found to be 29.8%, and 27.9% of all lost work days and 37.2% of all restricted work days were attributed to bariatric patient handling.32 Caregiver safety as well as patient safety is of the utmost importance in the context of obese spine patient handling. Ergonomically safe work environments that utilize state-of-the-art patient handling equipment must be a top priority for all health care organizations.32–40
Surgical Issues in Obesity
Shamji et al. completed an analysis of 244,170 thoracolumbar and lumbar spinal fusions done in obese patients. They found that these patients had an increased number of blood transfusions and an increased likelihood of discharge to assisted living. Morbidly obese patients undergoing dorsal fusion were more likely to experience wound complications and postoperative wound infections.41
Operative Table and Positioning
The Jackson table is radiolucent and has a load-bearing capacity of up to 500 pounds. The Jackson table allows the abdomen to hang freely in the prone position, reducing epidural venous bleeding. Appropriate and ample padding as well as immobilization are especially necessary for patient safety. Gel pads are used to protect from pressure and subsequent skin breakdown. Skin is protected before the use of tape for immobilization. Peripheral nerve palsies from positioning and the increased patient body mass can cause traction stresses on the axillary and/or peripheral neurovascular bundles.21 Operating table failure has been reported, so heightened attention to standard procedures should be followed.42
The goal of proper positioning is to obtain optimal exposure and visualization while optimizing cardiovascular and respiratory dynamics and avoiding blood loss, venous congestion, neurovascular compromise, and pressure point complications.43 Supine, lateral decubitus, kneeling, and sitting positions all require the same preplanned, individualized approach to ensure patient safety. Additionally, preprocedure general medical conditions and anesthetic considerations should be included in preoperative planning.44
The sitting position poses potential challenges due to the obese patient’s large ventral mass along with limited flexibility. Additionally, the obese patient has the tendency to slip downward during the procedure, and shoulder immobilization may interfere with the operative field. Generally, the prone position provides adequate positioning for dorsal cervical approaches with fewer potential concerns.43
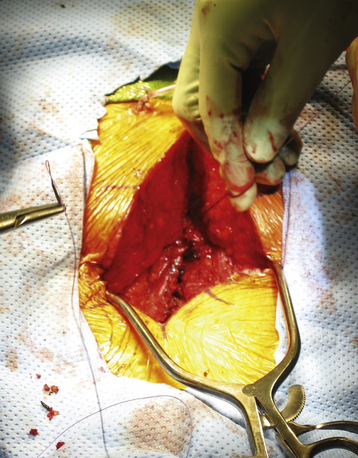
Preplanning is key, regardless of the patient positioning strategy used. Preplanning requires keen attention to available equipment, staffing, and what strategy is safest for the patient and care providers while still being able to meet the operative goals (Fig. 129-3).
Surgical Exposure
Optimal exposure depends directly on appropriate positioning and type of approach, appropriate incision size and configuration, adequate muscular relaxation, and the use of an appropriate retractor system. The approach and exposure must take into account the patient’s specific body habitus. Additionally, intraoperative localization can be challenging with this patient population.43
Wound Closure
Meticulous attention to tight wound closure will aid in the prevention of postoperative wound complications. The poor vascularity of adipose tissue and the overall thickness and lack of strength of the adipose layer for suture retention contribute to the morbidity associated with the wound in an obese patient. Dead space should be minimized with multilayered closure. Use of a closely spaced, interrupted dermal layer of suture, as well as approximation of the superficial fascia within the adipose layer, may add to the strength of the superficial approximation. Additionally, placement of a wound drain will prevent accumulation of blood and body fluid, which can be quite significant in the obese patient. Accumulation of blood and body fluid can lead to chronic wound leakage, a tense and painful wound area, hematoma formation, and potential for a large fluid-filled cavity in the surgical area and a nonhealing wound (Fig. 129-4).
Superficial drainage often is seen initially after surgery. Care providers must be taught to provide meticulous, frequent wound care. With persistent or recurrent drainage or dehiscence, general surgical techniques with superficial opening, debridement, and, if necessary, packing of the wound is warranted. Many wound-healing products are available, and consultation with a wound and skin care provider can be considered. Deeper subfascial infections usually require operative debridement and thorough irrigation followed by fascial reapproximation and layered drainage or suprafascial packing with healing by granulation. If debridement of the wound edges is required, large retention sutures or surgical undermining may be helpful for wound reapproximation.43
Postoperative Management and Complication Prevention
The relationship of obesity to perioperative complications in spine surgery was evaluated by Patel et al. They found the risk of major complications increased with increasing BMI. In patients whose BMI was 25 to 29.9, the estimated chance of a major complication was 14%. Risk of major complication increased to 20% with a BMI of 30 to 39.9, and to 36% when the BMI was 40 or over.21
Summary
Obesity is a global health care issue affecting children and adults. The spine surgeon requires a heightened awareness of the associated comorbid conditions and potential challenges in caring for this patient population. Significant surgical preplanning, orchestration of personnel and appropriate equipment, and coordination with the patient’s general medical providers are needed. Obesity itself is not a contraindication to surgery, but the patient must be well informed of his or her particular additional operative risks, and patient and physician expectations for the surgical intervention should be clearly communicated.
Patel N., Bagan B., Vadera S., et al. Obesity and spine surgery: relation to perioperative complications. J Neurosurg Spine. 2007;6:291-297.
Poirier P., Giles T., Bray G., et al. Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss: an update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2006;113:898-918.
Shiri R., Karppinen J., Leno-Arjas P. The association between obesity and low back pain: a meta-analysis. Am J Epidemiol. 2009;171:135-154.
Sinha A. Some anesthetic aspects of morbid obesity. Curr Opin Anaesthesiol. 2009;22:442-446.
Thorp K., Ogden L., Galactionova K. Weighty matters: how obesity drives poor health and health spending in the U.S. 2009. www.businessgrouphealth.org/pdfs/NBGH%20WeightyMatters_Final.pdf.. Accessed January 24, 2010
U.S. Department of Veterans Affairs. Safe bariatric patient handling toolkit. www.visn8.va.gov/patientsafetycenter/safePtHandling/toolkitBariatrics.asp. Accessed November 24, 2009
Yosipovitch G., DeVore A., Dawn A. Obesity and the skin: skin physiology and skin manifestation of obesity. J Am Acad Dermatol. 2007;6:901-916.
1. World Health Organization. www.who.int/mediacentre/factsheets/fs311/en/. Accessed December 6, 2011.
2. Flegal K., Carroll M., Ogden C., Curtin L. Prevalence and trends in obesity among US adults, 1999-2008. JAMA. 2010;303:235-241.
3. Centers for Disease Control. www.cdc.gov/obesity/data/trends.html. . Accessed December 7, 2011.
4. Centers for Disease Control. www.cdc.gov/obesity/causes/economics.html. . Accessed December 7, 2011
5. Thorp K., Ogden L., Galactionova K. Weighty matters: how obesity drives poor health and health spending in the U.S. 2009. . www.businessgrouphealth.org/pdfs/NBGH%20WeightyMatters_Final.pdf.. Accessed January 24, 2010
6. Ben-Sefer E., Ben-Natan M., Ehrenfeld M. Childhood obesity: current literature, policy and implications for practice. Int Nurs Rev. 2009;56:166-173.
7. Vismara L., Menegoni J., Zaina F., et al. Effect of obesity and low back pain on spinal mobility: a cross sectional study of women. J Neuroeng Rehabil. 2010;7:3.
8. Kalichman L., Guermazi A., Li L., Hunter D. Association between age, sex, BMI and CT-evaluated spinal degenerative features. J Back Musculoskelet Rehabil. 2009;22:189-195.
9. Hangai M., Kaneoka K., Kuno S., et al. Factors associated with lumbar intervertebral disc degeneration in the elderly. Spine J. 2008;8:732-740.
10. Kauppila L. Atherosclerosis and disc degeneration/low-back pain: a systematic review. Eur J Vasc Endovasc Surg. 2009;37:661-670.
11. Shiri R., Karppinen J., Leno-Arjas P. The association between obesity and low back pain: a meta-analysis. Am J Epidemiol. 2009;171:135-154.
12. Urquhart D., Bell R., Cicuttini F., et al. Low back pain and disability in community-based women: prevalence and associated factors. Menopause. 2009;16:24-29.
13. Shiri R., Solovieva S., Husgafvel-Pusiainen K., et al. The association between obesity and the prevalence of low back pain in young adults: the cardiovascular risk in young Finns study. Am J Epidemiol. 2008;167:1110-1119.
14. Khoueir P., Black M., Crookes P., et al. Prospective assessment of axial back pain symptoms before and after bariatric weight reduction surgery. Spine J. 2009;9:454-463.
15. Poirier P., Giles T., Bray G., et al. Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss: an update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2006;113:898-918.
16. Murphy P., Adams J. The pathophysiology of obesity and its implications for anesthesia. In: Hemmings J., Hopkins P., editors. Foundations of anesthesia: basic sciences for clinical practice. ed 2. Philadelphia: Elsevier; 2006:855-866.
17. Guh D., Zhang W., Bansback N., et al. The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health. 2009;9:1-20.
18. Cook C., Tackett S., Chah A., et al. Diabetes and perioperative outcomes following cervical fusion in patients with myelopathy. Spine. 2008;33:E254-E260.
19. Olson M., Nepple J., Riew D., et al. Risk factors for surgical site infection following orthopaedic spinal operations. J Bone Joint Surg [Am]. 2008;90:62-69.
20. Yosipovitch G., DeVore A., Dawn A. Obesity and the skin: skin physiology and skin manifestation of obesity. J Am Acad Dermatol. 2007;6:901-916.
21. Patel N., Bagan B., Vadera S., et al. Obesity and spine surgery: relation to perioperative complications. J Neurosurg Spine. 2007;6:291-297.
22. Pull ter Bunne A., Cohen D. Incidence, prevalence, and analysis of risk factors for surgical site infection following adult spinal surgery. Spine. 2009;34:1422-1428.
23. Veeravau A., Paril C., Lad S., Boakye M. Risk factors for postoperative spinal wound infections after spinal decompression and fusion surgeries. Spine. 2009;34:1869-1872.
24. Fang A., Hu S., Endres N., Bradford D. Risk factors for infection after spinal surgery. Spine. 2005;30:1460-1465.
25. Watter W., Baisden J., Bono C., et al. Antibiotic prophylaxis in spine surgery: an evidence-based clinical guideline for the use of prophylactic antibiotics in spine surgery. Spine J. 2009;9:142-146.
26. Sinha A. Some anesthetic aspects of morbid obesity. Curr Opin Anaesthesiol. 2009;22:442-446.
27. Schwartz A., Patil S., Laffan A., et al. Obesity and obstructive sleep apnea. Proc Am Thorac Soc. 2008;5:185-192.
28. Lewis K. Anesthesia issues in patients undergoing gastric-bypass surgery. In: Farray F., Forse R., editors. Bariatric surgery: a primer for your medical practice. Thorofare, NJ: Slack; 2006:83-104.
29. Poggesi I., Benedetti M., Whomsley R., et al. Pharmacokinetics in special populations. Drug Metab Rev. 2009;41:422-454.
30. Casati A., Putzu M. Anesthesia in the obese patient: pharmacokinetic considerations. J Clin Anesth. 2005;17:134-145.
31. Bureau of Labor Statistics. Nonfatal occupational injuries and illnesses requiring days away from work, 2008. USDL-09–1454. . www.bls.gov/news.release/archives/osh2_12042009.pdf.. Accessed November 24, 2009
32. Randall S., Pories W., Pearson A., Drake D. Expended occupational safety and health administration 300 log as metric for bariatric patient handling staff injuries. Surg Obes Relat Dis. 2009;5:463-468.
33. Muir M, Archer-Heese G. Essentials of a bariatric patient handling program. Online J Issues Nurs 14:1-8. Accessed January 31, 2009.
34. Camden S. Obesity: an emerging concern for patients and nurses. Online J Issues Nurs 14:1-8. Accessed January 31, 2009.
35. Rose M., Drake D., Baker G., et al. Caring for morbidly obese patients: safety considerations for nurse administrators. Nurs Manage. 2008;11:47-50.
36. Muir M., Archer-Heese G., McLean D. Handling of the bariatric patient in critical care: a case study of lessons learned. Crit Care Nurse Clin North Am. 2007;19:223-240.
37. AORN position statement on ergonomically healthy workplace practices. www.aorn.org/PracticeResources/AORNPositionStatements/Position_Ergonomics/. Accessed January 31, 2010
38. Edlich R., Hudson M., Buschbacher R., et al. Devastating injuries in healthcare workers: descriptions of the crisis and legislative solution to the epidemic of back injury from patient lifting. J Long Term Eff Med Implants. 2005;15:225-241.
39. Department of Veterans Affairs. Patient care ergonomics resource guide: safe patient handling and movement. www.visn8.va.gov/visn8/patientsafetycenter/resguide/ErgoGuidePtOne.pdf.. Accessed November 24, 2009
40. Safe Bariatric Patient Handling Toolkit. www.visn8.va.gov/patientsafetycenter/safePtHandling/toolkitBariatrics.asp. Accessed November 24, 2009.
41. Shamji M., Parker S., Cook C., et al. Morbidity associated with fusion of the thoracolumbar and lumbar spine. Neurosurgery. 2009;65:490-498.
42. Dauber M., Roth S. Operating table failure: another hazard of spine surgery. Anesth Analg. 2009;108:904-905.
43. Cheng J., Schmidt M., Mueller W., Benzel E. The obese patient. In: Benzel E., editor. Spine surgery: techniques, complication avoidance, and management. ed 2. Philadelphia: Elsevier; 2004:pp 1320-1332.
44. Schonauet C., Bocchetti A., Barbagallo G., et al. Positioning on surgical table. Eur Spine J. 2004;13(Suppl 1):S50-S55.