7
The normal menstrual cycle
Introduction
Evolutionary aspects
Humans are one of the few species which have a monthly reproductive cycle. Most mammals ovulate less frequently than once a month, for example, sheep ovulate once a year and rabbits ovulate in response to coitus. In these species, insemination usually leads to pregnancy, but in normal humans, there is only a 30% chance of conception at each ovulation. The high frequency of ovulation in our species compensates for our relatively low fertility.
Overview of the cycle
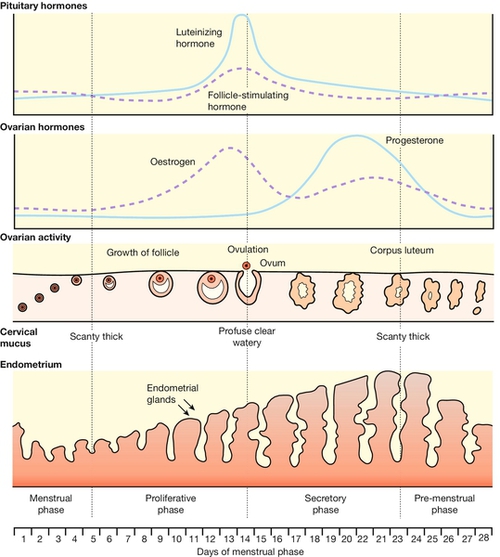
The menstrual cycle can be described by referring to either the uterus or the ovary. The endometrial cycle results from the growth and shedding of the uterine lining – the endometrium. At the end of the menstrual phase, the endometrium thickens again – the proliferative phase. After ovulation, endometrial growth stops and the glands become more active and full of secretions – the secretory phase.
These endometrial changes are controlled by the ovarian cycle. The average duration of the ovarian cycle is 28 days and it is composed of:
![]() a follicular phase
a follicular phase
![]() ovulation
ovulation
![]() a post-ovulatory or luteal phase.
a post-ovulatory or luteal phase.
If the cycle is prolonged, the follicular phase lengthens (longer time to ovulation) but the luteal phase remains constant at 14 days. Fundamental to the normal menstrual cycle are:
![]() an intact hypothalamo–pituitary–ovarian endocrine axis
an intact hypothalamo–pituitary–ovarian endocrine axis
![]() the presence of responsive follicles in the ovaries
the presence of responsive follicles in the ovaries
![]() a functional uterus.
a functional uterus.
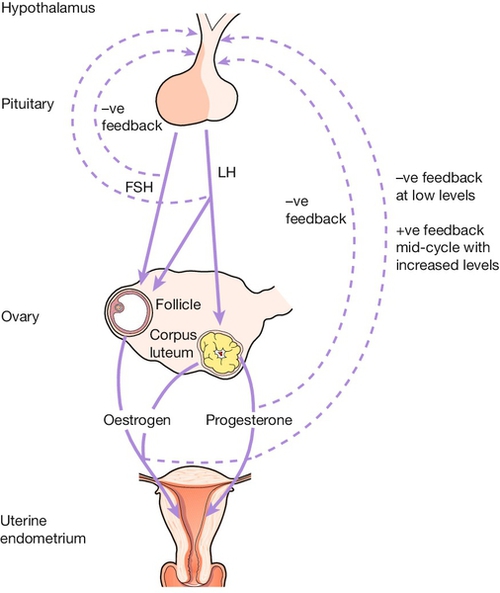
Endocrine control of the menstrual cycle
Control of follicular maturation and ovulation is exercised by the hypothalamo–pituitary–ovarian axis (Fig. 7.1). The hypothalamus controls the cycle, but it can itself be influenced by higher centres in the brain, allowing factors such as anxiety or stress to affect the cycle. The hypothalamus acts on the pituitary gland by secreting gonadotrophin-releasing hormone (GnRH), a decapeptide which is secreted in a pulsatile manner. The pulses are secreted approximately every 90 min. GnRH travels through the small blood vessels of the pituitary portal system to the anterior pituitary, where it acts on the pituitary gonadotrophs to stimulate the synthesis and release of follicle-stimulating hormone (FSH) and luteinizing hormone (LH). Although there are two gonadotrophins, it appears that there is a single releasing hormone for both.
FSH is a glycoprotein which stimulates growth of follicles during the ‘follicular phase’ of the cycle. FSH also stimulates sex hormone secretion, predominantly of oestradiol, by the granulosa cells of the mature ovarian follicle.
LH is also a glycoprotein. LH also stimulates sex hormone production (testosterone, which is subsequently converted by the action of FSH into oestradiol). LH plays an essential role in ovulation. It is the mid-cycle surge of LH which triggers rupture of the mature follicle with release of the oocyte. Post-ovulatory production of progesterone by the corpus luteum is also under the influence of LH.
Both FSH and LH and the other two glycoprotein hormones – thyroid-stimulating hormone (TSH) and human chorionic gonadotrophin (hCG) – are composed of two protein subunits, the alpha chain and the beta chain. The amino acid sequence of the alpha subunit is common to all four glycoproteins, but the beta chains are distinctive to each hormone. Sensitive assays for these hormones therefore have to be specific for the beta chain.
The cyclical activity within the ovary which constitutes the ovarian cycle is maintained by the feedback mechanisms which operate between the ovary, the hypothalamus, and the pituitary. These are described in the next section.
The ovarian cycle
Follicular phase
Days 1–8
At the start of the cycle, levels of FSH and LH rise in response to the fall of oestrogen and progesterone at menstruation. This stimulates development of 10–20 follicles. The follicle which is most sensitive to FSH, is the ‘dominant’ follicle, and is the one destined to reach full maturation and ovulation. This dominant follicle appears during the mid-follicular phase, while the remainder undergo atresia. With growth of the dominant follicle, oestrogen levels increase.
Days 9–14
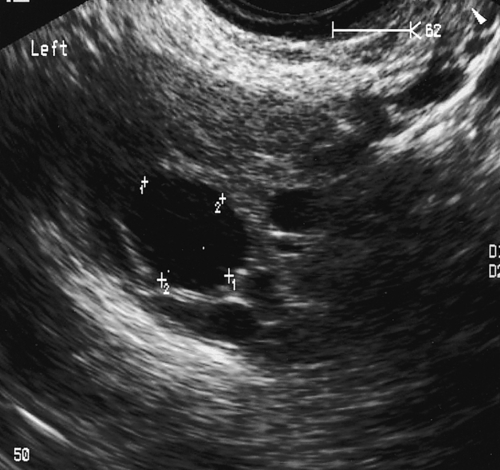
As the follicle increases in size, localized accumulations of fluid appear among the granulosa cells and become confluent, giving rise to a fluid-filled central cavity called the antrum (Fig. 7.2), which transforms the primary follicle into a Graafian follicle (see History box), in which the oocyte occupies an eccentric position, surrounded by two to three layers of granulosa cells termed the cumulus oophorus.
Associated with follicular maturation, there is a progressive increase in the production of oestrogen (mainly oestradiol) by the granulosa cells of the developing follicle. As the oestrogen level rises, the release of both gonadotrophins is suppressed (negative feedback), which serves to prevent hyperstimulation of the ovary and the maturation of multiple follicles.
The granulosa cells also produce inhibin. This has been implicated as a factor in the restriction of the number of follicles undergoing maturation.
Ovulation
Day 14
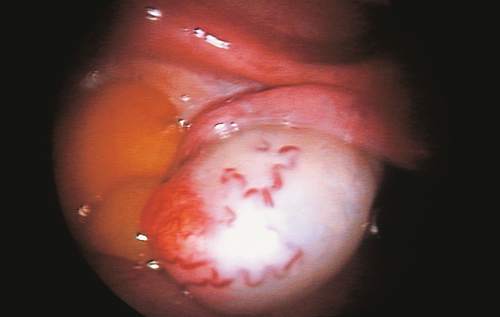
Ovulation is associated with rapid enlargement of the follicle, followed by protrusion from the surface of the ovarian cortex and rupture of the follicle with extrusion of the oocyte and adherent cumulus oophorus (Fig. 7.3). Some women can identify the time of ovulation because they experience a short-lived pain in one or other iliac fossa. Ultrasound studies have shown that this pain – known as ‘mittelschmerz’ – actually occurs just before follicular rupture.
The final rise in oestradiol concentration is thought to be responsible for the subsequent mid-cycle surge of LH and, to a lesser extent, of FSH – positive feedback. Immediately before ovulation there is a precipitous fall in oestradiol levels and an increase in progesterone production. Ovulation follows within 18 h of the mid-cycle surge of LH.
Luteal phase
Days 15–28
The remainder of the Graafian follicle which is retained in the ovary, is penetrated by capillaries and fibroblasts from the theca. The granulosa cells undergo luteinization and these structures collectively form the corpus luteum (Fig. 7.4). This is the major source of the sex steroid hormones, oestrogen and progesterone, secreted by the ovary in the postovulatory phase.
Establishment of the corpus luteum results in a marked increase in progesterone secretion and a second rise in oestradiol levels. Progesterone levels peak 1 week after ovulation (day 21 of the 28-day cycle). Tests of serum progesterone at this time may be used in fertility investigations to confirm the occurrence of ovulation.
During the luteal phase gonadotrophin levels reach a nadir and remain low until the regression of the corpus luteum, which occurs at days 26–28. If conception and implantation occur, the corpus luteum does not regress, because it is maintained by hCG secreted by the trophoblast. The detection of the presence of hCG in a sample of urine forms the basis of pregnancy testing. If, however, conception and implantation have not occurred successfully, the corpus luteum regresses, progesterone levels fall, and menstruation ensues. The consequent fall in the levels of sex hormones allows the FSH and LH levels to rise and initiate the next cycle.
The uterine cycle
The cyclical production of sex hormones by the ovary induces important changes in the uterus. These involve the endometrium and cervical mucus.
The endometrium
The endometrium is composed of two layers: a superficial layer which is shed in the course of menstruation and a basal layer which does not take part in this process but which regenerates the superficial layer during the subsequent cycle.
The junction between these layers is marked by a change in the character of the arterioles supplying the endometrium. The portion traversing the basal endometrium is straight, but thereafter its course becomes convoluted, giving rise to the spiral section of the arteriole. This anatomical configuration assumes importance in the physiological shedding of the superficial layers of the endometrium.
Proliferative phase
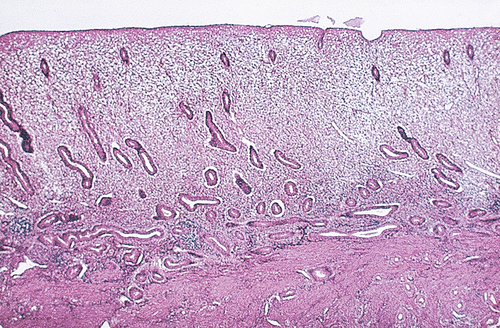
During the follicular phase in the ovary, the endometrium is exposed to oestrogen secretion. After menstruation, the secretion of oestradiol from the ovary brings about repair and regeneration of the endometrium. With ongoing exposure to oestradiol there is ongoing growth and proliferation of glands and blood vessels. At this stage – the ‘proliferative’ phase – the glands are tubular and arranged in a regular pattern, parallel to each other (Fig. 7.5).
Secretory phase
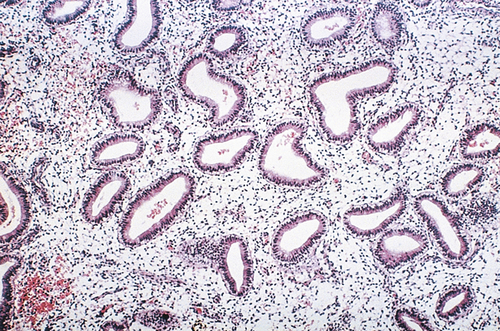
After ovulation, progesterone production induces secretory changes in the endometrial glands, preparing the endometrium for implantation (Fig. 7.6). This is first evident as the appearance of secretory vacuoles in the glandular epithelium below the nuclei. This swiftly progresses to secretion of material into the lumen of the glands, which become tortuous and their margins appear serrated.
Menstrual phase
Normally, the luteal phase of the ovary lasts for 14 days, at the end of which, regression of the corpus luteum is associated with a decline in ovarian oestrogen and progesterone production. This fall is followed by intense spasmodic contraction of the spiral section of the endometrial arterioles, giving rise to ischaemic necrosis, shedding of the superficial layer of the endometrium and bleeding.
The vasospasm appears to be due to local production of prostaglandins. Prostaglandins may also account for the increased uterine contractions at the time of the menstrual flow. The failure of menstrual blood to clot has been ascribed to the presence of local fibrinolytic activity in the endometrial blood vessels, which reaches a peak at the time of menstruation.
Cervical mucus
The glands of the cervix secrete cervical mucus. This changes in quantity and character throughout the cycle in response to sex hormones from the ovary:
![]() early in the follicular phase the cervical mucus is scant
early in the follicular phase the cervical mucus is scant
![]() later in the follicular phase, the increasing oestrogen levels induce changes in the composition of the mucus (becomes more stretchy). This change is described by the term ‘spinnbarkheit’. The water content increases progressively so that just before ovulation occurs the mucus has become watery and is easily penetrated by the spermatozoa. This mid-cycle mucus has a characteristic fern-like pattern when examined microscopically (Fig. 7.7).
later in the follicular phase, the increasing oestrogen levels induce changes in the composition of the mucus (becomes more stretchy). This change is described by the term ‘spinnbarkheit’. The water content increases progressively so that just before ovulation occurs the mucus has become watery and is easily penetrated by the spermatozoa. This mid-cycle mucus has a characteristic fern-like pattern when examined microscopically (Fig. 7.7).
![]() After ovulation the progesterone secreted by the corpus luteum counteracts the effect of the oestrogen, and the mucus becomes thick and impermeable. This prevents entry of further spermatozoa. This effect on mucus is one of the ways by which the progestogen-only methods of contraception exert their contraceptive effect.
After ovulation the progesterone secreted by the corpus luteum counteracts the effect of the oestrogen, and the mucus becomes thick and impermeable. This prevents entry of further spermatozoa. This effect on mucus is one of the ways by which the progestogen-only methods of contraception exert their contraceptive effect.
These changes can be monitored by the woman herself, if she is using the ‘rhythm method’ of contraception. In the clinic the changes can be monitored by examining cervical mucus under the low power of a microscope.
Other cyclical changes
Although the purpose of the cyclical changes in ovarian hormones is to affect the genital tract, these hormones circulate throughout the body and can affect other organs.
Basal body temperature
A rise in basal body temperature of approximately 0.5°C occurs following ovulation and is sustained until the onset of menstruation. This is due to the thermogenic effect of progesterone acting at the hypothalamic level. Should conception occur, the elevation in basal body temperature is maintained throughout pregnancy. A similar effect can be induced by the administration of progestogens.
Breast changes
The human mammary gland is very sensitive to oestrogen and progesterone. Breast swelling is often the first sign of puberty, in response to the small increase in ovarian oestrogen. Oestrogen and progesterone act synergistically on the breast, and, during the normal cycle, breast swelling occurs in the luteal phase, apparently in response to increasing progesterone levels. The swelling is probably due to vascular changes and is not due to changes in the glandular tissue.
Psychological changes
Some women notice changes in mood during the menstrual cycle, with an increase in emotional lability in the late luteal phase. Such changes may be directly due to falling levels of progesterone, although mood changes are not always closely synchronized with hormonal fluctuations. The dividing line between normal cyclical changes and the pre-menstrual syndrome is unclear (see Chapter 14).