16
Genital prolapse
Introduction
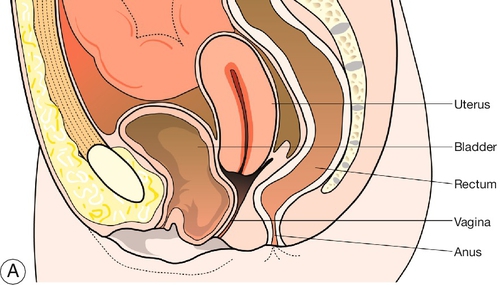
Uterovaginal prolapse is described as the descent of one or more of the pelvic organs (urethra, bladder, uterus, Pouch of Douglas (POD) and rectum) into the vagina. While prolapse of a single organ independently can happen, typically more than one organ will be involved. This is because all of the organs which can prolapse (with the exception of the POD) are attached either directly or indirectly to the pelvic floor musculature. Of women who have had children, 30% will develop prolapse. The lifetime risk of requiring surgery for prolapse is around 11%.
Aetiology
The aetiology of genital prolapse is pelvic floor muscle weakness. Other contributing factors are listed in Box 16.1. In addition, obesity, chronic cough and constipation, which all raise intra-abdominal pressure, can aggravate the condition.
Childbirth
Childbirth results in trauma to the pelvic floor and loss of tissue support to the female pelvic organs. While direct trauma can happen at the time of vaginal delivery, the biggest problem in the long term is pudendal nerve damage, which causes a gradual weakening of the fascia and neuromuscular tissue of the pelvic floor. A prolonged labour, in particular a prolonged second stage and a large baby are the biggest risk factors. The pudendal nerve is crushed against the bony pelvis during labour and the longer the patient is in labour, the worse the damage is likely to be. This explains why prolapse seldom happens immediately after childbirth but rather many years later. The same aetiology is responsible for stress urinary incontinence, which demonstrates the same time scale. While the aetiological problem starts in labour, some of the factors mentioned below, along with obesity, are typically the triggers for the development of symptomatic prolapse.
Menopause
The menopausal state, characterized by oestrogen deficiency and loss of connective tissue strength, is a causative factor in the development of prolapse.
Congenital
Congenital weakness and neurological deficiency of the tissues account for prolapse in a small proportion of women. Rarely, children may be born with prolapse or they may develop significant prolapse during childhood. There may also be anatomical variants that may make certain women more susceptible to prolapse in later life.
Gynaecological surgery
Although surgery is often used to treat prolapse, it may be responsible for a small number of cases. Suprapubic surgical procedures for urinary incontinence (e.g. Burch colposuspension – see History box) alter the anatomy such that the bladder neck is approximated behind the symphysis pubis. This increases gravitational effects on the pouch of Douglas, prolapse of which leads to enterocele. Prolapse of the vaginal vault is a not uncommon long-term consequence of a hysterectomy.
Genetic
Genetic factors have been implicated in the development of prolapse. It is uncommon, for example, in the African population, possibly related in some way to the different collagen content of tissues.
Classification
The classification of prolapse, and the main symptoms, are summarized in Table 16.1.
Table 16.1
Types of genital prolapse
| Original position of organs | Prolapse | Symptomsa |
| Anterior | Urethrocele
Cystocele |
Stress urinary incontinence Poor bladder emptying, residual urine, frequency and urinary infection |
| Central | Cervix/uterus (1st-, 2nd-, 3rd-degree and procidentia) and vaginal vault | Bleeding and/or discharge from ulceration in association with procidentia Backache |
| Posterior | Enterocele (POD) Rectocele |
Pressure, backache Difficulty in bowel emptying |
a In addition to the general symptoms of discomfort, dragging, the feeling of a ‘lump’, and, rarely, coital problems.
Urethrocele
A urethrocele is descent of the part of the anterior vaginal wall which is fused to the urethra. This is approximately the first 3–4 cm of the anterior wall superior to the urethral meatus. Any descent of this tissue may alter the urethrovesical angle and disrupt the continence mechanism, predisposing to stress urinary incontinence (SUI).
Cystocele
The bladder base lies immediately above this. Descent of this area is termed a cystocele (Fig. 16.1). Urethroceles and cystoceles may prolapse together, and when both are present the term cystourethrocele is used.
Uterus and cervix
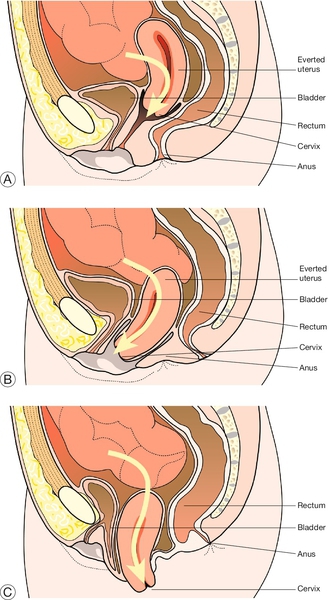
The cervix occupies the upper third of the vagina and descends when there is uterine prolapse. Uterine prolapse may be described as first, second or third degree (Fig. 16.2):
![]() first degree – there is descent of the uterus and cervix within the vagina but the cervix does not reach the introitus
first degree – there is descent of the uterus and cervix within the vagina but the cervix does not reach the introitus
![]() second degree – descent of the cervix to the level of the introitus
second degree – descent of the cervix to the level of the introitus
![]() third degree – the cervix and uterus protrude out of the vagina.
third degree – the cervix and uterus protrude out of the vagina.
Procidentia is a term used when the cervix, uterus and vaginal wall have completely prolapsed through the introitus. Exposure of the cervix and vagina outside the introitus may lead to ulceration of the cervix and thickening of the vaginal mucosa.
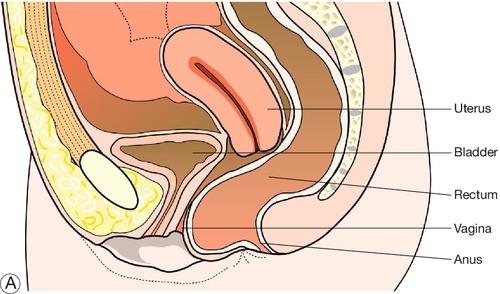
Rectocele
Weakening of the tissue that lies between the vagina and rectum (rectovaginal fascia) allows the rectum to protrude into the lower posterior vaginal wall, causing a rectocele (Fig. 16.3). Laxity of the perineum may also be present, which gives a gaping appearance to the fourchette (the posterior margin of the introitus).
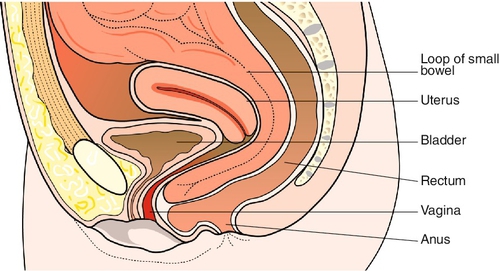
Enterocele
An enterocele is the only type of vaginal prolapse which is truly a hernia (Fig. 16.4). It has a sac, neck and contents. The sac is a protrusion of the peritoneum of the POD and may contain small bowel or omentum.
Symptoms
Prolapse may be asymptomatic and it may only be detected when women attend for a cervical smear test. The prolapse of one or more organs tends to cause the patient to feel that there is ‘something coming down’, and this is usually accompanied by discomfort and a dragging sensation. Furthermore, the organ prolapsing may malfunction giving further symptoms which require management (Table 16.1).
Although backache that characteristically improves when lying down, can be caused by prolapse (most typically uterus, vault or enterocele), pain is not. Women who are in a lot of pain may have a prolapse but it is not the cause of their symptoms. Coital difficulties are an uncommon presenting symptom.
Anterior wall prolapse may cause urinary symptoms because it involves bladder and urethra. While over 50% of women with SUI will have a prolapse, this will only occur if the bladder neck and continence mechanism prolapse. If not, the bladder descends and the patient has difficulty emptying the bladder, and retained urine then predisposes to recurrent urinary tract infections. Such patients may have urinary frequency secondary to a reduced functional capacity of the bladder, but it should be noted that any urgency and urge incontinence is not caused by prolapse and is likely to indicate the coexistence of an overactive bladder.
Uterine prolapse does not usually present until the woman feels a ‘lump’. If there is a procidentia, then there may be bleeding or discharge from ulceration of the cervix or vaginal wall.
Bowel symptoms related to a rectocele involve a feeling of incomplete evacuation of the bowel contents. When straining occurs with defecation, the rectocele balloons forward and some women need to digitally reduce the rectocele to pass stool. Enteroceles usually present as a lump but may be also associated with nonspecific lower abdominal discomfort and backache.
Signs
Examination for prolapse forms part of the general gynaecological examination. Abdominal examination, although historically done to detect a pelvic mass which may be pushing the pelvic organs downwards, is in fact more likely to detect a palpable bladder, which if found after voiding is a sign of urinary retention.
Pelvic examination is then performed, initially with the patient supine. On inspection of the vulva, one may note atrophic changes (scanty hair, thinning of the labia). The woman is asked to abduct her legs and strain. By gently parting the labia majora with the thumb and index finger of the left hand, prolapse may be seen appearing at the introitus. Vaginal atrophy may be seen suggesting the need for oestrogen treatment. Urinary leakage should be looked for on coughing, and an assessment of the perineum is made. A bimanual examination may then be performed, and may give a useful indication of uterine descent.
Examination in the left lateral position can also be helpful. This allows a systematic examination of the entire vagina, exerting gentle traction with the speculum on the posterior vaginal wall. Sponge forceps are occasionally used during this examination to reduce a large prolapse or to enable the examiner to distinguish the anatomy. The speculum can then be slowly withdrawn along the posterior wall of the vagina and the full extent of any rectocele will come into view. If a prolapse is not apparent with the woman lying down, it may sometimes be necessary to examine her in the standing position.
Management
If a prolapse is not causing symptoms and the woman is unaware of it, then she does not require treatment. Simply because a doctor notices laxity within the vagina does not mean that surgery should be performed.
Conservative
Conservative treatment should be the first-line management of mild to moderate prolapse. Patients should be advised about weight reduction, smoking cessation and normalization of fluid intake. Conservative measures may also be used for temporary relief before surgery in significant prolapse.
Supervised pelvic floor physiotherapy has been proven to reduce mild to moderate prolapse. The key word here is supervised. Simply giving the patient a leaflet about pelvic floor exercises and telling her to go and do them, while unlikely to do any harm, is also unlikely to produce any benefit. Sending an enthusiastic patient to an enthusiastic physiotherapist however, can produce cure/improvement rates of 60–70%. Pelvic floor physiotherapy is not effective when prolapse is well established, but it still has a role in the treatment of associated urinary incontinence, as well as a prophylactic intervention, particularly postpartum and postoperatively.
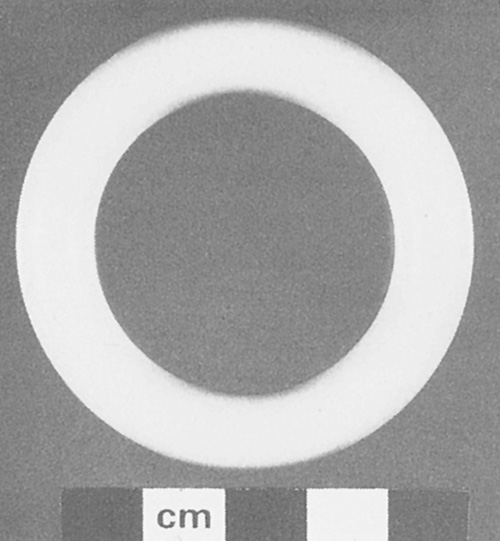
Pessaries are commonly used. A ring pessary is an inert plastic ring which is placed in the vagina so that one edge of the ring is behind the symphysis pubis and the other is in the posterior fornix (Figs 16.5 and 16.6). The ring stretches the vault of the vagina and thus supports the uterus. It may also help reduce cystocele but it will not reduce a rectocele. Once a ring is fitted, arrangements are usually made to change it every 4–6 months. At this examination, the vagina is inspected thoroughly for atrophic changes and ulceration due to pressure necrosis. Complications from the ring may include urinary symptoms (frequency, infection), vaginal discharge, bleeding or, very rarely, fistula formation (if the ring is neglected). Other types of pessary are available, particularly the ‘shelf’ pessary, which has a useful role in procidentia.
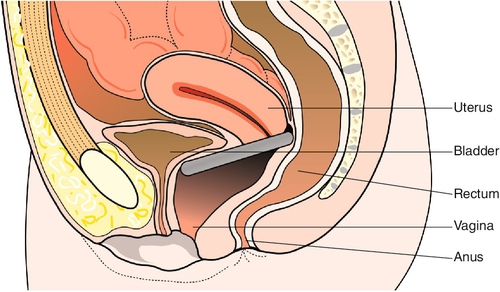
Fig. 16.6Ring pessary in situ.
Note that the anterior vaginal wall is elevated to reduce the cystocele and the uterine prolapse has been corrected.
If atrophy of the lower genital tract is noted in association with prolapse, a course of oestrogen therapy (commonly administered topically as a cream) may improve vaginal tissue thickness. This may improve some symptoms and it facilitates any planned vaginal surgery.
Surgery
Most procedures for the treatment of genital prolapse are performed through the vagina, with only a few requiring an abdominal approach. When considering a surgical technique, particular attention should be given to preserving the calibre of the vagina, if the woman wishes to remain sexually active. This aspect should always be discussed before surgery.
Anterior vaginal wall – anterior repair (anterior colporrhaphy)
Anterior vaginal wall prolapse may be associated with stress urinary incontinence which may need to be investigated prior to surgery. The principle of an anterior repair is to make a midline incision through the vaginal skin and to reflect the underlying bladder off the vaginal mucosa. Once this is achieved, lateral supporting sutures are placed into the fascia in order to elevate the bladder. Surgery should stop short of the bladder neck and urethra. If the patient has SUI she can have a suburethral tape inserted at the end of the repair. The remaining redundant vaginal skin that has been ‘ballooning’ down is excised, and the vaginal skin is then sutured closed.
Uterine descent – vaginal hysterectomy or Manchester repair
Vaginal hysterectomy is commonly performed for uterine prolapse. However, one must not presume that just because the uterus is prolapsing, it can be removed vaginally, as it may be too large to remove because of, for example, associated fibroids. One should also consider whether the uterus is being pushed down from a mass above (e.g. advanced ovarian cancer with gross ascites), or whether bowel is likely to be adherent to the uterus (e.g. after previous abdominopelvic surgery, endometriosis or severe infection). Once the uterus is removed, it is important that the supporting ligaments are approximated, so as to prevent further prolapse of the vaginal vault.
Manchester repair (also called ‘Fothergill repair’, see History box) has a role in treating a woman with significant cystocele and a degree of uterine prolapse, but is less commonly performed than vaginal hysterectomy. The uterosacral and transverse cervical (cardinal) ligaments are divided and shortened, the cervix is amputated, and the shortened ligaments are approximated anterior to the cervical stump. The anterior repair is performed and completed as above.
Posterior vaginal wall – posterior repair (posterior colpoperineorrhaphy)
The principles of a posterior repair are similar to those of an anterior repair. An incision is made in the vaginal wall and the rectum is separated from the vagina (Fig. 16.7). Supporting sutures are placed in the disrupted rectovaginal fascia to reduce the prolapse. The lax vaginal skin is then excised and the incision closed. This operation can be combined with a repair of the perineal body to support the perineum. Again, particular care must be taken not to narrow the vagina and create dyspareunia.
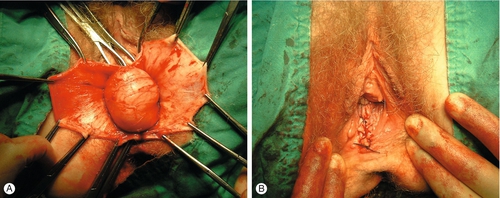
Fig. 16.7Posterior colporrhaphy.
(A) The posterior wall is opened in the midline to expose the rectum. (B) The posterior wall is closed after reducing the prolapse.
As the procedure reaches the apex of the rectocele, the surgeon must identify whether or not there is an enterocele present. If one is present, the peritoneum must be opened (avoiding bowel injury). The hernial sac must be transfixed and excised, and supporting lateral tissue approximated in order to prevent recurrence.
Total vault prolapse (after hysterectomy)
This condition refers to the complete eversion of the vagina following a hysterectomy (Fig. 16.8). It is effectively a procidentia without the uterus, not unlike a sock that has been turned inside out. Surgical options are sacrocolpopexy, sacrospinous fixation and vaginal mesh insertion.
Sacrocolpopexy
Sacrocolpopexy involves suturing the vaginal vault to the body of the sacrum, indirectly by using a polypropylene mesh interposed between the two structures. The procedure is performed through an abdominal incision but can be carried out laparoscopically.
Sacrospinous fixation
Sacrospinous fixation requires the surgeon to suture the top of the vaginal vault to the sacrospinous ligament. The procedure is performed through the vagina. Complications of the procedure include damage to the sciatic nerve and pudendal vessels.
Vaginal mesh repairs
Recurrence of prolapse after surgical correction is common, with up to 30% of women requiring a second operation within 5 years. The recurrence may be due to the fact that the repaired tissues were weak even before the original operation; consequently, there is increased interest in mesh-augmented pelvic floor repair. Meshes are used with the aim of improving tissue strength and support. Types of mesh used are synthetic biocompatible meshes (e.g. polypropylene) and biological meshes (e.g. porcine dermis or bovine pericardium), and these can also be either absorbable or non-absorbable.
Currently, mesh is most popularly provided as ‘mesh repair kits’. They use monofilament, low-weight, macroporous polypropylene meshes to reinforce the pubocervical and rectovaginal fascia. The operation involves the blind insertion of trocars into the obturator foramen, ischiorectal fossa, ileococcygeus muscle and sacrospinous ligament. Most meshes have three parts, which are placed between the bladder and vagina, through each obturator foramen and between the rectum and vagina (Fig. 16.9).
Meshes have been associated with an increased risk of complications, however, partly from the risks of insertion and partly because they are foreign bodies. Operative complications include bladder injuries, rectal injuries and vascular damage (cystoscopy is recommended to exclude bladder damage). Long-term complications include dyspareunia, erosion or rejection of the mesh and mesh-related infections. Infection after use of a vaginal polypropylene mesh has been reported in around 8% of cases, with erosions occurring in about 12%. Necrotizing fasciitis is also a possibility.
Although mesh repair kits are associated with low recurrence and low morbidity rates, some of the uncommon complications are serious and potentially life-threatening, and it is suggested that these repairs should be carried out only by specialists. One of the leading manufacturers of mesh repair kits has recently withdrawn their product following many expensive lawsuits in the USA and it remains to be seen whether this will dissuade surgeons from this type of repair.