The child in society
• likely cause: if the diarrhoea is likely to be from a viral illness or from a contaminated water supply if in a developing country
• severity of the child’s illness: the organism likely to be responsible and the child’s nutritional status
• management options: who will take care of the child when ill; is pre-prepared oral rehydration therapy available; is hospital treatment possible and what facilities can it offer?
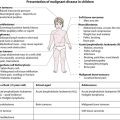
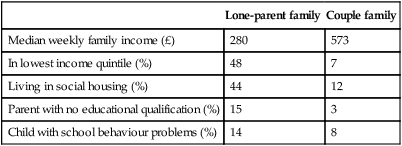
Important goals for a society are that its children and young people are healthy, safe, enjoy, achieve and make a positive contribution and achieve economic well-being (Every Child Matters, 2003 at: http://www.dcsf.gov.uk/everychildmatters). These are included in the UN Rights of the Child (see below). The way in which the environment impacts on a child achieving good health is exemplified by the contrast between the major child health problems in developed and developing countries. In developed countries these are a range of complex, often previously fatal, chronic disorders and behavioural, emotional or developmental problems. By contrast, in developing countries the predominant problems are infection and malnutrition (Box 1.1).
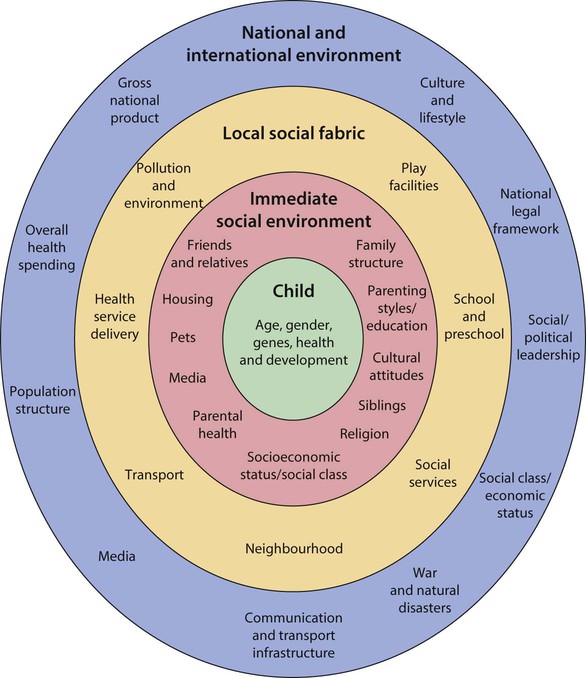
The child’s world
Children’s health is profoundly influenced by their social, cultural and physical environment. This can be considered in terms of the child, the family and immediate social environment, the local social fabric and the national and international environment (Fig. 1.1). Our ability to intervene as clinicians needs to be seen within this context of complex interrelating influences on health.
Immediate social environment
Family structure
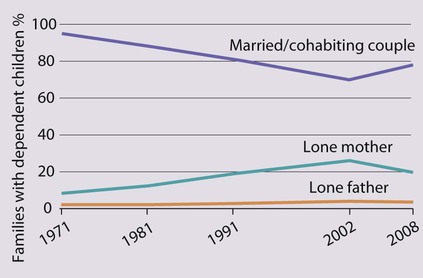
Although the ‘two biological parent family’ remains the norm, there are many variations in family structure. In the UK, the family structure has changed markedly over the last 30 years (Fig. 1.2).
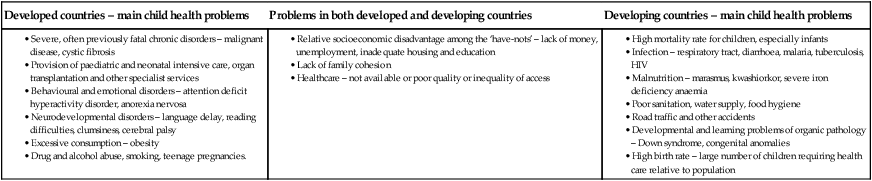
Single-parent households – One in four children now live in a single-parent household. Disadvantages of single parenthood include a higher level of unemployment, poor housing and financial hardship (Table 1.1). These social adversities may affect parenting resources, e.g. vigilance about safety, adequacy of nutrition, take-up of preventive services, such as immunisation and regular screening, and ability to cope with an acutely sick child at home.
Table 1.1
Comparison between parents who are single or couples
| Lone-parent family | Couple family | |
| Median weekly family income (£) | 280 | 573 |
| In lowest income quintile (%) | 48 | 7 |
| Living in social housing (%) | 44 | 12 |
| Parent with no educational qualification (%) | 15 | 3 |
| Child with school behaviour problems (%) | 14 | 8 |
General Household Survey, Office for National Statistics, England 2008.
Socioeconomic status
Socioeconomic status is a key determinant of health and well-being of children. It is estimated that 2.8 million children in the UK are living in poverty (below 60% of the national median income after adjustment for housing costs). The proportion of children in poverty in different countries is shown in Figure 1.3. Health issues in the UK in which prevalence rates are increased by poverty include:
National and international environment
Economic wealth
The lower the gross national income:
• the greater the proportion of the population who are children
• the higher the childhood mortality
• the higher the proportion of newborn infants with low birthweight
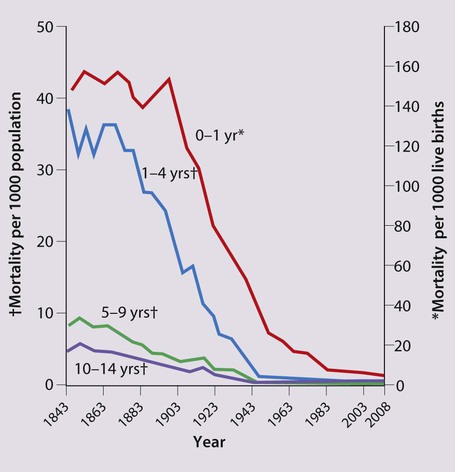
The dramatic reduction in childhood mortality in England over the last century is shown in Figure 1.4. It is primarily from improvements in living conditions such as improved sanitation and housing, and access to food and water. These have dramatically reduced fatalities from infectious disease. More recent contributions to this reduction have been increased availability and uptake of immunisation and major medical improvements in perinatal and infant care.
War and natural disasters
Children are especially vulnerable when there is war, civil unrest or natural disasters (Box 1.2). Not only are they at greater risk from infectious diseases and malnutrition but also they may lose their caregivers and other members of their families and are likely to have been exposed to highly traumatic events.
Children’s rights
Children’s rights are laid down in the United Nations Convention on the Rights of the Child, which has been ratified by all members of the United Nations, including the UK, but excepting the USA and Somalia (Box 1.3, Fig. 1.5). Unfortunately, the rights of many children are not met. Implications of the convention include the involvement of children in clinical decision-making and in issues of consent.
Global child health
Child mortality
Worldwide, each year, 8.8 million children under 5 years old die (Fig. 1.6). Infectious diseases, with undernutrition a major contributing factor, account for most deaths in children. Pneumonia and diarrhoea are the leading infectious causes of death. More than half of child deaths occurring after the neonatal period are due to just five preventable and treatable conditions: pneumonia, diarrhoea, malaria, measles and HIV.
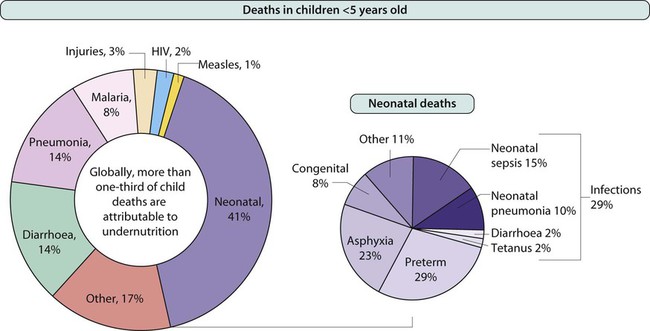
Where deaths occur
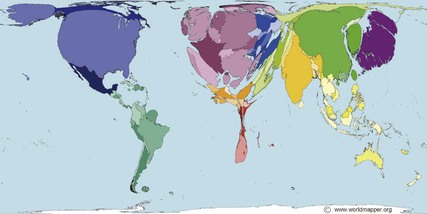
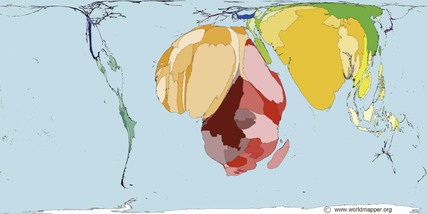
Although only about 48% of the world’s estimated 629 million under-5s live in sub-Saharan Africa and South Asia, 93% of child deaths occur in these two regions (Fig. 1.7). The difference in resources available is reflected in the difference in the number of healthcare professionals in different parts of the world. This is shown in diagrammatic form in Figure 1.8. Whereas the USA spends over $6000/person/year on health, the annual expenditure is only $25/person in the 49 lowest income countries. Put another way, the annual health budget available to the 1.2 billion people living in these countries is equivalent to that for the 6.5 million living in Arizona!
Reducing child mortality
The international community has taken many steps to improve child health in poor countries. Some are listed in Box 1.4.
The launch of the Integrated Management of Childhood Illness (IMCI) in 1992 was a major advance (Fig. 1.10). It recognised that an integrated management approach to childhood illness is required, including nutrition and preventative care in families and communities. In health facilities, sick children are triaged according to the presence of specific danger signs and management is planned according to algorithms which can be followed by non-medical staff.
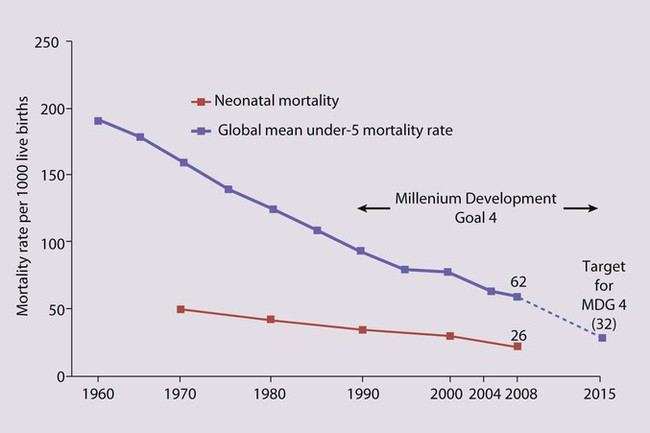
The major advance in global child health has been in the adoption of the Millennium Development Goals (MDGs), which has served as a major focus for the international community’s commitment to reduce child mortality (Fig. 1.11). There are specific targets for each goal. For MDG 4 it is to reduce child mortality in children <5 years by two-thirds, between the years 2000 and 2015. Contributions are also made by MDGs to improve maternal health and reduce mortality from malaria by insecticide-treated bednets and appropriate anti-malarial drugs and from HIV and TB.

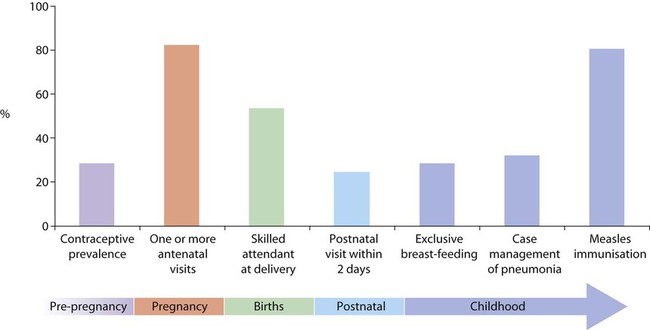
Some of the specific health measures targeted in maternal and child health are shown in Figure 1.12, together with the overall success in implementing them.
• One or more antenatal visits
• Skilled attendant at delivery
• Postnatal visit within 2 days
Progress in reducing under-5-year-old mortality is being made (Fig. 1.13), although in many of the poorest countries it is slow and patchy, and considerable effort will be required to meet the MDG 4 target.