26
Termination of pregnancy
Introduction
Termination of pregnancy, or therapeutic abortion, has been carried out for thousands of years. The provision of abortion in a legal, medically supervised and safe framework, is one of the most contentious issues in modern-day medicine. Many people have strongly held and often divergent opinions about abortion. Those who are pro-abortion maintain that they are ‘pro-choice’ and support the right of individuals to make their own decisions. They are sensitive to the difficulties of bringing an unwanted baby into the world, and are aware of the impact on both the woman concerned and society more broadly. Those who are anti-abortion, or ‘pro-life’, argue that the fetus is more than just part of the mother; it is a life in itself and should be protected, even if that means limiting the mother’s choices regarding her body.
There are many factors leading to unplanned pregnancy: contraception may have failed, or perhaps was not used at all; occasionally, intercourse without the woman’s consent has resulted in pregnancy. Of course, a woman may have an unplanned pregnancy but be pleased to be pregnant and continue the pregnancy. Another may have planned to be pregnant but then her circumstances may change and she feels unable to continue. Among women attending antenatal clinics, research demonstrates that only two-thirds of women had an intended pregnancy, with the rest either ambivalent or having an unplanned pregnancy. Although abortion should not be considered as a method of contraception, contraceptive failures do occur, and access to abortion allows women complete fertility regulation.
Abortion care forms a large part of the gynaecology workload in the UK, and therapeutic abortion is one of the commonest gynaecological procedures. Although doctors may have differing degrees of involvement in abortion services, most will come into contact with women who are seeking abortion at some point in their career, so need to be familiar with the legal framework and options open to the women.
Worldwide perspectives
There are over 100 million acts of sexual intercourse every day across the world, resulting in over 900 000 pregnancies. It is estimated that about 50% of these pregnancies are unplanned, and about 25% actually unwanted. Many women with an unwanted pregnancy will seek an abortion, and, as a result, about 150 000 pregnancies are terminated by induced abortion every day. There are over 50 million abortions worldwide every year and around one-third of these abortions are carried out in unsafe conditions. Illegal abortions are often performed in unclean conditions by unqualified people, causing considerable morbidity and mortality. Between 100 000 and 200 000 women die each year from unsafe abortion. In contrast, abortion performed in appropriate conditions with trained staff is a very safe procedure, with extremely low morbidity and mortality.
UK perspectives
The Abortion Act was passed in 1967, and after this, there was a rapid rise in the number of abortions carried out in England, Wales and Scotland. Currently, almost 190 000 abortions are carried out each year in England and Wales, with a further 12 500 in Scotland. Women of all reproductive ages have abortions, although the highest rate is among women aged 18–24 years. About 80% of women having abortions are unmarried, although many of these will have a regular partner. Just over half of women have already had a child and over one-third have had an abortion previously. Most terminations (78%) are carried out before 10 weeks of pregnancy, 13% are carried out between 10–12 weeks, and the remaining 9% are carried out at 13 weeks or more.
Legal and ethical aspects
Abortion is not available ‘on demand’ in the UK, and can only be carried out if certain criteria are met. The 1967 Abortion Act, as amended in 1991, states that abortion can be performed if two doctors agree that the pregnancy should be terminated on one or more grounds (Box 26.1).
Most abortions (98%) are carried out under Clause C of the Abortion Act, where two doctors agree that continuing the pregnancy would carry greater risk to the physical or mental health of the woman than abortion. A smaller number of abortions (1%) are carried out to protect the health of existing children. Clauses C and D carry an upper gestational limit of 24 weeks. The 1967 Abortion Act does not apply to Northern Ireland, where abortion is only legal under exceptional circumstances, e.g. to save the life of the mother.
Current methods of inducing abortion are now so safe that it is safer for the woman to have an early abortion than to continue to term and have a delivery. Of course, that does not mean that abortion should be recommended, but a clinician may consider a request for abortion when a woman feels that her health (or that of her children) will be adversely affected by continuing the pregnancy.
Although uncommonly used, the Abortion Act also allows abortion to be performed in an emergency situation upon the single signature of the doctor performing the abortion. Such an emergency abortion can be carried out either to save the life of the pregnant woman, or to prevent grave permanent injury to the physical or mental health of the pregnant woman.
Recent opinion polls have shown that most of the public support the right to abortion, with 65% agreeing that if a woman wants an abortion she should not have to continue with her pregnancy. Women requesting abortion need the agreement of two doctors, and will often rely on the support of their general practitioner for referral. Over 80% of British general practitioners described themselves as ‘broadly pro-choice’, and 18% as ‘broadly anti-abortion’. No doctor has to be involved in referring women for abortion, but the General Medical Council guidance advises that if a doctor is unable to make a referral for termination, then a timely referral of the woman to a colleague who does not hold similar views is obligatory; every doctor has an obligation to treat in an emergency situation.
Counselling before abortion
When a woman is considering abortion, it is important that she is able to weigh up the practical and emotional aspects of her decision, to ensure that the best choice is made in the circumstances. The Royal College of Obstetricians and Gynaecologists’ (RCOG) guidance recommends that the initial consultation appointment should be available within 5 days of referral, to avoid any unnecessary delays. She will require sympathetic but non-directional support so that she is able to explore her own feelings and to make her own informed decision. Many women with an unplanned pregnancy will make their decision within a few days of knowing that they are pregnant. Other women may remain undecided for some time. It is important that the decision to abort is made freely by the woman, and that she is not coerced by another party, for example a parent or partner. For this reason, it is imperative to speak to the woman alone at some point during the consultation.
Psychological problems and rates of depression are not increased after abortion when compared with background population risk, but some women may experience coping problems and distress. The counselling process can help to identify these women, and ensure that appropriate support is offered both before and after the abortion. Box 26.2 outlines risk factors for emotional problems.
Women who blame themselves for the pregnancy and subsequent abortion can struggle to come to terms with their decision. It can help to identify what went wrong that led to the pregnancy. Jointly agreeing a contraceptive plan with the woman can return a sense of control to her, and give her something positive for the future to take from the experience.
We are used to taking a structured gynaecological and sexual history, collecting factual information, such as date of last menstrual period, but we can help the woman to express her emotional needs by using some basic counselling techniques:
![]() Ask open-ended questions, e.g. ‘How did you feel about the pregnancy?’, rather than ‘Were you upset when you found out?’
Ask open-ended questions, e.g. ‘How did you feel about the pregnancy?’, rather than ‘Were you upset when you found out?’
![]() Actively listen to the patient, e.g. show interest in her views, and show understanding
Actively listen to the patient, e.g. show interest in her views, and show understanding
![]() Reassure her that her feelings are normal, e.g. saying ‘I understand that you are finding this difficult to talk about’
Reassure her that her feelings are normal, e.g. saying ‘I understand that you are finding this difficult to talk about’
![]() Encourage questions, e.g. say ‘What would you like to ask me about your choices?’, rather than ‘Any questions?’
Encourage questions, e.g. say ‘What would you like to ask me about your choices?’, rather than ‘Any questions?’
Some women need practical information to make their choice, such as details about maternity leave, housing rights, etc. or information about adoption. Timely referral to a social worker should be available.
Pre-abortion investigations
Once the woman has decided to proceed to abortion, there are a number of investigations which are usually performed, to ensure that the abortion is as safe as possible:
![]() Blood tests: haemoglobin is measured, and a sample is sent for ABO and rhesus blood grouping. Women who are rhesus negative will require anti-D immunoglobulin after the abortion (250 IU if < 20 weeks and 500 IU if > 20 weeks). HIV, haemoglobinopathy and other tests can be performed if indicated
Blood tests: haemoglobin is measured, and a sample is sent for ABO and rhesus blood grouping. Women who are rhesus negative will require anti-D immunoglobulin after the abortion (250 IU if < 20 weeks and 500 IU if > 20 weeks). HIV, haemoglobinopathy and other tests can be performed if indicated
![]() Estimation of gestation: this can be performed by either clinical examination or ultrasound. Most abortion clinics in the UK use ultrasound to confirm gestation before abortion. Ultrasound is essential if there is a possibility of ectopic pregnancy, or where gestation is unclear. Some women will not make the decision until they know the gestation of the pregnancy, i.e. they may decide to abort an early pregnancy, but would not wish to undergo a later abortion. Occasionally, women may request a copy of the scan, as a memento of the pregnancy. Ultrasound will sometimes show a non-viable pregnancy, which will then relieve the woman of a decision around abortion
Estimation of gestation: this can be performed by either clinical examination or ultrasound. Most abortion clinics in the UK use ultrasound to confirm gestation before abortion. Ultrasound is essential if there is a possibility of ectopic pregnancy, or where gestation is unclear. Some women will not make the decision until they know the gestation of the pregnancy, i.e. they may decide to abort an early pregnancy, but would not wish to undergo a later abortion. Occasionally, women may request a copy of the scan, as a memento of the pregnancy. Ultrasound will sometimes show a non-viable pregnancy, which will then relieve the woman of a decision around abortion
![]() Prevention of infection: infection can occur in about 10% of women after abortion, but is reduced with the use of antibiotics. RCOG guidance advises that all women undergoing abortion should be screened for Chlamydia trachomatis and receive prophylactic antibiotics on the day of abortion. Screening gives the opportunity to carry out partner notification (contact tracing) when there is a positive test, thus preventing reinfection of the woman and onward transmission. Some clinics treat everyone having an abortion with prophylactic antibiotics (commonly metronidazole and azithromycin), whereas others screen women for sexually transmitted infections, including chlamydia, and treat positive women and their partners
Prevention of infection: infection can occur in about 10% of women after abortion, but is reduced with the use of antibiotics. RCOG guidance advises that all women undergoing abortion should be screened for Chlamydia trachomatis and receive prophylactic antibiotics on the day of abortion. Screening gives the opportunity to carry out partner notification (contact tracing) when there is a positive test, thus preventing reinfection of the woman and onward transmission. Some clinics treat everyone having an abortion with prophylactic antibiotics (commonly metronidazole and azithromycin), whereas others screen women for sexually transmitted infections, including chlamydia, and treat positive women and their partners
![]() Cervical cytology: if a woman is due cervical cytology within the national screening programme, then this can be offered at the time of the clinic visit
Cervical cytology: if a woman is due cervical cytology within the national screening programme, then this can be offered at the time of the clinic visit
![]() Provision of information: information given verbally should be supported with written information for the woman to take away. This should include information about the types of abortion available, the risks and complications of abortion, who to contact if there are any problems after the procedure, and should be available in different languages.
Provision of information: information given verbally should be supported with written information for the woman to take away. This should include information about the types of abortion available, the risks and complications of abortion, who to contact if there are any problems after the procedure, and should be available in different languages.
Methods of abortion
Historically, a wide range of surgical and medical techniques have been used to cause therapeutic abortion. In the past two decades, advances in abortion techniques mean that safe and effective methods are now available at all stages of gestation. Medical methods have been increasing in frequency since the licensing of mifepristone in 1991. Both medical and surgical abortion can be offered up to 24 weeks, but availability varies in different geographical areas. The most appropriate method depends on gestation, medical history and the woman’s preference (Box 26.3).
Medical abortion
Mifepristone is a synthetic steroid which blocks the biological action of progesterone by binding to its receptor in the uterus and other organs. It is given orally under supervision of a doctor or nurse, in a premises licensed to carry out abortion. The woman is then allowed home. She returns to the unit 24–48 h later (usually 48 h) for administration of a prostaglandin, which can be given vaginally, buccally or sublingually. Bleeding usually starts within a few hours, followed by uterine contractions which expel the fetus and placenta. Most women experience period-like pains but there is much variation, with some women needing no pain relief while others (about 10–20%) requiring opiates. Bleeding usually continues for about 10 days after medical abortion.
Early medical abortion (up to 9 weeks’ gestation)
When a woman is less than 7 weeks’ pregnant, medical abortion is the most effective type of termination, with a lower failure rate than early surgical abortion. It is also a good choice between 7 and 9 weeks’ (63 days’) gestation.
The usual regimen is:
Mifepristone 200 mg orally, followed by misoprostol 800 μg vaginally 24–48 h later. Women can remain in the abortion unit until the abortion is complete, or can go home to complete the abortion.
Medical abortion in the late first trimester (9–12 weeks)
In the past, surgical termination alone has been offered to women in the late first trimester. However, it is now recognized that medical abortion is an effective alternative to surgical termination in the late first trimester.
The usual regimen is:
Mifepristone 200 mg orally, followed by misoprostol 800 μg vaginally 36–48 h later. Up to a further four doses of misoprostol 400 μg, either vaginally or orally, can be given until abortion occurs.
Medical abortion in the second trimester (13–24 weeks)
Traditionally, mid-trimester medical abortion was carried out using prostaglandin alone, or in combination with an oxytocin infusion. Not uncommonly, it would take several days for the abortion to be completed. Giving mifepristone prior to prostaglandin has been shown to reduce the length of time taken for the abortion to occur.
The usual regimen is:
Mifepristone 200 mg orally, followed by misoprostol 800 μg vaginally 36–48 h later. Up to a further four doses of misoprostol 400 μg orally, can be given until abortion occurs.
Surgical abortion
Surgical abortion below 7 weeks’ gestation
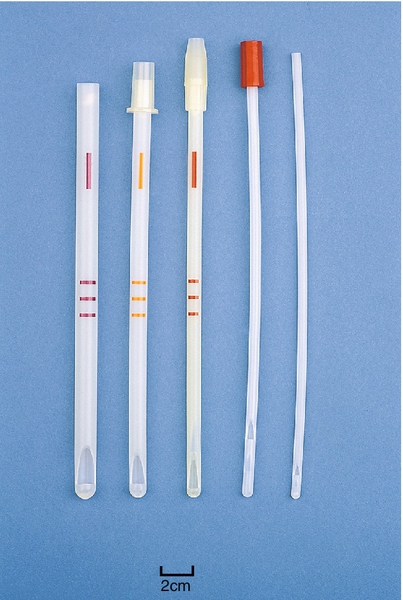
Surgical abortion below 7 weeks’ gestation has a higher failure rate than later surgical procedures and medical abortion at this gestation. However, abortion by manual vacuum aspiration can be performed at this early gestation, with appropriate measures to ensure the abortion is complete. A narrow suction curette of 4 or 5 mm diameter is inserted into the uterus under local paracervical block. The early pregnancy is aspirated using a 50 mL syringe. It is very important to ensure that the abortion is complete, either by identifying the products of conception or by hCG follow-up.
Surgical abortion at 7–14 weeks
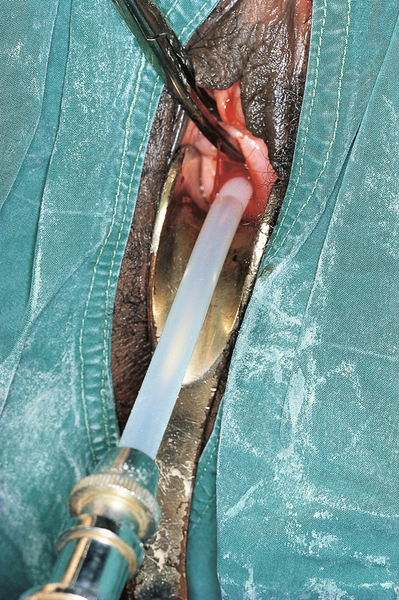
Surgical abortion at this gestation is performed by suction or vacuum aspiration, using a flexible suction curette, and a mechanical or electrical pump. The suction curette is inserted into the uterine cavity, after cervical dilatation, and the contents aspirated (Figs 26.1 and 26.2). The procedure can be carried out under general anaesthesia, local anaesthesia or conscious sedation depending on patient choice.
Cervical treatment with prostaglandin before surgical abortion reduces the risk of cervical trauma and uterine perforation, and is recommended for all cases.
The recommended regimen is:
Misoprostol 400 μg vaginally or sublingually 2–3 h prior to surgery.
Late surgical abortion (14–24 weeks)
Cervical preparation followed by dilatation and evacuation (D&E) can be offered in the second trimester. It is the method of choice in the USA, but in the UK, is offered by a limited number of doctors experienced in the technique. It may be necessary to dilate the cervix up to a diameter of 20 mm before the fetal parts can be extracted using special instruments. D&E has the advantage that the woman is unaware of the procedure. There is evidence from the USA that women prefer D&E to medical methods, although many nurses and doctors find the procedure disturbing.
Complications of abortion
Women should be advised that the risk of complications is low. Indeed, a termination is safer than continuing the pregnancy to term. Complications do occasionally occur, however and women should be given information about where to seek help if there are problems.
Retained products of conception
This is the commonest complication following abortion, although it occurs in less than 5% of women. It is more common after medical abortion, and when surgical abortion is carried out at either very early or late gestations. Some women with retained products will require (further) surgical evacuation of the uterus, particularly if there is heavy or prolonged bleeding. Many women will pass the retained tissue spontaneously. Antibiotics can be given to reduce the risk of secondary infection until the tissue is passed.
Failure of abortion
Ongoing pregnancy after an abortion procedure is unusual, occurring in less than 1% of cases. Women should be advised of the importance of returning for follow-up, if there was any doubt over completeness at the time of termination, or there are continuing symptoms of pregnancy.
Post-abortion infection
Pelvic infection can occur in up to 10% of women after termination, but this can be at least halved with pre-abortion STI screening and use of antibiotics at the time of termination. Women should be advised about signs of infection such as pyrexia, pelvic pain and offensive vaginal discharge, and should return if concerned.
Haemorrhage
Significant haemorrhage of over 500 mL at the time of termination occurs in less than 1 in 1000 early abortion cases, rising to 4 in 1000 when over 20 weeks.
Trauma to the genital tract
Perforation of the uterus happens in about 1 in 1000 surgical cases, and is more common with later-gestation abortions and with less experienced surgeons. Cervical trauma is also uncommon (< 1 in 100) and is reduced by cervical preparation with prostaglandin. Uterine rupture has been described very occasionally with mid-trimester medical abortion.
Future fertility
Women often ask about the chance of an abortion affecting their future fertility. There is no established positive association between previous termination of pregnancy and future infertility, ectopic pregnancy or placenta praevia. There may be a slight increase in risk of subsequent miscarriage and pre-term delivery with later abortion, although the evidence is unclear.
Psychological sequelae
There is no evidence of lasting psychological harm to women undergoing abortion and indeed there is no difference in psychological sequelae if women abort or continue the pregnancy. Some women may be at higher risk of distress after the abortion, and can be identified at the time of pre-abortion consultation and offered greater support.
Abortion aftercare
Women should be provided with appropriate information of symptoms and signs of complications, and should be given a contact telephone number if she has concerns. There is no need for routine follow-up when the completion of the abortion was confirmed at the time.
Post-abortion contraception
Over one-third of terminations are carried out on women who have had a termination in the past, and ensuring that there is adequate contraception available can reduce the chance of a further abortion. All methods of hormonal contraception (combined pill, progestogen pill, implant, injection, patch, ring) can be started on the day of surgical abortion, or on the prostaglandin treatment day of medical abortion, with immediate contraceptive cover. Intrauterine contraception can be fitted immediately following termination. This can be done at the end of the surgical procedure, or following expulsion of the pregnancy with medical termination. Condoms can be used immediately after termination. Women are usually advised not to use a diaphragm within 6 weeks of mid-trimester abortion, in case refitting is required. Sterilisation can be carried out at the time of abortion although there is a higher failure rate and later regret. For this reason, some gynaecologists will recommend interval sterilization.
Conclusion
Over 200 000 women undergo therapeutic abortion each year in the UK. Women need to be well informed about pregnancy and abortion options, and supported to make an informed choice. A choice between medical and surgical abortion should be offered. A range of contraceptive options should be made available to women at the time of termination.