Chapter 52 Teaching Airway Management Outside the Operating Room
I Background
Management of the airway is the most important and potentially the most life-saving (or life-threatening) task that an anesthesiologist, emergency department (ED) physician, or intensivist performs. Missteps in airway management can result in mortality or significant morbidity. In 1985, the American Society of Anesthesiologists (ASA) Committee on Professional Liability began to analyze closed-claim malpractice cases to objectively assess adverse outcomes from anesthesia. The initial analysis of the data, published in 1990, revealed that respiratory events accounted for 34% of the claims (522/1541 cases) and that 85% of the respiratory events resulted in permanent neurologic injury or death.1 Three mechanisms of adverse outcome from respiratory events accounted for 73% of the events: inadequate ventilation (38%), esophageal intubation (18%), and difficult endotracheal intubation (DI; 17%).
The reviewers concluded that 90% of the cases of inadequate ventilation and esophageal intubation could have been prevented if monitoring with capnography and pulse oximetry had been employed. It was also concluded that only 36% of the cases of DI were easily preventable. In response to this finding, the Task Force on Management of the Difficult Airway (DA) was formed by the ASA. After an exhaustive search and evaluation of the medical literature concerning airway management published between 1973 and 1991, the task force published Practice Guidelines for Management of the Difficult Airway in March, 1993.2 These guidelines included recommendations for evaluation of the airway, basic preparation for DA management, strategy for intubation of the DA, and postoperative care. The Task Force also developed an algorithm for management of the DA. Updated guidelines, based on information accrued since 1993, were published in 2003.3 It can be anticipated that future updates based on experience with new airway devices will occur.4 Other organizations with interest in airway management have also published airway management guidelines.5
A Is There Evidence That the Difficult Airway Guidelines Have Been Effective in Reducing Adverse Airway Events?
A review of the closed claims database in 1999 revealed a decline in claims for adverse respiratory events, primarily related to a reduction in claims for inadequate ventilation and esophageal intubation.6 Claims for adverse events secondary to DI remained relatively constant, and claims for trauma to the upper airway increased. The claims for pharyngeal and esophageal trauma were frequently associated with DI. Another study, published in 2005, compared claims for DA management during two time periods: 1985–1992 (before DA guidelines) and 1993–1999 (after DA guidelines). Claims for adverse respiratory outcomes (death or brain death) during induction of anesthesia decreased by 67% during the latter period compared with the former. However, claims for similar adverse respiratory outcomes occurring during the maintenance phase of anesthesia, at extubation, or during recovery did not change.7
Although respiratory events are more likely to result in an adverse outcome, the incidence of patients with a DA in clinical anesthesia practice is actually quite low. The incidence of failure to intubate the trachea in a large series of surgical patients was only 0.3%.8 Although the most comprehensive published data have concerned perioperative airway management, airway management in the prehospital setting, in the ED, and in the intensive care unit (ICU) is no less important and must be included in any airway education program.9 Airway management is not an easy skill to learn, and educators must give careful consideration to the complexity of airway management and the ability of different types of health care providers to manage ventilation and endotracheal intubation.
Objectives for education in airway management include the theoretical and practical aspects of airway devices and techniques and a time-based environment that mimics actual clinical situations. The student must also gain an appreciation of the relationship between the practitioner and the patient and the effects that clinical decisions may have on outcome.10 The teaching program must allow the learner in a nonclinical environment to make choices that may result in an adverse outcome.
II Miller’s Learning Pyramid
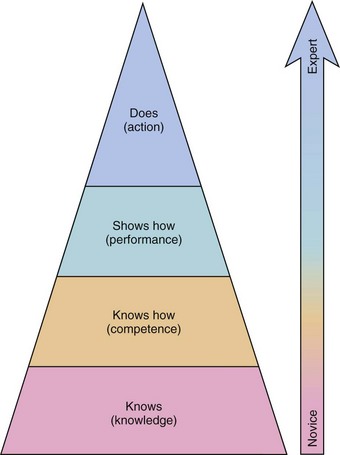
An airway teaching program must teach simple maneuvers (e.g., performing a jaw thrust) as well as complex skills such as awake fiberoptic intubation (FOI). The design of a successful education program begins with the development of clear objectives. What has to be taught, to whom, and how? The program must also address different knowledge and skill levels. Miller’s learning pyramid for assessment of clinical skills has four stages of ability: Knows, Knows How, Shows How, and Does (Fig. 52-1).11
Because skills and scientific information gained during simulator training may not be easy to transfer directly to clinical practice, the clinical environment is the best environment for developing airway management skills.12 Practicing techniques such as airway assessment, bag-mask ventilation (BMV), supralaryngeal airway (SLA) insertion, direct laryngoscopy, and FOI in actual patients would be ideal. The highest competence level (Does) in airway management ultimately requires practice in the clinical environment. There are, however, a number of barriers to training exclusively in the clinical arena (Box 52-1). Training outside the operating room (OR) or ICU is done to minimize the risk to patients and promote efficient clinical learning.
Box 52-1 Barriers to Teaching Difficult Airway Management in the Clinical Environment
III Computer-Based Learning
The pace of development of interactive computer-assisted instructional programs has surpassed simulation development over the past 10 years. Computer-assisted instruction can facilitate the organization and linkage of information directly applicable to clinical situations.13 A major advantage of computer-based instruction is the low cost after development and the lack of need for a human instructor. The learner can use the program at his or her own pace and as many times as necessary to achieve mastery of the subject. The increased power of laptop computers has reduced the need for computer centers and provides the learner with exceptional mobility. Computer-assisted instruction can also provide alternative learning methods for students who do not learn well with traditional teaching methods.
A clinical department can develop its own instructional programs or access existing programs via the Internet. The number of Web sites relevant to anesthesia continues to grow, and the Internet provides rapid access for users in remote locations.14 However, Internet programs are not peer-reviewed, and quality can be variable.15 The transition from Web 1.0 to Web 2.0 has encouraged more interactivity and improved the quality of Web-based education.16 The disadvantages of Web-based education, such as insufficient feedback and instructional ambiguity, can be overcome by providing local faculty input to supplement the Web-based program.
There are several objectives of an interactive airway management program (Box 52-2). One is to familiarize the learner with the anatomy and physiology of the upper airway. The complexity of the upper airway is often overlooked, and understanding of upper airway function can provide an early warning of impending respiratory difficulty. The structure and function of various airway devices can be displayed with diagrams, photographs, and videotapes. Computer-based multimedia programs can demonstrate device function and technique with a much more effective presentation than a traditional lecture format.
Box 52-2 Instructional Components of an Airway Management Educational Program
IV Efficacy of Simulation in Education
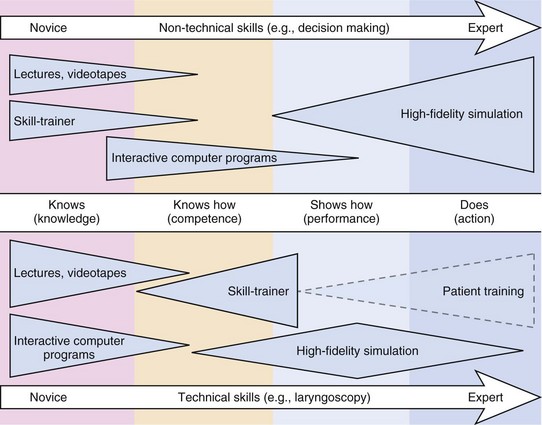
Simulation has been used for decades to address training problems in high-risk disciplines such as military science and aviation. Medical simulation began in the mid-1990s and has grown rapidly.17 Simulator training programs incorporate psychomotor and decision-making skills that address the highest level of competence in Miller’s pyramid: Does. When the programs are appropriately designed, simulation can close the gap between acquisition of skills and meaningful use of the acquired skills (Fig. 52-2). This may be especially true for rare situations. Because the incidence of the DA is low in clinical practice, two questions must be addressed: How can an anesthesiologist in clinical practice learn new airway skills? and How can the ramifications of critical decision points in airway management be learned?
The inherent nature of airway management includes uncertainty, complexity, time pressure, and high costs for failure. Simulation provides the ideal method for closely replicating the clinical situation and may help to scientifically evaluate strategies, decision points, and algorithm adherence.18,19 The efficacy of education with medical simulation is well established, but its effect on reducing the incidence of adverse patient outcomes is more controversial.18,20–24 It is easy to prove the effect of a theoretical lecture or workshop with a pretest and post-test. It is not easy to prove the effect of simulation on patient outcome in rare but life-threatening situations such as the DA. Nevertheless, there is evidence in the literature that simulator- and scenario-based training improves patient care.
V Types of Simulators
Simulators can be classified as low-fidelity (static) or high-fidelity (dynamic).
A Low-Fidelity Simulators
Mannequins do not always accurately replicate human anatomy and cannot be altered to represent abnormal anatomy. Such low-fidelity simulators provide neither physiologic data nor clinical feedback for the learner. Despite these shortcomings, however, effective skill transference to clinical use may be facilitated.25
B High-Fidelity Simulators
High-fidelity simulators, more commonly referred to as human patient simulators, offer many advantages over low-fidelity simulators. Physiologic parameters such as blood pressure, heart rate, pulse oximetry, capnography, breath sounds, peripheral pulses, and temperature can be programmed into the simulator. High-fidelity simulators cannot accommodate the variations in human anatomy.26 This is especially true for DI scenarios in which insertion of an SLA may be clinically effective. The reason is that the DI scenario in the simulator is created by supraglottic obstruction rather than laryngeal displacement.
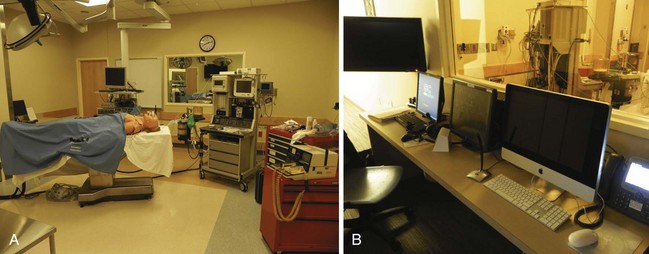
Many medical institutions and health care consortiums have invested in multipurpose simulation centers to provide training for different types of health care providers. These centers replicate ORs, ICU beds, ward beds, examination rooms, and ambulance bays to provide a realistic setting for trainees (Fig. 52-3). Simulation centers can employ full-time technicians to manage the technical aspects of simulation. This allows the teaching faculty to concentrate their efforts on curriculum development and the direction of simulation sessions.
Trainees from many disciplines need experience with simulation education. Licensure and board accreditation examination systems are rapidly incorporating an evaluation of performance with high-fidelity simulation.27–29
VI Airway Management Skills
There are several skills that the experienced airway provider must acquire in order to provide comprehensive airway management. Airway management skills are not easy to learn, the time to apply those skills to the apneic patient is short, and the risks of failure include death or permanent neurologic injury.30 Traditional educational programs depend on the accumulation of clinical experience, which may take years. Structured simulation-based teaching should provide a broader experience in a shorter period of time, thereby improving the airway management skills of a greater number of providers.
C Supralaryngeal Airways
Information that the learner should acquire during the initial phase of the training program includes the structural function of the device and correct insertion and positioning. Common to all SLA devices is their insertion over the tongue, into the hypopharynx, and above the glottic inlet. Although the type of SLA employed varies from institution to institution, it is beneficial to provide training with different SLA devices. There are several mannequins available for SLA insertion training, but performance varies, and the instructor must select one that is suitable for the particular device used.31
The depth and intensity of SLA training depends on the level of performance that is desired, and the goals for each type of medical provider must be clearly delineated. Anesthesiologists, who require the highest level of performance, must invest considerable time in mastering the use of the LMA. There are two learning curves: an initial learning phase consisting of 50 to 75 insertions, and a slower learning phase encompassing hundreds of insertions.32–34
D Conventional Direct Laryngoscopy
Conventional direct laryngoscopy has been a mainstay for airway management for decades and is considered by many to be the gold standard for emergency airway management. Skill development for direct laryngoscopy is difficult and requires more experience than previously thought.35 Numerous studies have demonstrated that alternative airway techniques, such as placement of an SLA, actually result in more rapid and effective ventilation than endotracheal intubation with conventional direct laryngoscopy. Such observations have caused many airway educators to change how they teach emergency airway management.36
A training course for providers who have little or no experience with conventional direct laryngoscopy should begin with lecture material that includes upper airway anatomy and physiology, the mechanics of direct laryngoscopy, and sequential instruction on the intubation process. Models have been developed that can be adjusted to reflect anatomic variants so that the student can see the effects of these variants on intubation technique.37 Mannequin practice with a VL has been shown to improve the success rate for intubation of patients.38 A clinical instructor should expect all novices to have extensive simulated experience before patient exposure. Selection of appropriate patients (such as lean, edentulous patients followed by patients with normal dentition) enhances the experience while reducing the likelihood of patient injury. Endotracheal intubation of patients who are likely to have rapid arterial oxygen desaturation, such as obese patients or children, should be done only after the learner has accumulated significant experience.
E Video Laryngoscopy
Advances in imaging technology have spawned a new class of intubation devices, the VLs.39 VLs continue to be refined and may in the future become the instrument of choice for all endotracheal intubations. The Bullard laryngoscope was introduced many years ago and was perhaps the first VL to have significant clinical application. The refinement of other imaging techniques has generated an increase in the number of different VLs now available. The basic components of all VLs are a rigid, anatomic blade and an imaging device that provides a view of the larynx without requiring line of sight. The important advantage of such a design is that it permits a reduction in the force that must be exerted by the laryngoscope blade on the patient’s upper airway in order to see the glottic inlet.
Even experienced laryngoscopists do not appreciate the differences in technique when they first use a VL. Comparative studies of various laryngoscopes provide information about performance in different scenarios, and students should be exposed to several VLs so they can determine which one is best for them.40,41 Once the technique of video laryngoscopy has been mastered, many prefer it to conventional direct laryngoscopy for even routine endotracheal intubations.
F Fiberoptic-Assisted Endotracheal Intubation
Fiberoptic-assisted endotracheal intubation (FOI) has revolutionized management of the DA. FFBs for airway management began to be used in anesthesia practice in the 1970s but initially did not gain widespread acceptance. The problem was a lack of effective training of anesthesiologists. In most cases, the FFB was used only when a DA was anticipated and the plan was for an awake intubation. The clinical situation, consequently, was an inexperienced endoscopist, an abnormal airway, and an awake, uncomfortable patient. The outcome was not likely to be pleasant or successful. It was not until creative airway management teachers developed effective teaching programs that FOI became a routine part of resident education.42,43 Although much progress has been made with resident education, there is still inconsistency among residency programs with respect to FOI.44
Performance of FOI is a skill that every advanced airway management provider should master. Although the process by which providers are taught this skill has not been standardized, there is sufficient evidence in the medical literature to provide guidance for instructional development. A department’s or institution’s ultimate training system may be influenced by financial and manpower resources. There are low-tech and high-tech models and simulators that can be used. Do skills learned with models and simulators transfer to clinical performance? Resolution of this question is central to the efficacy of medical simulation education and remains controversial.45 The preponderance of evidence concerning FOI affirms the theory that there is significant skill retention and transference.46–48
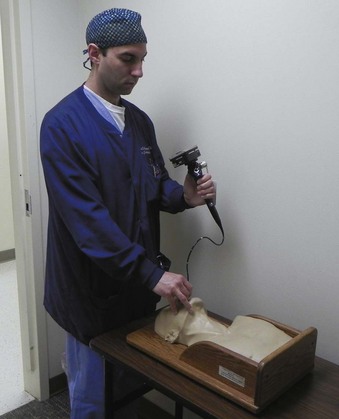
The course for FOI should begin with didactic material that describes upper airway anatomy, FFB construction and operation, and the fundamentals of FFB manipulation. This material may be presented in a traditional lecture format or via a computer program. The next phase of the program must permit the learner to practice FOI. This can be accomplished with static mannequins of the head and neck or with simple, nonanatomic models that require the learner to recognize objects or numbers after FFB manipulation. These models can be constructed with boxes or tubes that require the learner to visualize the images through the FFB during the process of FOI (Fig. 52-4). More realistic static mannequins are also available (Fig. 52-5). The video bronchoscope is a very useful device because the instructor can observe the intubation process on the monitor and offer suggestions to the learner as the intubation progresses (Fig. 52-6). Modern video bronchoscopes produce a high-resolution, wide-angle image of the airway. Teaching with a video bronchoscope improves the rapidity and success of endotracheal intubation by anesthesiology residents.49
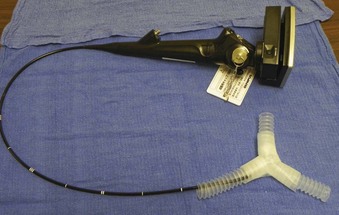
Figure 52-4 An inexpensive and easily constructed model of a tracheobronchial tree made from anesthesia circuit tubing.
There are high-fidelity simulators specifically designed for FFB training. These simulators accurately reproduce the responses to the user’s manipulations, including mucosal bleeding, coughing, and laryngeal motion with respiration. Goldman and associates demonstrated that virtual reality–trained novices quickly learned FFB manipulation, and after a short training period, they performed as well as experienced attending anesthesiologists.50 A high-fidelity simulator can replace the need for practice with animal and cadaver models. High-fidelity simulators are expensive and may not offer significant advantages over less expensive models. Virtual reality computer programs may provide the same benefits as high-tech bronchoscopic simulators.51
After the student has mastered the extraoperative phases of the training program, he or she is ready to begin clinical training with oral FOI of lean patients with normal airways receiving general anesthesia.52,53 This part of the training emphasizes FFB navigation, management of secretions in the airway, and passage of an endotracheal tube over the FFB. This teaching program works just as well for pediatric patients.54 The time required to become competent with FOI varies from resident to resident. Some may be very capable after 10 to 15 successful intubations, whereas others may require 25 to 50 intubations.55 After a resident is competent with FOI of normal patients, he or she can progress to patients that can be easily ventilated after induction of anesthesia but in whom laryngoscopy is difficult.
After proficiency with FOI of anesthetized patients can be demonstrated, the learner is ready to progress to awake intubation. The entire educational process can be completed in 4 to 6 weeks by most anesthesiology residents—a relatively short time to acquire such a valuable skill (Box 52-3). The challenge for residents from other specialties is having enough clinical opportunities after completing simulator training. Collaborative efforts among anesthesiologists; intensivists; ED physicians; ear, nose, and throat surgeons; and pulmonologists are required to meet the educational needs of all the appropriate disciplines.
G Invasive Airway Techniques
Invasive airway techniques are difficult to practice because of limited clinical opportunities. Although mannequins do not accurately replicate the clinical scenario for most invasive airway techniques, mannequin practice does allow the learner to practice the sequence of steps for emergency invasive airway management. Some institutions employ fresh cadavers, isolated animal tracheas, or anesthetized animals as models for invasive airway insertion (Fig. 52-7).56,57
The necessity for emergency invasive airway procedures has undoubtedly been diminished by the development of SLAs and VLs.58 This is fortunate in that providers with minimal invasive experience do not have a high success rate with invasive airway techniques and can encounter significant complications when performing them.59 However, there are still situations in which all noninvasive methods have failed and an emergent, invasive airway technique is required.
H Comprehensive Airway Management
The final step for educating individual medical providers who need broad airway skills, such as anesthesiologists, ED physicians, and critical care physicians, is a clinical rotation focused on airway management problems. The traditional approach to clinical airway training was based on the concept that each resident would acquire sufficient exposure to airway cases during residency (apprenticeship model). This teaching model promotes inconsistency among programs and individual inconsistencies within programs. Professional anesthesiology organizations have failed to provide specific guidelines for training in airway management. More progressive educators have instituted airway rotations in their residency programs to expose all residents to a wide variety of airway devices and techniques.60 As more clinicians who have had comprehensive airway training enter clinical practice, their training should provide a springboard for further professional development.61
Simulation can be employed to evaluate team performance and institutional protocols.62,63 This methodology will assume increasing importance as health care institutions merge into larger organizations and become more process oriented. For many processes it is yet unknown whether patient outcome is significantly improved, therefore a validation of their merit is required. Multidisciplinary simulated exercises may expose deficiencies in institutional procedures for management of high-risk patient events.
VII Conclusions
Training programs should develop simulation-based education curricula.64 Instruction in airway management is well suited for simulation. An alternative to developing an in-house simulation center is to use established simulation centers. The ASA has developed a process for simulation center endorsement, and the network of endorsed simulation centers continues to expand. There is little doubt that medical simulation at all levels of complexity has become an integral part of medical education.
VIII Clinical Pearls
• The first step in developing a simulation program is construction of a curriculum with clear educational objectives.
• The technology of the simulator should not interfere with teaching objectives.
• The type of simulator (low-fidelity or high-fidelity) should be matched to the educational plan.
• Simulation should replicate the clinical environment as closely as possible.
• Licensure and accreditation may in the future require measurement of performance on simulators.
All references can be found online at expertconsult.com.
9 Martin LD, Mhyre JM, Shanks AM, et al. 3,423 Emergency tracheal intubations at a university hospital. Anesthesiology. 2011;114:42–48.
10 McGaghie WC, Issenberg SB, Petrussa ER, et al. A critical review of simulation-based medical education research. Med Educ. 2010;44:50–63.
12 Rai MR, Popat MT. Evaluation of airway equipment: Man or manikin? Anaesthesia. 2011;66:1–3.
18 Borges BC, Boets S, Siu LW, et al. Incomplete adherence to the ASA difficult airway algorithm is unchanged after a high-fidelity simulation session. Can J Anaesth. 2010;57:644–649.
19 Eich C, Timmerman A, Russo SG, et al. A controlled rapid-sequence induction for infants may reduce unsafe actions and stress. Acta Anaesthesiol Scand. 2009;53:1167–1172.
20 Bruppacher HR, Alam SK, LeBlanc VR, et al. Simulation-based training improves physicians’ performance in patient care in high-stakes clinical setting of cardiac surgery. Anesthesiology. 2010;112:985–992.
22 Russo SG, Eich C, Barwig J, et al. Self-reported changes in attitude and behavior after attending a simulation-aided airway management course. J Clin Anesth. 2007;19:517–522.
27 DeMaria S, Levine AI, Bryson EO. The use of multi-modality simulation in the retraining of the physician for medical licensure. J Clin Anesth. 2010;22:294–299.
35 Mulcaster JT, Mills J, Hung OR, et al. Laryngoscopic intubation: Learning and performance. Anesthesiology. 2003;98:23–27.
42 Roberts JT. Preparing to use the flexible fiber-optic laryngoscope. J Clin Anesth. 1991;3:64–75.
60 Crosby E, Lane A. Innovations in anesthesia education: The development and implementation of a resident rotation for advanced airway management. Can J Anaesth. 2009;56:939–959.
1 Caplan RA, Posner KL, Ward RJ, et al. Adverse respiratory events in anesthesia: A closed claims analysis. Anesthesiology. 1990;72:828–833.
2 American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Practice guidelines for management of the difficult airway. Anesthesiology. 1993;78:597–602.
3 American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Practice guidelines for management of the difficult airway: An updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2003;98:1269–1277.
4 Amathieu R, Combes X, Abdi W, et al. An algorithm for difficult airway management, modified for modern optical devices (Airtraq laryngoscope, LMA CTrach). Anesthesiology. 2011;114:25–33.
5 Henderson JJ, Popat MT, Latto IP, et al. Difficult Airway Society guidelines for management of the unanticipated difficult intubation. Anaesthesia. 2004;59:675–694.
6 Cheney FW. The American Society of Anesthesiologists closed claims project. Anesthesiology. 1999;91:552–556.
7 Peterson GN, Domino KB, Caplan RA, et al. Management of the difficult airway: A closed claims analysis. Anesthesiology. 2005;103:33–39.
8 Rose DK, Cohen MM. The airway: Problems and predictions in 18,500 patients. Can J Anaesth. 1994;41:372–383.
9 Martin LD, Mhyre JM, Shanks AM, et al. 3,423 Emergency tracheal intubations at a university hospital. Anesthesiology. 2011;114:42–48.
10 McGaghie WC, Issenberg SB, Petrussa ER, et al. A critical review of simulation-based medical education research. Med Educ. 2010;44:50–63.
11 Miller GE. The assessment of clinical skills/competence/performance. Acad Med. 1990;65:S63–S67.
12 Rai MR, Popat MT. Evaluation of airway equipment: Man or manikin? Anaesthesia. 2011;66:1–3.
13 Cannon-Bowers JA. Recent advances in scenario-based training for medical education. Curr Opin Anesth. 2008;21:784–789.
14 Demczuk L, Gottschalk T, Littleford J. Introducing computer literacy into anesthesia curricula. Can J Anaesth. 2009;56:327–335.
15 Ruiz J, Candler C, Teasdale TA. Peer reviewing E-learning: Opportunities, challenges, and solutions. Acad Med. 2007;82:503–507.
16 Doyle DJ. Web-based education in anesthesiology. Curr Opin Anaesth. 2008;21:766–771.
17 Grenvik A, Schaefer JJ. Medical simulation training coming of age. Crit Care Med. 2004;32:2549–2550.
18 Borges BC, Boets S, Siu LW, et al. Incomplete adherence to the ASA difficult airway algorithm is unchanged after a high-fidelity simulation session. Can J Anaesth. 2010;57:644–649.
19 Eich C, Timmerman A, Russo SG, et al. A controlled rapid-sequence induction for infants may reduce unsafe actions and stress. Acta Anaesthesiol Scand. 2009;53:1167–1172.
20 Bruppacher HR, Alam SK, LeBlanc VR, et al. Simulation-based training improves physicians’ performance in patient care in high-stakes clinical setting of cardiac surgery. Anesthesiology. 2010;112:985–992.
21 Kuduvalli PM, Jervis A, Tighe SQ, et al. Unanticipated difficult airway management in anesthetized patients: A prospective study of the effect on mannequin training on management strategies and skill retention. Anaesthesia. 2008;63:364–369.
22 Russo SG, Eich C, Barwig J, et al. Self-reported changes in attitude and behavior after attending a simulation-aided airway management course. J Clin Anesth. 2007;19:517–522.
23 Nargozian CD. Simulation and airway-management training. Curr Opin Anesth. 2004;17:511–512.
24 Morgan PJ, Cleave-Hogg D, McIlroy J, et al. Simulation technology: A comparison of experiential and visual learning for undergraduate medical students. Anesthesiology. 2002;96:10–16.
25 Marsland C, Larsen P, Segal R, et al. Proficient manipulation of fibreoptic bronchoscope to carina by novices on first clinical attempt after specialized bench practice. Br J Anaesth. 2010;104:375–381.
26 Hesselfeldt R, Kristensen MS, Rasmussen LS. Evaluation of the airway of the SimMan full-scale patient simulator. Acta Anaesthesiol Scand. 2005;49:1339–1345.
27 DeMaria S, Levine AI, Bryson EO. The use of multi-modality simulation in the retraining of the physician for medical licensure. J Clin Anesth. 2010;22:294–299.
28 Ziv A, Rubin O, Sidi A, et al. Credentialing and certifying with simulation. Anesthesiol Clin. 2007;25:261–269.
29 De Visser H, Watson MO, Salvado O, et al. Progress in virtual reality simulators for surgical training and certification. Med J Australia. 2011;194:S38–S40.
30 Schaefer JJ. Simulators and difficult airway management skills. Pediatr Anesth. 2004;14:28–37.
31 Jackson KM, Cook TM. Evaluation of four airway training manikins as patient simulators for the insertion of eight different types of supraglottic airway devices. Anaesthesia. 2007;62:388–393.
32 Lopez-Gil M, Brimacombe J, Cebrian J, et al. Laryngeal mask airway in pediatric patients. Anesthesiology. 1996;84:807–811.
33 Brimacombe J. Analysis of 1500 laryngeal mask uses by one anaesthetist in adults undergoing routine anaesthesia. Anaesthesia. 1996;51:76–80.
34 Dierdorf SF. Education in the use of the laryngeal mask airway. Int Anesthesiol Clin. 1998;36:19–28.
35 Mulcaster JT, Mills J, Hung OR, et al. Laryngoscopic intubation: Learning and performance. Anesthesiology. 2003;98:23–27.
36 Timmerman A, Russo SG, Crozier TA, et al. Laryngoscopic versus intubating LMA guided tracheal intubation by novice users: A manikin study. Resuscitation. 2007;73:412–416.
37 Aiken SD, Delson N, Davidson TM, et al. A two-dimensional model of anatomic relationships during laryngoscopy. Anesth Analg. 2007;105:1118–1126.
38 Ayoub CM, Kanazi GE, Al Alami A, et al. Tracheal intubation following training with the GlideScope compared to direct laryngoscopy. Anaesthesia. 2010;65:674–678.
39 Kaplan MB, Ward D, Hagberg CA, et al. Seeing is believing: The importance of video laryngoscopy in teaching and in managing the difficult airway. Surg Endosc. 2006;20:S479–S483.
40 McElwain J, Malik MA, Harte BH, et al. Comparison of the C-MAC videolaryngoscope with the Macintosh, Glidescope, and Airtraq laryngoscopes in easy and difficult laryngoscopy scenarios in manikins. Anaesthesia. 2010;65:483–489.
41 Zamora JE, Nolan RL, Sharan S, et al. Evaluation of the Bullard, GlideScope, Viewmax, and Macintosh laryngoscopes using a cadaver model to simulate the difficult airway. J Clin Anesth. 2011;23:27–34.
42 Roberts JT. Preparing to use the flexible fiber-optic laryngoscope. J Clin Anesth. 1991;3:64–75.
43 Dykes MHM, Ovassapian A. Dissemination of fibreoptic airway endoscopy skills by means of a workshop utilizing models. Br J Anaesth. 1989;63:595–597.
44 Koppel JN, Reed AP. Formal instruction in difficult airway management. Anesthesiology. 1995;83:1343–1346.
45 Lynagh M, Burton R, Sanson-Fisher R. A systematic review of medical skills laboratory training: Where to from here? Med Edu. 2007;41:879–887.
46 Ovassapian A, Yelich SJ, Dykes MHM, et al. Learning fibreoptic intubation: Use of simulators v. traditional teaching. Br J Anaesth. 1988;61:217–220.
47 Naik VN, Matsumoto ED, Houston PL, et al. Fiberoptic intubation on anesthetized patients. Anesthesiology. 2001;95:343–348.
48 Blum MG, Powers TW, Sundaresan S. Bronchoscopy simulator effectively prepares junior residents to competently perform basic clinical bronchoscopy. Ann Thorac Surg. 2004;78:287–291.
49 Wheeler M, Roth AG, Dsida RM, et al. Teaching residents pediatric fiberoptic intubation of the trachea. Anesthesiology. 2004;101:842–846.
50 Goldmann K, Steinfeldt T. Acquisition of basic fiberoptic intubation skills with a virtual reality airway simulator. J Clin Anesth. 2006;18:173–178.
51 Boet S, Bould MD, Schaeffer R, et al. Learning fibreoptic intubation with a virtual computer program transfers to “hands on” improvement. Eur J Anaesth. 2010;27:31–35.
52 Erb T, Hampel KF, Schurch M, et al. Teaching the use of fiberoptic intubation in anesthetized, spontaneously breathing patients. Anesth Analg. 1999;89:1292–1295.
53 Cole AFD, Mallon JS, Rolbin SH, et al. Fiberoptic intubation using anesthetized, paralyzed, apneic patients. Anesthesiology. 1996;84:1101–1106.
54 Erb T, Marsch SCU, Hampl KF, et al. Teaching the use of fiberoptic intubation for children older than two years of age. Anesth Analg. 1997;85:1037–1041.
55 Johnson C, Roberts JT. Clinical competence in the performance of fiberoptic laryngoscopy and endotracheal intubation: A study of resident instruction. J Clin Anesth. 1989;1:344–349.
56 Tabas JA, Rosenson J, Price DD, et al. A comprehensive, unembalmed cadaver-based course in advanced emergency procedures for medical students. Acad Emerg Med. 2005;12:782–785.
57 Schober P, Hegemann MC, Schwarte LA, et al. Emergency cricothyrotomy: A comparative study of different techniques in human cadavers. Resuscitation. 2009;80:204–209.
58 Berkow LC, Greenberg RS, Kan KH, et al. Need for surgical airway reduced by a comprehensive difficult airway program. Anesth Analg. 2009;109:1860–1869.
59 Eisenburger P, Laczika K, List M, et al. Comparison of conventional surgical versus Seldinger technique emergency cricothyrotomy performed by inexperienced clinicians. Anesthesiology. 2000;92:687–690.
60 Crosby E, Lane A. Innovations in anesthesia education: The development and implementation of a resident rotation for advanced airway management. Can J Anaesth. 2009;56:939–959.
61 Drolet P. Management of the anticipated difficult airway: A systematic approach: Continuing professional development. Can J Anaesth. 2009;56:683–701.
62 Hunt EA, Shilkofski NA, Stavroudis TA, et al. Simulation: Translation to improved team performance. Anesthesiol Clin. 2007;25:301–319.
63 Andreatta P, Frankel J, Smith SB, et al. Interdisciplinary team training identifies discrepancies in institutional policies and practices. Am J Ob Gynecol. 2011;205:298–301.
64 Seropian MA. General concepts in full scale simulation: Getting started. Anesth Analg. 2003;97:1695–1705.