Tachyarrhythmias
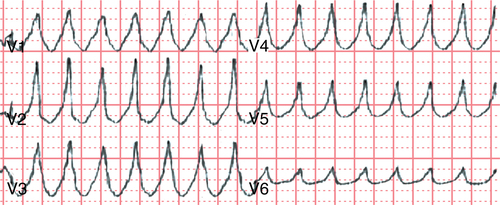
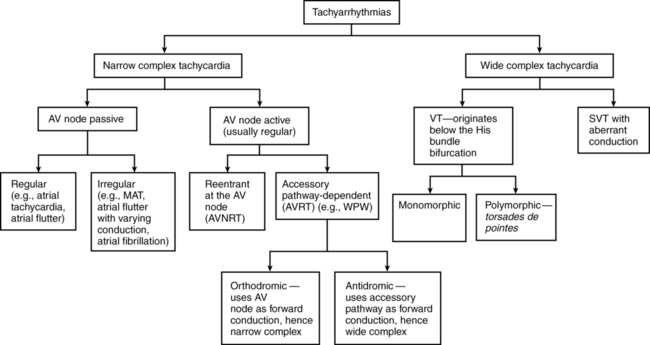
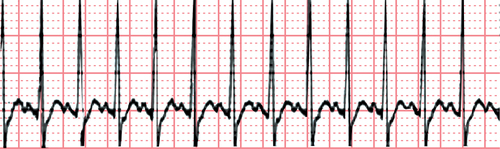
It is important to understand the mechanisms of these arrythmias because AV node-active tachycardias can usually be terminated by maneuvers that prolong AV node conduction, such as vagal maneuvers, or the administration of drugs, such as adenosine (Figure 36-1).
Wide complex tachycardias
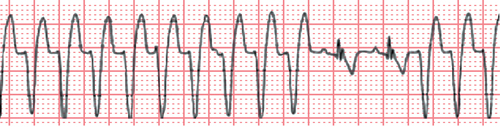
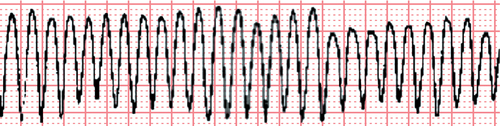
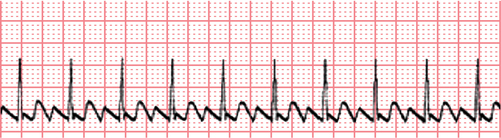
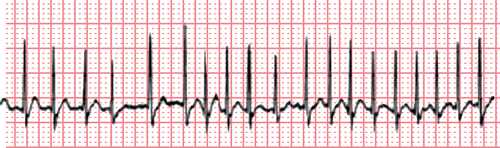
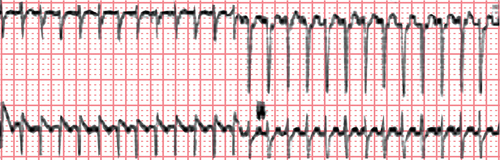
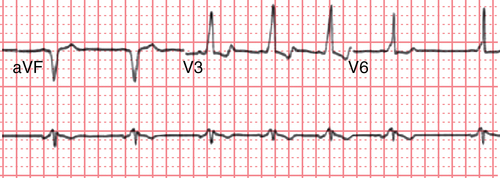
WCTs are defined as arrhythmias with a QRS complex duration longer than 0.12 sec at a rate greater than 100 beats/min. WCTs are presumed to be ventricular tachycardias (VTs) until proved otherwise, although some supraventricular tachycardias (SVTs) can present as WCT (SVT with aberrancy). Differentiating between SVTs with a wide QRS complex and a VT is critical because the treatment is very different (Figures 36-2 to 36-11).


Diagnosis
For the purpose of diagnosis, WCTs can be classified into four categories based on the following:
1. Origination above or below the bifurcation of the His bundle.
2. Presence of an SVT with aberrant ventricular conduction. SVT with aberrancy can be due to conduction slowing or bundle branch block. It can also be due to anterograde conduction over an accessory AV pathway (antidromic Wolff-Parkinson-White [WPW] syndrome).
3. Presence of a wide QRS waveform generated by ventricular pacing.
4. Presence of electrolyte abnormalities, such as hyperkalemia or hypokalemia, or the use of medications, such as tricyclic antidepressants and antihistamines (sodium channel blocking drugs).