Chapter 48 Syncope
Introduction
Syncope is a transient loss of consciousness (TLOC) with subsequent complete resolution and no focal neurologic deficits; it results from cerebral hypoperfusion and does not require specific resuscitative measures. Recent expert consensus conferences, position papers, and narrative reviews have covered the various aspects of syncopal syndromes.1–9
Epidemiology
Approximately 40% of people faint at least once in their lives, and at least 20% of adults faint more than once.10 (Many terms are used by patients to report syncope, such as faint, blackout, and funny spell. To avoid contributing to this plethora of miscommunication, this chapter uses faint and syncope interchangeably.) Syncope comprises 1% to 6% of emergency department (ED) visits, and most patients are admitted to the hospital largely because of diagnostic uncertainty and concern that an underlying cause might result in morbidity or death.11–32 People who faint often present first in their teens and twenties and may faint sporadically for decades.10 This long, usually benign, sporadic history can make for difficult decisions about therapy. An early peak incidence occurs at approximately 15 years for young women; a later important rise in incidence occurs in both sexes after age 65 years.4 Although many patients of all ages experience simple vasovagal syncope, clinicians need to remain vigilant and look for other causes, including sick sinus syndrome, a variety of tachyarrhythmias, carotid sinus syncope, valvular and structural heart disease, and orthostatic hypotension.1–46
Impact on the Health Care System
Although syncope accounts for approximately 1% of ED visits, most patients with syncope with otherwise unknown causes in the community and approximately 45% of syncope patients who present to EDs in North America and Europe experience simple vasovagal syncope. In the United States, approximately $2.4 billion is spent yearly in hospitals to treat syncope.6 In The Netherlands, among those younger than 65 years, 3.8 and 8.5 visits per 1000 person-years are made to family doctors for males and females, respectively.12 Canadian and Italian estimates for ED presentations are 2.5-fold and 3.5-fold higher, respectively, than the estimates from The Netherlands.6 The estimated direct impact on U.S. health care is $2.5 to $10 billion annually.4–6,33,34
Differential Diagnosis of Syncope
Transient Loss of Consciousness
Patients usually present with a history of TLOC, and although most of these patients experience syncope, the differential diagnosis of TLOC should be considered early in assessment. Other causes of apparent TLOC include epileptic and nonepileptic seizures, cataplexy, narcolepsy, pseudo-syncope, and rarer causes such as drop attacks and nonconvulsive epilepsy. The problem faced by assessing physicians is that patients may present simply with a history of unexplained losses of consciousness. The first step is to determine whether the loss of consciousness occurred because of syncope. The most common confusing presentations are addressed in this section. Not all these cause true loss of consciousness, but they can mimic it and therefore must be considered, albeit briefly.1,4
Convulsions and Syncope
Although patients experiencing syncope usually lose motor control and are flaccid while unconscious, they frequently present with a history of convulsions and syncope (Table 48-1).7,9 This raises the question of whether the patients have true epileptic convulsions or convulsions secondary to cerebral hypoperfusion. Stiffness and myoclonic jerking are not uncommon in the latter case and cause confusion in the minds of those who witness the episode. Convulsive syncope can usually be distinguished from epileptic seizures through careful history taking. Stiffness and myoclonus last only a few seconds; only rarely will these patients have a true generalized convulsion. Patients with convulsive syncope usually have a history of recurrent syncope and presyncope. It is often helpful to elicit a similar history of the characteristic presyncopal prodrome of the patient and the symptoms preceding the apparent convulsion. Convulsive syncope rarely occurs when the patient is in the supine position and is usually brief, lasting only a few seconds. Pallor usually accompanies vasovagal syncope, whereas cardiac syncope and epileptic seizures are often accompanied by cyanosis. Myoclonic tremors usually have a fine amplitude, and epileptic seizures usually have dramatically coarse movements. Tongue biting rarely occurs in convulsive syncope and usually involves the tip of the tongue rather than the lateral tongue, as seen in true epileptic seizures. After a syncopal episode, the patient is briefly dazed, but the condition clears within a minute, whereas epileptic seizures can be followed by confusion that can last hours. If a history does not provide a clear conclusion, further testing is warranted.
Table 48-1 Diagnostic Questions to Determine Whether Loss of Consciousness Is Due to Seizures or Syncope
| QUESTION | POINTS (IF YES) |
|---|---|
| At times, do you wake with a bitten tongue after your spells? | 2 |
| At times, do you have a sense of déjà vu or jamais vu before your spells? | 1 |
| At times, is emotional stress associated with losing consciousness? | 1 |
| Has anyone ever noted your head turning during a spell? | 1 |
| Has anyone ever noted that you are unresponsive, have unusual posturing or jerking limbs during your spells, or have no memory of your spells afterwards? (Score as yes for any positive response.) | 1 |
| Has anyone ever noted that you are confused after a spell? | 1 |
| Have you ever had spells of lightheadedness? | –2 |
| At times, do you sweat before your spells? | –2 |
| Is prolonged sitting or standing associated with your spells? | –2 |
The patient has seizures if the point score is ≥1 and syncope if the point score is <1.
From Sheldon R, Rose S, Ritchie D, et al: Historical criteria that distinguish syncope from seizures, J Am Coll Cardiol 40:142–148, 2002.
Pseudo-syncope
Functional or psychogenic syncope is often mistaken initially for true syncope.7,9 These patients often have an antecedent history of true vasovagal syncope, which usually becomes more frequent before presentation. The patients are usually young women who faint extremely frequently. Only the rare patient faints several times weekly to several times daily, but this is not unusual in pseudo-syncope. The spells can last many minutes, giving an appearance of syncope lasting up to an hour. The history usually does not include the transient autonomic symptoms that often accompany vasovagal syncope, and patients rarely volunteer a history of visual disturbances that often precede true syncope. These visual changes—blurring, tunneling down, spots, stars, and visual blackening—are caused by retinal hypoperfusion and are a reliable marker of a true hemodynamic disturbance.9 An antecedent history of physical or sexual abuse often exists. The diagnosis can occasionally be confirmed if the patient has a fainting spell in monitored situations such as during a tilt-table test (TTT) or while undergoing electroencephalography (EEG).
Orthostatic Hypotension
Orthostatic hypotension is defined conventionally as a drop in systolic blood pressure of at least 20 mm Hg or a drop in diastolic blood pressure of at least 10 mm Hg. New and more restrictive definitions are under consideration. The drop in blood pressure is a measurement, not a diagnosis. Several syndromes are characterized by presyncope or syncope caused by orthostatic hypotension. Not infrequently, symptomatic orthostatic hypotension occurs because of volume depletion of blood after a heavy meal. Initial orthostatic hypotension occurs within 5 to 20 seconds of arising quickly, often in association with standing and walking. Presyncope is much more common than syncope.9,35 The hypotension is caused by a transient draw-down of central arterial volume to the exercising bed, accompanied by a delay in baroreceptor-mediated compensation. No specific treatment is necessary. Drug-induced orthostatic hypotension is often caused by polypharmacy, including diuretics, vasodilators, and adrenergic receptor antagonists. Syndromes of orthostatic hypotension, in which symptoms develop over longer periods, usually occur in older patients. Here, the primary symptom is presyncope, and the longer the patient is upright, the worse is the lightheadedness. Syncope occurs less commonly and usually after prolonged upright posture. Primary autonomic failure occurs in the setting of one of several relatively uncommon neurodegenerative diseases such as pure autonomic failure, multiple system atrophy, and Parkinson disease. Finally, secondary autonomic failure can occur with damage to the autonomic nervous system caused by systemic diseases such as diabetes, Parkinson disease, or multiple-system atrophy.3,4,9,35
Cardiac Syncope
Syncope caused by arrhythmias or structural heart disease is much less common than vasovagal syncope but carries a risk of significant morbidity and death.4,5 It is usually caused by an abrupt drop in cardiac output and typically occurs within the first few seconds of onset of the arrhythmia. The most likely reason is that baroreceptor-mediated compensatory vasoconstriction takes 10 to 20 seconds to have an effect, leaving the patient unprotected for that time. However, reports also document the association of vasovagal syncope with supraventricular tachycardia (SVT), atrial fibrillation (AF), and inappropriate sinus bradycardia.36–38 Factors such as arterial baroreceptor sensitivity, posture of the patient, volume status, associated cardiopulmonary disease, and reflex peripheral vascular compensation all play a role in determining whether tachycardia could be the reason for the syncope. The diagnosis and management of these arrhythmias are covered in detail in other chapters of this book.
Patients often present with undocumented syncope and a documented substrate that might be related to the cause, such as syncope with bifascicular block.39–43 No clear consensus or firm evidence exists to guide treatment for these patients. In this setting, reasonable equipoise exists, for example, between implanting a loop recorder or performing an invasive electrophysiological study (EPS) and simply performing a therapeutic procedure such as pacemaker insertion. Importantly, the patients should be assessed for other cardiovascular risk factors that may take precedence in investigation and therapy. Patients with severe left ventricular systolic dysfunction and syncope usually require an implantable cardioverter-defibrillator, even though this might not treat neurally mediated syncope.4
Diagnosing the Cause of Syncope
Diagnostic Approach
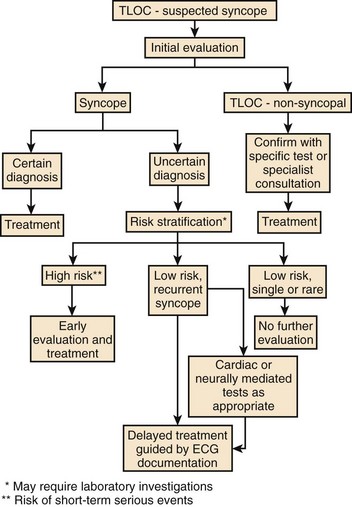
General principles with good evidence to support them have been reviewed in detail in the recent European Society of Cardiology (ESC) guidelines.4 History and physical examination are fundamental to the diagnosis of syncope. A detailed and accurate history provides a diagnosis in most cases, a prognosis for vasovagal syncope, an understanding of patient needs and preferences, and an economic basis for further investigation. The efficient use of investigations, as appropriate, should be based on the flow charts presented in the ESC document (Figure 48-1).
The first step in the differential diagnosis is to identify whether the TLOC episode was truly syncope, that is, a self-limited loss of consciousness caused by transient global hypoperfusion. Other causes of TLOC, such as epileptic seizures, narcolepsy, cataplexy, true drop attack, and hypoglycemic coma, should be briefly considered; however, in day-to-day clinical practice, they are rarely mistaken for syncope. Important and life-threatening potential causes such as cardiac syncope from arrhythmias or structural heart disease should be carefully considered in every case. Specific investigations can be selected on the basis of the initial assessment.1,4,6
History and Physical Examination
The initial evaluation of history, physical examination, and the electrocardiogram (ECG) often leads to a certain diagnosis. A Dutch study with more than 500 patients with TLOC found that, based on a 2-year follow-up, physicians who used only history, physical examination, and ECG made a diagnosis in 63% of the patients, with a diagnostic accuracy of 88%.44 If the diagnosis is certain, usually no further (or minimal) investigations are needed, and the focus then shifts to management. With an uncertain diagnosis, further careful, directed testing is usually necessary. The rare patient with frequent, recurrent episodes, especially in the context of other somatic concerns, may have a psychiatric illness.
Patients with syncope may describe their episodes in a variety of ways, including “dizziness,” “fainting,” “lightheadedness,” and “blackouts.” A prodrome may last from less than a second to several minutes. Most episodes occur when the patient is in the upright posture, occasionally in the sitting posture, and very rarely in the supine position. Patients often report additional presyncopal episodes and being able to avert syncope by sitting or lying down quickly. Patients are usually unresponsive for less than a minute and often fatigued for hours or even days after an episode but are oriented and responsive within minutes. Pallor is often observed.4–79
Recent work has suggested the importance of quantitative diagnostic scores.45–47 Quantitative histories and diagnostic scores are well known in other fields, and they improve diagnostic accuracy. A comprehensive set of questions that provides a single diagnosis out of all possible diagnoses does not exist; rather, the questions need to be asked in sequences of groups. First, determine if this is syncope or another diagnosis such as epilepsy. A point score that distinguished seizures from syncope with an accuracy of 94% was recently published (see Table 48-1).47 Second, determine whether the patient has structural heart disease by inquiring about his or her cardiovascular history. If the patient does not have structural heart disease, the diagnostic difference between reflex neurally mediated syncope and arrhythmic syncope depends on specific provocative situations, associated symptoms and signs, age of onset, and underlying arrhythmias. A quantitative score (Table 48-2) that works with more than 90% accuracy in patients younger than 60 years is widely available.46 Older patients often require further investigation.48 Another quantitative score has 99% sensitivity and 68% specificity for ventricular tachycardia (VT) in patients with structural heart disease (Table 48-3), and it is accurate with regard to diagnosis as well as arrhythmic and fatal outcomes.45
Table 48-2 Calgary Syncope Symptom Score for Structurally Normal Hearts
| QUESTION | POINTS (IF YES) |
|---|---|
| Is there a history of at least one of the following: bifascicular block, asystole, supraventricular tachycardia, diabetes? | –5 |
| At times, have bystanders noted you to turn blue during your faint? | –4 |
| Did your syncope start at age 35 years or older? | –3 |
| Do you remember anything about being unconscious? | –2 |
| Do you have spells of lightheadedness or faint with prolonged sitting or standing? | 1 |
| Do you sweat or feel warm before a faint? | 2 |
| Do you have spells of lightheadedness or faint with pain or in medical settings? | 3 |
The patient has vasovagal syncope if the point score is ≥–2.
From Sheldon R, Rose S, Connolly S, et al: Diagnostic criteria for vasovagal syncope based on a quantitative history, Eur Heart J 27:344–350, 2006.
Table 48-3 Calgary Syncope Symptom Score for Structural Heart Disease*
| QUESTION | POINTS (IF YES) |
|---|---|
| Was your age at first faint at age 34 years or later? | 3 |
| Are you a male? | 1 |
| Have you become lightheaded or fainted with prolonged sitting or standing? | –1 |
| Have you become lightheaded with stress?† | –2 |
| At times, are you tired for more than 1 minute after a fainting episode? | –2 |
| Do you have recurrent headaches? | –2 |
The patient has ventricular tachycardia if the score is ≥1 and vasovagal syncope if the score is <1.
* Diagnostic questions to determine whether syncope is caused by ventricular tachycardia or vasovagal syncope.
† The term “stress” was used in its colloquial sense and meant to capture psychosocial stress.
From Sheldon R, Hersi A, Ritchie D, et al: Syncope and structural heart disease: Historical criteria for vasovagal syncope and ventricular tachycardia, J Cardiovasc Electrophysiol 21:1358–1364, 2010.
These scores have several uses. They provide validated, quantitative, objective, diagnostic inclusion criteria that, by reducing the need for TTT, provide rapid translation of clinical trial results into community practice. In this setting, they provide reproducible criteria for clinical studies.49 Although these scores should not be the sole basis for diagnosis, they are useful aids in clinical practice. Finally, they may eventually provide a framework for evidence-based definitions of syndromes.
Finally, current understanding about predicting vasovagal syncope recurrence is much clearer.50–54 Almost all the predictive power is in the year immediately before presentation. A patient who has not fainted in the previous year has only a 7% risk of syncope in the next year, but a patient with at least one faint in the previous year has a 42% risk of syncope in the next year.50
Selection of Tests
The first stage of testing screens for a substrate for syncope, including careful clinical assessment, a resting ECG, and, when appropriate, short-term ECG monitoring, echocardiography, and blood work.6 This provides a presumptive diagnosis in most patients as well as a prognosis, which is particularly important because syncope with underlying heart disease is a risk for sudden cardiac death (SCD). The yield of blood tests in detecting the cause of syncope is only 2% to 3%, detecting mostly electrolyte or metabolic abnormalities causing seizure. A hematocrit level less than 0.3 is useful for the detection of gastrointestinal bleeding.27,55,56 Blood tests (hemoglobin, electrolytes, cardiac biomarkers) should be performed only in the presence of a clinical suspicion of occult hemorrhage, arrhythmias/seizures caused by electrolyte or metabolic abnormalities, or myocardial infarction (MI).
Tests such as echocardiography, coronary angiography, and radionuclide scintigraphy are of little value in unselected populations and should only be used when indicated by clinical assessment.57 The primary role of this form of testing is to establish or exclude the presence of potentially contributory structural heart disease. An echocardiogram should be obtained in the presence of known heart disease, data suggestive of structural heart disease, syncope secondary to cardiovascular cause, syncope with exertion, or a murmur.
Computed tomography (CT) of the head is performed in nearly half of all syncope patients but has a less than 1% likelihood of detecting a cause.58 Similarly, conventional EEG is rarely useful in the investigation of unselected patients with syncope. In contrast, although the yield of an ECG is less than 5% in unselected patients, it is noninvasive and inexpensive and can detect life-threatening abnormalities. Accordingly, it is recommended in all patients.
The second stage of testing is aimed at the specific cause of syncope. Here, provocative testing is used to induce a syncopal episode or to detect an abnormal physiological response that might explain the history of syncope. This includes tests such as TTT and EPS. Interpretation of these tests requires considerable judgment because these tests induce a physiological response (not the event itself) and are plagued by lack of sensitivity, lack of specificity, or both. An alternative approach is the use of long-term ECG monitoring with a Holter monitor and external and implantable loop recorders to document the cardiac rhythm associated with a spontaneous episode of syncope. Current devices do not detect hypotension.1,4,6
Tilt-Table Testing
TTT creates orthostatic stress that results in venous pooling and may simulate the hemodynamic changes seen in vasovagal syncope.59–67 The test is performed with continuous ECG and blood pressure monitoring; patients are initially placed in the supine position, and the table is tilted to an angle of 60 to 80 degrees. The patient is kept at this angle for 20 to 45 minutes; further drug provocation with isoproterenol, clomipramine, or nitroglycerin can be used for another 15 to 20 minutes. If symptomatic hypotension and bradycardia occur, the patient is promptly returned to the supine position to prevent injury and the test is concluded. Syncope or presyncope with a cardio-inhibitory response, vasodepressor response, or both reproducing the patient’s symptoms is considered a positive outcome.
As simple as TTT seems, these tests, in fact, contain numerous variables that affect the test outcome.65 Controlled studies have shown that the likelihood of positive tests depends on the angle and duration of the head-up tilt, whether and how a drug challenge is used, the number of head-up iterations during the test, the volume status of the subject, and the subject’s age. A variable correlation exists between the symptoms provoked by TTT and by the subject’s clinical symptoms and widely variable and usually unvalidated hemodynamic criteria to indicate a positive test. The test has not been validated against a gold standard population, and different TTT protocols identify patient populations that do not completely overlap. Patients with otherwise idiopathic syncope have the same baseline symptoms and symptom burden, the same clinical outcome, and the same statistical relationships between baseline symptoms and clinical outcome, regardless of a positive or negative TTT result.52 Finally, an intractable trade-off between diagnostic accuracy and specificity seems to be present. The mechanism observed with syncope at the time of TTT may not correlate with clinical episodes. Hence TTT should be used only in individuals in whom the history, physical examination, and ECG have not established the diagnosis.
Electrocardiographic Monitoring
The implantable loop recorder (ILR) is an ideal device for obtaining rhythms on a continuous basis.4,6,68 Its use is driven by the importance of symptom-rhythm correlation, particularly in settings in which syncope could have one or more causes. For example, AF may cause syncope because of tachycardia onset or pauses after arrhythmia termination. In addition, the high population prevalence of vasovagal syncope often raises vasodepression as a competing diagnosis when arrhythmias are considered.
The ILR is implanted under the skin and does not require any leads or external sensors; it has a pair of sensing electrodes on the shell. It can be automatically activated by an arrhythmia (high and low rate events) or by the patient using an external programmer. Current models have a battery life of 3 years and record the ECG signatures of infrequent syncopal episodes. Several studies have confirmed the usefulness of the ILR in establishing a symptom-rhythm correlation for syncope.68–78 On the whole, syncope recurs in 30% to 50% of patients. A few patients have tachyarrhythmia during syncope, but most of the heart rhythm disturbances are bradycardic. Many of these appear to be caused by reflex-mediated suppression of the sinoatrial and atrioventricular nodal functions during vasovagal syncope. However, the most common rhythm detected is sinus rhythm; presumably the cause of syncope is vasodepression without bradycardia. In the largest study, bradycardia was seen to accompany syncope in less than 30% of cases. The International Study on Syncope of Uncertain Etiology (ISSUE) investigators implanted ILRs in 111 patients with probable vasovagal syncope, regardless of their TTT results. Syncope recurred in 34% of patients, with marked bradycardia or asystole being the most common recorded arrhythmia during syncope (46% and 62%, respectively). The ISSUE investigators reported a classification of rhythm findings that helps distinguish among the causes of bradycardia (Box 48-1).69
Box 48-1 Classification of Rhythm Findings During Syncope as Documented by an Implantable Loop Recorder
Type 1: Asystole (RR pause ≥3 seconds)
Type 3: No or Slight Rhythm Variations (variations of heart rate <30% and >40 beats/min)
Type 4: Tachycardia (increase in heart rate >30% and >120 beats/min)
From Brignole M, Moya A, Menozzi C, et al: Proposed electrocardiographic classification of spontaneous syncope documented by an implantable loop recorder, Europace 7:14–18, 2005.
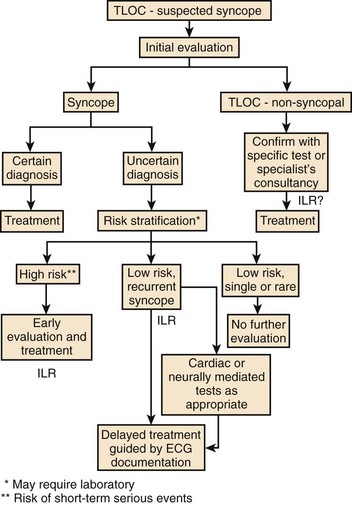
Two prospective randomized trials, one in Canada and one in the United Kingdom, compared early use of the ILR to conventional testing in patients undergoing a cardiac workup for unexplained syncope.6,73,79 Taken together, they demonstrated that ILR resulted in a higher diagnostic yield, at an earlier time, and at a generally lower cost compared with a conventional strategy. The ILR is not for everyone, and the recent European Heart Rhythm Association guidelines suggest a reasonable approach to its use (Figure 48-2).68 Clearly, the ILR is a useful tool for investigating patients with recurrent unexplained syncope when noninvasive test results are negative.4–668
Reflex Neurally Mediated Vasovagal Syncope
Symptoms
Patients develop nausea, diaphoresis, pallor, and loss of consciousness because of hypotension with or without significant bradycardia. Return to consciousness after seconds to 1 to 2 minutes is the norm. Those with adequate warning may be able to simply sit or lie down to prevent a full faint. However, some patients have little or no prodrome, no recognized precipitating stimulus, or marked bradycardia accompanying the faint. Older patients usually have an atypical presentation and may have a prodrome but may not recall it because of retrograde amnesia.9
Syncope Severity and Quality of Life
The vasovagal syncope syndrome has an extremely wide range of symptom burden. The symptom burden varies from a single syncopal spell in a lifetime to daily faints. Patients with frequent syncope have a markedly reduced quality of life, similar to that of patients with severe rheumatoid arthritis or chronic low back pain.80 The reduction in quality of life correlates with the frequency of syncope.81 Quality of life is substantially impaired in all dimensions of health, particularly in terms of mobility, usual activities, and self-care.82–85
Natural History
Vasovagal syncope affects all ages and both sexes. It usually first presents in adolescence and early adulthood, and the predilection to fainting is lifelong. Most patients seen in referral clinics have fainted repeatedly; in the authors’ specialty referral clinic, the median number of faints is 10 to 15, and the median duration of syncopal history is 15 to 20 years. In many patients, syncope appears to occur in clusters that last months to years. Many patients have more frequent presyncopal spells that limit daily activities. Therefore, most patients with syncope do not require lifetime therapy, but they frequently merit treatment that lasts from months to years.86 When assessing patients with syncope, clinicians need to be alert to the surprisingly marked impairment of quality of life that many patients endure, provide a perspective that lasts decades, and remember that the clinical state will probably fluctuate.4,50,51
Diet and Physical Maneuvers
Patients with syncope are encouraged to increase their salt and fluid intake, although the evidence in favor of this therapy is weak (Table 48-4). Patients with positive TTT result convert to a negative response on a subsequent test after receiving an intravenous volume load, and orthostatic tolerance improves with increased dietary salt. The usual reported dose of salt tablets is 6 to 9 g (100 to 150 mmol/L) per day. No substantial evidence exists supporting the use of exercise training to prevent syncope.
| TREATMENT | TREATMENT EFFECT | EVIDENCE |
|---|---|---|
| LIFESTYLE CHANGES | ||
| Increased intake of salt and fluid | Probably helpful | Moderate evidence |
| Physical exercise | Debatable effect | Weak evidence |
| Physical counterpressure | Probably helpful | Good evidence |
| ORTHOSTATIC TRAINING | ||
| Tilt training | Debatable effect | Moderate evidence |
| Home orthostatic training | Probably unhelpful | Good evidence |
| PHARMACOLOGIC THERAPY | ||
| β-Blockers | Probably unhelpful | Good evidence |
| Selected serotonin reuptake inhibitor antidepressants | Debatable effect | Moderate evidence |
| Midodrine | Probably helpful | Good evidence |
| Fludrocortisone | Debatable effect | Weak evidence |
| CARDIAC PACEMAKERS | ||
| Cardiac pacemakers: routine use | Probably unhelpful | Good evidence |
| Cardiac pacemakers: selected use in refractory cases with asystole | Debatable effect | Weak evidence |
From Kuriachan V, Sheldon RS, Platonov M: Evidence-based treatment for vasovagal syncope, Heart Rhythm 5:1609–1614, 2008.
Considerable evidence supports the use of physical counterpressure maneuvers (PCM). During PCM, the presyncopal patient does isometric contractions of either the legs (by leg crossing) or the arms and hands (by pulling apart gripped hands), or squats. The Physical Counterpressure Manoeuvres Trial (PC Trial) was a randomized, controlled trial comparing conventional therapy (fluid and salt intake, counseling, avoidance) against conventional therapy augmented by one of three maneuvers in 208 patients with vasovagal syncope.87 After 18 months of follow-up, PCM provided a significant 36% relative risk reduction. However, 35% of patients had insufficient prodromes to perform the techniques. These techniques should form the evidence-based core of the early, conservative care of vasovagal syncope.1,2,8
β-Blockers
At least five randomized clinical trials of β-adrenergic blockers for the prevention of syncope have been published (see Table 48-4).1,2 On the whole, the results were negative. One small, early study of atenolol showed positive results.88 The Prevention of Syncope Trial (POST) was a pivotal randomized, placebo-controlled, double-blind trial assessing the effects of metoprolol in vasovagal syncope over a 1-year treatment period.89 Metoprolol provided no benefit, with nearly identical outcome rates in both study arms.
Fludrocortisone
Fludrocortisone is a corticosteroid with mainly mineralocorticoid activity that results in sodium and water retention and potassium excretion, which would increase blood volume.1,2 A randomized, double-blind, placebo-controlled study found more symptoms in children treated with fludrocortisone compared with the group treated with placebo (see Table 48-4).90 The second Prevention of Syncope Trial (POST II), a multi-national, randomized, double-blind, controlled clinical trial assessing the effectiveness of fludrocortisone in adults with recurrent vasovagal syncope ended in July 2011. Results are pending.
α-Agonists
Midodrine is the sole α-adrenergic agonist with evidence of effectiveness. It is peripherally active, as is its metabolite. It alleviates the reduction in peripheral sympathetic neural outflow, which is responsible for venous pooling and vasodepression central to vasovagal syncope.91,92 A randomized, placebo-controlled, single-pill trial of midodrine to prevent syncope on TTT was positive (see Table 48-4).93 Two randomized, open-label trials showed positive results and prevention of syncope for up to 22 months.94 A randomized, placebo-controlled, double-blind, crossover study reported that midodrine significantly increased the number of symptom-free days in 16 highly symptomatic patients.95 However, the study period was only 28 days. The drug is well tolerated, albeit requiring frequent dosing. Side effects included supine hypertension, nausea, scalp paresthesias, piloerection, and rash but were dose related and easily reversible. Midodrine should not be used in patients with hypertension or heart failure.1,2
Serotonin Reuptake Inhibitors
The important role of serotonin in the regulation of heart rate and blood pressure led to speculation that fluctuation in central serotonin levels may contribute to vasovagal syncope. Indeed, a randomized, double-blind, placebo-controlled study of 68 consecutive patients who had not responded to other treatments reported positive outcomes.96 Disappointingly, a recent second randomized, placebo-controlled study of 96 patients found fluoxetine, propranolol, and placebo to be equal.97 Therefore evidence for the use of these drugs with vasovagal syncope is conflicting, and the drugs are not currently recommended.1,2
Permanent Pacemakers
Three open-label, historically controlled trials and three open-label, randomized clinical trials of permanent pacemakers in patients with frequent vasovagal syncope reported an approximate 90% reduction in the likelihood of a recurrence of syncope in paced patients (see Table 48-4). However, a placebo effect from the pacemaker could not be excluded. The Second Vasovagal Pacemaker Study (VPS II) was an international, placebo-controlled, double-blind, multi-center trial.98 Patients with active pacemakers had no significant benefit from pacing; this was confirmed by a smaller second study, the Vasovagal Syncope and Pacing Trial (SYNPACE).99
One unresolved question is whether the subset of patients with vasovagal syncope who have asystolic pauses during spontaneous syncope might benefit from pacing. Accordingly, the ISSUE investigators are conducting ISSUE 3, a multi-center, placebo-controlled, prospective, double-blind, randomized study.100 Patients with asystolic pauses detected by an ILR will have a pacemaker implanted with double-blind randomization to active pacing or sensing only; the design is similar to that of the VPS II study.1,2,101,102
Carotid Sinus Syncope
Carotid sinus syncope is a syndrome of syncope associated with a consistent clinical history, carotid sinus hypersensitivity, and the absence of other potential causes of syncope.4,98 Historical features that suggest the diagnosis are syncope or presyncope occurring with carotid sinus stimulation that reproduces clinical symptoms, or fortuitous Holter monitoring or other documentation of asystole during syncope following maneuvers that could stimulate the carotid sinus. The incidence of carotid sinus syncope is low and may be approximately 35 per 1 million per year. Carotid sinus syncope occurs in older patients, mainly in men. It tends to occur abruptly, with little prodrome, and only half the patients may recognize a precipitating event. These most typically include wearing tight collars, shaving, head turning (as in looking back to reverse a car), coughing, heavy lifting, and looking up.
Randomized Studies of Pacing
Recent prospective, randomized trials have examined outcomes on the basis of presence of pacing and mode.4,101 One prospective, randomized trial reaffirmed the important role of permanent pacing for carotid sinus syncope.103 Sixty patients with carotid sinus syncope were randomized to pacing or nonpacing therapy. During a follow-up of approximately 3 years, syncope recurred in 51% patients of the nonpaced group and in 9% of the paced group.
Pacing of patients with carotid sinus syndrome has been associated with a reduction in falls; furthermore, among patients with unexplained and recurrent falls, carotid sinus hypersensitivity is an important risk factor. The Syncope and Falls in the Elderly Pacing and Carotid Sinus Evaluation (SAFE PACE) trial was designed to determine whether cardiac pacing reduces falls in older patients with unexplained falls and a cardio-inhibitory response to CSM.104 Patients were randomized to receive a dual-chamber pacemaker with rate-drop responsiveness or no intervention. Patients who received a pacemaker had a highly significant 58% reduction in falls and a 40% reduction in syncope. Although these results suggest that many unexplained falls in older adults are caused by carotid sinus syncope and that they can be prevented with pacing, this was an open-label trial. The SAFE PACE II study randomized 141 older patients with unexplained falls and cardio-inhibitory carotid sinus hypersensitivity to receive a rate-drop-responsive, dual-chamber pacemaker or an ILR.105 No significant differences in falls between the paced and the loop recorder group were observed. These results are at odds with the findings in SAFE PACE, possibly because of differences in patient population or because of limited power.
Only one double-blind, placebo-controlled, crossover study of pacing in patients with recurrent, unexplained falls and carotid sinus hypersensitivity has been published. All 34 participants received a dual-chamber pacemaker with a rate-drop response programmer and were randomized to the DDD/RDR mode (on) versus the ODO mode (off); after 6 months, patients crossed over to the opposite mode. The relative risk of falling with the pacemaker on versus off was not statistically significant between the groups.106
Standardized Approaches in the Emergency Department
Epidemiologic findings of patients with syncope from EDs in Australia, Europe, the United Kingdom, and the United States report that the average patient age is 61 years and that 45% are men. The final diagnoses include vasovagal syncope in 43% of patients, cardiac in 14%, and other (including undiagnosed syncope) in 43%. Decision making in ED syncope assessment is often driven by risk assessment rather than by a precise diagnosis. Risk assessment decisions are aimed at two timelines for outcomes: (1) poor outcomes in the first 7 to 30 days, which mandate admission, and (2) poor outcomes beyond 30 days, which mandate early specialist assessment.6
Events After Presentation
Patients with syncope who present to the ED have a significant risk during follow-up, although this risk varies widely depending on the etiology.6 The composite estimate of outcomes is that approximately 0.7% of patients die in the next 7 to 30 days, and approximately 10% of patients die within 1 year. Nonfatal severe outcomes are generally defined as a significant new diagnosis, clinical deterioration, serious injury with recurrence, or a significant therapeutic intervention. An average of 7.5% of syncope ED visits have a nonfatal severe outcome while these patients are in the ED, and another 4.5% have a nonfatal severe outcome in the next 7 to 30 days.6 Only half of the nonfatal severe outcomes have cardiovascular causes. Therefore only a minority of patients will benefit from urgent assessment and treatment outside the ED, and only half of these are for cardiovascular disorders. In the case of some patients, the syncopal event may have little to do with overall outcome because many of the risk factors seem to identify older patients with high morbidity rates.
Risk Factors for Nonfatal Severe Outcomes
The most commonly identified risk factors for severe outcomes include an abnormal ECG, a history of cardiovascular disease, and hypotension; others include age greater than 60 years, syncope without prodrome, syncope occurring while supine and while exercising, hypertension, dyspnea, and anemia.15–23,27,33,107–111 The Canadian Cardiovascular Society defined major risk factors as those independently identified in more than one report and minor risk factors as those identified in only one report (Table 48-5). Patients with major risk factors should have an urgent cardiac specialist assessment within 2 weeks.6
Table 48-5 Risk Factors for Short-Term Outcomes According to the Canadian Cardiovascular Society
| Risk Factor | Variable |
| MAJOR (URGENT NEED FOR CARDIAC ASSESSMENT) | |
| Abnormal electrocardiogram | Any bradyarrhythmia, tachyarrhythmia, or conduction disease |
| New ischemia or old infarct | |
| History of cardiac disease | Ischemic, arrhythmic, obstructive, valvular |
| Hypotension | Systolic blood pressure <90 mm Hg |
| Heart failure | Either past history or current state |
| MINOR (POSSIBLE NEED FOR URGENT CARDIAC ASSESSMENT) | |
| Age | >60 years |
| Dyspnea | |
| Anemia | Hematocrit <0.30 |
| Hypertension | |
| Cerebrovascular disease | |
| Family history of early sudden cardiac death | Age <50 years |
| Specific situations | Syncope while supine, during exercise, or with no prodromal symptoms |
Major risk factors were independently derived in more than one study; minor risk factors were derived in only one study. Patients with syncope should have an urgent cardiac assessment in the presence of a single major risk factor.
From Sheldon RS, Morillo CA, Krahn AD, et al: Standardized approaches to the investigation of syncope: A position paper of the Canadian Cardiovascular Society, Can J Cardiol 27(2):246–253, 2011.
Emergency Department Risk Rules
On the whole, the ED diagnostic procedure for syncope has a sensitivity of 95% for early adverse outcomes and more than 99% for mortality.13,17,21,27,33,107,108,112–114 This is accompanied by specificities in the range of 30% to 60%. Therefore the key priority of a decision rule would be to maintain sensitivity and increase specificity. A common feature of the ED risk stratification rules is that to achieve 95% sensitivity for an early adverse event, the presence of any single risk factor moves the patient from the low-risk group. Standardized scores have been developed in Europe, the United Kingdom, and the United States. Although the scores predict outcome, they do not necessarily identify a treatable cause. The two studies with the best methodology and external validation are the San Francisco Syncope Rule and the Osservatorio Epidemiologico della Sincope nel Lazio (OESIL) score.27,111 Both were thoroughly developed, starting with epidemiologic risk factors and proceeding through validation studies. Very recently, the Risk Stratification of Syncope in the Emergency Department (ROSE) study reported the development and validation of a score (based on the BRACES mnemonic) for identifying high-risk patients with syncope (Table 48-6).33
| B | BNP level ≥300 pg/mL |
| Bradycardia ≤50 in ED or prehospital setting | |
| R | Rectal examination showing fecal occult blood (if suspicion of gastrointestinal bleeding) |
| A | Anemia (hemoglobin ≤90 g/L) |
| C | Chest pain associated with syncope |
| E | ECG showing Q wave (not in lead III) |
| S | Saturation ≤94% on room air |
A patient should be considered high risk and admitted if any of the seven criteria in the ROSE (Risk Stratification of Syncope in the Emergency Department) rule are present.
BNP, B-type natriuretic peptide; ED, emergency department; ECG, electrocardiogram.
From Reed MJ, Newby DE, Coull AJ, et al: The ROSE (Risk Stratification of Syncope in the Emergency Department) study, J Am Coll Cardiol 55:713–721, 2010.
The OESIL group identified four risk factors for 1-year mortality: (1) age greater than 65 years, (2) cardiovascular disease, (3) syncope without prodrome, and (4) an abnormal ECG.111 The risk score resulted in 0 to 4 points, with 1-year mortality rates ranging from 0.8% to 57%. This was partly validated in a small study by British investigators, who found 3-month serious outcomes to range from 0% to 37%, with deaths accounting for half the outcomes. Martin et al identified four similarly weighted independent risk factors (age greater than 45 years, history of heart failure, history of ventricular arrhythmias, and an abnormal ECG) that predicted 1-year death rates ranging from 2% to 30%.115 Therefore the factors that predict 1-year mortality are advanced age, cardiovascular disorders, and an abnormal ECG.
The San Francisco Syncope Rule (SFSR) identified independent predictors of serious morbidity and mortality within 7 days of presentation to the ED.27 High-risk patients could be identified by the presence of any one of five factors: (1) dyspnea, (2) hypotension, (3) congestive heart failure, (4) abnormal ECG, and (5) anemia. Although the SFSR was reported to have 96% sensitivity and 62% specificity, subsequent validation studies reported reduced accuracy. Admission rates with the SFSR would be increased with no gain in sensitivity when compared with the actual decision made by the ED physician.6
Impact of Guidelines
Do the ESC guidelines improve care? In 2001 and 2007, the American College of Emergency Physicians issued guidelines for the ED management of patients with syncope. A study that used high-risk features as a tool for identifying cardiogenic syncope had very high sensitivity and specificity statistics and, if implemented, would have reduced admissions by 29%, whereas the use of medium-risk features decreased specificity and increased admissions. The ESC guidelines recommend admission for significant heart disease, abnormal ECG, syncope during exercise or while supine, severe injury, family history of SCD, preceding palpitations, frequent episodes or high suspicion of cardiac syncope, arrhythmias, cardiopulmonary or neurologic disorders, or pacer implantation. McCarthy et al retrospectively assessed a pathway developed on the basis of these guidelines and found that 9.6% of the admissions could have been avoided if the pathway was used.14 Del Greco et al reported that the 2001 guidelines had no apparent effect on length of stay, extent of testing, or cost of hospitalization.116,117 Although ED syncope decision rules may have prognostic value, there is no compelling evidence that they improve diagnostic accuracy or reduce costs, and they may substantially increase costs.6
Syncope Management Units
The generally benign short-term outcome of patients with syncope raises the possibility of an entirely outpatient assessment of patients who do not have a declared outcome in the ED.6 The term syncope unit refers to any organized approach to investigation or, more narrowly in North America, as a geographically contained unit for assessing syncope. The ESC 2009 guidelines recommend the establishment of formal syncope units, either virtual or geographically contained, staffed by syncope experts, with easy access to all referring physicians.4
Kenny et al first introduced the concept of a dedicated syncope clinic or unit in a study of 65 consecutive older patients. A causal diagnosis was reached in 92% of patients. Subsequently, three small observational studies showed that with older patients, dedicated units achieved a diagnosis in almost all.117,118 However, none of these studies was controlled, and many diagnoses simply turned out to be accurate clinical judgments. In one study, a syncope and falls day clinic for older patients achieved a dramatic estimated reduction in bed occupancy (35% vs. 97% of expected) and length of stay (2.7 vs. 10.9 days expected).
Brignole et al compared six Italian hospitals that had an organized syncope unit with six matched hospitals not offering this service.119 A weak trend to fewer admissions and tests performed in the syncope unit hospitals was observed, but only 11% of eligible syncope patients had been referred to the unit. Ammirati et al reviewed 102 consecutive patients referred to their syncope unit as either outpatients or during hospitalization in a retrospective observational study.120 The syncope unit appeared to increase the diagnostic yield from 75% to 82% and reduced hospital costs by 85%, largely by eliminating unnecessary tests.
The Syncope Evaluation in the Emergency Department Study (SEEDS) was the only randomized study evaluating the efficiency and accuracy of the investigation of syncope with a dedicated syncope unit.28 SEEDS randomized 103 patients with intermediate risk for syncope to a syncope unit evaluation compared with a standard care approach. The unit provided 6 hours of ECG monitoring, echocardiography, an early TTT, and an arrhythmia consult. The diagnostic yield was higher in the syncope unit arm (67% vs. 10%), mostly because of vasovagal syncope incidence. Admission rates were lower in the syncope unit group (43% vs. 98% in the control group). No differences in total mortality or syncope recurrence were noted. Formal syncope units may increase the diagnostic yield and prevent unnecessary admissions and testing. This may be explained by advanced access to specialist assessment and related testing.
Syncope Investigation Protocols in the Hospital
Noting the limited impact of published guidelines, Brignole et al used the ESC 2001 guidelines to develop software with specific prompting tools and compared its effectiveness to conventional unstructured approaches.55 The Evaluation of Guidelines in Syncope Study 2 (EGSYS-2) was a parallel-arm, non-randomized comparison of 745 patients with syncope that showed an improved diagnostic yield (95% vs. 80%), a reduced admission rate (39% vs. 47%), and reduced costs. Later, it was validated in 541 patients in 11 large hospitals. Use of the software led to adherence to a guideline-based approach in 86% of patients and yielded a diagnosis in 98% of cases. Half of the diagnoses were initially obtained after clinical assessment and ECG, with limited and specified testing (1.9 tests per patient) yielding the remainder of the diagnoses. It is important to realize that, by design, the algorithm should have provided 100% diagnostic yield (whether correct or not), and a “syncope expert” was available by telephone to provide advice.
Similarly, Farwell and Sulke used a syncope diagnostic protocol at a single large hospital and compared the outcomes in 421 patients with those in 660 historic controls.79 The diagnostic yield increased from 71% to 78%, as did appropriate testing such as TTT and monitoring. However, very poor adherence to the protocol led to many more hospital admissions than recommended, and irrelevant testing such as brain imaging persisted. This led to unexpected and dramatic increases in costs and bed occupancy. Finally, Sarasin et al used a systematic investigation strategy that featured baseline assessment with ECG and limited laboratory testing in 611 patients.112 This simple initial stage led to a diagnosis in 69% of patients, with targeted testing in an additional 7%. Extensive testing was used only in the remaining 155 patients.
What lessons can be drawn from these studies? Algorithmic testing seems to be effective but probably will not work if it is complicated and not supported by expert advice. However, coupled with implementation tools, it improves the diagnostic yield and may reduce costs. The most important features of algorithmic testing may be facilitated access to specialist assessment and an online prompting tool.6
Key References
Berecki-Gisolf J, Sheldon RS. Indications for pacing in neurally mediated syncope syndromes. Ellenbogen, Wilkoff B, Kay CN, Lau CP. Clinical cardiac pacing and defibrillation, ed 4, Philadelphia: Elsevier, 2010.
Brignole M. Diagnosis and treatment of syncope. Heart. 2007;93:130-136.
Kuriachan V, Sheldon RS, Platonov M. Evidence-based treatment for vasovagal syncope. Heart Rhythm. 2008;5:1609-1614.
Linzer M, Yang EH, Estes NA, et al. Diagnosing syncope. Part 1: Value of history, physical examination, and electrocardiography. Clinical Efficacy Assessment Project of the American College of Physicians. Ann Intern Med. 1997;126:989-996.
Low PA, Singer W. Management of neurogenic orthostatic hypotension: An update. Lancet Neurol. 2008;7:451-458.
Moya A, Sutton R, Ammirati F, et al. Guidelines for the diagnosis and management of syncope (version 2009): The Task Force for the Diagnosis and Management of Syncope of the European Society of Cardiology (ESC). Eur Heart J. 2009;30:2631-2671.
Parry SW, Tan MP. An approach to the evaluation and management of syncope in adults. BMJ. 2010;340:c880.
Sheldon R. Tilt testing for syncope: A reappraisal. Curr Opin Cardiol. 2005;20:38-41.
Sheldon RS, Morillo CA, Krahn AD, et al. Standardized approaches to the investigation of syncope: A position paper of the Canadian Cardiovascular Society. Can J Cardiol. 2011;27(2):246-253.
Sud S, Massel D, Klein GJ, et al. The expectation effect and cardiac pacing for refractory vasovagal syncope. Am J Med. 2007;120:54-62.
van Dijk JG, Thijs RD, Benditt DG, Wieling W. A guide to disorders causing transient loss of consciousness: Focus on syncope. Nat Rev Neurol. 2009;5:438-448.
van Dijk N, Quartieri F, Blanc JJ, et al. Effectiveness of physical counterpressure maneuvers in preventing vasovagal syncope: The Physical Counterpressure Manoeuvres Trial (PC-Trial). J Am Coll Cardiol. 2006;48:1652-1657.
Wieling W, Colman N, Krediet CT, Freeman R. Nonpharmacological treatment of reflex syncope. Clin Auton Res. 2004;14(Suppl 1):62-70.
Wieling W, Krediet CT, van Dijk N, et al. Initial orthostatic hypotension: Review of a forgotten condition. Clin Sci (Lond). 2007;112:157-165.
Wieling W, Thijs RD, van Dijk N, et al. Symptoms and signs of syncope: A review of the link between physiology and clinical clues. Brain. 2009;132:2630-2642.
1 Brignole M. Diagnosis and treatment of syncope. Heart. 2007;93:130-136.
2 Kuriachan V, Sheldon RS, Platonov M. Evidence-based treatment for vasovagal syncope. Heart Rhythm. 2008;5:1609-1614.
3 Low PA, Singer W. Management of neurogenic orthostatic hypotension: An update. Lancet Neurol. 2008;7:451-458.
4 Moya A, Sutton R, Ammirati F, et al. Guidelines for the diagnosis and management of syncope (version 2009): The Task Force for the Diagnosis and Management of Syncope of the European Society of Cardiology (ESC). Eur Heart J. 2009;30:2631-2671.
5 Parry SW, Tan MP. An approach to the evaluation and management of syncope in adults. BMJ. 2010;340:c880.
6 Sheldon RS, Morillo CA, Krahn AD, et al. Standardized approaches to the investigation of syncope: A position paper of the Canadian Cardiovascular Society. Can J Cardiol. 2011;27(2):246-253.
7 van Dijk JG, Thijs RD, Benditt DG, Wieling W. A guide to disorders causing transient loss of consciousness: Focus on syncope. Nat Rev Neurol. 2009;5:438-448.
8 Wieling W, Colman N, Krediet CT, Freeman R. Nonpharmacological treatment of reflex syncope. Clin Auton Res. 2004;14(Suppl 1):62-70.
9 Wieling W, Thijs RD, van Dijk N, et al. Symptoms and signs of syncope: A review of the link between physiology and clinical clues. Brain. 2009;132:2630-2642.
10 Serletis A, Rose S, Sheldon AG, Sheldon RS. Vasovagal syncope in medical students and their first-degree relatives. Eur Heart J. 2006;27:1965-1970.
11 McDermott D, Quinn J. Response to “failure to validate the San Francisco Syncope Rule in an independent emergency department population”. Ann Emerg Med. 2009;53:693. author reply 693–693; author reply 694
12 Olde Nordkamp LR, van Dijk N, Ganzeboom KS, et al. Syncope prevalence in the ED compared to general practice and population: A strong selection process. Am J Emerg Med. 2009;27:271-279.
13 Bonney ME, Reed MJ, Gray AJ. The Prediction of Risk In Syncope using ECG characteristics (PRISE) pilot study: Can heart rate variability be used to predict risk in patients presenting to the emergency department with syncope? Emerg Med J. 2009;26:32-36.
14 McCarthy F, McMahon CG, Geary U, et al. Management of syncope in the emergency department: A single hospital observational case series based on the application of European Society of Cardiology Guidelines. Europace. 2009;11:216-224.
15 Schladenhaufen R, Feilinger S, Pollack M, et al. Application of San Francisco Syncope Rule in elderly ED patients. Am J Emerg Med. 2008;26:773-778.
16 Quinn J, McDermott D, Kramer N, et al. Death after emergency department visits for syncope: How common and can it be predicted? Ann Emerg Med. 2008;51:585-590.
17 Del Rosso A, Ungar A, Maggi R, et al. Clinical predictors of cardiac syncope at initial evaluation in patients referred urgently to a general hospital: The EGSYS score. Heart. 2008;94:1620-1626.
18 Birnbaum A, Esses D, Bijur P, et al. Failure to validate the San Francisco Syncope Rule in an independent emergency department population. Ann Emerg Med. 2008;52:151-159.
19 Grossman SA, Fischer C, Lipsitz LA, et al. Predicting adverse outcomes in syncope. J Emerg Med. 2007;33:233-239.
20 Sun BC, Hoffman JR, Mangione CM, Mower WR. Older age predicts short-term, serious events after syncope. J Am Geriatr Soc. 2007;55:907-912.
21 Reed MJ, Newby DE, Coull AJ, et al. The Risk stratification Of Syncope in the Emergency department (ROSE) pilot study: A comparison of existing syncope guidelines. Emerg Med J. 2007;24:270-275.
22 Sun BC, Mangione CM, Merchant G, et al. External validation of the San Francisco Syncope Rule. Ann Emerg Med. 2007;49:420-427. 427.e1-e4
23 Quinn J, McDermott D, Stiell I, et al. Prospective validation of the San Francisco Syncope Rule to predict patients with serious outcomes. Ann Emerg Med. 2006;47:448-454.
24 Lang ES. The San Francisco Syncope Rule was useful for stratifying risk in emergency department patients with syncope. Evid Based Med. 2006;11:186.
25 Sun BC, Emond JA, Camargo CAJ. Characteristics and admission patterns of patients presenting with syncope to U.S. emergency departments, 1992–2000. Acad Emerg Med. 2004;11:1029-1034.
26 Morag RM, Murdock LF, Khan ZA, et al. Do patients with a negative emergency department evaluation for syncope require hospital admission? J Emerg Med. 2004;27:339-343.
27 Quinn JV, Stiell IG, McDermott DA, et al. Derivation of the San Francisco Syncope Rule to predict patients with short-term serious outcomes. Ann Emerg Med. 2004;43:224-232.
28 Shen WK, Decker WW, Smars PA, et al. Syncope Evaluation in the Emergency Department Study (SEEDS): A multidisciplinary approach to syncope management. Circulation. 2004;110:3636-3645.
29 Grossman SA, Van Epp S, Arnold R, et al. The value of cardiac enzymes in elderly patients presenting to the emergency department with syncope. J Gerontol Biol Sci Med Sci. 2003;58:1055-1058.
30 Crane SD. Risk stratification of patients with syncope in an accident and emergency department. Emerg Med J. 2002;19:23-27.
31 Cunningham R, Mikhail MG. Management of patients with syncope and cardiac arrhythmias in an emergency department observation unit. Emerg Med Clin North Am. 2001;19:105-121. vii
32 Thakore SB, Crombie I, Johnston M. The management of syncope in a British emergency department compared to recent American guidelines. Scott Med J. 1999;44:155-157.
33 Reed MJ, Newby DE, Coull AJ, et al. The ROSE (risk stratification of syncope in the emergency department) study. J Am Coll Cardiol. 2010;55:713-721.
34 Thiruganasambandamoorthy V, Hess EP, Alreesi A, et al. External validation of the San Francisco Syncope Rule in the Canadian setting. Ann Emerg Med. 2010;55:464-472.
35 Wieling W, Krediet CT, van Dijk N, et al. Initial orthostatic hypotension: Review of a forgotten condition. Clin Sci (Lond). 2007;112:157-165.
36 Leitch JW, Klein GJ, Yee R, et al. Syncope associated with supraventricular tachycardia. An expression of tachycardia rate or vasomotor response? Circulation. 1992;85:1064-1071.
37 Brignole M, Gianfranchi L, Menozzi C, et al. Role of autonomic reflexes in syncope associated with paroxysmal atrial fibrillation. J Am Coll Cardiol. 1993;22:1123-1129.
38 Alboni P, Menozzi C, Brignole M, et al. An abnormal neural reflex plays a role in causing syncope in sinus bradycardia. J Am Coll Cardiol. 1993;22:1130-1134.
39 Marti-Almor J, Cladellas M, Bazan V, et al. Novel predictors of progression of atrioventricular block in patients with chronic bifascicular block. Rev Esp Cardiol. 2010;63:400-408.
40 Israel CW. Syncope and bifascicular block: Who needs a pacemaker? Rev Esp Cardiol. 2010;63:385-386.
41 Tabrizi F, Rosenqvist M, Bergfeldt L, Englund A. Time relation between a syncopal event and documentation of atrioventricular block in patients with bifascicular block: Clinical implications. Cardiology. 2007;108:138-143.
42 Tabrizi F, Rosenqvist M, Bergfeldt L, Englund A. Long-term prognosis in patients with bifascicular block–the predictive value of noninvasive and invasive assessment. J Intern Med. 2006;260:31-38.
43 Jeong JH, Kim JH, Park YH, et al. Incidence of and risk factors for bundle branch block in adults older than 40 years. Korean J Intern Med. 2004;19:171-178.
44 van Dijk N, Boer KR, Colman N, et al. High diagnostic yield and accuracy of history, physical examination, and ECG in patients with transient loss of consciousness in FAST: The Fainting Assessment study. J Cardiovasc Electrophysiol. 2008;19:48-55.
45 Sheldon R, Hersi A, Ritchie D, et al. Syncope and structural heart disease: Historical criteria for vasovagal syncope and ventricular tachycardia. J Cardiovasc Electrophysiol. 2010;21:1358-1364.
46 Sheldon R, Rose S, Connolly S, et al. Diagnostic criteria for vasovagal syncope based on a quantitative history. Eur Heart J. 2006;27:344-350.
47 Sheldon R, Rose S, Ritchie D, et al. Historical criteria that distinguish syncope from seizures. J Am Coll Cardiol. 2002;40:142-148.
48 Romme JJ, van Dijk N, Boer KR, et al. Diagnosing vasovagal syncope based on quantitative history-taking: validation of the Calgary Syncope Symptom Score. Eur Heart J. 2009;30:2888-2896.
49 Raj SR, Rose S, Ritchie D, Sheldon RS. The Second Prevention of Syncope Trial (POST II)—a randomized clinical trial of fludrocortisone for the prevention of neurally mediated syncope: Rationale and study design. Am Heart J. 2006;151:1186.e11-1186.e17.
50 Sumner GL, Rose MS, Koshman ML, et al. Recent history of vasovagal syncope in a young, referral-based population is a stronger predictor of recurrent syncope than lifetime syncope burden. J Cardiovasc Electrophysiol. 2010;21:1375-1380.
51 Sheldon RS, Sheldon AG, Serletis A, et al. Worsening of symptoms before presentation with vasovagal syncope. J Cardiovasc Electrophysiol. 2007;18:954-959.
52 Sheldon R, Rose S, Koshman ML. Comparison of patients with syncope of unknown cause having negative or positive tilt-table tests. Am J Cardiol. 1997;80:581-585.
53 Malik P, Koshman ML, Sheldon R. Timing of first recurrence of syncope predicts syncopal frequency after a positive tilt table test result. J Am Coll Cardiol. 1997;29:1284-1289.
54 Sheldon R, Rose S, Flanagan P, et al. Risk factors for syncope recurrence after a positive tilt-table test in patients with syncope. Circulation. 1996;93:973-981.
55 Brignole M, Menozzi C, Bartoletti A, et al. A new management of syncope: Prospective systematic guideline-based evaluation of patients referred urgently to general hospitals. Eur Heart J. 2006;27:76-82.
56 Martin GJ, Adams SL, Martin HG, et al. Prospective evaluation of syncope. Ann Emerg Med. 1984;13:499-504.
57 Linzer M, Yang EH, Estes NA, et al. Diagnosing syncope. Part 1: Value of history, physical examination, and electrocardiography. Clinical Efficacy Assessment Project of the American College of Physicians. Ann Intern Med. 1997;126:989-996.
58 Mendu ML, McAvay G, Lampert R, et al. Yield of diagnostic tests in evaluating syncopal episodes in older patients. Arch Intern Med. 2009;169:1299-1305.
59 Delepine S, Prunier F, Leftheriotis G, et al. Comparison between isoproterenol and nitroglycerin sensitized head-upright tilt in patients with unexplained syncope and negative or positive passive head-up tilt response. Am J Cardiol. 2002;90:488-491.
60 el Bedawi KM, Hainsworth R. Combined head-up tilt and lower body suction: A test of orthostatic tolerance. Clin Auton Res. 1994;4:41-47.
61 Ermis C, Samniah N, Sakaguchi S, et al. Comparison of catecholamine response during tilt-table-induced vasovagal syncope in patients <35 to those >65 years of age. Am J Cardiol. 2004;93:225-227.
62 Kenny RA, Ingram A, Bayliss J, Sutton R. Head-up tilt: A useful test for investigating unexplained syncope. Lancet. 1986;1:1352-1355.
63 Mosqueda-Garcia R, Furlan R, Fernandez-Violante R, et al. Sympathetic and baroreceptor reflex function in neurally mediated syncope evoked by tilt. J Clin Invest. 1997;99:2736-2744.
64 Oraii S, Maleki M, Minooii M, Kafaii P. Comparing two different protocols for tilt table testing: sublingual glyceryl trinitrate versus isoprenaline infusion. Heart. 1999;81:603-605.
65 Sheldon R. Tilt testing for syncope: A reappraisal. Curr Opin Cardiol. 2005;20:38-41.
66 Sheldon R, Koshman ML. A randomized study of tilt test angle in patients with undiagnosed syncope. Can J Cardiol. 2001;17:1051-1057.
67 Sheldon R, Rose S, Koshman ML. Isoproterenol tilt-table testing in patients with syncope and structural heart disease. Am J Cardiol. 1996;78:700-703.
68 Brignole M, Vardas P, Hoffman E, et al. Indications for the use of diagnostic implantable and external ECG loop recorders. Europace. 2009;11:671-687.
69 Brignole M, Moya A, Menozzi C, et al. Proposed electrocardiographic classification of spontaneous syncope documented by an implantable loop recorder. Europace. 2005;7:14-18.
70 Brignole M, Sutton R, Menozzi C, et al. Early application of an implantable loop recorder allows effective specific therapy in patients with recurrent suspected neurally mediated syncope. Eur Heart J. 2006;27:1085-1092.
71 Brignole M, Sutton R, Wieling W, et al. Analysis of rhythm variation during spontaneous cardioinhibitory neurally-mediated syncope. Implications for RDR pacing optimization: An ISSUE 2 substudy. Europace. 2007;9:305-311.
72 Hoch JS, Rockx MA, Krahn AD. Using the net benefit regression framework to construct cost-effectiveness acceptability curves: An example using data from a trial of external loop recorders versus Holter monitoring for ambulatory monitoring of “community acquired” syncope. BMC Health Serv Res. 2006;6:68.
73 Krahn AD, Klein GJ, Yee R, et al. Cost implications of testing strategy in patients with syncope: Randomized assessment of syncope trial. J Am Coll Cardiol. 2003;42:495-501.
74 Krahn AD, Klein GJ, Yee R, Norris C. Final results from a pilot study with an implantable loop recorder to determine the etiology of syncope in patients with negative noninvasive and invasive testing. Am J Cardiol. 1998;82:117-119.
75 Krahn AD, Klein GJ, Yee R, et al. Use of an extended monitoring strategy in patients with problematic syncope. Reveal Investigators. Circulation. 1999;99:406-410.
76 Moya A, Brignole M, Sutton R, et al. Reproducibility of electrocardiographic findings in patients with suspected reflex neurally-mediated syncope. Am J Cardiol. 2008;102:1518-1523.
77 Solano A, Menozzi C, Maggi R, et al. Incidence, diagnostic yield and safety of the implantable loop-recorder to detect the mechanism of syncope in patients with and without structural heart disease. Eur Heart J. 2004;25:1116-1119.
78 Sud S, Klein GJ, Skanes AC, et al. Predicting the cause of syncope from clinical history in patients undergoing prolonged monitoring. Heart Rhythm. 2009;6:238-243.
79 Farwell DJ, Sulke AN. Does the use of a syncope diagnostic protocol improve the investigation and management of syncope? Heart. 2004;90:52-58.
80 Linzer M, Gold DT, Pontinen M, et al. Recurrent syncope as a chronic disease: Preliminary validation of a disease-specific measure of functional impairment. J Gen Intern Med. 1994;9:181-186.
81 Rose MS, Koshman ML, Spreng S, Sheldon R. The relationship between health-related quality of life and frequency of spells in patients with syncope. J Clin Epidemiol. 2000;53:1209-1216.
82 Gammage MD. Impact of syncope on quality of life: Do we need another tool? Europace. 2009;11:1265-1266.
83 Rose MS, Koshman ML, Ritchie D, Sheldon R. The development and preliminary validation of a scale measuring the impact of syncope on quality of life. Europace. 2009;11:1369-1374.
84 van Dijk N, Sprangers MA, Boer KR, et al. Quality of life within one year following presentation after transient loss of consciousness. Am J Cardiol. 2007;100:672-676.
85 van Dijk N, Sprangers MA, Colman N, et al. Clinical factors associated with quality of life in patients with transient loss of consciousness. J Cardiovasc Electrophysiol. 2006;17:998-1003.
86 Sheldon RS, Amuah JE, Connolly SJ, et al. Design and use of a quantitative scale for measuring presyncope. J Cardiovasc Electrophysiol. 2009;20:888-893.
87 van Dijk N, Quartieri F, Blanc JJ, et al. Effectiveness of physical counterpressure maneuvers in preventing vasovagal syncope: The Physical Counterpressure Manoeuvres Trial (PC-Trial). J Am Coll Cardiol. 2006;48:1652-1657.
88 Mahanonda N, Bhuripanyo K, Kangkagate C, et al. Randomized double-blind, placebo-controlled trial of oral atenolol in patients with unexplained syncope and positive upright tilt table test results. Am Heart J. 1995;130:1250-1253.
89 Sheldon R, Connolly S, Rose S, et al. Prevention of Syncope Trial (POST): A randomized, placebo-controlled study of metoprolol in the prevention of vasovagal syncope. Circulation. 2006;113:1164-1170.
90 Salim MA, Di Sessa TG. Effectiveness of fludrocortisone and salt in preventing syncope recurrence in children: A double-blind, placebo-controlled, randomized trial. J Am Coll Cardiol. 2005;45:484-488.
91 Yamazaki R, Tsuchida K, Aihara H. Effects of alpha-adrenoceptor agonists on cardiac output and blood pressure in spinally anesthetized ganglion-blocked dogs. Arch Int Pharmacodyn Ther. 1988;295:80-93.
92 Yamazaki R, Tsuchida K, Aihara H. Effects of midodrine on experimentally induced postural hypotension and venous pooling in dogs. Res Commun Chem Pathol Pharmacol. 1987;58:323-337.
93 Kaufmann H, Saadia D, Voustianiouk A. Midodrine in neurally mediated syncope: A double-blind, randomized, crossover study. Ann Neurol. 2002;52:342-345.
94 Perez-Lugones A, Schweikert R, Pavia S, et al. Usefulness of midodrine in patients with severely symptomatic neurocardiogenic syncope: A randomized control study. J Cardiovasc Electrophysiol. 2001;12:935-938.
95 Ward CR, Gray JC, Gilroy JJ, Kenny RA. Midodrine: A role in the management of neurocardiogenic syncope. Heart. 1998;79:45-49.
96 Di Girolamo E, Di Iorio C, Sabatini P, et al. Effects of paroxetine hydrochloride, a selective serotonin reuptake inhibitor, on refractory vasovagal syncope: A randomized, double-blind, placebo-controlled study. J Am Coll Cardiol. 1999;33:1227-1230.
97 Theodorakis GN, Leftheriotis D, Livanis EG, et al. Fluoxetine vs. propranolol in the treatment of vasovagal syncope: A prospective, randomized, placebo-controlled study. Europace. 2006;8:193-198.
98 Connolly SJ, Sheldon R, Thorpe KE, et al. Pacemaker therapy for prevention of syncope in patients with recurrent severe vasovagal syncope: Second Vasovagal Pacemaker Study (VPS II): A randomized trial. J Am Med Assoc. 2003;289:2224-2229.
99 Raviele A, Giada F, Menozzi C, et al. A randomized, double-blind, placebo-controlled study of permanent cardiac pacing for the treatment of recurrent tilt-induced vasovagal syncope. The vasovagal syncope and pacing trial (SYNPACE). Eur Heart J. 2004;25:1741-1748.
100 Brignole M. International study on syncope of uncertain aetiology 3 (ISSUE 3): Pacemaker therapy for patients with asystolic neurally-mediated syncope: Rationale and study design. Europace. 2007;9:25-30.
101 Berecki-Gisolf J, Sheldon RS. Indications for pacing in neurally mediated syncope syndromes. Ellenbogen, Wilkoff B, Kay CN, Lau CP. Clinical cardiac pacing and defibrillation, ed 4, Philadelphia: Elsevier, 2010.
102 Sud S, Massel D, Klein GJ, et al. The expectation effect and cardiac pacing for refractory vasovagal syncope. Am J Med. 2007;120:54-62.
103 Brignole M, Menozzi C, Lolli G, et al. Long-term outcome of paced and nonpaced patients with severe carotid sinus syndrome. Am J Cardiol. 1992;69:1039-1043.
104 Kenny RA, Richardson DA, Steen N, et al. Carotid sinus syndrome: A modifiable risk factor for nonaccidental falls in older adults (SAFE PACE). J Am Coll Cardiol. 2001;38:1491-1496.
105 Ryan DJ, Nick S, Colette SM, Roseanne K. Carotid sinus syndrome, should we pace? A multicentre, randomised control trial (SAFEPACE 2). Heart. 2010;96:347-351.
106 Reference deleted in proofs
107 Meisel ZF, Pollack CV, Mechem CC, Pines JM. Derivation and internal validation of a rule to predict hospital admission in prehospital patients. Prehosp Emerg Care. 2008;12:314-319.
108 Costantino G, Perego F, Dipaola F, et al. Short- and long-term prognosis of syncope, risk factors, and role of hospital admission: Results from the STePS (Short-Term Prognosis of Syncope) study. J Am Coll Cardiol. 2008;51:276-283.
109 Bartoletti A, Fabiani P, Adriani P, et al. Hospital admission of patients referred to the emergency department for syncope: A single-hospital prospective study based on the application of the European Society of Cardiology Guidelines on syncope. Eur Heart J. 2006;27:83-88.
110 Hing R, Harris R. Relative utility of serum troponin and the OESIL score in syncope. Emerg Med Australas. 2005;17:31-38.
111 Colivicchi F, Ammirati F, Melina D, et al. Development and prospective validation of a risk stratification system for patients with syncope in the emergency department: The OESIL risk score. Eur Heart J. 2003;24:811-819.
112 Sarasin FP, Pruvot E, Louis-Simonet M, et al. Stepwise evaluation of syncope: A prospective population-based controlled study. Int J Cardiol. 2008;127:103-111.
113 Elesber AA, Decker WW, Smars PA, et al. Impact of the application of the American College of Emergency Physicians recommendations for the admission of patients with syncope on a retrospectively studied population presenting to the emergency department. Am Heart J. 2005;149:826-831.
114 Sarasin FP, Hanusa BH, Perneger T, et al. A risk score to predict arrhythmias in patients with unexplained syncope. Acad Emerg Med. 2003;10:1312-1317.
115 Martin TP, Hanusa BH, Kapoor WN. Risk stratification of patients with syncope. Ann Emerg Med. 1997;29:459-466.
116 Del Greco M, Cozzio S, Scillieri M, et al. Diagnostic pathway of syncope and analysis of the impact of guidelines in a district general hospital. The ECSIT study (epidemiology and costs of syncope in Trento). Ital Heart J. 2003;4:99-106.
117 Kenny RA, O’Shea D, Walker HF. Impact of a dedicated syncope and falls facility for older adults on emergency beds. Age Ageing. 2002;31:272-275.
118 Dey AB, Bexton RS, Tyman MM, et al. The impact of a dedicated “syncope and falls” clinic on pacing practice in northeastern England. Pacing Clin Electrophysiol. 1997;20:815-817.
119 Brignole M, Disertori M, Menozzi C, et al. Management of syncope referred urgently to general hospitals with and without syncope units. Europace. 2003;5:293-298.
120 Ammirati F, Colaceci R, Cesario A, et al. Management of syncope: Clinical and economic impact of a syncope unit. Europace. 2008;10:471-476.