Chapter 68 Surgical Indications in Spine Trauma
Instability
As defined by White and Panjabi1 nearly two decades ago, instability is the inability “of the spine under physiological loads to limit patterns of displacement so as not to damage or irritate the spinal cord or nerve roots and, in addition, to prevent incapacitating deformity or pain caused by structural changes.” Their description of instability implies concepts of immediate or delayed neural compromise, deformity, and/or pain in conjunction with activities of normal daily living.
Determining spinal instability is not all black or white but, rather, encompasses shades of gray. Many schemes for the classification of instability have been suggested. In general, instability may be acute or chronic. Acute instability may be further defined as overt versus limited (Box 68-1). Acute instability may represent a threat to neural elements, may function as a pain generator, or may lead to progressive deformity if left unattended. Chronic instability may be subdivided as glacial instability, in which deformity occurs slowly over the course of time, similar to the movement of a glacier, or as a dysfunctional segment motion, in which the involved joint shows abnormal motion. As opposed to glacial instability, dysfunctional segment motion does not lead to deformity but rather to a pain syndrome associated with dysfunctional joint movement.
BOX 68-1 Instability Categorization Scheme
From Benzel EC: Biomechanics of spine stabilization, New York, 2001, Thieme.
Overt Instability
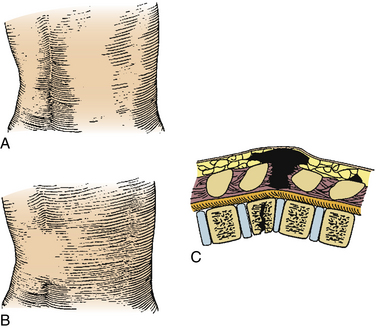
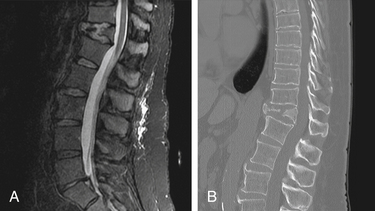
Overt instability is defined as the inability of the spine to support the weight of the torso. It is generally assumed when circumferential spinal integrity is lost. In effect, both anterior and posterior elements are compromised. Such injuries usually occur with larger force vectors or in patients with poor bone quality or biomechanical disadvantage (see later discussion). Compromise of the ventral elements can easily be demonstrated on plain film, CT, or MRI. Assessment of the dorsal elements, especially ligamentous structures, may be more challenging. Fat suppression or short tau inversion recovery (STIR) sequencing may illustrate ligamentous edema and suggest dorsal instability, but true disruption of the posterior tension band may be difficult to demonstrate.2 Flexion-extension films may be extremely dangerous in the face of overt instability. Disruption of the posterior ligamentous tension band may be noted on palpation of the affected area (Fig. 68-1).
Surgical Indications
Neural Compromise
Strong consideration should be given to patients with spinal cord, nerve root, and/or cauda equina compression with resulting neurologic deficits. Although still controversial, a growing body of evidence suggests that early decompression is the single most important predictor of neurologic recovery in spinal cord injury (SCI). Animal studies consistently show that neurologic recovery is enhanced by early spinal cord decompression.3,4 However, it is difficult to extrapolate the data for the effective application of decompression in the clinical setting from these animal models. To date, the clinical studies that have examined the role of surgical decompression in SCI are limited to class II and III evidence. One randomized controlled trial5 showed no benefit to early (<72 hours) decompression; however, several recent prospective series suggest that early decompression (<12 hours) can be performed safely and may improve neurologic outcomes.6,7 La Rosa et al.8 published a meta-analysis of the literature addressing the issue of early decompression and its role in acute SCI. They reviewed all published clinical studies and extracted data on 1687 patients. Patients were divided into three treatment groups: early decompression (<24 hours), delayed decompression (>24 hours), and conservative management. Statistically, early decompression resulted in better outcomes than either delayed decompression or conservative management. However, on homogeneity analysis, only data for patients with incomplete SCI who underwent early decompression were reliable. These studies concluded that early decompression can only be considered as a practice option. The Surgical Treatment of Acute Spinal Cord Injury Study (STASCIS)9 is a prospective, randomized controlled, multicenter trial that is currently in progress and seeks to determine the best timing of surgical decompression in SCI. In the authors’ opinion, surgery should be attempted in a medically stable patient as early as clinically feasible, often within 24 hours of admission.
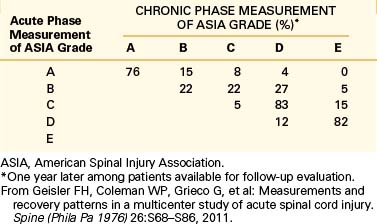
The American Spinal Injury Association impairment scale10 (ASIA), which is a modified Frankel classification,11 describes the completeness of an SCI. It has two main components: motor and sensory. The ASIA motor score of 0 to 5 is assigned for each muscle group innervated by spinal levels C5 to T1 and L2 to S1. This gives 10 levels on each side of the body, or a maximum possible score of 100. A sensory score of 0 to 2 is assigned for each dermatome from C2 to S4-5, using light touch and pinprick sensation. This gives 28 levels for a possible score of 56 on each side, or a maximum possible score of 112. Table 68-1 describes ASIA grading. The ASIA impairment scale has been shown to have great prognostic value, with chances of marked recovery more frequent in patients with better baseline scores. Table 68-2 shows the prognostic value of the ASIA impairment scale from the Sygen study group data.12
TABLE 68-1 American Spinal Injury Association Impairment Scale
| Class | Description |
|---|---|
| A | Complete: No motor or sensory function preserved in sacral segments S4-5 |
| B | Incomplete: Sensory but no motor function preserved below the neurologic level (includes sacral segments S4-5) |
| C | Incomplete: Motor function preserved below the neurologic level (more than half of key muscles below the neurologic level have a muscle grade <3) |
| D | Incomplete: Motor function preserved below the neurologic level (more than half of key muscles below the neurologic level have a muscle grade ~3) |
| E | Normal: Sensory and motor function normal |
From Frankel HL, Hancock DO, Hyslop G, et al: The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. I. Paraplegia 7:179–192, 1969.
Overt Instability
Columns
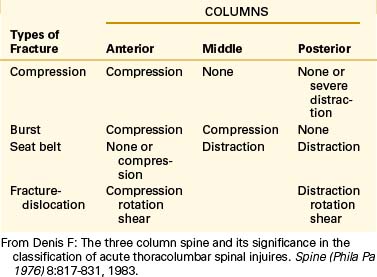
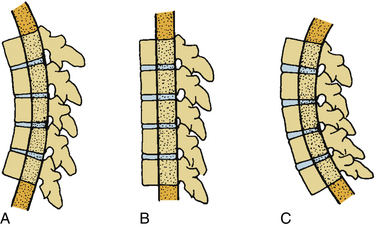
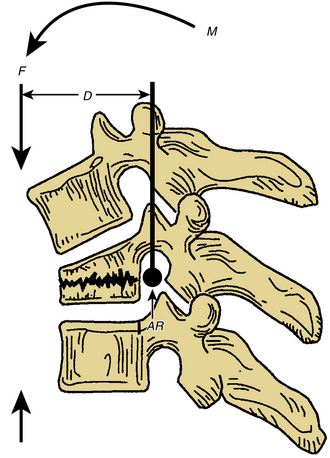
As previously described, overt instability refers to circumferential loss of spinal integrity. Compromise of only one column (either anterior or posterior) is considered limited instability only. The concept of “columns” is at the center of understanding spinal stability (Fig. 68-2) and dates back to the 1960s. In their seminal article, Kelly and Whitesides13 describe the concept of two columns as “one of solid bone and one composed of neural arches . . . Working together, these two columns support the body’s weight.” Later, Denis14 introduced the concept of a middle column, consisting of the posterior half of the vertebral body and disc and posterior longitudinal ligament. Depending on the pattern of column injury, he suggested four types of spinal fractures: compression, burst, seat belt–type, and fracture-dislocation (Table 68-3). The middle column suggested by Denis is interesting because it allows for specific assessment of the neutral axis. The neutral axis is the longitudinal axial weight-bearing zone about which spinal element distraction or compression does not significantly occur with flexion or extension (Fig. 68-3). As a rule, it is often suggested that compromise of two of the three Denis columns constitutes overt instability.

FIGURE 68-2 The “column” concepts of spinal stability. The concept described by Louis20 (left) assigns significance to the vertebral body and the facet joint complexes (lateral masses) on either side of the dorsal spine. Denis’s three-column concept (right) assigns significance to the region of the neutral axis and the integrity of the posterior vertebral body wall (the middle column). The two-column construct (left) relies on anatomically defined structures, the vertebral body (anterior column), and the posterior elements (posterior column). Louis’s three-column concept (left) similarly relies on anatomically defined structures.
(From Benzel EC: Biomechanics of spine surgery. Copyright © 2001 by the American Association of Neurological Surgeons, Rolling Meadows, IL.)
Mechanism of Injury Classification
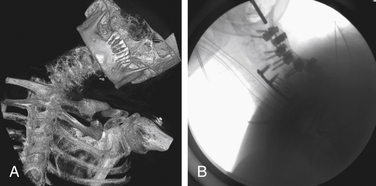
To date, the most commonly used classification scheme for traumatic spinal injuries is the Arbeitsgemeinschaft für Osteosynthesefragen system (AO) classification.15 This scheme categorizes fractures and other spinal injuries by type, groups, subgroups, and specifications. The AO classification is extensive and often difficult to remember in the clinical context if not used regularly. It provides comprehensive coverage of all possible fracture types and therefore is of the utmost importance in research. Nonetheless, knowledge of its basic types and groups is useful in a clinical context, as it provides a helpful template for understanding the mechanism of injury. This classification scheme categorizes fractures in three major mechanisms of injury. Type A fractures are ventral column injuries resulting from axial load, with or without flexion (Box 68-2 and Fig. 68-4). Type B fractures are distraction injuries in flexion or extension, resulting in compromise of ventral and dorsal elements (Box 68-3 and Fig. 68-5). Type C fractures are ventral and dorsal column injuries with translation and/or rotation (Box 68-4 and Fig. 68-6).
BOX 68-2 AO Classification: Type A Injuries: Vertebral Body Compression
|
|
AO, Arbeitsgemeinschaft für Osteosynthesefragen.
From Magerl F, Aebi M, Gertzbein SD, et al: A comprehensive classification of thoracic and lumbar injuries. Eur Spine J 3:184–201, 1994.
BOX 68-3 AO Classification: Type B Injuries: Anterior and Posterior Element Injury with Distraction
From Magerl F, Aebi M, Gertzbein SD, et al: A comprehensive classification of thoracic and lumbar injuries. Eur Spine J 3:184–201, 1994.
AO, Arbeitsgemeinschaft für Osteosynthesefragen.
BOX 68-4 AO Classification: Type C Injuries: Anterior and Posterior Element Injury with Rotation
From Magerl F, Aebi M, Gertzbein SD, et al: A comprehensive classification of thoracic and lumbar injuries. Eur Spine J 3:184–201, 1994.
AO, Arbeitsgemeinschaft für Osteosynthesefragen.
Type A injuries have compromise of only the anterior column (the posterior column is intact). These injuries are thus considered “stable” and usually do not require surgical stabilization. It is wisest to consider that they may have limited instability and may need to be observed for delayed glacial instability. Furthermore, patients with type A injuries requiring decompression of neural elements may require stabilization due to the “iatrogenic” disruption of the posterior column. In effect, these types of A injuries may “become” B injuries. Types B and C injuries are overtly unstable and should be considered for surgical stabilization.
Resting and Dynamic Radiologic Parameters
Trauma, especially to the ligamentous structures, may result in excessive angulation and/or translation deformity (Table 68-41), which may render the spine grossly unstable (overt instability) or lead to progressive deformity over time (glacial instability from acute limited instability). In the cervical spine, displacement of 3.5 mm and/or angulation of greater than 11 degrees on plain film, or translation of 3.5 mm on flexion-extension film, with rotational motion of greater than 20 degrees should be considered unstable. In the lumbar spine, displacement of 4.5 mm and/or angulation of greater than 22 degrees on plain film, or translation of 4.5 mm on flexion-extension film, with rotational motion of greater than 15 to 25 degrees (depending on the level) should be considered unstable. The thoracic spine is inherently “stabilized” by the rib cage. Therefore, lower values of translation and angulation are considered unstable.
| Resting | Dynamic | |
|---|---|---|
| Subaxial cervical spine | >3.5 mm displacement >11˚ angulation |
>3.5 mm translation >20˚ angulation |
| Thoracic spine | >2.5 mm displacement >5˚ angulation |
|
| Lumbar spine | >4.5 mm displacement >22˚ angulation |
>4.5 mm translation >15˚ L1-4 >20˚ L4-5 >25˚ L5-S1 |
From White AA, Panjabi MM: Clinical biomechanics of the spine, ed 2, Philadelphia, 1990, Lippincott.
Progressive Deformity from Limited Instability
As previously discussed, certain fractures with limited instability may be at risk for delayed progression (i.e., glacial instability), leading to deformity. In an attempt to predict the risk of such chronic instability, certain authors have devised point systems, such as the one suggested by White and Panjabi1 (Table 68-5), which assigns relative scores to the involved columns, the amount of resting and dynamic translation and angulation, the presence of neural injury, and other minor factors. In this system, a score of 5 or more is suggestive of overt instability, and patients with this score should be considered for surgical stabilization. A score of 2 to 4 is suggestive of limited instability, and such patients should be observed for delayed instability.
TABLE 68-5 Quantitation of Acute Instability for Subaxial Cervical, Thoracic, and Lumbar Injuries
| Condition | Points Assigned |
|---|---|
| Loss of integrity of anterior (and middle) column | 2 |
| Loss of integrity of posterior column(s) | 2 |
| Acute resting translational deformity | 2 |
| Acute resting angulation deformity | 2 |
| Acute dynamic translational deformity exaggeration | 2 |
| Acute dynamic angulation deformity exaggeration | 2 |
| Neural element injury | 3 |
| Acute disc narrowing at level of suspected pathology | 1 |
| Dangerous loading anticipated | 1 |
From White AA, Panjabi MM: Clinical biomechanics of the spine, ed 2, Philadelphia, 1990, Lippincott.
Acutely, burst fractures result from direct axial loading without ventral or dorsal angulation, as opposed to wedge compression fractures that occur as a result of axial loading with a ventrally or dorsally applied vector force, with a given perpendicular distance for the instantaneous axis of rotation (IAR) of that given vertebra. The force (F) at a given distance (D) from the IAR results in a given moment arm (M) (Fig. 68-7). The magnitude and speed of the applied moment arm determine the resulting bony and/or ligamentous deformation. The resulting deformity in the sagittal or coronal plane leads to either kyphosis or scoliosis, which increases the distance from the IAR, thus increasing the gravitational moment arm applied to that segment, leading to the progression of the deformity. Hence, “deformity begets deformity.”
Thoracolumbar Injury Classification and Severity Score
Management of thoracolumbar spinal trauma should be based on comprehensive evaluation of the clinical and radiographic information available at the time of initial assessment. The classification systems mentioned previously (Kelly, Denis, AO, radiologic parameters, and the White and Panjabi point system) have been developed to help physicians devise a treatment strategy. However, significant interobserver variability has been noted with these mechanistic classifications as injuries are classified by inferring unknown injury patterns rather than by a description of known or presenting injury.16 To address these limitations, a new classification scheme has been proposed by the Spine Trauma Study Group in 2005 that uses spinal injury morphology combined with the neurologic status of the patient and the critical importance of the posterior ligamentous structures in medical decision making.17 This new system, the Thoracolumbar Injury Classification and Severity Score (TLICS), assigns numeric values to each injury based on the categories of morphology of injury, integrity of the PLC, and neurologic involvement (Table 68-6).
TABLE 68-6 Thoracolumbar Injury Classification and Severity Score Scale
| Category | Points |
|---|---|
| Injury Morphology | |
| Compression | 1 |
| Burst | +1 |
| Translational/rotational | 3 |
| Distraction | 4 |
| Neurologic Status | |
| Intact | 0 |
| Nerve root | 2 |
| Cord, conus medullaris | |
| Incomplete | 3 |
| Complete | 2 |
| Cauda equina | 3 |
| Posterior Ligamentous Complex Integrity | |
| Intact | 0 |
| Injury suspected/indeterminate | 2 |
| Injured | 3 |
From Vaccaro AR, Lehman RA Jr, Hurlbert RJ, et al: A new classification of thoracolumbar injuries: the importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine (Phila Pa 1976) 30:2325-2333, 2005.
A numeric value is assigned for each injury subcategory based on the severity of injury. These individual scores are then added to produce an injury severity score, which, in turn, aids in medical decision making by providing both diagnostic and prognostic information with a weighted injury severity score. Stable injury patterns (TLICS <4) may be treated nonoperatively with brace immobilization and active patient mobilization. Unstable injury patterns (TLICS >4) may be treated operatively with deformity correction and neurologic decompression and spinal stabilization, followed by active patient mobilization.
Although the TLICS system has shown good to excellent intra- and interobserver reliability throughout a spectrum of spine treatment providers,18,19 many of the initial studies were performed by individuals involved with its development. Therefore, a broader application of the system across multiple physicians and trauma centers may further validate or refute this classification system in the future.
American Spinal Injury Association: Reference Manual of the International Standards for Neurological Classification of Spinal Cord Injury, ed 6, Chicago, 2003.
La Rosa G., Conti A., Cardali S., et al. Does early decompression improve neurological outcome of spinal cord injured patients? Appraisal of the literature using a meta-analytical approach. Spinal Cord. 2004;42:503-512.
Magerl F., Aebi M., Gertzbein S.D., et al. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994;3:184-201.
Vaccaro A.R., Lehman R.A.Jr., Hurlbert R.J., et al. A new classification of thoracolumbar injuries: the importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine. 2005;30:2325-2333.
White A.A., Panjabi M.M. Clinical biomechanics of the spine, ed 2. Philadelphia: Lippincott; 1990.
1. White A.A., Panjabi M.M. Clinical biomechanics of the spine, ed 2. Philadelphia: Lippincott; 1990.
2. Saifuddin A. MRI of acute spinal trauma. Skeletal Radiol. 2001;30:237-246.
3. Dolan E.J., Tator C.H., Endrenyi L. The value of decompression for acute experimental spinal cord compression injury. J Neurosurg. 1980;53:749-755.
4. Aki T., Toya S. Experimental study on changes of the spinal-evoked potential and circulatory dynamics following spinal cord compression and decompression. Spine (Phila Pa 1976). 1984;9:800-809.
5. Vaccaro A.R., Daugherty R.J., Sheehan T.P., et al. Neurologic outcome of early versus late surgery for cervical spinal cord injury. Spine (Phila Pa 1976). 1997;22:2609-2613.
6. Duh M.S., Shepard M.J., Wilberger J.E., Bracken M.B. The effectiveness of surgery on the treatment of acute spinal cord injury and its relation to pharmacological treatment. Neurosurgery. 1994;35:240-249.
7. Tator C.H., Duncan E.G., Edmonds V.E., et al. Comparison of surgical and conservative management in 208 patients with acute spinal cord injury. Can J Neurol Sci. 1987;14:60-69.
8. La Rosa G., Conti A., Cardali S., et al. Does early decompression improve neurological outcome of spinal cord injured patients? Appraisal of the literature using a meta-analytical approach. Spinal Cord. 2004;42:503-512.
9. Baptiste D.C., Fehlings M.G. Update on the treatment of spinal cord injury. Prog Brain Res. 2007;161:217-233.
10. American Spinal Injury Association: Reference Manual of the International Standards for Neurological Classification of Spinal Cord Injury, ed 6, Chicago, 2003.
11. Frankel H.L., Hancock D.O., Hyslop G., et al. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. I. Paraplegia. 1969;7:179-192.
12. Geisler F.H., Coleman W.P., Grieco G., Poonian D. Measurements and recovery patterns in a multicenter study of acute spinal cord injury. Spine (Phila Pa 1976). 2001;26:S68-S86.
13. Kelly R.P., Whitesides T.E.Jr. Treatment of lumbodorsal fracture-dislocations. Ann Surg. 1968;167:705-717.
14. Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976). 1983;8:817-831.
15. Magerl F., Aebi M., Gertzbein S.D., et al. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994;3:184-201.
16. Schweitzer K.M.Jr., Vaccaro A.R., Lee J.Y., Grauer J.N. Confusion regarding mechanisms of injury in the setting of thoracolumbar spinal trauma: a survey of the Spine Trauma Study Group (STSG). J Spinal Disord Tech. 2006;19:528-530.
17. Vaccaro A.R., Lehman R.A.Jr., Hurlbert R.J., et al. A new classification of thoracolumbar injuries: the importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine (Phila Pa 1976). 2005;30:2325-2333.
18. Patel A.A., Vaccaro A.R., Albert T.J., et al. The adoption of a new classification system: time-dependent variation in interobserver reliability of the thoracolumbar injury severity score classification system. Spine (Phila Pa 1976). 2007;32:E105-E110.
19. Raja Rampersaud Y., Fisher C., Wilsey J., et al. Agreement between orthopedic surgeons and neurosurgeons regarding a new algorithm for the treatment of thoracolumbar injuries: a multicenter reliability study. J Spinal Disord Tech. 2006;19:477-482.
20. Louis R. Spinal stability as defined by the three-column spine concept. Anat Clin. 1985;7:33-42.