Chapter 24 Surgical diathermy
Physical principles
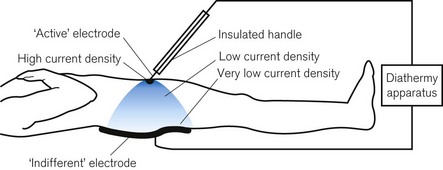
Radio frequency (RF) surgical diathermy or electrosurgery uses the heat generated by an electric current,1 often delivered at more than 200 V, passing through a small amount of tissue to cut, destroy or vaporize that tissue and to create haemostasis by causing coagulation and sealing of small blood vessels. Passing an electric current through the body causes all the tissue through which it passes to heat up. For this effect to be clinically useful, the current must pass through a small area of tissue at the active electrode. In contrast, at the indifferent electrode of the diathermy plate, which completes the electrical circuit, the current must pass from the skin surface to a large area to prevent burns where they are undesirable. This is the concept of current density.
Current density
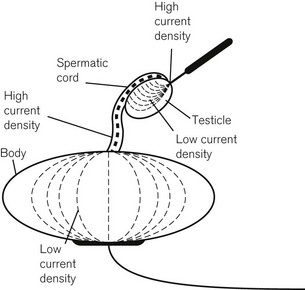
Current density refers to the current per unit cross-sectional area. With a large conductive area, such as at the patient plate, there is a low current density and, although the amount of heat generated is the same at the active electrode, the heat is rapidly conducted away. At the contact point of the active electrode, the current density is high, the heat being generated over a small area, thus creating the desired surgical effect (Fig. 24.1).
It is necessary to pass considerable currents through the human body to produce enough heat to have this effect. Under normal circumstances, the accidental passage of electric current at mains frequency (50 Hz) through the body has several highly undesirable effects, including burns, muscle spasm leading to asphyxiation and ventricular fibrillation. However, it was found experimentally years ago that, although living tissues, especially conducting and contractile tissues, are maximally sensitive to electric current at mains frequency, this sensitivity decreases at lower frequencies (including direct current (DC)) and decreases markedly at very high frequencies (Fig. 23.3).
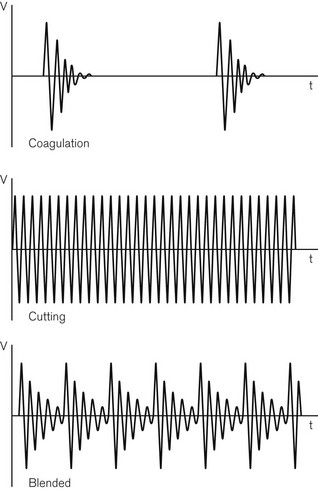
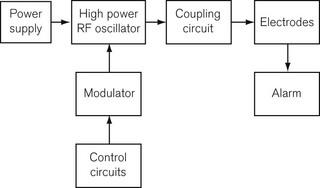
Diathermy frequencies used in surgery are in the region of 0.4–1.5 MHz. RF diathermy machines are, in fact, powerful radio transmitters and would cause severe interference to radio receivers, even at some distance. Without good screening, RF diathermy signals can capacitatively couple with ECG or other amplifiers and grossly interfere with the biological signal being monitored. For this reason, by international agreement, only certain narrow frequency bands are used. A sine waveform has been found to be better for cutting and a damped waveform for coagulation (Fig. 24.2). A combined waveform is also available, usually referred to as ‘blend’, which is commonly used during cystoscopic resections of a bladder tumour or prostate. Although the frequency band is narrow, the current required to produce an effect may vary widely between patients as shown in a study in patients during prostatectomy.2 A block diagram of a RF diathermy machine is shown in Fig. 24.3. A high-power, high-frequency oscillator or generator is controlled by a modulator to produce the necessary waveforms. The output of the generator is led through coupling circuits to optimize impedance matching between the generator and the ‘indifferent’ and the ‘active’ electrodes. The circuitry normally contains a 0.01 µF capacitor from the indifferent electrode to earth. It will be recalled that the electrical impedance (the term used to describe electrical resistance at different frequencies of current) is inversely proportional to both the frequency of the current and the magnitude of the capacitance; therefore, this capacitor in the diathermy circuit provides a low impedance (20 Ω) route to earth for the high-frequency diathermy current, but a high impedance (300 kΩ) to any incidental low-frequency mains current. This effectively isolates the circuit from earth against mains leakage current. The risk of electrocution from a diathermy apparatus is, therefore, much reduced, but the risk of burns should not be underestimated (see below). Where the indifferent lead (i.e. the plate) socket is at earth potential, as it is in many older diathermy sets, it is vitally important that the lead is connected to the correct terminal of the diathermy apparatus. If the plate were accidentally connected to the active terminal, when the foot switch is depressed the patient might be burned at all points connected to earth (i.e. where the body is in contact with those parts of the operating table at earth potential).
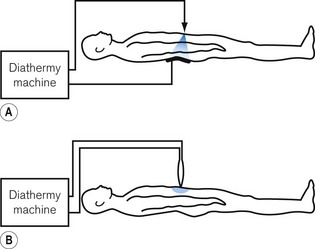
The above description is of a unipolar arrangement. However, some diathermy sets are capable of being used with a bipolar system in which the current passes from one blade of a pair of forceps to the other. The circuit is earth-free and the current does not pass through any part of the patient’s body, other than that grasped by the forceps (Fig. 24.4). The power required is small and electrically safer, but it is suitable only for the coagulation of small pieces of tissue or blood vessels. It is particularly suitable for ophthalmic or neurosurgical procedures, and is also more acceptable in the presence of a cardiac pacemaker (see below). From a safety point of view, it should be used whenever possible.
Accidents due to diathermy
Electrical burns
Electrical burns occur with diathermy use in the following ways:
• Accidental depression of the foot switch when the forceps or cutting electrode is inadvertently in contact with some part of the patient can result in significant burns. This may be prevented by keeping the forceps in an insulated quiver when not in use; it is also minimized by the installation of an audible alarm which sounds when the foot switch is depressed. This must never be turned down to inaudible levels. The indicator light on the machine is useful as a confirmation that the machine is working, but cannot warn of unintentional activation.
• Burns can arise where there is intermittent or partial contact of the plate surface and the skin resulting in areas of high current density due to the small area of contact at these points. Some diathermy machines give an audible warning if the plate lead is not plugged in, or if the electrical continuity of the lead is broken. However, an absence of the audible warning is not proof that the plate has been correctly applied to the patient. Some diathermy sets incorporate an isolating transformer which allows them to have a fully floating output; the patient is then unharmed if the indifferent electrode is neglected, providing it is not inadvertently connected to earth.
• Burns can also be caused, even if the patient plate is not applied, by the electrical circuit being completed via the operating table and the floor, or other points through which a patient may be inadvertently earthed. Although ECG leads represent the most likely pathway to earth to allow diathermy burns, other monitors can also provide an earth route resulting in burns from radio frequency currents; these can include temperature probes3 and Doppler probes.4 It is also possible, for example, for the tracheal mucosa to be severely damaged if the patient is inadvertently earthed through the damp endotracheal tube and the anaesthetic machine, hence the use of isolating transformers on modern electrically powered anaesthetic workstations.
• Another danger, which is seldom appreciated, is the risk of infarction when unipolar diathermy is used on an organ which has been temporarily raised on its vascular pedicle. The classical injury is that caused to the testis, when raised from the scrotum on its vas deferens. Fig. 24.5 shows that the current density is greatly increased in the vas, thus causing its destruction. For this reason, bipolar diathermy is by far the preferred option. The same applies to diathermy for use in appendages such as digits. If unipolar diathermy must be used, then the exposed testis must remain in contact with the rest of the body and its electrical conduction must be improved by the interposition of a saline soaked swab.
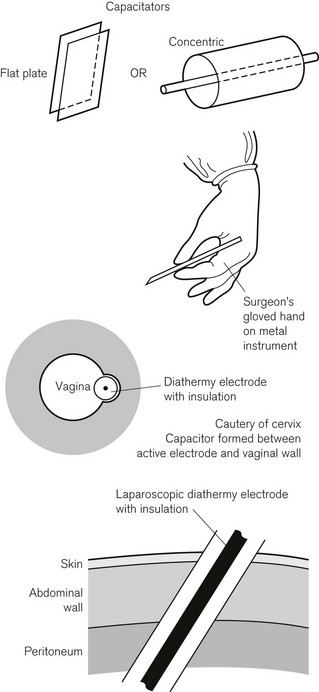
• Burns can be caused by capacitative coupling through intact insulation. The concept of capacitative coupling is shown in Fig. 24.6. Any two electrical conductors separated by an insulator form a capacitor. Such a capacitor can be formed in the space between, for example, the metal lighting housing over an operating table and the patient on the table. This is one pathway for inducing a (mains frequency) capacitative current in another electrical circuit connected to a patient (ECG leads), which may merely distort the ECG signal (see Chapter 14). One property of a capacitor is its decreasing impedance (the term used to describe frequency-dependent electrical resistance) and, therefore, increased current flow as the frequency of the AC current increases. This means that high-frequency diathermy currents are a significant potential hazard for burns in this respect. A capacitor may be formed between the diathermy probe and a surgeon’s finger holding that probe, with the surgeon’s glove acting as the intervening insulator.5 Burns may be caused to the surgeon’s gloved fingers in contact with the probe by capacitative coupling if the capacitatively induced current through the surgeon’s finger finds a pathway to earth (for example through his boots, if there is not perfect insulation to the floor, or through his contact with another earthed surface). Another example of a capacitor is an insulated diathermy probe in contact with the vaginal wall during cervical cautery; burns to vaginal tissue might occur by capacitative coupling if the induced current finds an earth pathway, which it might do despite best attempts to avoid this; note that no assumption is made in these examples concerning an earthed, a non-earthed or a faulty diathermy circuit. Another example of possible capacitative coupling can occur during laparoscopic surgery (see below). The probe and the surrounding tissue act as capacitor plates, with the probe’s insulation between them; capacitative coupling of high-frequency diathermy current may result in a tissue burn at this site rather than at the probe tip when the diathermy is activated.
Diathermy and laparoscopic surgery
In the same way as external diathermy has hazards, laparoscopic surgery also has electrical hazards associated with its use.6 There is a danger of current leakage to the patient from laparoscopic instruments, causing either apparent malfunction of laparoscopically applied unipolar diathermy, or tissue damage at the cannula site or other sites outside the operator’s field of vision.
The stray current pathways may be due to:
• insulation breaks in the diathermy applicator
• capacitative coupling through intact insulation; or
• direct coupling between the active electrode and other organs or metal instruments outside the field of vision.
Capacitative coupling between a laparoscopic cannula and electrically isolated but adjacent tissues is shown in Fig. 24.6. The problem is aggravated by the use of plastic-coated cannulae of small diameter, which are used to produce smaller scars;7 the smaller the cannula, the greater the capacitance and the larger the stray current passed at a given frequency.
Diathermy and pacemakers
The use of RF diathermy should be avoided in patients with internal or external pacemakers as there is a risk of inhibition of or damage to the pacemaker, either of which can cause its failure to function.8 There is also the risk of causing burns to cardiac tissue at the conductive sites of the pacemaker wire. Bipolar diathermy is much preferred if diathermy must be used and then only at sites well away from the pacemaker and its connections.9 This is discussed further in Chapter 25.
Fires and explosions
The causes of fires and explosions, of which diathermy may be one,10 are discussed in Chapter 23. The external cases of diathermy machines are made to be gastight. Pressure gradients can develop across the gas-proof seal; if, due to an internal electrical fault, the inside of the device is heated and fumes are generated, rupture of the device can occur.
1 Haag R, Cuschieri A. Recent Advances in high frequency electrosurgery: development of automated systems. J Roy Coll Surg Edinb. 1993;38:354–364.
2 Hill PD. Measurement of surgical diathermy current during transurethral resection of the prostate gland. Clin Phys Physiol Meas. 1992;13:323–334.
3 Parker EO. Electrosurgical burn at the site of esophageal temperature probe. Anaesthesiology. 1984;60:93–95.
4 Block EC, Burton LW. Electrosurgical burn using a battery operated Doppler monitor. Anaesthesia and Analgesia (Cleve). 1979;58:339–342.
5 Tucker RD, Ferguson S. Do surgical gloves protect staff during electrosurgical procedures? Surgery. 1991;110:892–895.
6 Department of Health. Safety Action Bulletin – Diathermy injury during laparoscopic surgery, SAB (94)38 September 1994, London, Department of Health, 1994.
7 Voyles CR, Tucker TD. Education and engineering solutions for potential problems with laparoscopic monopolar electrosurgery. Am J Surg. 1992;164:57–62.
8 Kellow NH. Pacemaker failure during TURP. Anaesthesia. 1993;48:136–138.
9 Allen M. Pacemakers and implantable cardioverter defibrillators. Anaesthesia. 2006;61:883–890.
10 Dhebri AR, Afify SE. Free gas in the peritoneal cavity: the final hazard of diatherm. Postgrad Med J. 2002;78:496–497.